Genetic Influence on Chemotherapy-Induced Nausea and Vomiting: A Narrative Review
Chemotherapy-induced nausea and vomiting (CINV) is a phenomenon common to patients being treated for a solid or hematologic malignancy. This adverse effect to cancer treatment persists in about half of all patients receiving highly emetogenic treatment, despite prophylaxis with serotonin (5-hydroxytryptamine-3 [5-HT3]) antagonists, steroids, and additional agents. Two broad categories increase risk for CINV: the emetogenic potential of chemotherapeutic drugs and patient-specific risk factors, such as younger age, female gender, low or no alcohol intake, and history of motion sickness or pregnancy-induced nausea. Despite these predictors for CINV, guidelines for prophylaxis continue to be based solely on the emetogenicity of agents administered. New strategies for CINV are unlikely until additional data emerge.
Jump to a section
Chemotherapy-induced nausea and vomiting (CINV) is a phenomenon common to patients being treated for a solid or hematologic malignancy. This adverse effect to cancer treatment persists in about half of all patients receiving highly emetogenic treatment (He et al., 2014; Zoto et al., 2015), despite prophylaxis with serotonin (5-hydroxytryptamine-3 [5-HT3]) antagonists, steroids, and additional agents. Two broad categories increase risk for CINV: the emetogenic potential of chemotherapeutic drugs (Hesketh et al., 1997) and patient-specific risk factors, such as younger age (Roscoe et al., 2010), female gender (Hesketh et al., 2006), low or no alcohol intake (Warr, Street, & Carides, 2011), and history of motion sickness or pregnancy-induced nausea (Pirri et al., 2011). Despite these predictors for CINV, guidelines for prophylaxis continue to be based solely on the emetogenicity of agents administered. New strategies for CINV are unlikely until additional data emerge.
Pharmacogenomics may or may not yield such data. New research into serotonin antagonists and how these drugs work differently in individuals with varying genetic makeup is affecting the knowledge of patient-specific CINV risk factors. Single nucleotide polymorphisms (SNPs) are DNA base substitutions that may affect protein function in the serotonin pathway, the neurologic pathway affected by chemotherapy in the peripheral nervous system in the gut and in the central nervous system (Bayo et al., 2012). This research has generated early knowledge with regard to SNPs that influence serotonin binding, drug metabolism, and drug transport proteins. The purpose of this review is to synthesize the current literature regarding genetic influence on CINV (see Table 1) and to explore the implications this has for nursing practice and research.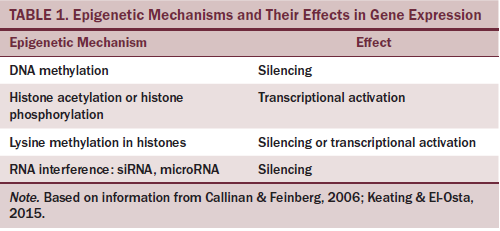
Serotonin Receptor Polymorphisms
The neurotransmitter serotonin binds to its associated receptor in the postsynapse of the peripheral and central nervous systems (Bayo et al., 2012). This receptor is made of five protein subunits, 5-HT3A-E. Different combinations of protein subunits bind together to form a pentamer (Niesler et al., 2007). In theory, polymorphisms in any of the genes responsible for receptor proteins could affect that protein’s function. In such a case, the pentameric serotonin receptor may become less responsive to serotonin antagonists, placing patients at higher risk for CINV.
From the sole study evaluating 5-HT3A receptor proteins, 21 polymorphisms were identified (Kaiser et al., 2004). However, none of the altered proteins created any statistically significant effect on CINV. Findings from the four studies looking at 5-HT3B were conflicting. One study found 13 polymorphisms in the 5-HT3B gene (Tremblay et al., 2003) but only one deletion variant that may have influenced CINV, and this variant did not reach significance. This finding was duplicated in a second study (Ward, Kotasek, & McKinnon, 2008), but it was not supported in two other 5-HT3B studies (Fasching et al., 2008; Perwitasari et al., 2011). The two studies noting a trend with the deletion variant had German samples, whereas the studies not finding that variant had Indonesian (Perwitasari et al., 2011) and Australian (Fasching et al., 2008) populations. This is noteworthy because some SNPs have been found more frequently in specific ethnicities.
The two studies that evaluated 5-HT3C receptor proteins also varied in their findings. Fasching et al. (2008) found a single variant associated with a 50% risk for CINV in the first 24 hours after treatment, compared with risks of 19% and 22% for the other two 5-HT3C variants examined. However, this finding was not reproduced in a second study (Ward et al., 2008). A single study, to date, has evaluated the 5-HT3D receptor gene (Hammer et al., 2010). A single SNP was found to correlate with higher risk for CINV. However, this finding failed to reach statistical significance.
Studies into serotonin receptor polymorphisms have yielded conflicting results. No strong evidence exists to assimilate into clinical nursing practice. This early research requires more diverse chemotherapy regimens, population diversity, and randomization to generate data influential to clinical practice.
Cytochrome P450 Polymorphisms
The effects of the cytochrome P450 family of enzymes on drug metabolism are well known. CINV research has investigated how polymorphisms in two enzymes, CYP2D6 and CYP3A4, influence the rate of serotonin antagonist metabolism in ways not previously understood. Rate of metabolism has been categorized into four groups: poor metabolizers, intermediate metabolizers, efficient metabolizers, and ultrarapid metabolizers (Sachse, Brockmöller, Bauer, & Roots, 1997). Theoretically, a patient with a high rate of drug metabolism may be underdosed for CINV, and a patient with a slow rate of metabolism may be using excess medication when the therapeutic ceiling has already been met.
Two studies have evaluated CYP2D6 and CINV (Kaiser et al., 2002; Perwitasari et al., 2011). Both studies demonstrated a higher rate of CINV for patients with SNPs associated with faster drug metabolism. Only Kaiser et al.’s (2002) study reached statistical significance. The difference may be ethnic. Kaiser et al.’s (2002) Caucasian sample (N = 270) had 8% (n = 21) poor metabolizers and 2% (n = 5) ultrarapid metabolizers, whereas Perwitasari et al.’s (2011) Indonesian sample (N = 202) contained only intermediate and effective metabolizers.
One study into CINV and serotonin antagonist metabolism sampled 158 Malaysian patients with breast cancer (Hassan & Yusoff, 2011). The sample was stratified by ethnic origin into individuals of Chinese, Malaysian, or Indian descent. The results suggested a statistically significant higher risk for CINV among those of Chinese descent. This difference was attributed to earlier studies suggesting higher enzymatic activity for CYP3A4 in Chinese patients with breast cancer (Huang et al., 2003) and lower CYP3A4 enzymatic activity in individuals of Indian descent (Rais, Chawla, & Kohli, 2006).
These early studies into CINV and serotonin antagonist metabolism have not yet produced results translatable to clinical practice. However, these early data are compelling; larger studies will help to establish this area’s potential relevance to nursing practice.
Transport Protein Polymorphisms
Transport proteins play a protective role for cells, influencing how much of a drug enters a target cell and removing excess drug once inside (Jonker, Wagenaar, Van Eijl, & Schinkel, 2003; Sakaeda, Nakamura, & Okumura, 2002). Two transport proteins, adenosine triphosphate-binding cassette subfamily B member 1 (ABCB1) and organic cation transporter 1 (OCT1), have been evaluated for polymorphisms that may affect serotonin antagonist availability and increase CINV risk.
Four studies have examined ABCB1 polymorphisms for influence on CINV (Babaoglu et al., 2005; He et al., 2014; Perwitasari et al., 2011; Zoto et al., 2015). Three studies (Babaoglu et al., 2005; He et al., 2014; Zoto et al., 2015) have found an association between the ABCB1 3435TT genotype and better control of CINV; however, the results of He et al. (2014) were not statistically significant. Perwitasari et al. (2011) used haplotype rather than genotype analysis and found that one ABCB1 haplotype (CTG) had an increased risk for CINV but only in the delayed phase of CINV.
A single study has been published evaluating the effect of OCT1 on serotonin antagonist drugs (Tzvetkov et al., 2012). Patients with loss-of-function SNPs in OCT1 were found to have higher blood concentration of tropisetron (Navoban®) and less CINV. Ondansetron (Zofran®) levels were not affected.
To date, some findings in the protein transport literature have shown reproducibility. This is encouraging and should stimulate additional inquiry. Nurses should be aware that SNPs in transport proteins may explain some degree of CINV treatment failure.
Areas of Future Research
Neurokinin 1 (NK1) antagonists are another category of therapy for highly emetogenic chemotherapy (Hesketh, Aapro, Street, & Carides, 2010). These agents (e.g., aprepitant [Emend®], fosaprepitant [Emend IV®]) are used alongside serotonin antagonists and steroids as a triple-drug anti-CINV regimen. Patients receiving NK1 antagonists may also have genetic polymorphisms that affect the efficacy of these drugs. To date, NK1 antagonists have not been evaluated in this way.
A similar pharmacogenomic approach may be applicable to older anti-CINV agents. Diphenhydramine (Benadryl®), prochlorperazine (Compazine®), and metoclopramide (Reglan®) have largely been replaced by the serotonin antagonists, NK1 antagonists, and steroids. Within the percentage of patients that fail standard-of-care CINV prophylaxis, a subset for whom older agents are genetically optimal may exist. In this way, pharmacogenomic research may create new therapeutic options for these older pharmaceuticals.
A few of the studies reviewed attempted to correlate genotype with patient-specific risk factors for CINV (e.g., motion sickness history). However, no study was specifically designed for this, and no correlation was found. Despite this, patient-specific risk factors likely have a genetic basis and are in urgent need of dedicated inquiry.
Implications for Nursing
Although this stage of research into the genetics of CINV may seem to have limited value to nursing practice, this is not the case. Nursing’s role in assessing and intervening in CINV is complemented by this new knowledge in multiple ways.
Prophylaxis failure: Research into genetic polymorphisms that affect CINV reminds oncology nurses that this phenomenon remains a frequent area of clinical concern. Therefore, while genetic polymorphisms continue to be evaluated in the laboratory setting, nurses must continue to use all of the anti-CINV strategies available through current data. Knowing prior to the administration of chemotherapy which patient-specific risk factors for CINV a particular patient may possess is useful. In this way, nurses can better identify those patients who may need a more detailed strategy for breakthrough anti-CINV drug use, more specific diet recommendations, and more collaborative one-on-one time for future CINV management.
Family history: Oncology nurses are skilled at doing the most basic genetic assessment: the family history. Asking about CINV in other family members with cancer may be helpful. A patient may recall that a relative experienced CINV during his or her cancer treatment and may even know the efficacy of the medicines used. Expanding the genetic assessment that nursing already implements to include a family history of CINV would be a logical first step toward including the genetics of CINV into clinical practice.
Patient education: Patients experiencing CINV despite prophylaxis need supportive explanations with regard to why emetic control was unsuccessful. Awareness of possible polymorphisms gives nurses a potential tool for patient education and support. In addition, explaining to patients suffering from CINV that the cancer research community cares about them and is pursuing better treatment may offer hope.
Conclusion
As the genetic influence on CINV continues, the implications for nursing practice will grow. The day may come when CINV instruments are developed that quantify all CINV risk factors (including genetics) and give nurses a tool from which to recommend patient-specific anti-CINV strategies. This emerging knowledge regarding one of the most feared side effects of cancer treatment can only improve the art and the science of what nursing does every day.
References
Babaoglu, M.O., Bayar, B., Aynacioglu, A.S., Kerb, R., Abali, H., Celik, I., & Bozkurt, A. (2005). Association of the ABCB1 3435C>T polymorphism with antiemetic efficacy of 5-hydroxytryptamine type 3 antagonists. Clinical Pharmacology and Therapeutics, 78, 619–626. doi:10.1016/j.clpt.2005.08.015
Bayo, J., Fonseca, P.J., Hernando, S., Servitja, S., Calvo, A., Falagan, S., . . . Barnadas, A. (2012). Chemotherapy-induced nausea and vomiting: Pathophysiology and therapeutic principles. Clinical and Translational Oncology, 14, 413–422. doi:10.1007/s12094-012-0818-y
Fasching, P.A., Kollmannsberger, B., Strissel, P.L., Niesler, B., Engel, J., Kreis, H., . . . Strick, R. (2008). Polymorphisms in the novel serotonin receptor subunit gene HTR3C show different risks for acute chemotherapy-induced vomiting after anthracycline chemotherapy. Journal of Cancer Research and Clinical Oncology, 134, 1079–1086. doi:10.1007/s00432-008-0387-1
Hammer, C., Fasching, P.A., Loehberg, C.R., Rauh, C., Ekici, A.B., Jud, S.M., . . . Niesler, B. (2010). Polymorphism in HTR3D shows different risks for acute chemotherapy-induced vomiting after anthracycline chemotherapy. Pharmacogenomics, 11, 943–950. doi:10.2217/pgs.10.67
Hassan, B.A., & Yusoff, Z.B. (2011). Genetic polymorphisms in the three Malaysian races effect granisetron clinical antiemetic actions in breast cancer patients receiving chemotherapy. Asian Pacific Journal of Cancer Prevention, 12, 185–191. doi:10.1007/bf01208844
He, H., Yin, J.Y., Xu, Y.J., Li, X., Zhang, Y., Liu, Z.G., . . . Liu, Z.Q. (2014). Association of ABCB1 polymorphisms with the efficacy of ondansetron in chemotherapy-induced nausea and vomiting. Clinical Therapeutics, 36, 1242–1252. doi:10.1016/j.clinthera.2014.06.016
Hesketh, P.J., Aapro, M., Street, J.C., & Carides, A.D. (2010). Evaluation of risk factors predictive of nausea and vomiting with current standard-of-care antiemetic treatment: Analysis of two phase III trials of aprepitant in patients receiving cisplatin-based chemotherapy. Supportive Care in Cancer, 18, 1171–1177. doi:10.1007/s00520-009-0737-9
Hesketh, P.J., Grunberg, S.M., Herrstedt, J., de Wit, R., Gralla, R.J., Carides, A.D., . . . Horgan, K.J. (2006). Combined data from two phase III trials of the NK1 antagonist aprepitant plus a 5HT3 antagonist and a corticosteroid for prevention of chemotherapy-induced nausea and vomiting: Effect of gender on treatment response. Supportive Care in Cancer, 14, 354–360. doi:10.1007/s00520-005-0914-4
Hesketh, P.J., Kris, M.G., Grunberg, S.M., Beck, T., Hainsworth, J.D., Harker, G., . . . Lindley, C.M. (1997). Proposal for classifying the acute emetogenicity of cancer chemotherapy. Journal of Clinical Oncology, 15, 103–109.
Huang, P., Zhu, B., Wang, L.S., Ouyang, D.S., Huang, S.L., Chen, X.P., & Zhou, H.H. (2003). Relationship between CYP3A activity and breast cancer susceptibility in Chinese Han women. European Journal of Clinical Pharmacology, 59, 471–476. doi:10.1007/s00228-003-0649-4
Jonker, J.W., Wagenaar, E., Van Eijl, S., & Schinkel, A.H. (2003). Deficiency in the organic cation transporters 1 and 2 (Oct1/Oct2 [Slc22a1/Slc22a2]) in mice abolishes renal secretion of organic cations. Molecular and Cellular Biology, 23, 7902–7908. doi:10.1128/mcb.23.21.7902-7908.2003
Kaiser, R., Sezer, O., Papies, A., Bauer, S., Schelenz, C., Tremblay, P.B., . . . Brockmöller, J. (2002). Patient-tailored antiemetic treatment with 5-hydroxytryptamine type 3 receptor antagonists according to cytochrome P-450 2D6 genotypes. Journal of Clinical Oncology, 20, 2805–2811. doi:10.1200/jco.2002.09.064
Kaiser, R., Tremblay, P.B., Sezer, O., Possinger, K., Roots, I., & Brockmöller, J. (2004). Investigation of the association between 5-HT3A receptor gene polymorphisms and efficiency of antiemetic treatment with 5-HT3 receptor antagonists. Pharmacogenetics, 14, 271–278. doi:10.1097/00008571-200405000-00001
Niesler, B., Walstab, J., Combrink, S., Möller, D., Kapeller, J., Rietdorf, J., . . . Brüss, M. (2007). Characterization of the novel human serotonin receptor subunits 5-HT3C, 5-HT3D, and 5-HT3E. Molecular Pharmacology, 72, 8–17. doi:10.1124/mol.106.032144
Perwitasari, D.A., Wessels, J.A., van der Straaten, R.J., Baak-Pablo, R.F., Mustofa, M., Hakimi, M., . . . Guchelaar, H.J. (2011). Association of ABCB1, 5-HT3B receptor and CYP2D6 genetic polymorphisms with ondansetron and metoclopramide antiemetic response in Indonesian cancer patients treated with highly emetogenic chemotherapy. Japanese Journal of Clinical Oncology, 41, 1168–1176. doi:10.1093/jjco/hyr117
Pirri, C., Katris, P., Trotter, J., Bayliss, E., Bennett, R., & Drummond, P. (2011). Risk factors at pretreatment predicting treatment-induced nausea and vomiting in Australian cancer patients: A prospective, longitudinal, observational study. Supportive Care in Cancer, 19, 1549–1563. doi:10.1007/s00520-010-0982-y
Rais, N., Chawla, Y.K., & Kohli, K.K. (2006). CYP3A phenotypes and genotypes in North Indians. European Journal of Clinical Pharmacology, 62, 417–422. doi:10.1007/s00228-006-0105-3
Roscoe, J.A., Morrow, G.R., Colagiuri, B., Heckler, C.E., Pudlo, B.D., Colman, L., . . . Jacobs, A. (2010). Insight in the prediction of chemotherapy-induced nausea. Supportive Care in Cancer, 18, 869–876. doi:10.1007/s00520-009-0723-2
Sachse, C., Brockmöller, J., Bauer, S., & Roots, I. (1997). Cytochrome P450 2D6 variants in a Caucasian population: Allele frequencies and phenotypic consequences. American Journal of Human Genetics, 60, 284–295.
Sakaeda, T., Nakamura, T., & Okumura, K. (2002). MDR1 genotype-related pharmacokinetics and pharmacodynamics. Biological and Pharmaceutical Bulletin, 25, 1391–1400. doi:10.1248/bpb.25.1391
Tremblay, P.B., Kaiser, R., Sezer, O., Rosler, N., Schelenz, C., Possinger, K., . . . Brockmoller, J. (2003). Variations in the 5-hydroxytryptamine type 3B receptor gene as predictors of the efficacy of antiemetic treatment in cancer patients. Journal of Clinical Oncology, 21, 2147–2155. doi:10.1200/jco.2003.05.164
Tzvetkov, M.V., Saadatmand, A.R., Bokelmann, K., Meineke, I., Kaiser, R., & Brockmöller, J. (2012). Effects of OCT1 polymorphisms on the cellular uptake, plasma concentrations and efficacy of the 5-HT3 antagonists tropisetron and ondansetron. Pharmacogenomics Journal, 12, 22–29. doi:10.1038/tpj.2010.75
Ward, M.B., Kotasek, D., & McKinnon, R.A. (2008). Investigation of HRT3C mutations for association with 5HT(3) receptor antagonist anti-emetic efficacy. Pharmacogenomics, 9, 1027–1033. doi:10.2217/14622416.9.8.1027
Warr, D.G., Street, J.C., & Carides, A.D. (2011). Evaluation of risk factors predictive of nausea and vomiting with current standard-of-care antiemetic treatment: Analysis of phase 3 trial of aprepitant in patients receiving adriamycin-cyclophosphamide-based chemotherapy. Supportive Care in Cancer, 19, 807–813. doi:10.1007/s00520-010-0899-5
Zoto, T., Kilickap, S., Yasar, U., Celik, I., Bozkurt, A., & Babaoglu, M.O. (2015). Improved anti-emetic efficacy of 5-HT3 receptor antagonists in cancer patients with genetic polymorphisms of ABCB1 (MDR1) drug transporter. Basic and Clinical Pharmacology and Toxicology, 4, 354–360. doi:10.1111/bcpt.12334
About the Author(s)
Kiernan is a lecturer in the Faculty of Nursing at the University of Windsor in Ontario, Canada. No financial relationships to disclose. Mention of specific products do not indicate or imply endorsement by the Oncology Nursing Forum or the Oncology Nursing Society. Kiernan can be reached at jasonk@uwindsor.ca, with copy to editor at ONFEditor@ons.org.

