Women’s Knowledge of Genomic Testing and Precision Medicine in Breast Cancer Treatment Decision-Making
Purpose: To understand awareness of genetic and genomic testing, as well as decision-making, in women diagnosed with breast cancer.
Participants & Setting: 29 African American/Black and Latina/Hispanic women diagnosed with breast cancer.
Methodologic Approach: A semistructured interview guide was used in focus groups conducted via videoconference. Transcripts were analyzed using thematic analysis.
Findings: Many of the women understood the concept of genetic testing to identify the BRCA1/BRCA2 variant, but none of them were aware of genomic testing and its implications for personalized medicine. Participants discussed provider and patient roles in treatment decision-making, identifying roles that the physician might play in treatment planning, from primary decision-maker to collaborator.
Implications for Nursing: As the number of precision cancer treatments expands, patients must be able to comprehend the information provided to make informed decisions about their treatment. Providers should do a better job of explaining potential treatments so that patients feel they are part of the decision-making process. Addressing gaps in treatment access and uptake requires providers to prioritize patient engagement and understanding.
Jump to a section
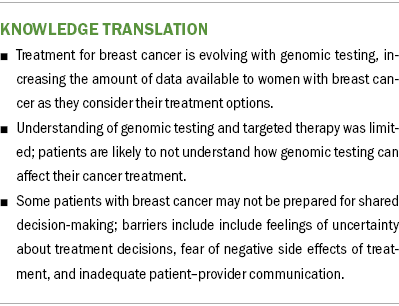
Breast cancer (BC) surgery can be considered preference sensitive in that women diagnosed with the disease may have choices to make regarding their treatment. For example, there may be two or more surgical treatment options that are equally effective (Baliski & Hamm, 2020). Because of the opportunity to weigh in on treatment options, there has been an active effort to increase shared decision-making, particularly for women with early-stage cancer (Shickh et al., 2023). Advances in genetic and genomic testing have increased the amount of data available to women as they consider their options for BC treatment (Baliski & Hamm, 2020; Shickh et al., 2023). Covvey et al. (2019) found that barriers to shared decision-making included feelings of uncertainty about treatment decisions, fear of negative side effects of treatment, and inadequate patient–provider communication.
Genetic testing checks for variants or changes in a person’s DNA, but genomic testing examines a tumor’s molecular composition. Advances in genomic testing have led the way toward precision medicine, a treatment that is specific to a tumor’s genetic polymorphism. This focused treatment has been found to improve the overall efficacy of cancer treatment in clinical trials and practice. However, according to a study by Pinilla et al. (2022) about precision medicine in early-stage triple-negative BC, translating research into practice in BC continues to be a long-term challenge.
Various factors contribute to the underuse of precision medicine in clinical practice, including patient-level factors, such as a lack of knowledge and awareness and serious concerns about the possible release or misuse of test results (Erdmann et al., 2021); physician-level factors, such as a lack of knowledge about and confidence in the use of precision medicine (Schaibley et al., 2022); and system-level factors, such as cost (Bombard et al., 2015) and a lack of genetic counselors (Bamshad et al., 2018).
The decision to use precision medicine in BC would directly follow from the oncologist’s knowledge of and comfort with ordering genetic and genomic testing for certain cancers. Although there is limited evidence in the literature regarding physicians’ knowledge of such testing, a study of 262 physicians in various specialties from the University of Kansas Medical Center found that 63% of the respondents did not believe that their genetics education in medical school or residency had adequately prepared them to use genetic testing on their patients (French et al., 2023).
In 2019, at six conference settings, community-based oncologists were surveyed using case studies to determine whether they could match the genetic variant to the targeted therapy most appropriate for that alteration, a necessary step in the use of precision medicine (Singh et al., 2019). More than 60% of the oncologists answered questions incorrectly or stated that they did not know the answers. To compare community oncologists with those in academic practice, community oncologists reported using genomic testing for patients with lung cancer 33% of the time, whereas academic oncologists used genomic testing 74% of the time in patients with lung cancer (Singh et al., 2019). Delays in the diffusion of new treatments to physicians in community settings as compared to physicians in academic medical centers can be mitigated by the presence of a local champion for innovation (Jerome-D’Emilia & Begun, 2005).
An additional factor implicit in the consideration of precision medicine is the stage of disease. Although the National Comprehensive Cancer Network (2024) guidelines recommend the use of genomic testing in the staging of BC, as of April 2024, the guidelines do not include specific recommendations for the use of precision medicine. Genomic testing is frequently used to determine whether to order chemotherapy in the treatment of BC (Bombard et al., 2015; Sparano et al., 2019).
Many clinical trials are evaluating the use of precision medicine in the BCs that are most difficult to treat, primarily metastatic BC. As for early-stage disease, triple-negative BC has a high risk of distant recurrence and death and limited options for commonly used treatments, so it is also an important area for clinical trials (Pinilla et al., 2022).
When looking at knowledge of genomic testing and precision medicine in women diagnosed with BC, the oncologist’s knowledge of and comfort with the use of genomic testing and precision medicine is a major factor in the patient’s awareness and knowledge of this field of medicine. However, when genetic and genomic testing are ordered, new questions may be raised about how and when complex information should be shared with women diagnosed with BC (Tsimberidou et al., 2020). Researchers have explored women’s preferences for receiving test results (Kaphingst et al., 2016), the amount and type of information women want to receive with test results (Schmidlen et al., 2014; Seo et al., 2017), and the prevalence of patient-centered communication in clinical encounters in which test results are shared (O’Neill et al., 2021). Genetic testing may have implications for a patient’s family in addition to the patient’s treatment, so shared decision-making concerning whether to test at all, as well as how and when to share information, is crucial. To best inform patients and engage them in decision-making, oncologists and surgeons caring for patients with cancer must not only offer the appropriate testing but also educate their patients so that they can understand why the tests are being recommended, what the benefits may be, and how their treatment may be configured for optimum efficacy.
The primary aim of this study was to ascertain the level of knowledge of genetic and genomic testing and precision medicine in a diverse group of women diagnosed with BC. In addition to this aim, the perceptions that women had about their role in decision-making in relation to their physician’s style of presenting treatment information were assessed.
Methodologic Approach
This qualitative study used focus group methodology. The sample consisted of women who received BC treatment at MD Anderson Cancer Center at Cooper in Camden, New Jersey. To recruit participants, the research team distributed flyers (in English and Spanish) to women in hospital-affiliated BC support groups, as well as to healthcare providers. The flyers instructed prospective participants to contact a research team member via telephone or email. The research team member did an initial verbal review of the informed consent process, and, if the prospective participant agreed to move forward, offered date, time, and language options for focus groups. Eligible women identified as African American/Black or Latina/Hispanic, were aged 18 years or older, and spoke English or Spanish. The women had to have completed treatment for BC (stage I, II, or III) in the past year, or they were living with metastatic cancer (stage IV). This study was reviewed and considered exempt by the Cooper University Hospital Institutional Review Board.
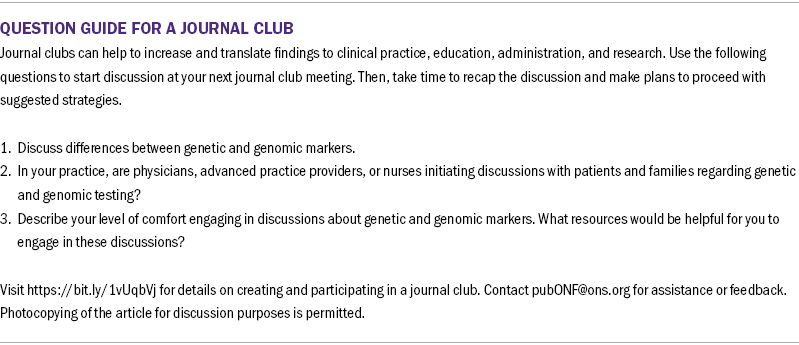
Six focus groups were conducted remotely using videoconferencing technology during March 2022 and completed when saturation was reached. The 60- to 90-minute focus groups, with two to nine participants per group, were conducted during a two-week period. One group was entirely in Spanish, and the remaining five were conducted in English. Each focus group began with a reading of the informed consent, followed by a series of open-ended questions and follow-up prompts (see Figure 1). Each participant received a $25 gift card. All interviews were audio recorded with permission and transcribed verbatim.
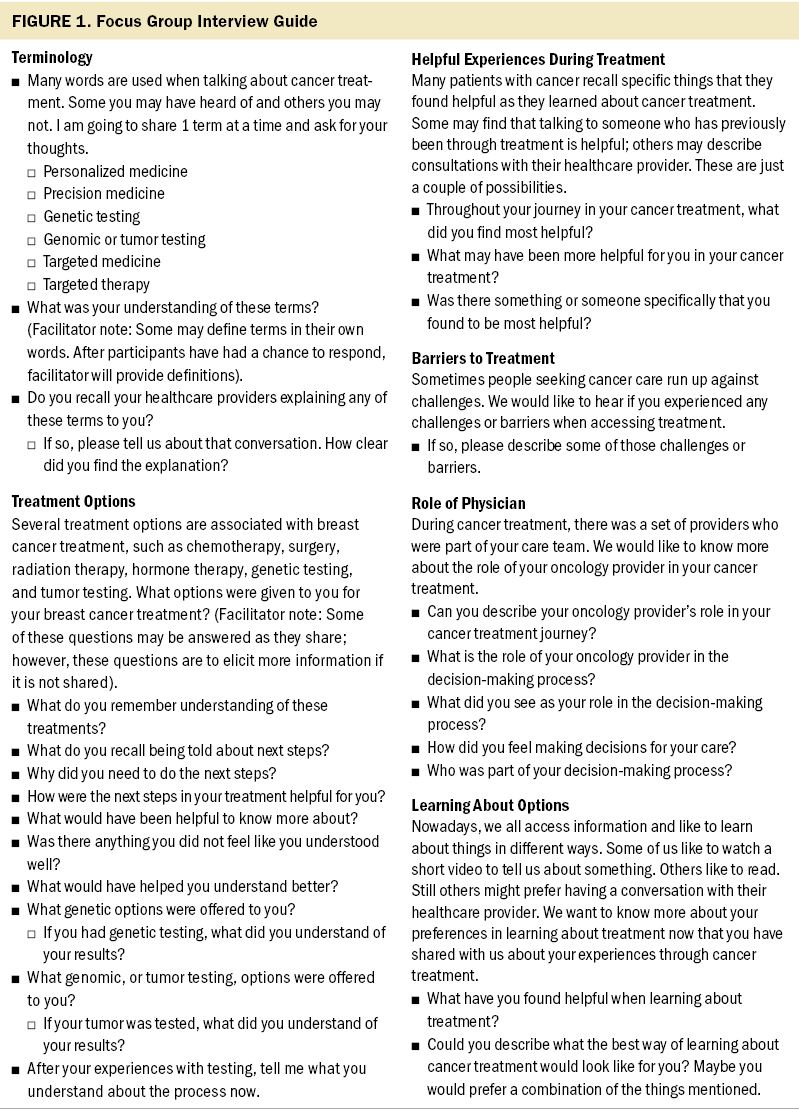
Transcripts were analyzed using thematic analysis, which allows researchers to draw themes from the experiences and knowledge of the participants (Braun & Clarke, 2006). To begin the analysis, two members of the research team (B.S. and L.H.) independently reviewed the audio recordings and transcripts to begin the coding process by identifying relevant text and attaching labels to these sections. The use of multiple researchers allowed for investigator triangulation, which would improve the credibility of the results (Polit & Beck, 2018). Working iteratively and collaboratively, the researchers were able to recognize patterns and recode initial labels into categories of increased abstraction (Wuest, 2012). These two researchers agreed on a specific number of codes, which were organized and compiled into themes. E.R.-R., C.O., S.W., and B.J.-D. then reviewed the audio recordings and transcripts, considering the identified themes, and any differences were resolved through consensus.
Findings
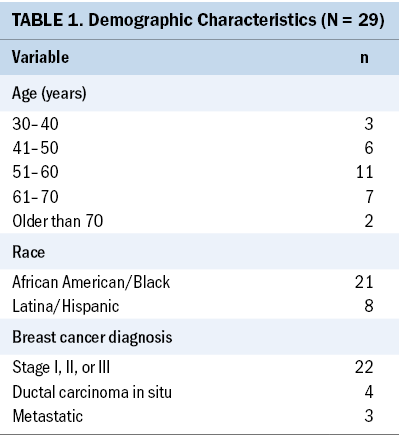
Twenty-nine women participated in this study. Of these, 21 identified as African American/Black and 8 as Latina/Hispanic (see Table 1). Five of the Latina/Hispanic participants chose to join the Spanish-language focus group, with the other Latina/Hispanic participants joining an English-speaking group. Group members’ ages ranged from 32 to 79 years, with an average age of 55 years. Three participants stated that they were diagnosed with metastatic cancer (stage IV), and 22 reported having undergone treatment in the past year for stage I, II, or III BC; despite presenting the inclusion criteria during recruitment, 4 participants later reported that they were diagnosed with ductal carcinoma in situ.
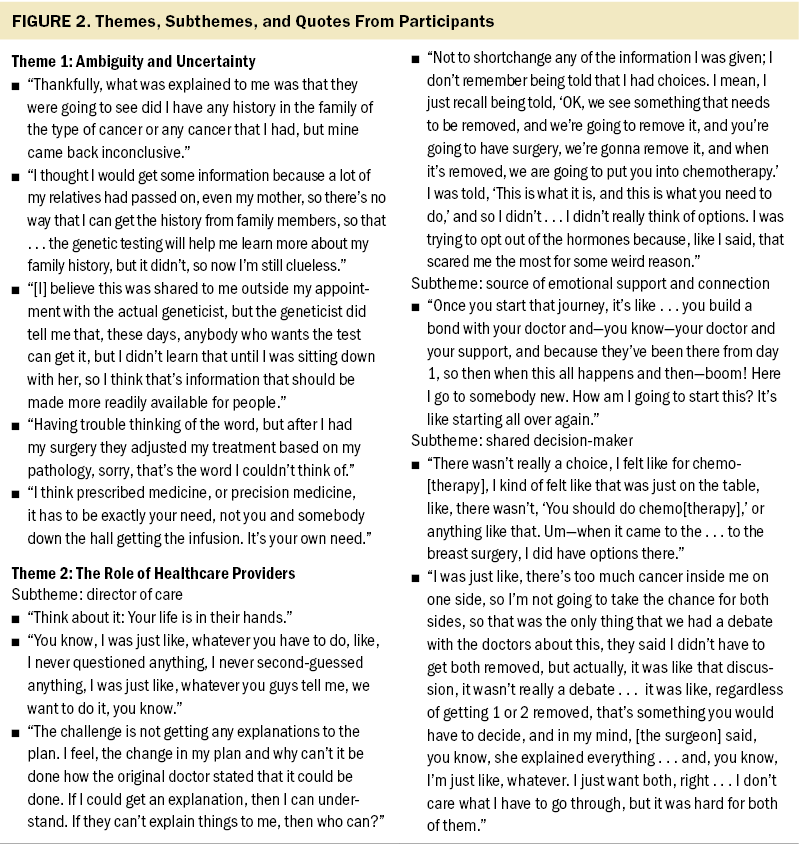
Two main themes and several subthemes were noted in the transcripts. The themes found were (a) ambiguity and uncertainty and (b) the role of healthcare providers. The themes shared a focus on aspects of obtaining necessary knowledge to potentially allow for a shared decision-making model in the treatment of BC, including lack of adequate knowledge, need for more information, the source and timing of information, and the women’s perceptions of their providers as sources of information and support.
Theme 1: Ambiguity and Uncertainty
Early in each focus group, the interviewer introduced several terms, such as personalized medicine, precision medicine, genetic testing, genomic or tumor testing, targeted medicine, and targeted therapy. Of these terms, genetic testing elicited the most widespread recognition, with most participants indicating that they recognized the term and understood its meaning. Those who offered definitions linked their understandings to personal experiences, describing either their own genetic testing experiences or their reasons for not pursuing genetic testing when it was offered. However, none of the participants understood the concepts of precision or personalized medicine as a means of using genomic testing to identify a more targeted approach for their treatment. The connections that most of them made with genetic testing appeared to be related to testing for the BRCA1/BRCA2 gene variant. Figure 2 presents themes and corresponding quotes.
Although participants shared their perception that their doctors had adequately explained genetic testing and that testing had been offered to them, perceptions differed as to the value of such testing. Several reported that their testing results did not provide useful information. Most understood genetic testing to have the potential to help inform decision-making, not only for themselves but also for their family members, but few were able to identify genetic testing as informing their treatment processes. Those who had opted for genetic testing linked their decisions to family dynamics, both past and future. Some spoke of having approached genetic testing as an opportunity to get information that was no longer available to them directly because of deaths or separations from families of origin. Others connected genetic testing to concerns for their own children’s health.
One participant in the Spanish-language focus group shared that she had declined to get genetic testing based on her understanding that it was not needed for her because she was the first person in her family to ever have cancer. Similarly, a participant in another focus group shared that, at the time of her genetic testing, she had not understood that the testing could be potentially beneficial for her treatment.
Understanding of targeted therapy was also quite limited. Three participants in the Spanish-language group described targeted medicine as treatment you receive for your specific cancer because not all cancers are the same. The women understood targeted treatment as that which was based on their specific histology. Two participants linked personalized treatment to their experiences of having received personal care and attention from doctors. Other participants linked the concept of personalized medicine to adjustments in chemotherapy made because of adverse reactions. In two of the focus groups, the word targeted led to a discussion among participants about their doctors having drawn boundaries around tissue to be targeted for radiation. Several participants noted the difficulty in retaining and recalling the information they received, particularly when treatments have similar names, when different providers use different terms, and when a great deal of information is presented at the same time. One participant stated, “The terms that doctors use are difficult to understand sometimes, as these are not words widely used.” Another participant explained, “I don’t think there was anything else they could have told me, um, I just kind of wish I understood it a little bit more.”
Theme 2: The Role of Healthcare Providers
Focus group participants described the role of their physicians (surgeons and oncologists) as fitting into the following three subthemes: director of care, source of emotional support and connection, and shared decision-maker. However, these subthemes were not mutually exclusive, in that a given participant may have experienced different types of interactions with the same doctor at different stages of treatment.
Subtheme: director of care: Participants whose responses aligned with the director of care subtheme shared that they saw the doctor’s role as applying expertise to construct a treatment plan and the patient’s role as being to follow that plan, without any room for shared decision-making. Women’s experiences of their provider as a director of care were not always positive. One of the Spanish language–group participants stated that change over time in her doctors led to significant changes in her treatment plan without adequate explanation.
Although the women did not directly consider their role to include decision-making when receiving care from a director of care–inclined physician, several women shared their perceptions of finding encouragement and reassurance in instances when their physicians altered advice or changed the course of treatment as new information emerged. They interpreted the fact that their physicians communicated such changes with them in an ongoing and open way as signifiers of a trusting patient–doctor relationship. One woman stated, “I just left it up to the doctors and I tried not to look too deep into it, because—I’m like, ‘It’s out of my hands, it’s out of my control.’”
Subtheme: source of emotional support and connection: Participants spoke at length about their doctors as sources of emotional support and connection. They placed a high value on concrete manifestations of emotional support or connection from doctors, including hugs, photos taken with the treatment team at key moments in the treatment process, and the provision of a telephone number that participants could call for support at any time. One Spanish-language participant connected her experiences of emotional support and connection to her own professional role as a cosmetologist and to faith. She stated, “I’m a cosmetologist, and I felt like I wasn’t in the hospital, that I was in the beauty salon, because the people there are a blessing from God.”
Two participants identified the emotional connection they felt with their doctors as something they recognized retrospectively after losing those providers to a retirement or job change.
Subtheme: shared decision-maker: In some instances, participants described the role of the physicians as providing clear, comprehensive information on more than one option, and their patient role as being able to choose, from among these options, the one that best suited them. Women described primarily being given options for surgery. For example, some of the women were given the choice between a lumpectomy and a mastectomy, as well as between a single and bilateral mastectomy. Participants often identified choices being given in terms of more aggressive or less aggressive options; for example, choosing a bilateral mastectomy although their cancer had been confined to one breast was a more aggressive option. One participant stated:
There wasn’t really a choice, I felt like, for chemo[therapy], I kind of felt like that was just on the table, like, there wasn’t, “You should do chemo[therapy],” or anything like that. Um—when it came to the . . . to the breast surgery, I did have options there.
When characterizing their relationships with physicians as shared decision-making, with options given by providers and considered by patients, participants recognized a distinction and hierarchy between information and treatments needed for survival and information and treatments related to appearance. The decision to have a bilateral mastectomy appeared to be one that patients made on their own after being presented with choices of surgical treatments.
Discussion
The primary aim of this study was to assess knowledge and understanding of advances in BC care that are the result of genetic and genomic testing in a diverse sample of women. Although the women were all treated at the same location, the women were not necessarily all low income, and their insurance status was unknown. Despite demographic variations, responses were quite consistent regarding questions about precision medicine or targeted treatment. All the women recalled discussions with their physicians about genetic testing; however, it was clear they were more likely to be thinking of BRCA1/BRCA2 testing rather than testing of the tumor to allow for focused treatment (i.e., genomic testing). BRCA1/BRCA2 testing has been used in clinical practice for more than 20 years (Toland et al., 2018). Since 2013, when actress Angelina Jolie made public her decision to undergo a bilateral mastectomy because of BRCA1/BRCA2 testing, social media mentions and public awareness campaigns have increased knowledge of the test (Gubar, 2018). This is not the case for genomic testing and precision medicine.
Stallings et al. (2023) evaluated women’s knowledge of genetic testing and precision medicine in a sample of women recruited at a federally qualified community health center in Tennessee. Their sample was primarily African American/Black (89%), and the highest level of education was a high school diploma. This study found that the women were confused about precision medicine and genetic testing. Although a subjective measure of health literacy was relatively high in this sample, 42% of the participants believed that genes had little effect on health. This lack of understanding is consistent with what was found in the current study.
In a qualitative study of Black and White women diagnosed with BC and prescribed chemotherapy, genetic knowledge was found to be relatively high, which may be related to the fact that the majority of the women (74.5%) had at least some college education (McCall et al., 2021). In this study, years of education and household income were found to be associated with increased genetic knowledge. Genetic knowledge was evaluated with a basic genetic knowledge test; Black women scored lower, although there were two questions of basic knowledge that they were more likely to answer correctly. The researchers concluded that genetic knowledge was high in this group and that Black women did not appear to be hesitant to participate in research of this kind, although it was noted that two of the Black participants declined germline genetic testing that was recommended by their physician and one of the Black participants limited her testing to BRCA1/BRCA2 even though a more comprehensive screening test was recommended (McCall et al., 2021). The findings of this study should encourage further research that goes beyond the question of race and ethnicity as determining factors in a patient’s understanding of genetic and genomic testing. Unfortunately, neither education level nor income was reported in the study, so such considerations cannot be addressed.
When considering knowledge and understanding of information provided to patients with BC in general, the theme of ambiguity and uncertainty also emerged in the context of women’s experiences of getting a large amount of or too much information and being unable to fully understand it. In a qualitative study of 313 women who had been diagnosed with BC in a diverse sample, Freedman et al. (2022) found that patients’ knowledge about BC and their treatment showed great variation. More than 25% of the women reported that they actively avoided information, and Black and Latina respondents were less likely to be able to answer questions about their cancer. The women interviewed in this study expressed concern with the overwhelming amount of information they were provided.
A woman’s understanding of her disease and treatment can be expected to play a role in her readiness for shared decision-making. In an American Society of Clinical Oncology Educational Book, Shickh et al. (2023) explained the importance of shared decision-making in the care of patients diagnosed with BC, particularly in reference to the use of genetic testing. With the goal of clinician and patient cocreating a comprehensive cancer plan, patients should be provided with the tools to further their understanding of the proposed treatment so that they can make informed decisions about their plan of care. However, as in the subtheme of director of care, it was apparent that not all clinicians were promoting shared decision-making, and it is possible that not all patients are ready to take on that role.
In a study on patients’ perceptions of shared decision-making, Josfeld et al. (2021) found that participants reported a high need for information, which correlated with their education level, but that they also felt overwhelmed by the amount of information needed, which was consistent with the findings in the current study. In a study of cognitive biases that can affect decision-making, Ozdemir and Finkelstein (2018) describe one such bias, power distance, as the inequality that exists between more and less powerful members of society. Physicians tend to be seen as very powerful members of society, and patients who perceive physicians in this respect may want to follow the physician’s guidance regardless of their own desires to determine treatment. This is consistent with the subtheme of director of care, in which participants in the current study held the physician in high regard and wanted them to be the decision-maker in the treatment plan.
Limitations
As in all qualitative research, limitations to generalizability may occur. The focus groups in this study were conducted within a community with a low socioeconomic status and with a diverse sample of women. However, the participants were not asked about insurance coverage or income, so it is not possible to say that this was a low-income group of women; these factors may limit the generalizability of these findings. In addition, the researchers relied on participants’ reports regarding their stage of cancer and treatments used, but they did not confirm these reports with the patients’ health records.
Additional limitations may be related to the fact that this study limited enrollment to African American/Black and Latina/Hispanic women; therefore, assumptions cannot be made as to whether poverty, rather than race and ethnicity, may be a determining factor in a woman’s knowledge of precision medicine. One can assume that patients who are being treated in low-resource hospitals, specifically those located in rural areas, or that treat a high percentage of uninsured patients or Medicaid recipients may be less likely to use innovative, high-technology treatments. Further research is needed to determine additional and potentially modifiable factors that may limit a patient’s knowledge of genomic testing and precision medicine.
Implications for Nursing and Conclusion
Despite numerous studies of decision-making in BC treatment, as new methods of treatment (such as precision medicine based on genomic testing) evolve, there will be a need for more information to be shared with patients to allow for informed decision-making. The findings from this study make clear that women do not understand the very basics of genomic testing, although all participants were aware of BRCA1/BRCA2 genetic testing. Efforts to educate patients in general about the promise of precision medicine would be a first step in bringing this level of treatment to patients with cancer. Based on this sample, it appears that providers need to adjust their approach to patient education and counseling to help patients with BC understand all the ramifications of precision medicine and how they can benefit from these novel approaches to care.
About the Authors
Evelyn Robles-Rodríguez, DNP, APN, AOCN®, is the director of outreach, prevention, and survivorship at MD Anderson Cancer Center at Cooper in Camden, NJ; Linda Houser, PhD, MSW, is a professor in the School of Social Work at Salisbury University in Maryland; Belkys Sanchez, LCSW, is a doctoral student in the Center for Social Work Education at Widener University in Chester, PA; Catherine Ormerod, MSS, MLSP, was, at the time of this writing, the executive vice president and Stefanie Washburn, MSW, LSW, is the manager of healthcare provider outreach, both at Living Beyond Breast Cancer in Bala Cynwyd, PA; Staci K. Oertle, MSN, APN, ANP-BC, AOCNP®, is a lead nurse practitioner at MD Anderson Cancer Center at Cooper; and Bonnie Jerome-D’Emilia, PhD, MPH, RN, is an associate professor in the School of Nursing at Rutgers University–Camden in New Jersey. This research was funded, in part, by grants provided from Genentech (G-79136) to MD Anderson Cancer Center at Cooper and Living Beyond Breast Cancer and by AstraZeneca Pharmaceuticals (72802013) and Gilead (16645) to Living Beyond Breast Cancer. Robles-Rodríguez, Houser, Sanchez, Ormerod, and Washburn contributed to the conceptualization and design. Robles-Rodríguez and Sanchez completed the data collection. Robles-Rodríguez, Houser, and Ormerod provided the analysis. Robles-Rodríguez, Houser, Oertle, and Jerome-D’Emilia contributed to the manuscript preparation. Robles-Rodríguez can be reached at robles-evelyn@cooperhealth.edu, with copy to ONFEditor@ons.org. (Submitted November 2023. Accepted February 14, 2024.)
References
Baliski, C., & Hamm, J. (2020). Does receipt of preference sensitive care impact patient reported outcomes following breast cancer surgery? American Journal of Surgery, 219(5), 746–749. https://doi.org/10.1016/j.amjsurg.2020.02.060
Bamshad, M.J., Magoulas, P.L., & Dent, K.M. (2018). Genetic counselors on the frontline of precision health. American Journal of Medical Genetics. Part C, Seminars in Medical Genetics, 178(1), 5–9. https://doi.org/10.1002/ajmg.c.31610
Bombard, Y., Rozmovits, L., Trudeau, M., Leighl, N.B., Deal, K., & Marshall, D.A. (2015). The value of personalizing medicine: Medical oncologists’ views on gene expression profiling in breast cancer treatment. Oncologist, 20(4), 351–356. https://doi.org/10.1634/theoncologist.2014-0268
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. http://doi.org/10.1191/1478088706qp063oa
Covvey, J.R., Kamal, K.M., Gorse, E.E., Mehta, Z., Dhumal, T., Heidari, E., . . . Zacker, C. (2019). Barriers and facilitators to shared decision-making in oncology: A systematic review of the literature. Supportive Care in Cancer, 27, 1613–1637. https://doi.org/10.1007/s00520-019-04675-7
Erdmann, A., Rehmann-Sutter, C., & Bozzaro, C. (2021). Patients’ and professionals’ views related to ethical issues in precision medicine: A mixed research synthesis. BMC Medical Ethics, 22(1), 116. https://doi.org/10.1186/s12910-021-00682-8
Freedman, R.A., Ko, N.Y., Lederman, R.I., Gagnon, H., Fikre, T., Gundersen, D.A., . . . Keating, N.L. (2022). Breast cancer knowledge and understanding treatment rationales among diverse breast cancer survivors. Breast Cancer Research and Treatment, 196(3), 623–633. https://doi.org/10.1007/s10549-022-06752-8
French, E.L., Kader, L., Young, E.E., & Fontes, J.D. (2023). Physician perception of the importance of medical genetics and genomics in medical education and clinical practice. Medical Education Online, 28(1), 2143920. https://doi.org/10.1080/10872981.2022.2143920
Gubar, S. (2018, September 20). Raising awareness of BRCA mutations. The New York Times. https://www.nytimes.com/2018/09/20/well/live/raising-awareness-of-brca-…
Jerome-D’Emilia, B., & Begun, J.W. (2005). Diffusion of breast conserving surgery in medical communities. Social Science and Medicine, 60(1), 143–151. https://doi.org/10.1016/j.socscimed.2004.04.022
Josfeld, L., Keinki, C., Pammer, C., Zomorodbakhsch, B., & Hübner, J. (2021). Cancer patients’ perspective on shared decision-making and decision aids in oncology. Journal of Cancer Research and Clinical Oncology, 147(6), 1725–1732. https://doi.org/10.1007/s00432-021-03579-6
Kaphingst, K.A., Ivanovich, J., Biesecker, B.B., Dresser, R., Seo, J., Dressler, L.G., . . . Goodman, M.S. (2016). Preferences for return of incidental findings from genome sequencing among women diagnosed with breast cancer at a young age. Clinical Genetics, 89(3), 378–384. https://doi.org/10.1111/cge.12597
McCall, M.K., Ibikunle, S., Murphy, Y., Hunter, K., & Rosenzweig, M.Q. (2021). Knowledge and attitudes about genetic testing among Black and White women with breast cancer. Journal of Racial and Ethnic Health Disparities, 8(5), 1208–1216. https://doi.org/10.1007/s40615-020-00878-5
National Comprehensive Cancer Network. (2024). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Breast cancer [v.1.2024]. https://www.nccn.org
O’Neill, S.C., Vadaparampil, S.T., Street, R.L., Jr., Moore, T.F., Isaacs, C., Han, H.S., . . . Eggly, S. (2021). Characterizing patient–oncologist communication in genomic tumor testing: The 21-gene recurrence score as an exemplar. Patient Education and Counseling, 104(2), 250–256. https://doi.org/10.1016/j.pec.2020.08.037
Ozdemir, S., & Finkelstein, E.A. (2018). Cognitive bias: The downside of shared decision making. JCO Clinical Cancer Informatics, 2, 1–10. https://doi.org/10.1200/cci.18.00011
Pinilla, K., Drewett, L.M., Lucey, R., & Abraham, J.E. (2022). Precision breast cancer medicine: Early stage triple negative breast cancer—A review of molecular characterisation, therapeutic targets and future trends. Frontiers in Oncology, 12, 866889.
Polit, D.F., & Beck, C.T. (2018). Essentials of nursing research: Appraising evidence for nursing practice (9th ed.). Lippincott Williams and Wilkins.
Schaibley, V.M., Ramos, I.N., Woosley, R.L., Curry, S., Hays, S., & Ramos, K.S. (2022). Limited genomics training among physicians remains a barrier to genomics-based implementation of precision medicine. Frontiers in Medicine, 9, 757212.
Schmidlen, T.J., Wawak, L., Kasper, R., García-España, J.F., Christman, M.F., & Gordon, E.S. (2014). Personalized genomic results: Analysis of informational needs. Journal of Genetic Counseling, 23(4), 578–587. https://doi.org/10.1007/s10897-014-9693-8
Seo, J., Ivanovich, J., Goodman, M.S., Biesecker, B.B., & Kaphingst, K.A. (2017). Information topics of greatest interest for return of genome sequencing results among women diagnosed with breast cancer at a young age. Journal of Genetic Counseling, 26(3), 511–521. https://doi.org/10.1007/s10897-016-0006-2
Shickh, S., Leventakos, K., Lewis, M.A., Bombard, Y., & Montori, V.M. (2023). Shared decision making in the care of patients with cancer. American Society of Clinical Oncology Educational Book, 43, e389516. https://doi.org/10.1200/edbk_389516
Singh, B.P., Britton, S.L., Prins, P., Yin, C., Lankford, M.L., Willey, J.P., . . . Marshall, J. (2019). Molecular profiling (MP) for malignancies: Knowledge gaps and variable practice patterns among United States oncologists (Onc). Journal of Clinical Oncology, 37(Suppl. 15), 10510. https://doi.org/10.1200/JCO.2019.37.15_suppl.10510
Sparano, J.A., Gray, R.J., Ravdin, P.M., Makower, D.F., Pritchard, K.I., Albain, K.S., . . . Sledge, G.W., Jr. (2019). Clinical and genomic risk to guide the use of adjuvant therapy for breast cancer. New England Journal of Medicine, 380(25), 2395–2405. https://doi.org/10.1056/nejmoa1904819
Stallings, S.C., Richmond, J., Canedo, J.R., Beard, K., Bonnet, K., Schlundt, D.G., . . . Aldrich, M.C. (2023). Assessing patient-level knowledge of precision medicine in a community health center setting. Journal of Community Genetics, 14(2), 197–210. https://doi.org/10.1007/s12687-023-00632-4
Toland, A.E., Forman, A., Couch, F.J., Culver, J.O., Eccles, D.M., Foulkes, W.D., . . . Brody, L.C. (2018). Clinical testing of BRCA1 and BRCA2: A worldwide snapshot of technological practices. NPJ Genomic Medicine, 3, 7.
Tsimberidou, A.M., Fountzilas, E., Nikanjam, M., & Kurzrock, R. (2020). Review of precision cancer medicine: Evolution of the treatment paradigm. Cancer Treatment Reviews, 86, 102019. https://doi.org/10.1016/j.ctrv.2020.102019
Wuest, J. (2012). Grounded theory: The method. In P.L. Munhall (Ed.), Nursing Research: A Qualitative Perspective (5th ed., pp. 225–256). Jones and Bartlett Learning.




