eHealth Literacy and Partner Involvement in Treatment Decision Making for Men With Newly Diagnosed Localized Prostate Cancer
Purpose/Objectives: To examine how the eHealth literacy of partners of patients with newly diagnosed prostate cancer affects their involvement in decision making, and to identify the factors that influence their eHealth literacy.
Design: Cross-sectional exploratory study.
Setting: North Carolina.
Sample: 142 partners of men with newly diagnosed localized prostate cancer.
Methods: A telephone survey and descriptive and multiple linear regression analyses were used.
Main Research Variables: The partners’ eHealth literacy, involvement in treatment decision making, and demographics, and the health statuses of the patients and their partners.
Findings: Higher levels of eHealth literacy among partners were significantly associated with their involvement in getting a second opinion, their awareness of treatment options, and the size of the social network they relied on for additional information and support for treatment decision making for prostate cancer. The factor influencing eHealth literacy was the partners’ access to the Internet for personal use, which explained some of the variance in eHealth literacy.
Conclusions: This study described how partners’ eHealth literacy influenced their involvement in treatment decision making for prostate cancer and highlighted the influencing factors (i.e., partners’ access to the Internet for personal use).
Implications for Nursing: When helping men with prostate cancer and their partners with treatment decision making, nurses need to assess eHealth literacy levels to determine whether nonelectronically based education materials are needed and to provide clear instructions on how to use eHealth resources.
Jump to a section
Aside from skin cancer, prostate cancer is the most frequently diagnosed cancer in men in the United States, with more than 161,360 new cases diagnosed in 2016 (American Cancer Society [ACS], 2017). About 92% of the patients will have localized or regional disease (Siegel et al., 2012). For men with newly diagnosed localized prostate cancer, no single treatment strategy is clearly superior in terms of mortality. Serious tradeoffs exist in different treatment-related side effects (National Cancer Institute [NCI], 2016a) and their negative impact on men’s quality of life (Skolarus et al., 2014). Partners of men in sexual relationships have reported experiencing higher levels of distress and worse quality of life than the patients themselves (Song et al., 2010). Along with cancer diagnoses and treatment decision making, partners face potential role transitions, interruptions to daily life, and strains on their marital and sexual relationships (Galbraith, Fink, & Wilkins, 2011; Hanly, Mireskandari, & Juraskova, 2014; O’Brien et al., 2011; Wittmann et al., 2014; Woottenet al., 2014). Partners’ emotional distress related to prostate cancer and their concerns about the patients’ distress can influence their mental health, quality of life, and ability to cope (Chambers et al., 2013; Street et al., 2010), as well as the patients’ quality of life (Hagedoorn, Sanderman, Bolks, Tuinstra, & Coyne, 2008; Lafaye et al., 2014). Research has indicated that the quality of life of patients and their partners are significantly related (Song et al., 2010).
Given the negative, diffuse impact of the side effects of treatments for prostate cancer on men and their partners and the overwhelming amount of information about treatment options, a solid understanding of treatment options, risks, and benefits is necessary for informed decision making. For men with prostate cancer and their partners, sufficient accurate information and active communication with healthcare providers are vital to achieving an informed treatment decision and ensuring that they will experience the best quality of life after treatment (National Comprehensive Cancer Network, 2014).
More than 70% of adults and their family caregivers in the United States reported receiving information and support from physicians or other healthcare professionals and family and friends during serious health episodes (Fox & Duggan, 2013; Pew Research Center, 2012). On the other hand, partners of men with prostate cancer often receive limited or no information from healthcare providers (Ezer, Chachamovich, & Chachamovich, 2011; Galbraith et al., 2011), despite that partners of men with localized prostate cancer are usually their information gatherers, primary caregivers, and major sources of emotional and practical support (Ervik, Nordøy, & Asplund, 2013). The responsibilities and care tasks associated with the cancer survivorship trajectory from treatment decision making to post-treatment self-management and beyond can exceed partner caregivers’ knowledge and skills (Given, Given, & Sherwood, 2012), which may motivate them to seek information about diagnosis, treatment options, and related issues from other mediums, including eHealth sources (Fox, Duggan, & Purcell, 2013). Illness-related information and numerous health management tools have rapidly expanded and are now available to the public on the Internet (Zulman, Kirch, Zheng, & An, 2011). Supportive eHealth programs are used to educate people of different ages, genders, literacy levels, and disease stages (Rini et al., 2015; Schover et al., 2011; Song et al., 2015; Thorndike et al., 2013; Zulman, Kirch, et al., 2011; Zulman, Schafenacker, et al., 2011).
To maximize the benefits of eHealth technologies and strategies, nurses should assess eHealth literacy levels (i.e., the ability of potential users to seek, find, understand, and appraise health information from electronic sources and apply their knowledge to address or solve health issues) (Norman & Skinner, 2006). Assessing the eHealth literacy level of caregiver partners of men with prostate cancer is particularly important, because partners are actively involved in treatment decision making, including information gathering (Symes et al., 2015). However, research to date has ignored the eHealth literacy of family caregivers, its relationship to partners’ caregiving activities, and its influencing factors, which are the focus of the current study.
Theoretical Framework
This study is guided by B.F. Skinner’s Operant Conditioning theory (McLeod, 2015), which suggests that intentional actions (i.e., operant actions) affect the environment (and a variety of behaviors), and that certain processes make certain operant behaviors more or less likely to occur. Skinner identified three types of operant actions and their associated behaviors: neutral operants neither increase nor decrease the probability of a behavior being operated, reinforcers (either positive or negative) increase the probability of a behavior being operated, and punishers decrease the likelihood of a behavior being operated (Skinner, 1938).
The authors of the current study aimed to examine the level of eHealth literacy of partners of men with newly diagnosed localized prostate cancer. The partners’ eHealth literacy was operationalized as the proxy of their use of technology to find information from electronic sources and their application of that knowledge to address or solve health problems. Based on Operant Conditioning, the authors hypothesized that a higher level of eHealth literacy among partners would be a positive reinforcer that would increase their involvement in treatment decision making after a prostate cancer diagnosis. The authors aimed to test this hypothesis and identify the factors that influenced the eHealth literacy of partners of men with prostate cancer.
Methods
This was a cross-sectional exploratory study. Patient–partner couples were recruited from the North Carolina Prostate Cancer Comparative Effectiveness and Survivorship Study (NC ProCESS), a population-based cohort study (Chen et al., 2015). NC ProCESS included a cohort of men with newly diagnosed localized prostate cancer enrolled by the Rapid Case Ascertainment (RCA) of the North Carolina Central Cancer Registry. The RCA uses an accelerated process to capture new cases of prostate cancer from across North Carolina within four weeks of diagnosis, allowing a prompt collection of baseline data and recruitment of diverse participants with different socioeconomic statuses, races and ethnicities, rural/urban residences, and treatment locations (community versus cancer centers).
Partner caregivers were eligible regardless of their race/ethnicity or gender if they (a) were aged 21 years or older, (b) were identified as the partner/spouse of a man diagnosed with localized prostate cancer within the past three months, and (c) understood and spoke English. The authors excluded partners who had been diagnosed with cancer (except early-stage skin cancer) within the previous year or were receiving active treatment for cancer, because their information seeking and coping (the focus of the main study) likely would not have focused primarily on the patients’ prostate cancer diagnosis and management.
Procedure
The study protocol and recruitment processes were published previously (Chen et al., 2015; Symes et al., 2015). Institutional review board approval was obtained from the University of North Carolina at Chapel Hill. At the end of their three-month telephone survey (after most patients had made decisions about their treatment), patient participants in the NC ProCESS were asked whether they had a partner and if they would like their partners to be contacted for participation in the study, which was named the Care for Family Project.
Of the 488 patients the authors approached, 389 had a partner and gave the authors permission to contact her. Participants were not excluded based on gender identity or sexual orientation, but no same-sexcouples participated in the study. A research assistant mailed the partners a brochure and a written consent form that provided an explicit explanation of the Care for Family Project. Two weeks after mailing the study information, a research assistant contacted 316 partners via phone, provided them with further explanation, answered questions, and ensured them that the study materials were strictly confidential and would not affect patient care. After screening for the eligibility of partners who agreed to participate, the research assistant obtained informed consent and surveyed 281 partners by phone, with a response rate of 58% and a recruitment rate of 89% (Symes et al., 2015). Each phone interview lasted about 30–60 minutes. All interviews were completed and recorded within one to three months of the initiation of the patients’ prostate cancer treatment. 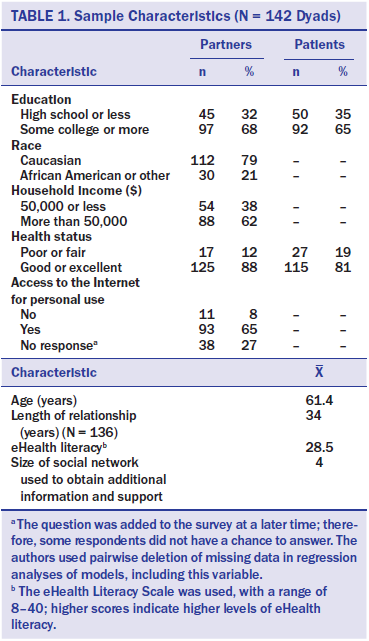
Participants received a $30 gift certificate by mail upon completion of the survey. All research assistants had prior phone survey experience and received 64 hours of training on patient eligibility criteria, informed consent, and phone interview techniques. The authors also held weekly project meetings with all research staff to discuss the interviews. Two researchers who did not call participants randomly checked 50% of the recorded interviews to ensure survey consistency. Discrepancies between recorded interviews and the research datasets were discussed at weekly project meetings, data entry errors were corrected if indicated, and research assistants were informed about quality improvement for future surveys.
Measures
eHealth literacy was measured using the eight-itemeHealth Literacy Scale (eHEALS) (Norman & Skinner, 2006). The five-point Likert-type responses ranged from 1 (strongly disagree) to 5 (strongly agree), with higher scores indicating higher levels of eHealth literacy. The Cronbach alpha of eHEALS was 0.94. Activities that partners engaged in during treatment decision making (Symes et al., 2015) were measured by eight items assessed as yes (presence of activity) or no (absence of activity). The activities were gathering information, visiting doctor(s) with the patient, participating in conversations with the patient’s doctor, seeking a second opinion, discussing treatment options with the patient, providing emotional support to the patient, being aware of treatment options, and being aware of treatment risks and side effects. The size of the social support network that partners used to obtain additional information and support was assessed using a question from an epidemiology study of men with prostate cancer (Schroeder et al., 2006). The score of the size of the social network ranged from 0–14 and included partners, parents and in-laws, neighbors, friends, church members, coworkers, therapists, and children. 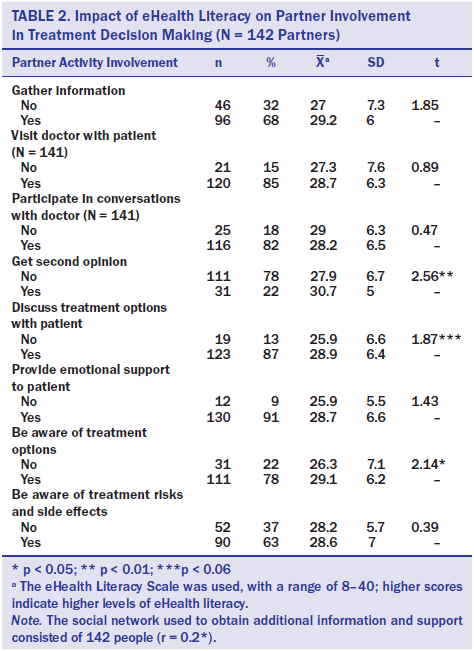
Selected based on literature review (Choi & Dinitto, 2013; Chung & Nahm, 2015; Kontos, Blake, Chou, & Prestin, 2014; Norman & Skinner, 2006; Park, Moon, & Baeg, 2014; Tennant et al., 2015; Xie, 2011), potential influencing factors for eHealth literacy included patients’ and partners’ demographics (e.g., age, education, race, household income), health status (reported by the partners and categorized into poor or fair versus good or excellent), and partners’ access to the Internet for personal use (yes or no).
Data Analysis
The authors analyzed the data using SPSS®, version 22.0. Demographic data and the variables of interest were summarized using descriptive statistics. The bivariate relationships between eHealth literacy and the categorical characteristic variables were analyzed using t tests or one-way analysis of variance, whereas the bivariate relationships between eHealth literacy and continuous variables were examined using the Pearson product-moment correlation test. The relationships between eHealth literacy and potential influencing factors were examined using multiple regression analysis. First, the authors fitted the full model where partner eHealth literacy was predicted by all significant variables in bivariate analyses. Then they obtained a parsimonious adjusted model using backward elimination, sequentially eliminating any variables that were not significant at an alpha of 0.05. Pairwise, deletion of missing data was used in regression analyses.
Results
In this study, 142 partners completed the phone interviews related to eHealth literacy (see Table 1). The average partner was aged 61 years, and the average duration of partner–patient relationships was 34 years. About 79% of the respondents were Caucasian. Two-thirds had at least some college or higher levels of education. About 62% reported household incomes of more than $50,000 per year. Only 12% of partners reported poor or fair overall health. Eight percent of the respondents had no access to the Internet for personal use, and the mean eHealth literacy score was 28.5, out of a possible range of 8–40, with higher scores indicating higher levels of eHealth literacy. The social network scale ranged from 1–9 points, and the average size of partners’ network for additional information and support was 4.
Partner eHealth Literacy and Treatment Decision Making
As displayed in Table 2, partners’ eHealth literacy was significantly associated with their involvement in seeking a second opinion and their awareness of treatment options. Partners who helped patients get second opinions reported significantly higher levels of eHealth literacy, and partners who were aware of treatment options reported higher levels of eHealth literacy. Partners’ levels of eHealth literacy were also positively correlated with the size of the social network they used to obtain additional information and support for treatment decision making for prostate cancer (r = 0.2, p < 0.05).
Factors Influencing eHealth Literacy
The results of the bivariate analysis are shown in Table 3. Partner age, education levels, race, household income, and access to the Internet for personal use, and patients’ and partners’ health statuses all were significantly associated with partners’ eHealth literacy levels.
The results of the full and adjusted models of eHealth literacy and the influencing factors are displayed in Table 4. The full model included all variables that were significant in bivariate analyses. eHealth literacy was significantly related to partners’ access to the Internet for personal use. These variables of interest (i.e., partner age, education level, race, income, access to the Internet for personal use, and patient and partner health statuses) explained 30% of the variance in partners’ eHealth literacy. In the adjusted model, the significant relationships between partners’ eHealth literacy and their access to the Internet for personal use remained significant. The eHEALS scores of patients with access to the Internet for personal use were, on average, 10.6 points higher (p <0.001) than the scores of those without access. This variable alone explained 29% of the variance in eHealth literacy.
Discussion
The increasing availability of eHealth programs and online health information provides patients and their families with opportunities to improve their health education and knowledge and, ultimately, to promote health. However, effective use of these resources depends on individual eHealth literacy. The authors of the current study examined how eHealth literacy related to family caregiving (i.e., partner involvement in decision making for treatment of localized prostate cancer) and identified the influencing factors of eHealth literacy among partners of men with prostate cancer. The eHealth literacy level among partners of men with prostate cancer was lower than that of adolescent and young adult populations (Norman & Skinner, 2006), similar to that of older adult Internet users in the United States (Chung & Nahm, 2015; Park et al., 2014), but higher than the literacy levels of the lung cancer survivor population, with a median age of 71 years (Milne et al., 2014). Guided by the Operant Conditioning theory, the authors found that higher eHealth literacy levels among partners were positively related to their engagement in seeking a second opinion, awareness of treatment options, and use of a large social network for gathering information and support for treatment decision making. 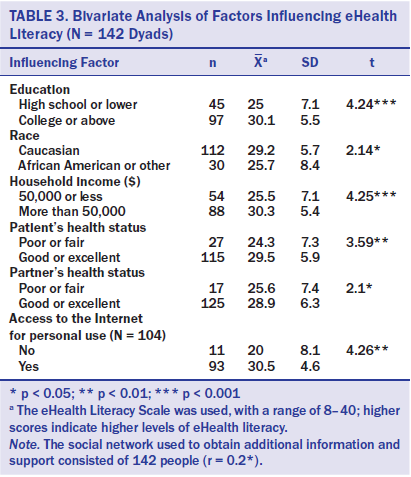
In addition, the authors found that the partners’ eHealth literacy was positively related to their access to the Internet for personal use but not related to their age, race, household income, health status, or the patients’ health status. A Pew Internet Research Center survey in 2013 revealed that only 56% of Americans older than 65 years were connected to and used the Internet, compared with 83% of those aged 50–64 years, and that 53% did not have high-speed broadband connections at home (Smith, 2014). Prostate cancer is most prevalent among men aged 65 years or older (National Cancer Institute, 2016b; Siegel et al., 2012). Considering the significant impact of partners’ personal Internet access on eHealth literacy, lack of connection to the Internet among older populations indicates less of an opportunity for patients and their partners to benefit from eHealth technologies and educational resources. Healthcare providers need to be mindful of these challenges when preparing health education strategies to mitigate the potential negative effects of low eHealth literacy on the health of older population.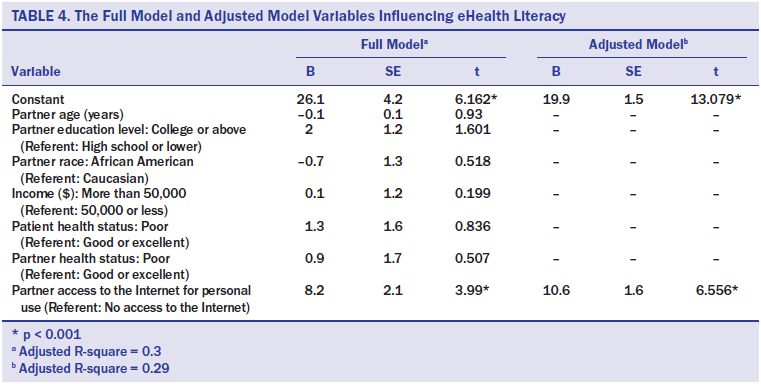
The most important finding of this study was that eHealth literacy was positively related to partners’ involvement in treatment decision making for patients with newly diagnosed localized prostate cancer, supporting the authors’ hypothesis. Given that partners play an integral role in gathering information and providing care and support to patients (Ervik et al., 2013) and that patients rely on family caregivers to gather information from different sources to make treatment decisions (Given et al., 2012; Turner et al., 2011), the authors’ research findings indicate that partners with low eHealth literacy may be disadvantaged because they are not aware of all treatment options. In addition, they are less likely to obtain information and support from online resources from other sources, such as from other doctors when seeking second opinions and from their social networks of relatives and friends. The finding that patients’ eHealth literacy levels were related to their degree of seeking information before medical appointments was consistent with the findings of other studies (Hu, Bell, Kravitz, & Orrange, 2012) and suggests that clinicians need to pay close attention to the eHealth literacy levels of men with newly diagnosed localized prostate cancer and their partners. When helping patients and partners with low eHealth literacy make treatment decisions, clinicians should provide not only information about all treatment options but alternative reader-friendly and nonelectronically based sources of information and support (e.g., books, videos), or offer clear instruction on how to access and use eHealth resources.
Although the findings were partially consistent with that of previous research in which access to the Internet and education levels were related to eHealth literacy (Agree, King, Castro, Wiley, & Borzekowski, 2015; Chung & Nahm, 2015; Neter & Brainin, 2012; Norman & Skinner, 2006), the results should be interpreted with caution given the small sample. Adult Internet users in the United States with lower socioeconomic status and who were older aged were less likely to engage in eHealth programs or health information–seeking behaviors compared to their younger or wealthier counterparts (Agree et al., 2015; Kontos et al., 2014; Tennant et al., 2015). In addition, in one study (Jimbo et al., 2013), patients’ lack of Internet access and low computer literacy were identified as perceived barriers to using web-based decision aids for colorectal cancer screening.
The current study’s participants were recruited throughout all 100 counties in North Carolina using RCA. This resource allowed the authors to timely recruit a diverse population of participants that comprise similar proportions of Caucasian men with prostate cancer and minorities in North Carolina, who are often underrepresented in studies.
Limitations
This study focused on eHealth literacy and related issues among partners of men with prostate cancer. Future research is needed to examine whether partners’ eHealth literacy levels actually affect men’s treatment decision making. The authors assessed the eHealth literacy only of female partners of patients with localized prostate cancer, which made it impossible to examine gender differences in eHealth literacy among spousal caregivers. Future research is needed to differentiate the role effects (patient versus partner) from the gender effects in eHealth literacy and related issues.
The small sample size limited the generalizability of this study. With noted disparities across racial and social groups with cancer (ACS, 2015), future research is needed to examine eHealth literacy and related issues using a large sample of family caregivers with diverse sociodemographic backgrounds to identify the groups that bear disproportionate burdens in obtaining information and support. This endeavor will strengthen the implementation, uptake, and impact of eHealth programs and facilitate cancer care. Last, the eHEALS required respondents to self-reporttheir level of eHealth literacy and Internet use and access, which may have been affected by social desirability.
Implications for Nursing
The findings may imply that, despite the growing number of eHealth programs available in different settings and their potential health benefits for patients with cancer and their family caregivers, a large numberof older adults in the United States may not benefit from eHealth technology advancement because of a lack of access to the Internet for personal use, which is associated with low levels of eHealth literacy. Nurses play vital roles in providing information and resources and in educating patients and their families. They need to assess eHealth literacy among men with newly diagnosed localized prostate cancer and their partners to maximize the information support they receive during treatment decision making. To help men and their partners with low eHealth literacy make informed treatment decisions, nurses should provide clear instructions on how to use eHealth resources or provide educational information and materials that are not electronically based. Nurses should also encourage patients and their partners with low eHealth literacy to involve family members with high eHealth literacy in online information searching and the use of existing eHealth programs.
The findings suggest that clinical care and public health communication efforts attempting to eliminate the digital divide should acknowledge differential eHealth literacy challenges and employ comprehensive approaches to better address persistent information needs of patients and their family caregivers. Some possible solutions include developing credible, one-stop eHealth programs that require minimum Internet navigation skills so that partner caregivers with low eHealth literacy can get information, and offering support and/or skills training for patients and improve their own health. Providing access to the Internet (e.g., provide a tablet computer to access health information while waiting for an appointment or cancer treatment) and clear instruction on how to use eHealth information and resources could be alternative approaches for health services to removing the barriers to good eHealth literacy and to improving partners’ information-seeking options. Providingaccess to the Internet can also enable patients and partners to use online support groups, forums, and other programs for information and support and, therefore, enhance the size and strength of their existing social networks. Research has indicated that men with prostate cancer and their partners often use online forums and other sources to obtain and validate information prior to and after visiting their healthcare providers (Salonen, Ryhänen, & Leino-Kilpi, 2014). For some with low eHealth literacy, involving other family members (e.g., children, grandchildren) in online information searching or the use of existing eHealth programs may also be necessary and effective.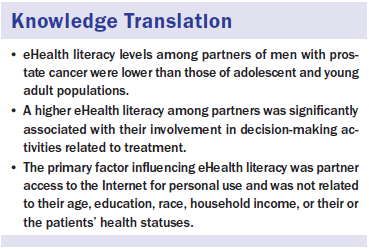
Conclusion
This study examined how eHealth literacy among partner caregivers relates to their involvement in treatment decision making for men with localized prostate cancer and identified the influencing factors of their eHealth literacy. Partners with higher eHealth literacy reported greater involvement in seeking second opinion(s), greater awareness of treatment options, and the use of larger social networks to obtainadditional information and support for treatmentdecision making. Partners’ eHealth literacy was positively related to their access to the Internet for personal use but was not related to their age, race, education, and household income, or the health status of patients and partners. These findings are highly relevant to the implementation and dissemination of eHealth cancer care programs among the aging population in the United States.
[[{"type":"media","view_mode":"media_original","fid":"30151","attributes":{"alt":"","class":"media-image","height":"479","typeof":"foaf:Image","width":"366"}}]]
The authors gratefully acknowledge the staff, advisory committees, and research participants in the NC ProCESS and the Care for Family Project for their important contributions.
About the Author(s)
Song is an assistant professor in the School of Nursing at the University of North Carolina at Chapel Hill; Tatum is an urban planner, climate scientist, and anthropologist at Universität Humburg in Germany; Greene is a clinical nurse I at Duke University Hospital in Durham, NC; and Chen is an associate professor in the Department of Radiation Oncology at the University of North Carolina at Chapel Hill. This research (Care for Family Project) was funded by the University Cancer Research Fund from the University of North Carolina Lineberger Comprehensive Cancer Center (principal investigator [PI]: Song) and grants (KL2TR001109 and UL1TR001111) from the National Institutes of Health/National Center for Advancing Translational Sciences through support from the North Carolina Translational and Clinical Science Institute (PIs: Runge, Buse, and Carey, awarded to Song). The North Carolina Prostate Cancer Comparative Effectiveness and Survivorship Study was funded by the Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services, as part of the DEcIDE program (HHSA290-2005-0040-ITO6, PI:Chen). Song, Tatum, and Chen contributed to the conceptualization, design, and manuscript preparation. Song provided statistical support and the analysis. All of the authors completed the data collection. Song can be reached at lsong@unc.edu, with copy to editor at ONFEditor@ons.org. Submitted April 2016. Accepted for publication June 2, 2016.

