Body-Related Shame and Guilt Predict Physical Activity in Breast Cancer Survivors Over Time
Purpose/Objectives: To test body-related shame and guilt as predictors of breast cancer survivors’ (BCS’) moderate to vigorous intensity physical activity (MVPA) during six months and to examine motivational regulations as mediators of this association.
Design: Prospective study.
Setting: Survivors were recruited through advertisements and oncologist referrals from medical clinics and hospitals in Montreal, Quebec, Canada.
Sample: 149 female BCS.
Methods: Self-reports of body-related shame and guilt, motivational regulations, and MVPA were measured among BCS at baseline. MVPA was assessed a second time six months later. Residual change scores were used.
Main Research Variables: Body-related shame and guilt; external, introjected, and autonomous (identified and intrinsic) motivational regulations; MVPA.
Findings: In the multiple mediation models, body-related shame was associated with low levels of MVPA, as well as external, introjected, and autonomous motivational regulations. Guilt was related to high levels of MVPA and introjected and autonomous motivational regulations. Indirect effects linked shame, guilt, and MVPA via autonomous motivation. Only body-related shame was a significant predictor of six-month changes in MVPA.
Conclusions: Based on these results, the specific emotions of shame and guilt contextualized to the body differentially predict BCS’ health motivations and behavior over time.
Implications for Nursing: Survivorship programs may benefit from integrating intervention strategies aimed at reducing body-related shame and helping women manage feelings of guilt to improve physical activity.
Jump to a section
Many women who survive breast cancer will experience subsequent challenges to their mental and physical health, such as fear of recurrence, emotional distress, reduced quality of life, concerns about physical appearance, pain, nausea, and decreased physical functioning (Ewertz & Jensen, 2011). Moderate to vigorous intensity physical activity (MVPA) has been identified as a nonpharmacologic therapy that can help prevent or relieve many of these disease- and treatment-related challenges (Demark-Wahnefried & Jones, 2008; Sabiston & Brunet, 2012). However, the majority of breast cancer survivors (BCS) are not sufficiently active at levels known to exert health benefits (Devoogdt et al., 2010; Sabiston & Brunet, 2012). Because being physically active is safe, feasible, and efficacious among BCS, increasing MVPA has been identified as a public health initiative.
Identifying factors related to participation in MVPA among BCS can help to inform the development of targeted and effective interventions aimed at enhancing optimal health and well-being. In the current study, self-objectification, objectified body consciousness, and self-determination theories are used as guiding frameworks to identify body-related shame, body-related guilt, and motivational consequences as modifiable factors associated with BCS’ MVPA over time.
Body-Related Shame and Guilt
Self-conscious emotions are evoked by self-reflection and self-evaluation (Tracy & Robins, 2004). They are founded in social relationships when people interact, appraise, and judge themselves and others. The specific emotion of body-related shame is defined as a negative feeling about oneself or global self-blame (e.g., “I am fat”) that individuals experience when they fail to meet internalized social standards in relation to the body (Sabiston & Castonguay, 2014; Tracy & Robins, 2004). Based on self-objectification theory and objectified body consciousness (Fredrickson & Roberts, 1997; McKinley & Hyde, 1996), women evaluate their body against a socially defined and often unattainable ideal physique and continually monitor themselves. Failure to meet these internalized standards and preoccupation with one’s appearance may result in the emotional consequence of body-related shame that can foster maladaptive health behaviors (e.g., low PA) (Castonguay, Pila, Wrosch, & Sabiston, 2015; Castonguay, Sabiston, Kowalski, & Wilson, 2016; Sabiston et al., 2010). In the case of breast cancer, survivorship is a critical period in which women may confront weight gain, alterations to body shape, scars, hair loss, removal or disfigurement of the breast(s), muscle loss and/or weakness, lymphedema, reductions in functional mobility, and menopausal symptoms as a consequence of undergoing treatment (Helms, O’Hea, & Corso, 2008; Taleghani, Yekta, & Nasrabadi, 2006). Provided that the current ideal female body endorsed by Western culture is characterized by thinness, toned muscles, flawless skin, long hair, and well-developed breasts across the lifespan (Halliwell & Dittmar, 2003; Pruis & Janowsky, 2010), survivors are at risk for feeling an even greater discrepancy from this ideal than they did pretreatment (Helms et al., 2008). BCS commonly feel ashamed about their new bodies and turn to beautification techniques for fear of social rejection and loss of femininity (Boquiren, Esplen, Wong, Toner, & Warner, 2013; Pitts, 2004). As such, breast cancer may act as a stimulus for the development of the negative self-conscious emotions of shame and guilt (LoConte, Else-Quest, Eickhoff, Hyde, & Schiller, 2008; Pitts, 2004). Because shame is elicited in response to global failures of the self and often results in motivations to withdraw and escape from others, it is a difficult emotion to alter (Tangney & Tracy, 2012). As such, shame in general and in the context of the body has the potential to be a devastatingly painful experience. In the context of cancer, survivors may globalize their perceived failures to meet idealized beauty standards and blame themselves for their body appearance and weight, leading to avoidance of MVPA participation. Although research supports the assertion that increased feelings of body-related shame can promote disengagement from and lower levels of PA, they have been limited to healthy adult men and women (Castonguay et al., 2015, 2016; Sabiston et al., 2010).
Body-related guilt is defined as negative feelings about one’s behavioral transgression(s) or behavioral self-blame (e.g., “I haven’t exercised since I started my cancer treatment, and that’s why I gained weight”) and typically involves a sense of strain and remorse over the failure (Sabiston & Castonguay, 2014; Tracy & Robins, 2004). Although guilt and shame are similar in many ways, they are distinct experiences with divergent functions. Because guilt is elicited in response to a specific behavior, it is typically less painful than shame and may motivate women to repair the perceived wrongdoing (Conradt et al., 2007; Sabiston et al., 2010). When examined separately from shame, body-related guilt has been shown to be weakly related or unrelated to psychopathologic indicators (e.g., depression) (Castonguay et al., 2016; Conradt et al., 2007) and has demonstrated either no or positive associations with PA (Castonguay et al., 2015; Sabiston et al., 2010). Therefore, feelings of guilt may be used as a motivational tool to engage in strategies, such as MVPA, that may mitigate the physical changes resulting from breast cancer. MVPA has been shown to help women lose weight and body fat, circumvent weight gain, and build muscle tone (Irwin et al., 2009). BCS might be motivated by feelings of guilt to engage in MVPA to improve their physical fitness. The associations between body-related shame, guilt, and MVPA have not been examined among BCS. Based on extant research findings (Castonguay et al., 2015; Sabiston et al., 2010), motivational regulations are likely to be important factors that link body-related emotions and MVPA.
Emotions, Motivation, and Physical Activity
Motivation is recognized as one of the primary factors linking emotions and behavior (Lazarus, 1999). Organismic integration theory (Deci & Ryan, 1985) is a widely used micro-theory that is broadly focused on motivation. Deci and Ryan (1985) conceptualized motivation as a continuum ranging from amotivation (i.e., complete lack of self-determination, when an individual lacks intention to engage in behavior) to intrinsic motivation (i.e., high self-determination, when a behavior is driven by interest or enjoyment in the task itself). In between these extreme ends of the continuum, organismic integration theory defines four types of extrinsic motivational regulations that differ in levels of self-determination and internalization: external regulation (i.e., participate to fulfill external demands), introjected regulation (i.e., participate to avoid feeling guilty or to protect one’s self-worth), identified regulation (i.e., participate because of the personal importance associated with the outcome of the activity), and integrated regulation (i.e., participate to achieve benefits that are considered important and are congruent with core values and beliefs). Often, the more self-determined motives are highly correlated and are combined into an autonomous motivation score (Brunet, Burke, & Sabiston, 2013; Segatto, Sabiston, Harvey, & Bloom, 2013). Generally, higher levels of self-determined motivational regulations are more positively linked to intentions to be active, increased efforts, higher PA levels, and adherence as compared to lower levels of self-determined motivational regulations in healthy populations (Teixeira, Carraça, Markland, Silva, & Ryan, 2012) and patients with cancer (Brunet et al., 2013; Finnegan et al., 2007; Milne, Wallmman, Guilfoyle, Gordon, & Courneya, 2008; Peddle, Plotnikoff, Wild, Au, & Courneya, 2008).
Researchers using cross-sectional study designs with healthy adult women and men have reported positive relations between shame and the less self-determined motivational regulations (i.e., external and introjected), and negative associations with the more self-determined ones (i.e., identified and intrinsic), which were negatively associated with PA (Castonguay et al., 2015; Sabiston et al., 2010). Body-related guilt was positively linked to motivational regulations along the continuum, and positively and negatively linked to PA via the motivational regulations, which implies that body-related guilt may hold maladaptive and reparative qualities. However, the findings cannot be generalized to women who have faced a life-threatening breast cancer diagnosis because many survivors report experiencing emotional turmoil, health problems, and decreases in PA following treatment (Ewertz & Jensen, 2011). The time immediately following treatment is particularly vulnerable because of the reduced support from health practitioners (e.g., reductions in physician appointments); high expectations for roles, responsibilities, and appearance to return to normal; and management of side effects from treatment, such as fatigue, pain, weight gain, and depression symptoms, which are often barriers to MVPA (Sabiston, Brunet, Vallance, & Meterissian, 2014; Ventura et al., 2013). Therefore, exploring the links between BCS’ body-related shame, body-related guilt, motivational regulations, and MVPA is warranted.
Purpose
The aim of the current longitudinal study was to examine whether body-related shame and guilt would predict changes in BCS’ MVPA during six months. The authors hypothesized that body-related shame would predict relatively low levels of PA over time, whereas feelings of guilt would be associated with comparatively higher levels of PA. A second objective was to examine motivational regulations as mediators of the association between body-related shame and guilt and MVPA. Shame was expected to be positively associated with more extrinsic regulations and negatively associated with more self-determined regulations. An inverse pattern was expected for body-related guilt. In addition, the authors anticipated that indirect effects would be present, linking self-conscious emotions and MVPA via motivational regulations.
Methods
Participants and Procedures
Data for this study were drawn from the Life After Breast Cancer: Moving On longitudinal study, which was focused on examining the physical and mental health determinants and consequences of PA in BCS (Sabiston, Wrosch, & O’Loughlin, 2008). Prior to recruitment, approval for the study was obtained from the ethics boards of McGill University and McGill University Health Centre in Montreal, Quebec, Canada. Participants were a convenience sample of 201 women who had completed primary treatment for stages I–III breast cancer. Survivors were recruited to participate in a longitudinal study investigating the natural developmental changes in lifestyle behaviors through advertisements and oncologist referrals from medical clinics and hospitals in Montreal, Quebec, Canada. Women were asked to contact the research team by telephone to obtain additional details on the study. Women were eligible if they met the following criteria: (a) aged 18 years or older, (b) had first diagnosis of breast cancer within the past year, (c) were at least 20 weeks after primary treatment (i.e., surgery or chemotherapy), (d) had the ability to provide informed consent, (e) had the ability to read and speak in English or French, and (f) reported no health concerns that prevented them from engaging in PA.
One hundred forty-nine women (74%) from the convenience sample completed measures on guilt, shame, motivation regulations, and MVPA about nine months post–treatment completion (time 1) and completed measures on MVPA six months later (time 2). The questionnaires were mailed to participants. Group comparisons were conducted to examine whether women who provided data at both time points differed from women who did not. There were no differences in any of the main study variables (p > 0.09) except that participants who provided MVPA data at follow-up had a lower body mass index (BMI) than participants who did not provide activity data (F[1, 197] = 3.86, p = 0.05, h² = 0.019). BMI was calculated from objectively assessed weight and height in kg/m2.
Women were aged 30–79 years, and the majority of participants had been diagnosed with stage I or II breast cancer, were an average of 16 months postdiagnosis, and were somewhat overweight and Caucasian (see Table 1). Reported cancer treatments were lumpectomy, lymph node dissection, unilateral mastectomy, bilateral mastectomy, chemotherapy, radiation therapy, endocrine manipulation therapy, and reconstructive surgery. Most women received at least two treatment combinations, and about half were still receiving endocrine manipulation therapy. 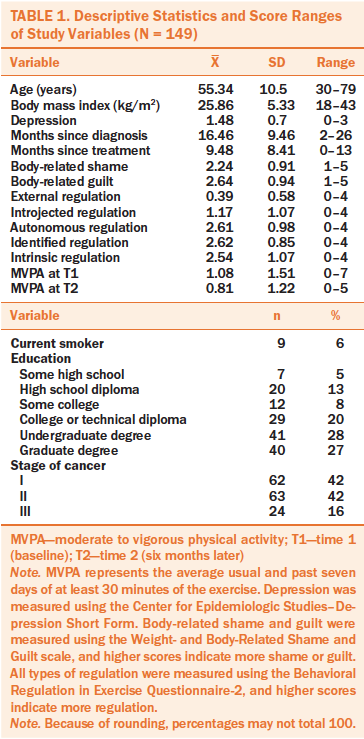
Measures
MVPA was measured at times 1 and 2 with Prochaska, Sallis, and Long’s (2001) screening tool. Two items (“During the past seven days, on how many days were you physically active for a total of at least 30 minutes per day?” and “During a typical or usual week, on how many days are you physically active for a total of at least 30 minutes per day?”) were combined to create a composite score assessing weekly MVPA. Researchers have reported acceptable reliability coefficients (two-week test–retest reliability, r = 0.77), as well as evidence for the construct validity of subjective PA by showing moderate positive correlations with objective measures of PA (accelerometer, r ≥ 0.4) and indicators of fitness in various populations (e.g., BMI) (Janssen et al., 2005; Prochaska et al., 2001). To obtain a measure of six-month changes in MVPA, a residual was calculated in a regression analysis by predicting time 2 levels by time 1 levels and saving the coefficients.
Body-related shame and guilt were assessed at time 1 using the Weight- and Body-Related Shame and Guilt (WEB-SG) scale (Conradt et al., 2007). The WEB-SG scale is a 12-item measure assessing shame (6 items) regarding the body, figure, and weight (e.g., “I am ashamed of myself when others get to know how much I really weigh”) and guilt (6 items) regarding eating habits, exercising, and weight control (e.g., “When I can’t manage to work out physically, I feel guilty”). Item responses ranged from 0 (never) to 4 (always). An average score was calculated for each subscale based on the instrument guidelines. In line with previous self-conscious emotions research (Conradt et al., 2007; Sabiston et al., 2010), shame and guilt were statistically separated using regression analyses to create guilt-free shame and shame-free guilt residual scores prior to conducting the main analyses (i.e., guilt was regressed on shame to create a guilt-free shame score, and shame was regressed on guilt to generate a shame-free guilt score). Previous evidence of internal consistency for the WEB-SG subscale scores include Cronbach alpha coefficients from 0.86–0.92, and convergent and discriminant validity evidence have been documented (Conradt et al., 2007). Cronbach alpha coefficients for the current sample scores for shame and guilt subscales were 0.85 and 0.88, respectively.
Motivational regulations for PA embedded in organismic integration theory were assessed at time 1 using the Behavioral Regulation in Exercise Questionnaire-2 (BREQ-2) (Markland & Tobin, 2004). The BREQ-2 is a 19-item inventory assessing amotivation (4 items; e.g., “I don’t see the point in exercising”), and external (4 items; e.g., “because others say I should”), introjected (3 items; e.g., “I feel guilty when I don’t exercise”), identified (4 items; e.g., “I value the benefits of exercise”), and intrinsic (4 items; e.g., “I exercise because it’s fun”) motivational regulations. Responses to each item were reported on a five-point Likert-type scale from 0 (not true for me) to 4 (very true for me). Scores for each of the motivational regulations were computed by averaging response options across subscales. Construct validity evidence, including structural validity and convergent validity of the BREQ-2 scores, have been reported in exercise contexts. Support for estimates of internal consistency of scores (Cronbach alpha) from each of the regulations has been reported (Wilson, Sabiston, Mack, & Blanchard, 2012). Cronbach alpha coefficients in the current study ranged from 0.75–0.94 for all motivational regulation subscales. Amotivation was not included in the current analyses because the subscale scores are typically skewed and demonstrate weak predictive validity evidence for behavior (Wilson et al., 2012). In addition, amotivation is a construct that is assessed in sedentary samples and/or PA initiates and was not of interest for the current study (Wilson, Rodgers, Loitz, & Scime, 2006).
Sociodemographic and cancer-related variables assessed as covariates were the following: participants’ age, education (0 [did not complete high school] to 5 [postgraduate degree]), BMI, depression, cancer stage (I–III), months since diagnosis, and months since treatment. The Center for Epidemiologic Studies–Depression Short Form (CES-D-10) (Andresen, Malmgren, Carter, & Patrick, 1994) was used to assess depressive symptoms. The 10-item CES-D-10 includes items, such as “I felt depressed,” rated on a four-point Likert-type scale ranging from 0 (rarely) to 3 (most of the time). A mean score was calculated by averaging the 10 items. Responses reflected how the participant felt or behaved during the past week. A score of 10 or greater is indicative of risk for expressing clinical levels of depression. Evidence of internal consistency and validity of scale scores have been demonstrated (Andresen et al., 1994). The Cronbach alpha coefficient was 0.81 in the current study.
Data Analysis
The data were first examined for accuracy of entry, patterns of missing data, potential outliers, and violations of the assumptions of multivariate analysis in SPSS®, version 22.0 (Tabachnick & Fidell, 2007). Missing data for independent variables with less than 5% and missingness were addressed using multiple imputation. Preliminary analyses were conducted to examine direction and strength of changes in MVPA over time using t tests and calculated effect sizes (Cohen’s d). Zero-order correlations were then calculated between study variables. Multiple mediation with bootstrapping procedures (i.e., nonparametric resampling) (Hayes, 2013) was employed to examine the direct and indirect effects of body-related shame and guilt on time 1 and changes in MVPA via motivational regulations (i.e., amotivation, external, introjected, identified, and intrinsic). The SPSS macro PROCESS (Hayes, 2013) was used to conduct the analyses. Given the restrictions in the macro, separate models were estimated for body-related shame and guilt. Participants’ age, education, BMI, depression, stage of breast cancer, time since diagnosis, and time since treatment were entered as covariates in the models. Evidence for mediation in the bootstrap samples (k = 5,000) was observed with the absence of zero in the 95% bias corrected and accelerated confidence interval of the estimate.
Results
Less than 5% of the data were missing on any one variable, and the assumptions of data normality, homoscedasticity, and linearity required for multivariate analyses were met. Multicollinearity evidence was found for identified and intrinsic regulations (r = 0.74) (Tabachnick & Fidell, 2007). An autonomous motivation variable was calculated by computing the mean of the eight items assessing identified regulation and intrinsic motivation (Brunet et al., 2013) to avoid that multicollinearity inflates the size of error terms and weakens the results of multiple regression (Tabachnick & Fidell, 2007). At baseline, participants reported moderate to high levels of body-related shame and guilt, which are comparable with values reported in other studies of healthy adult women and BCS (Fang, Chang, & Shu, 2014; Sabiston et al., 2010). Participants reported engaging in about one day of at least 30 minutes or more of MVPA per week. These findings indicate that, similar to other BCS, a substantial portion of the sample may be at risk for poor health because they are not engaging in the recommended 150 minutes per week of MVPA (Devoogdt et al., 2010; Sabiston & Brunet, 2012). Based on the results from t-test analyses, MVPA significantly decreased during six months (t = –9.13, p ≤ 0.001, d = 0.57).
The zero-order correlations between the main study variables are reported in Table 2. Body-related shame was significantly negatively related to MVPA at times 1 and 2, and body-related guilt was positively associated with MVPA at time 1. Body-related shame was also positively correlated with external regulation and negatively linked to introjected and autonomous motivational regulations. Body-related guilt was positively associated with introjected and autonomous motivational regulations. 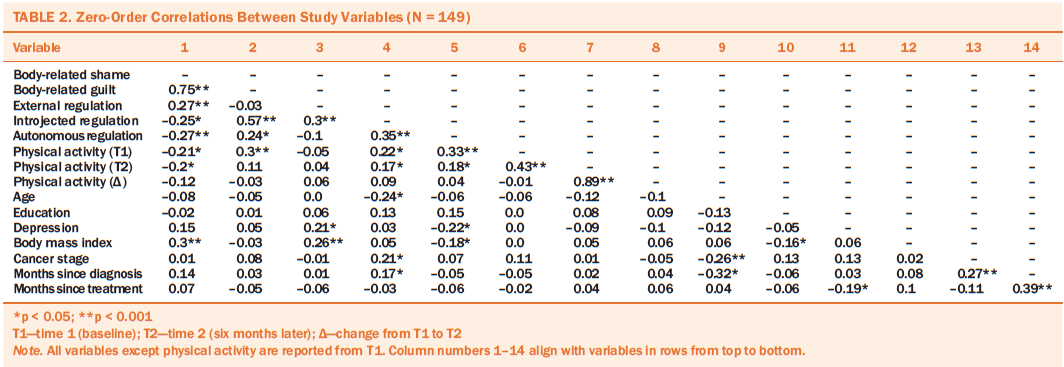
The results of the multiple mediation analyses for the model assessing body-related shame and guilt as predictors of time 1 and changes in MVPA are reported in Table 3. Unstandardized beta coefficients and standard errors for direct effects and bootstrap estimates, confidence intervals, and amount of variance explained for the indirect effects beyond the covariates are displayed in each table. Body-related shame was positively associated with external and negatively associated with introjected and autonomous motivational regulations in the models predicting time 1 levels of MVPA and changes in MVPA. In addition, body-related shame directly and indirectly (via autonomous motivation) predicted low levels of MVPA at time 1. Body-related guilt was positively associated with introjected and autonomous motivational regulations at time 1 and changes in MVPA and also directly predicted high levels of MVPA at time 1. A significant indirect effect suggested that the positive association between guilt and MVPA at time 1 was mediated by higher levels of autonomous motivation. Only body-related shame was a significant predictor of changes in MVPA, indicating that BCS’ MVPA involvement may decrease as a function of higher levels of shame.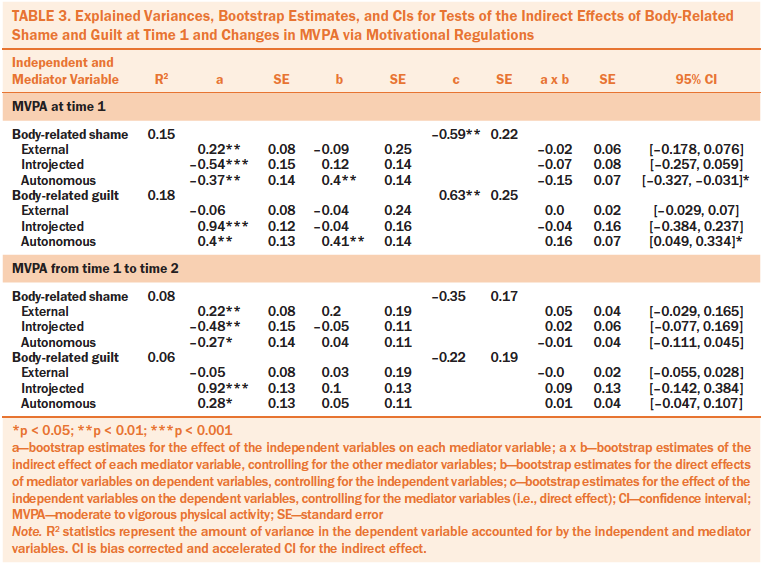
The obtained effects were not altered when the introjected regulation item of the BREQ-2 that taps feelings of guilt was deleted from the scale. The coefficient values estimating the relationship between guilt and introjected regulation for time 1 (0.86) and changes (0.85) in MVPA were slightly lower than those presented in the original models.
Discussion
The results of this study demonstrate that BCS who experienced high levels of body-related shame reported lower levels of and six-month decreases in MVPA in the 18 months following diagnosis. Feelings of shame were positively associated with the less autonomous motivational regulations and negatively associated with more autonomous motivation. Autonomous motivational regulations further mediated the shame (MVPA relation at time 1). These findings suggest that survivors who blame themselves for their weight and appearance may be setting themselves up for relatively immediate and long-term failure of maintaining PA motivation and behavior during the early months following treatment when activity levels steadily decline (Sabiston et al., 2014). Such detrimental effects may occur because BCS may compare their bodies to ideals projected in Western culture, to same-aged healthy peers, or to themselves prior to breast cancer and feel that they are further away from body-related ideals (Helms et al., 2008). Such a comparison is a likely catalyst for negative emotions like shame and guilt. Because shame is a socially motivated emotion and has consistently been linked to desires to hide and escape social contexts (Tangney & Tracy, 2012), it is not surprising that BCS may engage less frequently in PA or participate only to fulfill external demands (e.g., comply with doctor’s orders). This conclusion is consistent with tenets of self-objectification theory (Fredrickson & Roberts, 1997; McKinley & Hyde, 1996) and organismic integration theory (Deci & Ryan, 1985), postulating that feelings of shame may undermine health-relevant motivations and behaviors in women.
The current findings also converge with cross-sectional research in non-cancer populations, documenting that shame contextualized to the body is associated with a host of maladaptive behaviors, including inactivity with total PA (i.e., light, moderate, and vigorous) and MVPA (Castonguay et al., 2015; Sabiston et al., 2010). These findings present initial empirical evidence of the potential links between body-related shame, motivation, and MVPA in an oncology population. They further suggest that objectification theory, objectified body consciousness, and organismic integration theory provide useful frameworks for furthering the understanding of PA levels among BCS. These findings can be used as an important first step in identifying modifiable mechanisms that may help (or harm) women to engage in, and even change, their lifestyle behavioral patterns following diagnosis and treatment. Because of the immediate and enduring damaging effects of shame on health behavior, intervention strategies that minimize body-specific shame among women who have lived with breast cancer are needed. Strategies used by the oncology care team may include helping women to minimize the importance of body weight and appearance and discouraging objectification of their bodies (Fredrickson & Roberts, 1997). This may be facilitated through psychoeducational programs that help women recognize and dispute cultural messages focused on narrow views of beauty that exclude women who have lived with breast cancer and learn about the manipulation techniques used by the media for sales and marketing (Posavac, Posavac, & Weigel, 2001). Based on self-conscious emotions theory (Tracy & Robins, 2004) and empirical work (Castonguay, Brunet, Ferguson, & Sabiston, 2012), interventions may also focus on manipulating cognitive appraisals that elicit shame. Practitioners could encourage survivors to hold realistic expectations of their bodies to lessen the difference between their actual and ideal body. Survivors who are prone to feelings of shame could be directed to attribute the cause of the failure to an external factor rather than to themselves being defective (e.g., relating weight gain to drugs used in cancer treatment).
In addition, the analyses showed that feelings of guilt were positively related to self-determined forms of motivation, which mediated higher levels of concurrent MVPA. In support of the study’s hypotheses, body-related shame and guilt differentially were shown to relate to PA motivation and behavior over time. A conclusion of this pattern is that the differential effects of self-conscious emotions can be lasting. In particular, feelings of guilt may serve as a short-term reparative function and may motivate PA behaviors, which contradicts the more maladaptive nature of this emotion frequently described in the general guilt literature (Tangney & Tracy, 2012), as well as research extending self-objectification framework to guilt and disordered eating behavior (Calogero & Pina, 2011) and MVPA (Castonguay et al., 2015). Clinicians may be able to guide their patients toward making cognitive appraisals that are directed to specific behavioral mishaps (guilt) rather than blaming themselves for failure (shame). In this way, they may instill in their patients the belief that they have some control over their appearance and weight (e.g., increased muscle mass). An important future endeavor is to develop and evaluate the effectiveness of interventions aimed at facilitating feelings of guilt to promote self-determined forms of motivation and MVPA in the early survivorship phase. Although these strategies may be effective for initiating MVPA, their effectiveness in prolonged participation is uncertain because they are driven, at least in part, by external factors (Deci & Ryan, 1985). As such, an integration of these strategies with the self may need to be supported by the clinician. Researchers are further encouraged to assess body-related guilt across more time points and across the survivorship trajectory to explore the sustainability of guilt as a positive and reparative emotion for PA.
Consistent with the literature on motivational regulations and PA (Teixeira et al., 2012), autonomous (identified and intrinsic) regulations were the motives most consistently associated with initial MVPA in the current study. One pathway by which feelings of guilt and shame can influence MVPA is related to enhancing or diminishing, respectively, self-determined motivation. Therefore, oncology care team members should work to promote perceptions of competence, autonomy, and relatedness (Deci & Ryan, 1985) by encouraging their patients to participate in activities that are self-selected, give them opportunities to accomplish and master a task, and provide an environment that allows for meaningful socialization with others.
A strength of the current research is the use of a prospective longitudinal design because it extends previous cross-sectional findings in the literature and permits the examination of the temporal associations between body-related shame, body-related guilt, motivational regulations, and MVPA behavior among women who completed treatment for breast cancer. This is one of the first studies to examine components of self-objectification theory in an oncology population. Understanding self-objectification, along with body-related shame and guilt, in women who have lived with breast cancer is important. Once the immediate threat of survival has dissipated, they are faced with the challenge of negotiating their new, changed bodies, which often leads to substantial emotional turmoil and increased risk for physical health declines (Fang et al., 2014; Helms et al., 2008).
Limitations
Several limitations to this study should be considered. First, the items used to assess body-related shame and guilt were designed to explore more weight-related aspects of the body and do not capture some other factors that may be relevant to BCS, such as hair texture or physical function, limiting its use with survivors who are not sensitive to weight-related aspects of appearance. Future researchers should consider using an instrument that may more fully represent shame and guilt emotional experiences in this population (Castonguay et al., 2016). Second, although shame and guilt are the most frequently studied self-conscious emotions, other emotions (e.g., authentic pride) may also influence MVPA (Castonguay et al., 2016), which would provide an alternative focus toward body appreciation and should be addressed in future research. Third, data were drawn from only two assessment points about six months apart, which limits their use for assessing long-term outcomes. However, the timing of the two assessments may be unique because, in the six months after treatment for breast cancer, women may experience greater marked changes in their body appearance or function than during other times in the survivorship trajectory. They may also experience late- and longer-term effects from the treatment in this period. Fourth, participants were from a volunteer convenience sample, and women who provided follow-up PA data had a lower measured BMI than those who did not provide data. However, BMI was not associated with the main study variables; therefore, this bias likely did not compromise the interpretation of the findings. Researchers should cross-validate the current findings in women with varying weight status. Fifth, the creation of an autonomous motivation score limits potential emergence of divergent relationships among identified and intrinsic regulations and body-related self-conscious emotions and MVPA. Sixth, high coefficient values were observed between guilt and introjected motivational regulations in the mediation model predicting MVPA. Although values of such magnitude are consistent with previous research (Castonguay et al., 2015; Sabiston et al., 2010), they may reflect that at least one BREQ-2 item assessing introjected regulation appears to tap feelings of guilt. Potential item overlap may have contributed to inflated relationships in the current study.
Implications for Nursing
Few studies specifically focus on the body-related self-conscious emotional experiences of women who have recently been treated for breast cancer. Consequently, healthcare professionals may not be sensitized to the specific experience of body-related emotions in patients with cancer. In practice, healthcare professionals need to consider how emotions related to the body can affect health behaviors and associated mental and physical health. Nurses should be prepared to assess a variety of emotional experiences, including shame and guilt, that may be uncommon or not routinely reported by patients to help BCS engage in more MVPA. Referrals to mental health counselors should be made when problems are identified. In addition, nurses and other healthcare professionals could work to develop survivorship care plans focused on these body-related, self-conscious emotions and help survivors navigate them in the early post-treatment period. Practitioners and researchers should work to design and develop programs aimed at reducing the negative body-related emotions via cognitive behavioral therapy and cognitive dissonance. Specifically, nurses and clinicians should be cognizant of the potential role of objectified body consciousness in promoting cancer-related body image discomfort in BCS during the survivorship phase. Encouraging women to clarify their perceptions of their bodies after receiving treatment is necessary and may be achieved by helping women redefine personal standards of beauty, femininity, and role functioning that are realistic, achievable, and less focused on societal expectations (Boquiren et al., 2013). Adjusted views of the self may facilitate flexibility in self-perceptions and diminish potential negative self-evaluative emotions, such as shame, post-treatment (Castonguay et al., 2012). In addition, nurses and other oncology care team members can help women who are prone to feeling shame attribute causes of their perceived body-related failure to external factors (e.g., genetics for changes in weight) or a specific behavioral transgression (e.g., not exercising) rather than placing blame on themselves for being flawed. 
Conclusion
This prospective study illustrates the diverging effects of body-related shame (maladaptive) and body-related guilt (adaptive) on health-related motivations and behaviors in an oncology population. The identification of these mechanisms advances theory on the health-related consequences of body-related self-conscious emotions following the completion of treatment for the disease. In addition, modifying experiences of shame and guilt represents an effective nonpharmacologic treatment that can improve physical health and well-being for patients with cancer (Tangney & Tracy, 2012).
[[{"type":"media","view_mode":"media_original","fid":"33251","attributes":{"alt":"","class":"media-image","height":"498","typeof":"foaf:Image","width":"369"}}]]
About the Author(s)
Castonguay is a postdoctoral fellow and Wrosch is a professor, both in the Department of Psychology at Concordia University in Montreal, Quebec; and Pila is a PhD candidate and Sabiston is an associate professor, both in the Faculty of Kinesiology and Physical Education at the University of Toronto in Ontario, all in Canada. This research was funded by a grant from the Canadian Institutes of Health Research (CIHR) awarded to Sabiston and Wrosch. Additional support was provided by the CIHR and a grant from the Social Sciences and Humanities Research Council of Canada awarded to Wrosch. Castonguay is supported by a postdoctoral fellowship from the CIHR. Castonguay, Wrosch, and Sabiston contributed to the conceptualization and design, completed the data collection, and provided statistical support. Castonguay and Wrosch provided the analysis. All authors contributed to the manuscript preparation. Castonguay can be reached at andree.castonguay@mail.mcgill.ca, with copy to editor at ONFEditor@ons.org. Submitted July 2016. Accepted for publication December 26, 2016.
References
Andresen, E.M., Malmgren, J.A., Carter, W.B., & Patrick, D.L. (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiological Studies Depression Scale). American Journal of Preventive Medicine, 10, 77–84.
Boquiren, V.M., Esplen, M.J., Wong, J., Toner, B., & Warner, E. (2013). Exploring the influence of gender-role socialization and objectified body consciousness on body image disturbance in breast cancer survivors. Psycho-Oncology, 22, 2177–2185. doi:10.1002/pon.3271
Brunet, J., Burke, S.M., & Sabiston, C.M. (2013). The benefits of being self-determined in promoting physical activity and affective well-being among women recently treated for breast cancer. Psycho-Oncology, 22, 2245–2252. doi:10.1002/pon.3287
Calogero, R.M., & Pina, A. (2011). Body guilt: Preliminary evidence for a further subjective experience of self-objectification. Psychology of Women Quarterly, 35, 428–440. doi:10.1177/0361684311408564
Castonguay, A.L., Brunet, J., Ferguson, L., & Sabiston, C.M. (2012). Weight-related actual and ideal self-states, discrepancies, and shame, guilt, and pride: Examining associations within the process model of self-conscious emotions. Body Image, 9, 488–494. doi:10.1016/j.bodyim.2012.07.003
Castonguay, A.L., Pila, E., Wrosch, C., & Sabiston, C.M. (2015). Body-related self-conscious emotions relate to physical activity motivation and behavior in men. American Journal of Men’s Health, 9, 209–221. doi:10.1177/1557988314537517
Castonguay, A.L., Sabiston, C.M., Kowalski, K.C., & Wilson, P.M. (2016). Introducing an instrument to measure body and fitness-related self-concious emotions: The BSE-FIT. Psychology of Sport and Exercise, 23, 1–12. doi:10.1016/j.psychsport.2015.10.003
Conradt, M., Dierk, J.M., Schlumberger, P., Rauh, E., Hebebrand, J., & Rief, W. (2007). Development of the Weight- and Body-Related Shame and Guilt Scale (WEB-SG) in a nonclinical sample of obese individuals. Journal of Personality Assessment, 88, 317–327. doi:10.1080/00223890701331856
Deci, E.L., & Ryan, R.M. (1985). Intrinsic motivation and self-determination in human behavior. New York, NY: Plenum Press.
Demark-Wahnefried, W., & Jones, L.W. (2008). Promoting a healthy lifestyle among cancer survivors. Hematology/Oncology Clinics of North America, 22, 319–342. doi:10.1016/j.hoc.2008.01.012
Devoogdt, N., Van Kampen, M., Geraerts, I., Coremans, T., Fieuws, S., Lefevre, J., . . . Chistiaens, M.R. (2010). Physical activity levels after treatment for breast cancer: One-year follow-up. Breast Cancer Research and Treatment, 123, 417–425. doi:10.1007/s10549-010-0997-6
Ewertz, M., & Jensen, A.B. (2011). Late effects of breast cancer treatment and potentials for rehabilitation. Acta Oncologica, 50, 187–193. doi:10.3109/0284186X.2010.533190
Fang, S.-Y., Chang, H.-T., & Shu, B.-C. (2014). Objectified body consciousness, body image discomfort, and depressive symptoms among breast cancer survivors in Taiwan. Psychology of Women Quarterly, 38, 563–574. doi:10.1177/0361684314552652
Finnegan, L., Wilkie, D.J., Wilbur, J., Campbell, R.T., Zong, S., & Katula, S. (2007). Correlates of physical activity in young adult survivors of childhood cancers [Online exclusive]. Oncology Nursing Forum, 34, E60–E69. doi:10.1188/07.ONF.E60-E69
Fredrickson, B.L., & Roberts, T. (1997). Objectification theory: Toward understanding women’s lived experiences and mental health risks. Psychology of Women Quarterly, 21, 173–206. doi:10.1111/j.1471-6402.1997.tb00108.x
Halliwell, E., & Dittmar, H. (2003). A qualitative investigation of women’s and men’s body image concerns and their attitudes toward aging. Sex Roles, 49, 675–684. doi:10.1023/B:SERS.0000003137.71080.97
Hayes, A.F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press.
Helms, R.L., O’Hea, E.L., & Corso, M. (2008). Body image issues in women with breast cancer. Psychology, Health and Medicine, 13, 313–325. doi:10.1080/13548500701405509
Irwin, M.L., Alvarez-Reeves, M., Cadmus, L., Mierzejewski, E., Mayne, S.T., Yu, H., . . . DiPietro, L. (2009). Exercise improves body fat, lean mass, and bone mass in breast cancer survivors. Obesity, 17, 1534–1541. doi:10.1038/oby.2009.18
Janssen, I., Katzmarzyk, P.T., Boyce, W.F., Vereecken, C., Mulvihill, C., Roberts, C., . . . Pickett, W. (2005). Comparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patterns. Obesity Reviews, 6, 123–132. doi:10.1111/j.1467-789X.2005.00176.x
Lazarus, R.S. (1999). Stress and emotion: A new synthesis. New York, NY: Springer.
LoConte, N.K., Else-Quest, N.M., Eickhoff, J., Hyde, J., & Schiller, J.H. (2008). Assessment of guilt and shame in patients with non-small-cell lung cancer compared with patients with breast and prostate cancer. Clinical Lung Cancer, 9, 171–178. doi:10.3816/CLC.2008.n.026
Markland, D., & Tobin, V. (2004). A modification of the Behavioral Regulation in Exercise Questionnaire to include an assessment of amotivation. Journal of Sport and Exercise Psychology, 26, 191–196. doi:10.1123/jsep.26.2.191
McKinley, N.M., & Hyde, J.S. (1996). The objectified body consciousness scale: Development and validation. Psychology of Women Quarterly, 20, 181–215. doi:10.1111/j.1471-6402.1996.tb00467.x
Milne, H.M., Wallmman, K.E., Guilfoyle, A., Gordon, S., & Courneya, K.S. (2008). Self-determination theory and physical activity among breast cancer survivors. Journal of Sport and Exercise Psychology, 30, 23–38.
Peddle, C.J., Plotnikoff, R.C., Wild, T.C., Au, H.J., & Courneya, K.S. (2008). Medical, demographic, and psychosocial correlates of exercise in colorectal cancer survivors: An application of self-determination theory. Supportive Care in Cancer, 16, 9–17. doi:10.1007/s00520-007-0272-5
Pitts, V. (2004). Illness and internet empowerment: Writing and reading breast cancer in cyberspace. Health, 8, 33–59. doi:10.1177/1363459304038794
Posavac, H.D., Posavac, S.S., & Weigel, R.G. (2001). Reducing the impact of media images on women at risk for body image disturbance: Three targeted interventions. Journal of Social and Clinical Psychology, 20, 324–340. doi:10.1521/jscp.20.3.324.22308
Prochaska, J.J., Sallis, J.F., & Long, B. (2001). A physical activity screening measure for use with adolescents in primary care. Archives of Pediatrics and Adolescent Medicine, 155, 554–559. doi:10.1001/archpedi.155.5.554
Pruis, T.A., & Janowsky, J.S. (2010). Assessment of body image in younger and older women. Journal of General Psychology, 137, 225–238.
Sabiston, C.M., & Brunet, J. (2012). Reviewing the benefits of physical activity during cancer survivorship. American Journal of Lifestyle Medicine, 6, 167–177. doi:10.1177/1559827611407023
Sabiston, C.M., & Castonguay, A.L. (2014). Self-conscious emotions. In R. Eklund & G. Tenenbaum (Eds.), Encyclopedia of sport and exercise psychology (pp. 623–626). Thousand Oaks, CA: Sage Publications.
Sabiston, C.M., Brunet, J., Kowalski, K.C., Wilson, P.M., Mack, D.E., & Crocker, P.R. (2010). The role of body-related self-conscious emotions in motivating women’s physical activity. Journal of Sport and Exercise Psychology, 32, 417–437.
Sabiston, C.M., Brunet, J., Vallance, J.K., & Meterissian, S. (2014). Prospective examination of objectively assessed physical activity and sedentary time after breast cancer treatment: Sitting on the crest of the teachable moment. Cancer Epidemiology, Biomarkers and Prevention, 23, 1324–1330. doi:10.1158/1055-9965.EPI-13-1179
Sabiston, C.M., Wrosch, C., & O’Loughlin, J. (2008). Physical activity among breast cancer survivors: Understanding the impact on biological risk factors and psychological health over time. Canadian Institutes of Health Research.
Segatto, B., Sabiston, C.M., Harvey, W.J., & Bloom, G.A. (2013). Exploring relationships among distress, psychological growth, motivation, and physical activity among transplant recipients. Disability and Rehabilitation, 35, 2097–2103. doi:10.3109/09638288.2013.807882
Tabachnick, B.G., & Fidell, L.S. (2007). Using multivariate statistics. Boston, MA: Allyn and Bacon.
Taleghani, F., Yekta, Z.P., & Nasrabadi, A.N. (2006). Coping with breast cancer in newly diagnosed Iranian women. Journal of Advanced Nursing, 54, 265–272. doi:10.1111/j.1365-2648.2006.03808_1.x
Tangney, J.P., & Tracy, J.L. (2012). Self-conscious emotions. In M. Leary & J.P. Tangney (Eds.), Handbook of self and identity (2nd ed., pp. 446–478). New York, NY: Guilford Press.
Teixeira, P.J., Carraça, E.V., Markland, D., Silva, M.N., & Ryan, R.M. (2012). Exercise, physical activity, and self-determination theory: A systematic review. International Journal of Behavioral Nutrition and Physical Activity, 9, 78. doi:10.1186/1479-5868-9-78
Tracy, J.L., & Robins, R.W. (2004). Putting the self into self-conscious emotions: A theoretical model. Psychological Inquiry, 15, 103–125. doi:10.1207/s15327965pli1502_01
Ventura, E.E., Ganz, P.A., Bower, J.E., Abascal, L., Petersen, L., Stanton, A.L., & Crespi, C.M. (2013). Barriers to physical activity and healthy eating in young breast cancer survivors: Modifiable risk factors and associations with body mass index. Breast Cancer Research and Treatment, 142, 423–433. doi:10.1007/s10549-013-2749-x
Wilson, P.M., Rodgers, W.M., Loitz, C.C., & Scime, G. (2006). “It’s who I am…Really!” The importance of integrated regulation in exercise contexts. Journal of Applied Biobehavioral Research, 11, 79–104. doi:10.1111/j.1751-9861.2006.tb00021.x
Wilson, P.M., Sabiston, C.M., Mack, D.E., & Blanchard, C.M. (2012). On the nature and function of scoring protocols used in exercise motivation research: An empirical study of the behavioral regulation in exercise questionnaire. Psychology of Sport and Exercise, 13, 614–622. doi:10.1016/j.psychsport.2012.03.009

