Factors Associated With Medication Beliefs in Patients With Cancer: An Integrative Review
Problem Identification: Medication beliefs are linked to medication adherence in cancer treatment. Oral cancer treatments are increasing, making patients responsible for self-managing medication at home.
Literature Search: A literature search was performed using CINAHL®, PubMed, and PsycINFO. Included studies were published in English from 2000–2017 and examined medication beliefs among participants aged 18 years or older who were prescribed cancer medication.
Data Evaluation: Articles were organized by study design, how medication beliefs were measured, and whether psychometric testing was evaluated. Articles were scored to indicate rigor of medication belief measurements. Themes of factors associated with medication beliefs were compiled.
Synthesis: The review represented several cancer and cancer medication types. Various methods were used to elicit medication beliefs. Medication beliefs influence decisions to initiate or continue cancer medications, and those beliefs are multifaceted. Nurses have a critical role in evaluating and supporting facilitative medication beliefs.
Implications for Research: Nurses can address medication beliefs and clarify treatment misconceptions. Understanding factors influencing medication beliefs can inform future interventions to improve adherence and symptom management.
Jump to a section
The development of oral cancer medications (OCMs) has sharply increased since 2004 (Mancini, McBride, & Kruczynski, 2013). More than half of the cancer treatments recently approved by the U.S. Food and Drug Administration (FDA) are in oral form (Center Watch, 2018), and that number is expected to increase with the anticipation of more clinical trials involving OCMs. OCMs often have narrow therapeutic ranges and safety margins (Neuss et al., 2013; Vioral, Leslie, Best, & Somerville, 2014), making managing medication regimens essential for improved patient outcomes.
Medication beliefs are linked to patient outcomes, such as symptom experience and adherence, in a number of chronic illnesses, including cancer (Chater, Parham, Riley, Hutchison, & Horne, 2014; Horne, Weinman, & Hankins, 1999; Kalichman, Kalichman, & Cherry, 2016; Lu et al., 2016; Saratsiotou et al., 2011); however, less is known about factors influencing those beliefs. With OCMs being increasingly prescribed, the responsibility of self-managing medication falls onto patients and their caregivers (Given, Spoelstra, & Grant, 2011). OCM regimens can be complex and involve side effects that can make adherence and symptom management challenging (Given et al., 2011). Cancer is regarded as a chronic condition requiring long-term use of OCMs (National Comprehensive Care Network, n.d.). Therefore, factors associated with cancer medication beliefs that can influence medication taking in the home environment warrant closer exploration.
The aim of this integrative review was to explore medication beliefs and associated factors among patients receiving medication to treat cancer and provide a synthesis of current measures to evaluate medication beliefs. The scope of the review is broad to include all types of cancer medication (oral and IV) because research is scarce regarding beliefs specific to anticancer medications. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist helped guide methods for this review (Moher, Liberati, Tetzlaff, & Altman, 2009).
Methods
Search Strategies
A literature search was performed using CINAHL®, PubMed, and PsycINFO as primary search engines. Specific search terms were “medication beliefs” OR “treatment beliefs” OR “medication perceptions” OR “treatment perceptions” OR “medication views” OR “treatment views” OR “medication attitudes” OR “treatment attitudes” AND “chemotherapy” OR “oral agents” OR “antineoplastic agents” OR “targeted agents” OR “cancer.” Key terms were incorporated into a complex search strategy to narrow results.
A second search was performed in CINAHL, PubMed, and PsycINFO specific to the Beliefs About Medicines Questionnaire (BMQ) using the following key terms: “Beliefs about Medicine* Questionnaire” AND “chemotherapy” OR “oral agents” OR “antineoplastic agents” OR “targeted agents” OR “oral cancer medication” OR “anticancer” OR “cancer.” MeSH (Medical Subject Headings) terms were not used because results did not yield applicable literature.
Inclusion and Exclusion Criteria
Inclusion criteria comprised research articles published from 2000–2017 in English that included an examination of medication beliefs among participants aged 18 years or older who were prescribed or undergoing medication treatment for cancer. A well-known measure of medication beliefs, the BMQ, was published in late 1999 and is the rationale to include articles published after this time. Articles were excluded if beliefs were not specific to cancer medication treatment, if articles presented medication beliefs of physicians or caregivers, or if articles focused on beliefs about cancer-related pain medication.
Search Outcome
The initial search produced 259 results. After accounting for duplicate studies, 251 articles remained. The 251 article titles and abstracts were screened. An additional 207 articles were excluded for not meeting inclusion criteria, leaving 44 articles for full-text review of inclusion criteria. Thirty-six articles met full inclusion criteria and were included in the review (see Figure 1). 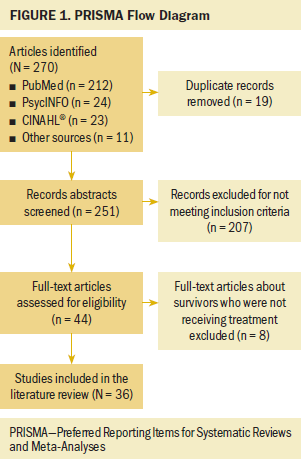
Data Evaluation
Articles were derived from several diverse methodologies. Using the data analysis strategy set forth by Whittemore and Knafl (2005), data were reduced by first organizing articles by type of study design. Articles then were organized by how cancer-specific medication beliefs were measured. Articles were further organized by whether psychometric testing was evaluated on the instrument used (excluding those using qualitative methods). The rationale for categorizing articles based on how medication beliefs were measured was to provide a review of the state of the science with what is currently known regarding medication beliefs in individuals with cancer. Articles were given one of five ratings to indicate the rigor of medication belief measurements, with higher numbers indicating stronger methodologic measurements. Literature and systematic reviews were not rated because they simply summarized studies and medication belief measurements. Last, themes of factors associated with medication beliefs were compiled.
Results
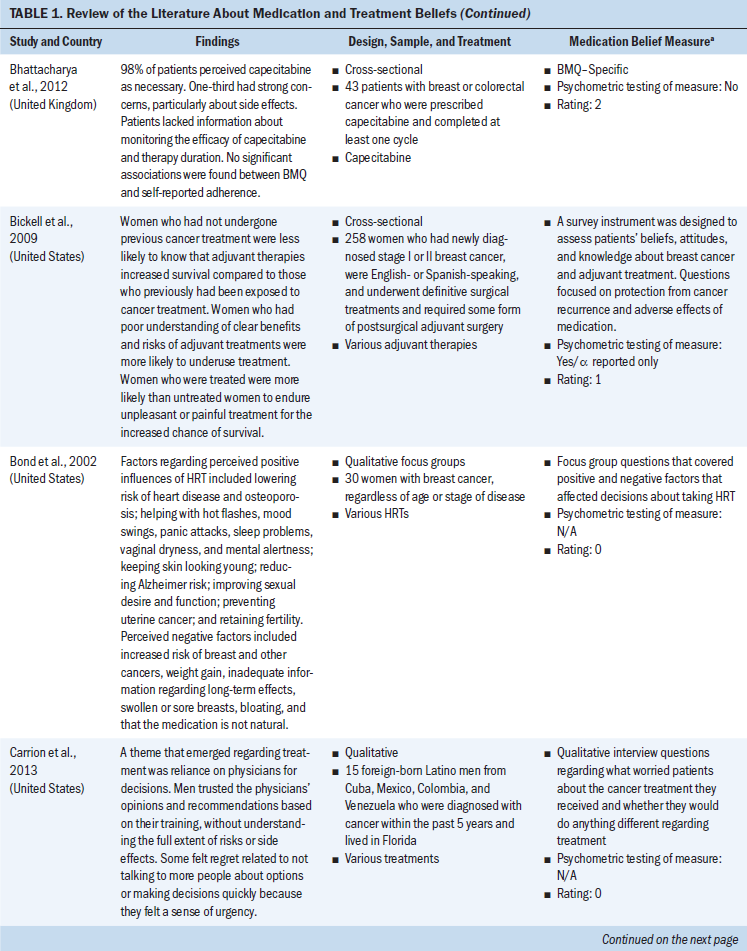
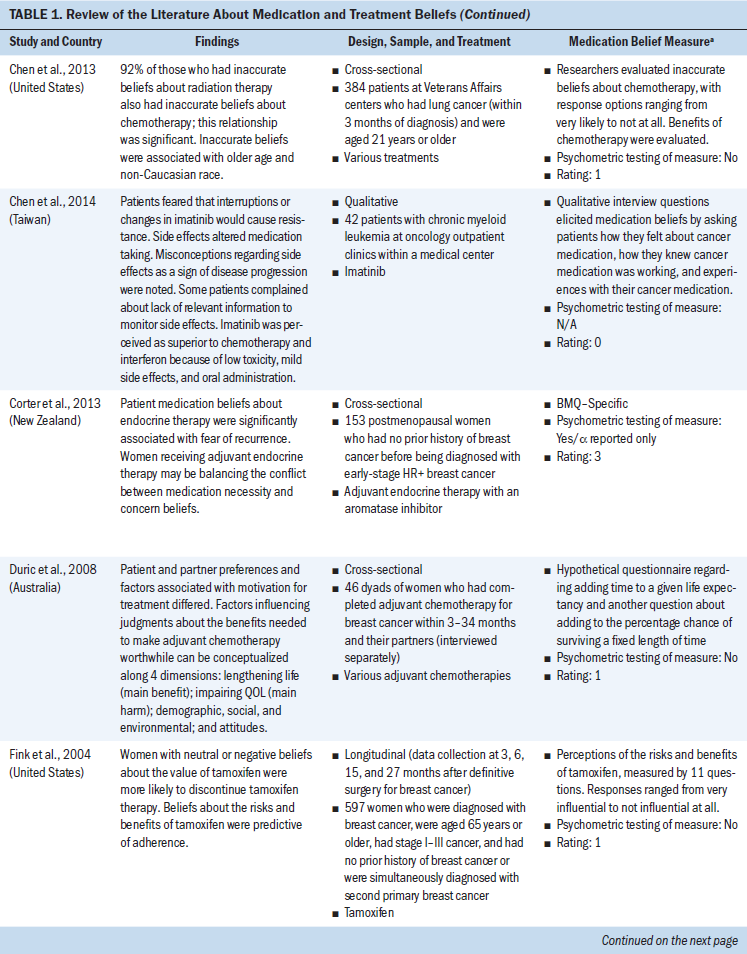
Publication dates for included articles range from 2001–2017. Studies were largely cross-sectional, accounting for 18 of the 36 studies. Five qualitative studies supplied rich data on patients’ perceptions and beliefs about oral chemotherapy and other cancer treatments. Three literature reviews, two systematic reviews, and eight longitudinal studies also were included.
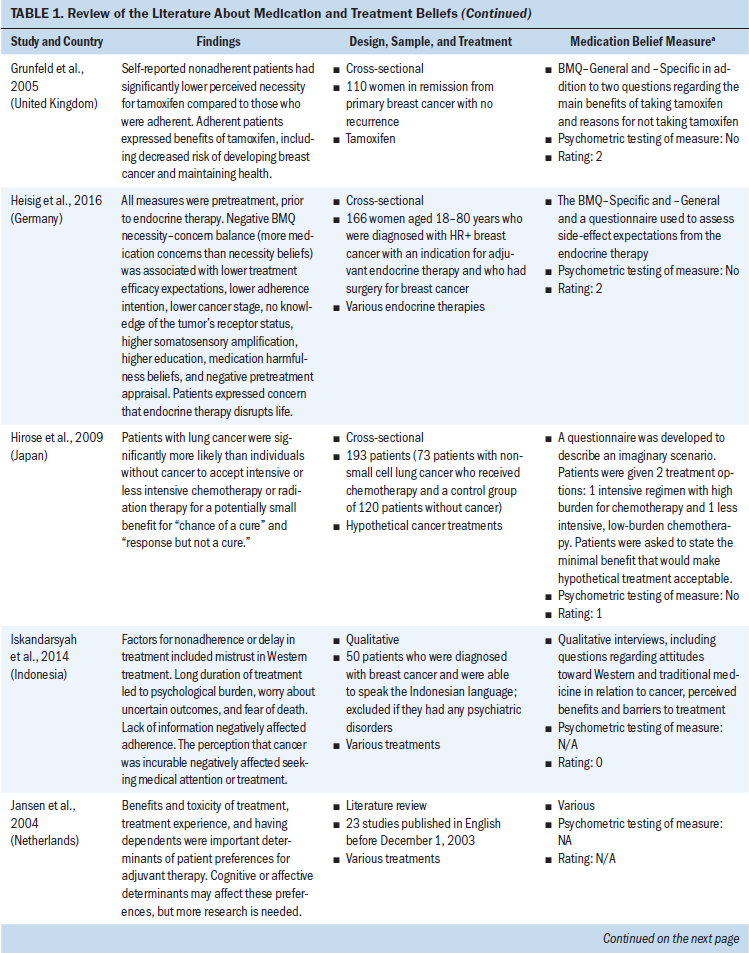
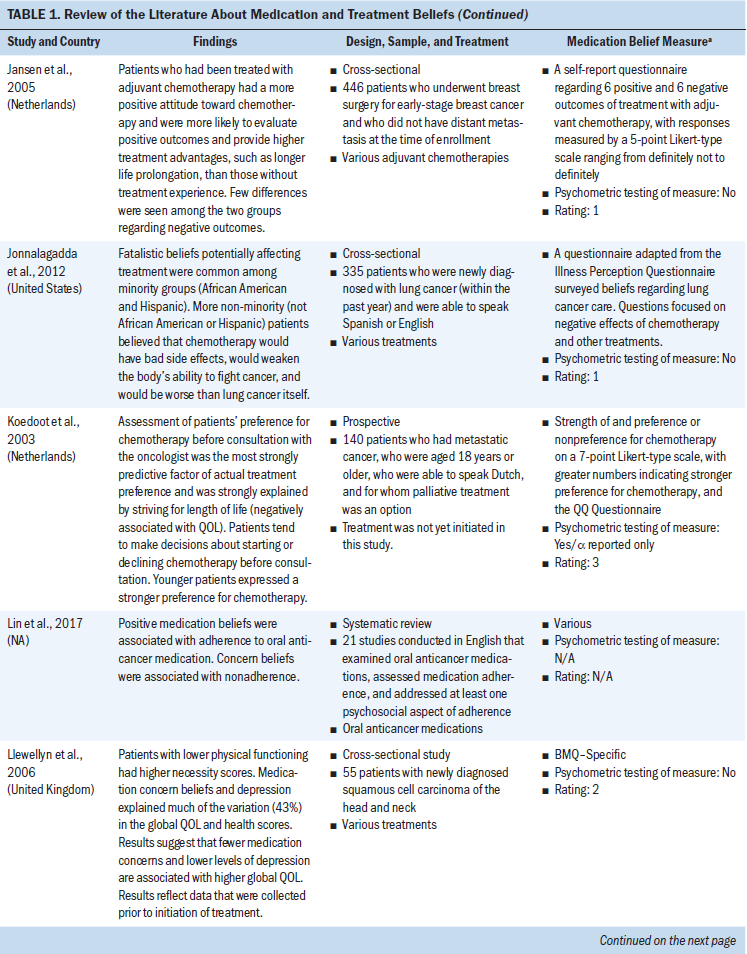
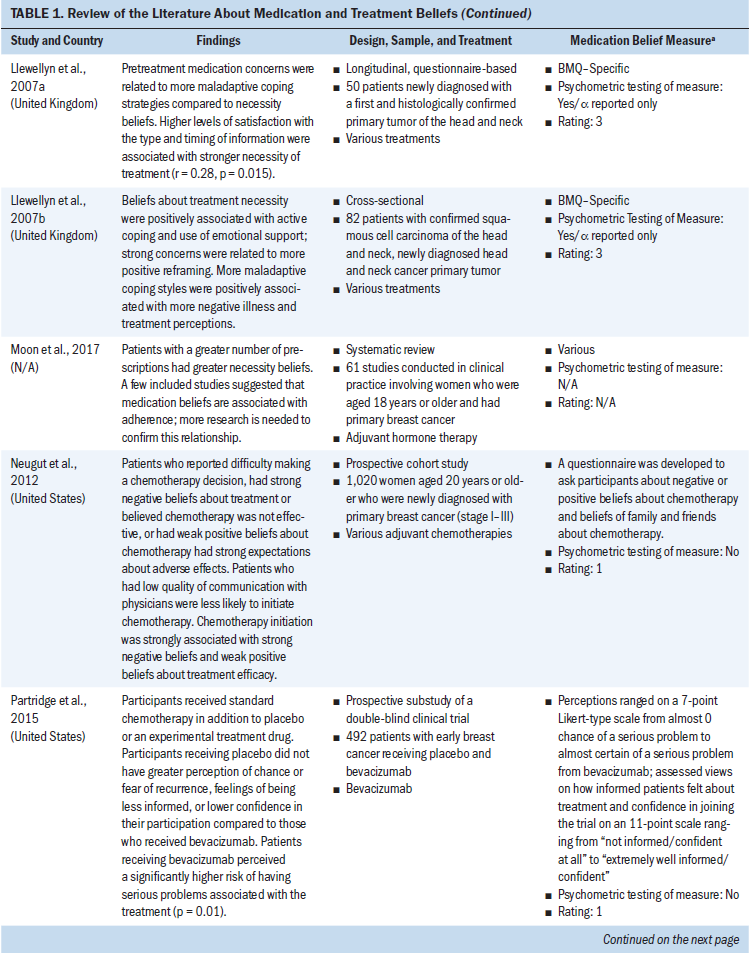
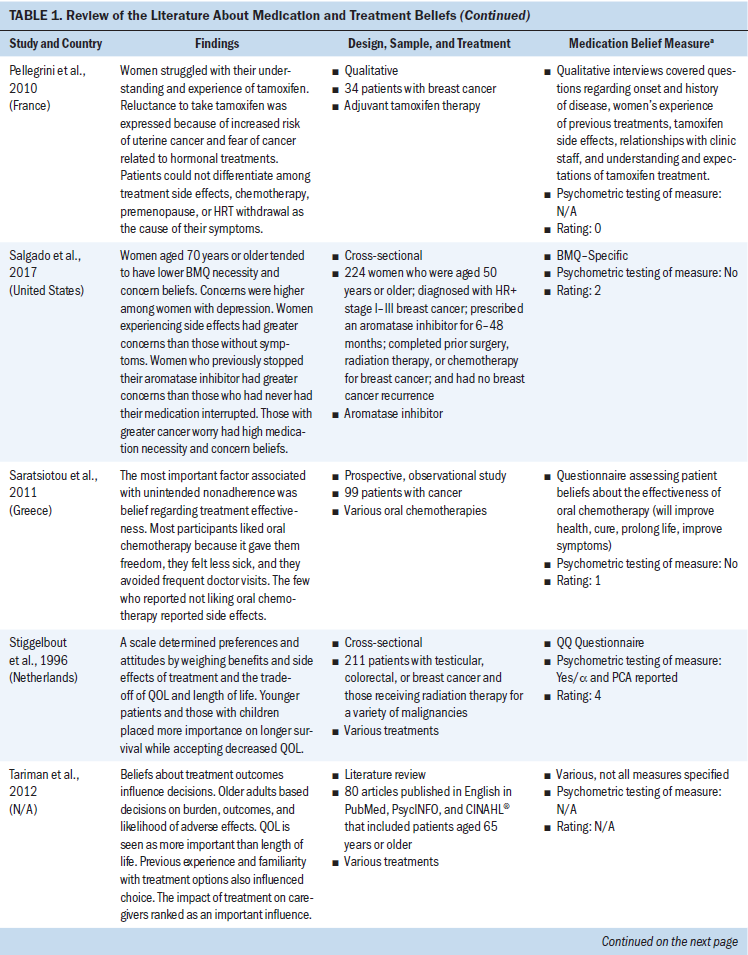
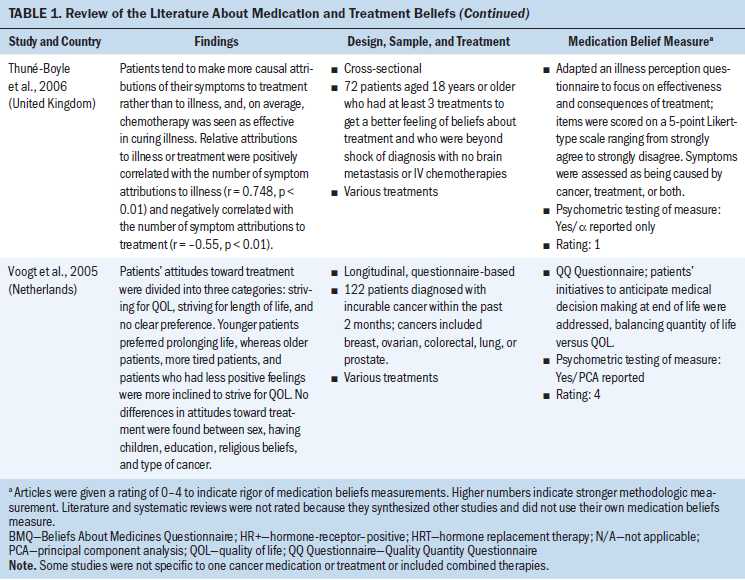
All study participants were aged 18 years or older. Several types of cancer were represented (chronic myeloid leukemia and breast, ovarian, testicular, colorectal, prostate, lung, and head and neck cancer). Some studies concentrated on specific cancer types, and others examined medication and treatment beliefs among patients with various cancer types. Breast cancer represented the most frequent type of cancer. Cancer medications consisted mostly of oral adjuvant chemotherapies and endocrine therapies. Other cancer medications included various IV chemotherapies and oral targeted agents (see Table 1). 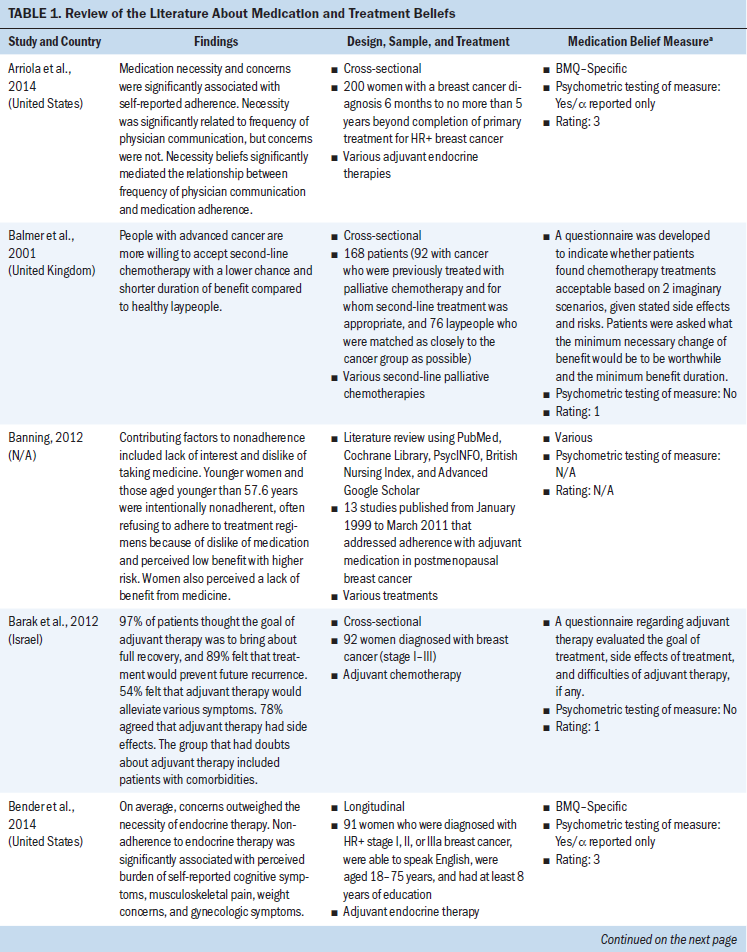
Settings
Study participants were mainly recruited from outpatient and hospital-based oncology clinics. Studies spanned across several countries (the United States, the United Kingdom, Taiwan, Japan, New Zealand, Indonesia, France, Australia, the Netherlands, Israel, and Greece). Most studies were conducted in the United States (10 studies) and the United Kingdom (7 studies).
Medication Beliefs Measures
Only two measures of medication and treatment beliefs were consistent: the BMQ and the Quality Quantity Questionnaire (QQ Questionnaire).
The BMQ–Specific focuses on beliefs about medication that are prescribed for a specific illness, as opposed to medication in general, and is comprised of two subscales. The necessity subscale evaluates whether patients perceive that their medication is needed to treat their illness, and the concern subscale evaluates possible distrust in medications (Horne et al., 1999).
The QQ Questionnaire is specific to people with cancer and measures perceptions regarding the benefit of treatment against the risks or side effects of cancer treatment (Stiggelbout, De Haes, Kiebert, Kievit, & Leer, 1996). Specifically, the QQ Questionnaire measures how perceptions of cancer medication guide a balance between an individual’s quality of life (QOL) versus length (quantity) of life (Stiggelbout et al., 1996).
Additional questionnaires have been developed to evaluate perceptions of cancer treatments (Balmer, Thomas, & Osborne, 2001; Bickell, Weidmann, Fei, Lin, & Leventhal, 2009; Partridge et al., 2015; Thuné-Boyle, Myers, & Newman, 2006). For example, Thuné-Boyle et al. (2006) developed a questionnaire evaluating beliefs involving the effectiveness of cancer treatment and whether patients perceived symptoms to be a result of their cancer, the cancer treatment, or both.
Some research studies used qualitative interviews to elicit cancer medication and treatment beliefs that represented perceived benefits, barriers, or risks associated with cancer treatment (Iskandarsyah et al., 2014). Qualitative research used broad questions regarding positive and negative aspects of cancer treatment (Bond, Hirota, Fortin, & Col, 2002).
Factors Associated With Medication Beliefs
Benefit versus risk: Medication-taking behavior can be influenced by a benefit–risk analysis in which patients weigh the benefits of medication against the risks associated with medication, such as adverse symptoms (Banning, 2012; Bickell et al., 2009). For example, individuals with breast cancer participating in a focus group revealed that they weighed the risk of breast cancer recurrence with concerns, such as osteoporosis and loss of youthfulness, when making decisions about initiating hormone replacement therapy (Bond et al., 2002). In another study, continued adherence was reported among individuals with breast cancer who felt that benefits of tamoxifen therapy (selective estrogen receptor modulator hormonal therapy) outweighed risks, underscoring the link between a patient’s medication beliefs and oral adherence (Fink, Gurwitz, Rakowski, Guadagnoli, & Silliman, 2004).
Patients with life-threatening illnesses, such as advanced cancer, may weigh benefits and risks differently than those with lower-stage cancers. Several studies reported that patients were willing to accept treatment that had high risk for symptoms and side effects with very little gain of life expectancy or improvement of prognosis (Balmer et al., 2001; Hirose et al., 2009; Stiggelbout et al., 1996); perhaps this was because they had no other options for maintaining current health. Balmer et al. (2001) found that patients choosing second-line chemotherapy were accepting of treatment involving toxicities and social disruption, even if it meant only gaining one to two months of survival time. Although it can only be speculated, patients who have experienced failed cancer treatment in the past may have lower expectations that cancer treatment will be effective and already understand the symptoms and side effects of treatments; therefore, they are willing to accept higher risk and lower benefit (Balmer et al., 2001). Alternately, once patients have failed to respond to one cancer treatment, they may believe a treatment that produces more symptoms and side effects is more effective to treat cancer and may be willing to suffer the negative consequences of treatment even if the benefit is unknown or low (Balmer et al., 2001).
In contrast, although some treatments, such as adjuvant endocrine therapy and tamoxifen, have shown the benefit of increased cancer-free survival in individuals with breast cancer, many do not adhere to their medication for the time prescribed, perhaps because of symptoms (Arriola et al., 2014; Pellegrini et al., 2010). Patients who weigh risks of treatment more heavily than benefits may decide not to initiate or adhere to treatment (Horne et al., 1999). Other studies have reported that individuals with cancer are more likely to discontinue treatment or report lower adherence intention if they had a negative decisional balance (higher risk than benefit) than those with positive decisional balance (higher benefit than risk) on the BMQ (Fink et al., 2004; Gatti, Jacobson, Gazmararian, Schmotzer, & Kripalani, 2009; Heisig et al., 2016; Moon, Moss-Morris, Hunter, Carlisle, & Hughes, 2017).
Misunderstanding the benefits and risks of treatment is critical because this analysis can negatively affect medication beliefs, initiation, or adherence to the cancer medication (Bickell et al., 2009; Bond et al., 2002). Beliefs about cancer medication and treatment outcomes can affect the treatment decisions of individuals with cancer (Tariman, Berry, Cochrane, Doorenbos, & Schepp, 2012). Providing patients with information they can understand assists them in the benefit–risk analysis of cancer treatment.
Adherence: Saratsiotou et al. (2011) reported that patients’ OCM beliefs were the most important factor associated with medication adherence, demonstrating that those with lower beliefs that the medication could treat the illness reported lower adherence, and those with greater beliefs in medication effectiveness reported higher adherence. Arriola et al. (2014) reported that higher BMQ necessity and lower concern beliefs were associated with medication adherence among individuals with breast cancer receiving adjuvant endocrine therapy. Individuals with breast cancer who felt that the benefits of tamoxifen therapy outweighed the risks had continued tamoxifen adherence, and those with either neutral or negative medication beliefs were more likely to stop tamoxifen (Fink et al., 2004; Grunfeld, Hunter, Sikka, & Mittal, 2005). Overall, patients with more positive medication perceptions are more likely to initiate and continue their cancer treatment compared to those with less positive medication perceptions (Banning, 2012; Neugut et al., 2012).
Symptoms and side effects: The number and type of symptoms and side effects from cancer or cancer treatment can vary across cancer and medication types (Thuné-Boyle et al., 2006). Symptoms are important to explore because they can lead to nonadherence or discontinuation of cancer treatment and decreased QOL (Corter, Findlay, Broom, Porter, & Petrie, 2013; Thuné-Boyle et al., 2006). A symptom is an experience of subjective disturbance, whereas a side effect is an undesirable result of a medication or treatment that also could present in the form of a symptom. Symptoms and side effects may be used to weigh whether patients adhere to cancer treatment because they may believe their symptoms outweigh the benefit of taking medication (Bender et al., 2014; Bhattacharya, Easthall, Willoughby, Small, & Watson, 2012; Gatti et al., 2009; Iskandarsyah et al., 2014). Patients experiencing side effects with cancer medication report higher concerns compared to those with no side effects (Salgado et al., 2017).
Cancer medication treatments are unique in that they often result in more symptoms than the illness itself (Thuné-Boyle et al., 2006), leaving individuals with cancer susceptible to negative cancer medication beliefs. Patients with chronic myeloid leukemia (CML) receiving imatinib noted side effects as the main concern of cancer treatment (Chen, Chen, Huang, & Chang, 2014). Patients may begin to weigh the risk of severe symptoms and side effects with the benefit of cancer treatment to slow disease progression or prolong survival (Jansen et al., 2005). Individuals with cancer may find it difficult to take a medication that makes them feel worse than before they began taking medication (Horne, 2003). Partridge et al. (2015) reported that individuals with breast cancer who were told they were randomized to receive bevacizumab versus a placebo (in addition to standard treatment) perceived a significantly higher risk of having a serious problem caused by the cancer treatment, indicating negative medication expectancies based on potential misconceptions surrounding the medication.
Research indicates that symptom experience may vary among individuals taking the same cancer medication, implying that nonpharmacologic factors influence symptoms (Thuné-Boyle et al., 2006). In addition, medication beliefs may affect the way patients experience symptoms (Corter et al., 2013) by biasing internal (somatic sensation) or external (physician counseling) information. This phenomenon has not been well explored for patients receiving cancer medications. For example, patients who have endured symptoms as a result of prior cancer treatments or other chronic conditions may develop negative medication beliefs or anticipate symptoms as a result of past medication experiences (Barsky, Saintfort, Rogers, & Borus, 2002; Heller, Chapman, & Horne, 2015). Patients with these negative medication experiences may be biased to focus attention on bodily sensations that they assume are from the medication or may bias information they receive regarding their cancer medication, while consciously or unconsciously blocking out positive aspects of medication.
In contrast, patients who have compromised physical functioning from symptoms of their cancer may perceive a greater need for their cancer medication (Llewellyn, McGurk, & Weinman, 2006). In addition, patients with symptoms of the cancer itself may have relief once starting treatment. One study revealed that patients with CML were satisfied with the way imatinib relieved disease-related fatigue and allowed them to resume normal activities of daily living (Chen et al., 2014). However, patients also may perceive symptoms as further disease progression, which can negatively affect perceived medication efficacy (Chen et al., 2014). Symptoms and side effects can play a dynamic role in the way illness representations are formed and medications are perceived.
Patient–provider relationship: The patient–provider relationship can influence medication perceptions. Arriola et al. (2014) found that more frequent physician communication was associated with greater cancer medication necessity beliefs among individuals with breast cancer. However, Iskandarsyah et al. (2014) reported that patients may feel inferior to physicians and do not question the cancer treatment plan out of respect or to avoid conflict. Others place trust in and rely on physicians who are trained in cancer care to make treatment decisions (Carrion, Nedjat-Haiem, & Marquez, 2013). A study of individuals with breast cancer noted that the healthcare provider’s recommendation about hormone replacement therapy was important and even swayed their treatment decisions, despite previously held beliefs about medication (Bond et al., 2002), which indicates that medication beliefs can be influenced by providers.
Previous experiences: Medication beliefs can be influenced by prior experiences with health, illness, and medications (Iskandarsyah et al., 2014). One study of individuals with breast cancer described women developing fatalistic beliefs of cancer based on the experiences of their family or friends (Iskandarsyah et al., 2014). Some studies have shown that prior exposure to chemotherapy influences a patient’s perceptions of treatment (Jansen et al., 2005; Jansen, Otten, & Stiggelbout, 2004). For example, patients who have gone through infusion chemotherapy tend to be more favorable toward treatment than those who have never had chemotherapy (Jansen et al., 2005). Bickell et al. (2009) found that women with breast cancer who were untreated were less likely to know the benefits of adjuvant treatment and had more negative treatment beliefs compared to patients who had been treated previously. Having experience with cancer also may give patients a more realistic, positive perception of cancer or its treatment (Del Castillo, Godoy-Izquierdo, Vásquez, & Godoy, 2011). Cognitive reappraisals of cancer and cancer treatment may lead to more positive cancer medication beliefs (Jansen et al., 2005) after symptoms of cancer are relieved or disease progression is slowed as a result of cancer medication.
In contrast, those with negative experiences of cancer, such as seeing a loved one suffer or experiencing a medication interruption themselves, may have more negative cancer medication perceptions (Del Castillo et al., 2011). Patients taking aromatase inhibitors (AIs) who had to stop treatment with another AI reported higher medication concern beliefs compared to those who had never experienced a stoppage (Salgado et al., 2017). Previous experiences with health, illness, and medication are individualized and should be reviewed with patients prior to initiation of treatment to clarify misconceptions about cancer medication and to promote positive medication beliefs.
Cancer treatment context: When examining medication beliefs, the context or intended goal of cancer treatment is important to consider. Patients with various cancer stages and prognoses may view cancer medications differently. One treatment may be curative, and the other may be palliative; this can shape different expectations and perceptions of cancer treatment. For example, Heisig et al. (2016) reported that a lower stage of cancer was associated with greater medication concern compared to medication necessity beliefs. Chen et al. (2013) found that 64% of 384 patients diagnosed with incurable lung cancer had an unrealistic belief that radiation therapy would treat their cancer or extend life expectancy, and they revealed that 92% of these patients were significantly more likely to hold the same inaccurate beliefs about chemotherapy. These results indicate a gap in patients’ understanding of their prognosis and various treatment options (Chen et al., 2013). Medication beliefs are intertwined with an individual’s illness representations. Patients must understand their cancer diagnosis and prognosis; otherwise, medication beliefs can develop based on misconceptions.
For patients with metastatic cancer, treatment choices can be supported by a patient’s medication beliefs (Koedoot et al., 2003). By examining beliefs about continuing treatment despite challenges of side effects, poor QOL, and the possibility that cancer treatment would be ineffective in treating the cancer, one study reported that life-prolonging treatment was more frequently sought over comfort if survival was predicted to be more than six months (Stiggelbout et al., 1996). Another study revealed that individuals newly diagnosed with cancer were more likely to prefer life-prolonging treatment than those who had experienced cancer longer, which may indicate a change in treatment beliefs across the cancer treatment trajectory (Balmer et al., 2001; Voogt et al., 2005). However, Voogt et al. (2005) reported that patients diagnosed with fatal cancer (less than six-month life expectancy) expressed a decline in striving for length of life with prolonged treatment, and QOL tended to be more important as imminent death was near. Findings suggest that a patient’s medication beliefs can change over time, underscoring the importance of assessing medication beliefs more than once (Voogt et al., 2005). However, research examining how medication beliefs change over time and factors influencing these changes is limited.
Fear of recurrence: Fear of cancer recurrence can affect how patients perceive their treatment. Bond et al. (2002) noted that cancer treatment beliefs are not a straightforward cognitive process but rather are influenced by emotions, such as fear (Bond et al., 2002). Two studies reported that greater fear of recurrence was associated with higher medication concern beliefs and higher medication necessity beliefs (Corter et al., 2013; Salgado et al., 2017). Corter et al. (2013) indicated that individuals with breast cancer taking adjuvant endocrine therapy may weigh the belief that they need the medication to protect them from cancer recurrence with the concern that the medication may not treat their cancer. The preceding statement is difficult to understand, given that the BMQ was used to elicit medication beliefs and that the concerns subscale measures distrust in medications, not treatment efficacy. Barak, Ostrowsky, and Kreitler (2012) described patients placing preventing cancer recurrence in the future as a main goal of adjuvant therapy, perhaps indicating that the fear of recurrence may motivate them to adhere to the treatment and increase medication necessity beliefs. Fear of recurrence appears to have positive and negative effects on patients’ cancer medication beliefs, possibly because fear of recurrence can motivate patients to take their medication based on necessity or symptoms associated with cancer, or because symptoms or side effects caused by the medication can be interpreted as recurring disease.
Information and education: Information regarding medication or treatment options can activate medication beliefs by way of cognitive processing. Information is essential to facilitating patient understanding of the disease process and treatment because it allows patients to weigh the benefits and risks of treatment options or no treatment (Barak et al., 2012; Bickell et al., 2009). Without proper knowledge regarding disease and treatment options, patients may develop beliefs based on misconceptions, which can negatively affect patient outcomes (Chen et al., 2013).
Some patients may have unrealistic or inaccurate beliefs about their cancer prognosis with treatment (Chen et al., 2013). Those with misconceptions about the disease progression itself may not trust that cancer medication can result in remission (Chen et al., 2014). Satisfaction with the type and timing of information was associated with stronger medication necessity beliefs among individuals with head and neck cancer (Llewellyn, McGurk, & Weinman, 2007a). In contrast, Bhattacharya et al. (2012) found no association between patients’ medication necessity beliefs and satisfaction with the information about medication.
Bhattacharya et al. (2012) noted that patients taking capecitabine expressed gaps in knowledge regarding when the medication would take effect and how they could know whether the treatment was working. Patients may rely on diagnostic testing, such as computerized tomography scans or laboratory testing, for confirmation of the medication’s efficacy. For patients with CML, a rapid drop in white blood cell counts below the normal range post-treatment resulted in the belief that imatinib was efficacious to control cancer (Chen et al., 2014).
Some patients may think their cancer is incurable (Iskandarsyah et al., 2014) or that long-term OCM use could cause resistance to the medication (Chen et al., 2014); these thoughts also can affect medication beliefs. Cancer medication often does not show immediate improvement in health, unlike medications for other chronic illnesses. Education is essential at treatment initiation to explain medication expectations and the plan for testing throughout the cancer trajectory. Oncology professionals must clarify medication misconceptions to form and support favorable medication beliefs.
Coping and depression: Coping among individuals with cancer is associated with medication beliefs. In a study of individuals with head and neck cancer, baseline BMQ concerns were significantly positively associated with positive and negative coping strategies, such as self-distraction, venting, planning, denial, substance use, use of instrumental support, and behavioral disengagement one month after treatment for head and neck cancer (Llewellyn et al., 2007a). Baseline BMQ necessity was significantly positively associated with active coping, positive reframing, substance use, and planning (Llewellyn et al., 2007a); however, these associations declined during a six- to eight-month period after treatment (Llewellyn et al., 2007a). Similar results have been reported (Llewellyn, McGurk & Weinman, 2007b). Findings imply that more positive medication beliefs are associated with more adaptive coping, and medication concerns are linked to more maladaptive coping strategies. Only one study linked depression to cancer medication beliefs, associating self-reported depression with higher medication concern beliefs compared to those with no depression (Salgado et al., 2017).
Demographic factors: Reporting of sociocultural factors that can influence cancer medication beliefs is inconsistent (Bickell et al., 2009; Chen et al., 2013; Jonnalagadda et al., 2012; Nedjat-Haiem, Lorenz, Ell, Hamilton, & Palinkas, 2012). Voogt et al. (2005) reported that cancer treatment beliefs did not differ among sex, education, or cancer type. In addition, Bickell et al. (2009) observed that older age and presence of comorbidities accounted for lower use of adjuvant therapies, indicating that patients who have prior experience with illness and who are older may develop more medication concerns. Bond et al. (2002) found that younger women expressed more concern about their survival and QOL, whereas older women worried more about comorbid conditions other than cancer. Salgado et al. (2017) reported that women aged older than 70 years had lower medication necessity and concern beliefs compared to those aged younger than 70 years. The relationship between medication beliefs and patient sociodemographic factors remains inconclusive.
Discussion
Medication beliefs among individuals with cancer are multifaceted and are encompassed within a larger context of cancer illness representation. Understanding medication beliefs among individuals with cancer is in its infancy stage, and more rigorous measures are needed in research studies to elicit such beliefs. The BMQ provides a way to quantify medication beliefs among individuals with cancer, but studies fail to perform factor analysis to determine if the original underlying constructs hold in this population. The BMQ allows for statistically associating factors with medication beliefs and is a viable option for eliciting medication beliefs among individuals with cancer.
Another measure that most commonly quantified medication beliefs among individuals with cancer was the QQ Questionnaire. Use of this questionnaire in cancer research permits the awareness of possible differences in cancer treatment preferences among younger and older patients, with younger patients striving for quantity of life and older patients striving for QOL. More research using the BMQ and QQ Questionnaire is needed, particularly regarding examining medication beliefs among patients receiving OCM and in longitudinal studies across the cancer treatment trajectory. Research involving established instruments can inform interventions that can improve positive medication beliefs and decrease medication concerns to maintain adherence among patients who manage their cancer medication in the home environment.
Information is essential for patients to fully understand their illness and medication and treatment options (Barak et al., 2012; Pellegrini et al., 2010). The interplay between medication beliefs and symptoms needs further investigation, because negative medication expectancies can affect the way in which symptoms are experienced (Faasse & Petrie, 2013; Thuné-Boyle et al., 2006). Symptoms also play a large role in the benefit–risk analysis when making decisions about initiating or continuing cancer medication or treatment (Bickell et al., 2009). Cancer symptoms can increase patients’ perceptions that medication is needed to treat their illness, whereas symptoms experienced after initiation of cancer medication can negatively affect medication perceptions. Demographic variables associated with medication beliefs are inconclusive. Understanding medication beliefs among individuals with cancer may lead to important key factors affecting symptom management and adherence to cancer medication. As more OCMs are being offered and patients are required to self-manage complex regimens and symptoms in the home environment, medication beliefs may be a crucial factor associated with patient outcomes.
Overall, studies have presented a variety of factors associated with medication beliefs among patients receiving cancer treatment, including benefit–risk analysis; adherence; symptoms and side effects; patient–provider relationships; prior exposure to health, illness, and medications; cancer treatment characteristics; fear of recurrence; information regarding the diagnosis or cancer treatment; coping; and demographics. Despite the increased use of oral oncolytic agents, these medications were not well represented in the review. However, cancer medication, regardless of type or drug classification, appears to be associated with similar factors. More systematic reviews are focusing on medication beliefs specific to oral adherence (Lin, Clark, Tu, Bosworth, & Zullig, 2017; Moon et al., 2017). Research is slowly beginning to evaluate more factors that could be associated with medication beliefs beyond adherence. For example, research surrounding medication beliefs involves studies that explore negative medication expectancies and their role in the development of medication beliefs (Faasse & Petrie, 2013; Heller et al., 2015), the examination of medication beliefs and their link to the cancer-related symptom experience (Corter et al., 2013), depression (Salgado et al., 2017), and the importance of patient education in the formulation of cancer medication beliefs (Chen et al., 2013; Llewellyn et al., 2007a).
Limitations
The current integrative review has limitations. Some studies assessed medication perceptions among individuals with cancer before initiating treatment, and others had been exposed to treatment, making comparing results difficult. Perceptions about cancer treatment were measured by various means, often using newly developed questionnaires, making comparing studies challenging. Factor analysis was lacking for articles using the BMQ to measure medication beliefs in the cancer population, which was not represented during the original psychometric testing of the scale (Horne et al., 1999); the original psychometric evaluation of the BMQ revealed that only 3 of 524 patients had a cancer diagnosis. Some studies used newly developed questionnaires that failed to report reliability and validity testing. Other studies combined the use of chemotherapy with other cancer treatment, such as radiation therapy or surgery, making differentiating results problematic. In addition, some studies were based on hypothetical scenarios in which individuals with cancer were questioned about treatment choices based on imaginary situations involving chemotherapy rather than actual experiences (Hirose et al., 2009). Targeted oral oncolytic agents were not well represented, perhaps because of the rise in use of these medications or the assumption by oncology professionals that patients receiving OCMs are mostly adherent.
Implications for Nursing Practice
Nurses are positioned to elicit cancer medication beliefs. Reliable and valid measurements, such as the BMQ, can be used to help elicit such beliefs in the clinical setting (Horne et al., 1999). The OCM trend is increasing (Moseley & Nystrom, 2009), and nurses must be aware of factors influencing medication beliefs and clarify misconceptions to promote facilitative medication beliefs. Medication beliefs can change over time and should be addressed regularly, particularly when changes in a patient’s prognosis, treatment plan, or assessment of symptoms are noted. Nurses should be aware that medication beliefs can influence medication-taking behavior and are closely linked with adherence (Arriola et al., 2014; Lin et al., 2017; Moon et al., 2017; Saratsiotou et al., 2011). Depression also should be carefully evaluated because it can negatively affect medication beliefs and heighten concern for taking cancer medication (Salgado et al., 2017). Nurses are at the forefront of patient education and can provide trusted oncology resources regarding a patient’s cancer treatment. Patient education is critical in the development of medication beliefs and can help patients weigh the benefits and risks of cancer treatment (Barak et al., 2012; Bickell et al., 2009). 
Conclusion
Additional research is needed to better understand how medication beliefs may lead to an exacerbated symptom experience, via negative medication expectancies, and to test interventions that can improve medication beliefs, specifically targeting patients starting a new treatment regimen. Research using reliable and valid measurement tools to elicit medication beliefs among individuals with cancer is needed. Factor analysis on reliable and valid tools, such as the BMQ, is needed to determine if latent factors underlying medication beliefs among individuals with cancer differ from other chronic illnesses. More research specific to OCM beliefs is needed as well.
[[{"fid":"43516","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"height":310,"width":626,"class":"media-element file-default","data-delta":"1"}}]]
About the Author(s)
Victoria K. Marshall, PhD, RN, is a graduate and Barbara A. Given, PhD, RN, FAAN, is a distinguished professor, both in the College of Nursing at Michigan State University in East Lansing. No financial relationships to disclose. Marshall completed the data collection and contributed to the manuscript preparation. Given provided statistical support. Both authors contributed to the conceptualization and design and provided the analysis. Marshall can be reached at marsh421@msu.edu, with copy to ONFEditor@ons.org. (Submitted November 2017. Accepted February 7, 2018.)
References
Arriola, J.K.R., Mason, T.A., Bannon, K.A., Holmes, C., Powell, C.L., Horne, K., & O’Regan, R. (2014). Modifiable risk factors for adherence to adjuvant endocrine therapy among breast cancer patients. Patient Education and Counseling, 95, 98–103. https://doi.org/10.1016/j.pec.2013.12.019
Balmer, C.E., Thomas, P., & Osborne, R.J. (2001). Who wants second-line, palliative chemotherapy? Psycho-Oncology, 10, 410–418.
Banning, M. (2012). Adherence to adjuvant therapy in post-menopausal breast cancer patients: A review. European Journal of Cancer Care, 21, 10–19. https://doi.org/10.1111/j.1365-2354.2011.01295.x
Barak, F., Ostrowsky, L.A., & Kreitler, S. (2012). Adjuvant chemotherapy for breast cancer patients: Patients’ expectations and physicians’ attitudes. Palliative and Supportive Care, 10, 107–114. https://doi.org/10.1017/S1478951511000733
Barsky, A.J., Saintfort, R., Rogers, M.P., & Borus, J.F. (2002). Nonspecific medication side effects and the nocebo phenomenon. JAMA, 287, 622–627.
Bender, C.M., Gentry, A.L., Brufsky, A.M., Casillo, F.E., Cohen, S.M., Dailey, M.M., . . . Sereika, S.M. (2014). Influence of patient and treatment factors on adherence to adjuvant endocrine therapy in breast cancer. Oncology Nursing Forum, 41, 274–285. https://doi.org/10.1188/14.ONF.274-285
Bhattacharya, D., Easthall, C., Willoughby, K.A., Small, M., & Watson, S. (2012). Capecitabine non-adherence: Exploration of magnitude, nature and contributing factors. Journal of Oncology Pharmacy Practice, 18, 333–342. https://doi.org/10.1177/1078155211436022
Bickell, N.A., Weidmann, J., Fei, K., Lin, J.J., & Leventhal, H. (2009). Underuse of breast cancer adjuvant treatment: Patient knowledge, beliefs, and medical mistrust. Journal of Clinical Oncology, 27, 5160–5167. https://doi.org/10.1200/JCO.2009.22.9773
Bond, B., Hirota, L., Fortin, J., & Col, N. (2002). Women like me: Reflections on health and hormones from women treated for breast cancer. Journal of Psychosocial Oncology, 20(3), 39–56. https://doi.org/10.1300/J077v20n03_03
Carrion, I.V., Nedjat-Haiem, F.R., & Marquez, D.X. (2013). Examining cultural factors that influence treatment decisions: A pilot study of Latino men with cancer. Journal of Cancer Education, 28, 729–737. https://doi.org/10.1007/s13187-013-0522-9
Center Watch. (2018). FDA approved drugs for oncology. Retrieved from https://www.centerwatch.com/drug-information/fda-approved-drugs/therape…
Chater, A.M., Parham, R., Riley, S., Hutchison, A.J., & Horne, R. (2014). Profiling patient attitudes to phosphate binding medication: A route to personalising treatment and adherence support. Psychology and Health, 29, 1407–1420. https://doi.org/10.1080/08870446.2014.942663
Chen, A.B., Cronin, A., Weeks, J.C., Chrischilles, E.A., Malin, J., Hayman, J.A., & Schrag, D. (2013). Expectations about the effectiveness of radiation therapy among patients with incurable lung cancer. Journal of Clinical Oncology, 31, 2730–2735. https://doi.org/10.1200/JCO.2012.48.5748
Chen, L.C., Chen, T.C., Huang, Y.B., & Chang, C.S. (2014). Disease acceptance and adherence to imatinib in Taiwanese chronic myeloid leukaemia outpatients. International Journal of Clinical Pharmacy, 36, 120–127. https://doi.org/10.1007/s11096-013-9867-8
Corter, A.L., Findlay, M., Broom, R., Porter, D., & Petrie, K.J. (2013). Beliefs about medicine and illness are associated with fear of cancer recurrence in women taking adjuvant endocrine therapy for breast cancer. British Journal of Health Psychology, 18, 168–181. https://doi.org/10.1111/bjhp.12003
Del Castillo, A., Godoy-Izquierdo, D., Vázquez, M.L., & Godoy, J.F. (2011). Illness beliefs about cancer among healthy adults who have and have not lived with cancer patients. International Journal of Behavioral Medicine, 18, 342–351. https://doi.org/10.1007/s12529-010-9141-6
Duric, V.M., Butow, P.N., Sharpe, L., Heritier, S., Boyle, F., Beith, J., . . . Stockler, M.R. (2008). Comparing patients’ and their partners’ preferences for adjuvant chemotherapy in early breast cancer. Patient Education and Counseling, 72, 239–245. https://doi.org/10.1016/j.pec.2008.02.021
Faasse, K., & Petrie, K.J. (2013). The nocebo effect: Patient expectations and medication side effects. Postgraduate Medical Journal, 89, 540–546. https://doi.org/10.1136/postgradmedj-2012-131730
Fink, A.K., Gurwitz, J., Rakowski, W., Guadagnoli, E., & Silliman, R.A. (2004). Patient beliefs and tamoxifen discontinuance in older women with estrogen receptor–positive breast cancer. Journal of Clinical Oncology, 22, 3309–3315. https://doi.org/10.1200/JCO.2004.11.064
Gatti, M.E., Jacobson, K.L., Gazmararian, J.A., Schmotzer, B., & Kripalani, S. (2009). Relationships between beliefs about medications and adherence. American Journal of Health-System Pharmacy, 66, 657–664. https://doi.org/10.2146/ajhp080064
Given, B.A., Spoelstra, S.L., & Grant, M. (2011). The challenges of oral agents as antineoplastic treatments. Seminars in Oncology Nursing, 27, 93–103. https://doi.org/10.1016/j.soncn.2011.02.003
Grunfeld, E.A., Hunter, M.S., Sikka, P., & Mittal, S. (2005). Adherence beliefs among breast cancer patients taking tamoxifen. Patient Education and Counseling, 59, 97–102. https://doi.org/10.1016/j.pec.2004.10.005
Heisig, S.R., Shedden-Mora, M.C., von Blanckenburg, P., Rief, W., Witzel, I., Albert, U.S., & Nestoriuc, Y. (2016). What do women with breast cancer expect from their treatment? Correlates of negative treatment expectations about endocrine therapy. Psycho-Oncology, 25, 1485–1492. https://doi.org/10.1002/pon.4089
Heller, M.K., Chapman, S.C., & Horne, R. (2015). Beliefs about medication predict the misattribution of a common symptom as a medication side effect—Evidence from an analogue online study. Journal of Psychosomatic Research, 79, 519–529. https://doi.org/10.1016/j.jpsychores.2015.10.003
Hirose, T., Yamaoka, T., Ohnishi, T., Sugiyama, T., Kusumoto, S., Shirai, T., . . . Adachi, M. (2009). Patient willingness to undergo chemotherapy and thoracic radiotherapy for locally advanced non-small cell lung cancer. Psycho-Oncology, 18, 483–489.
Horne, R. (2003). Treatment perceptions and self-regulation. In L.D. Cameron, & H. Leventhal (Eds.), The self-regulation of health and illness behaviour (pp. 138–153). New York, NY: Routledge.
Horne, R., Weinman, J., & Hankins, M. (1999). The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychology and Health, 14, 1–24. https://doi.org/10.1080/08870449908407311
Iskandarsyah, A., de Klerk, C., Suardi, D.R., Soemitro, M.P., Sadarjoen, S.S., & Passchier, J. (2014). Psychosocial and cultural reasons for delay in seeking help and nonadherence to treatment in Indonesian women with breast cancer: A qualitative study. Health Psychology, 33, 214–221. https://doi.org/10.1037/a0031060
Jansen, S.J., Otten, W., Baas-Thijssen, M.C., van de Velde, C.J., Nortier, J.W., & Stiggelbout, A.M. (2005). Explaining differences in attitude toward adjuvant chemotherapy between experienced and inexperienced breast cancer patients. Journal of Clinical Oncology, 23, 6623–6630. https://doi.org/10.1200/JCO.2005.07.171
Jansen, S.J., Otten, W., & Stiggelbout, A.M. (2004). Review of determinants of patients’ preferences for adjuvant therapy in cancer. Journal of Clinical Oncology, 22, 3181–3190. https://doi.org/10.1200/JCO.2004.06.109
Jonnalagadda, S., Lin, J.J., Nelson, J.E., Powell, C.A., Salazar-Schicchi, J., Berman, A.R., . . . Wisnivesky, J.P. (2012). Racial and ethnic differences in beliefs about lung cancer care. Chest, 142, 1251–1258. https://doi.org/10.1378/chest.12-0330
Kalichman, S., Kalichman, M.O., & Cherry, C. (2016). Medication beliefs and structural barriers to treatment adherence among people living with HIV infection. Psychology and Health, 31, 383–395. https://doi.org/10.1080/08870446.2015.1111371
Koedoot, C.G., de Haan, R.J., Stiggelbout, A.M., Stalmeier, P.F., de Graeff, A., Bakker, P.J., & de Haes, J.C. (2003). Palliative chemotherapy or best supportive care? A prospective study explaining patients’ treatment preference and choice. British Journal of Cancer, 89, 2219–2226. https://doi.org/10.1038/sj.bjc.6601445
Lin, C., Clark, R., Tu, P., Bosworth, H.B., & Zullig, L.L. (2017). Breast cancer oral anti-cancer medication adherence: A systematic review of psychosocial motivators and barriers. Breast Cancer Research and Treatment, 165, 247–260. https://doi.org/10.1007/s10549-017-4317-2
Llewellyn, C.D., McGurk, M., & Weinman, J. (2006). Head and neck cancer: To what extent can psychological factors explain differences between health-related quality of life and individual quality of life? British Journal of Oral and Maxillofacial Surgery, 44, 351–357. https://doi.org/10.1016/j.bjoms.2005.06.033
Llewellyn, C.D., McGurk, M., & Weinman, J. (2007a). Illness and treatment beliefs in head and neck cancer: Is Leventhal’s common sense model a useful framework for determining changes in outcomes over time? Journal of Psychosomatic Research, 63, 17–26. https://doi.org/10.1016/j.jpsychores.2007.01.013
Llewellyn, C.D., McGurk, M., & Weinman, J. (2007b). The relationship between the Patient Generated Index (PGI) and measures of HR-QoL following diagnosis with head and neck cancer: Are illness and treatment perceptions determinants of judgment-based outcomes? British Journal of Health Psychology, 12, 421–437.
Lu, Y., Arthur, D., Hu, L., Cheng, G., An, F., & Li, Z. (2016). Beliefs about antidepressant medication and associated adherence among older Chinese patients with major depression: A cross-sectional survey. International Journal of Mental Health Nursing, 25, 71–79. https://doi.org/10.1111/inm.12181
Mancini, R., McBride, A., & Kruczynski, M. (2013). Oral oncolytics: Part 1—Financial, adherence, and management challenges. Oncology, 27, 742–744.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D.G. (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLOS Medicine, 6(6), e1000097. https://doi.org/10.1371/journal.pmed.1000097
Moon, Z., Moss-Morris, R., Hunter, M.S., Carlisle, S., & Hughes, L.D. (2017). Barriers and facilitators of adjuvant hormone therapy adherence and persistence in women with breast cancer: A systematic review. Patient Preference and Adherence, 11, 305–322. https://doi.org/10.2147/PPA.S126651
Moseley, W.G., & Nystrom, J.S. (2009). Dispensing oral medications: Why now and how? Community Oncology, 6, 358–361. https://doi.org/10.1016/S1548-5315(11)70259-5
National Comprehensive Care Network. (n.d.). Managing cancer as a chronic condition. Retrieved from http://www.nccn.org/patients/resources/life_after_cancer/managing.aspx
Nedjat-Haiem, F.R., Lorenz, K.A., Ell, K., Hamilton, A., & Palinkas, L. (2012). Experiences with advanced cancer among Latinas in a public health care system. Journal of Pain and Symptom Management, 43, 1013–1024. https://doi.org/10.1016/j.jpainsymman.2011.06.018
Neugut, A.I., Hillyer, G.C., Kushi, L.H., Lamerato, L., Leoce, N., Nathanson, S.D., . . . Hershman, D.L. (2012). Noninitiation of adjuvant chemotherapy in women with localized breast cancer: The breast cancer quality of care study. Journal of Clinical Oncology, 30, 3800–3809. https://doi.org/10.1200/JCO.2012.43.8168
Neuss, M.N., Polovich, M., McNiff, K., Esper, P., Gilmore, T.R., LeFebvre, K.B., . . . Jacobson, J.O. (2013). 2013 updated American Society of Clinical Oncology/Oncology Nursing Society chemotherapy administration safety standards including standards for the safe administration and management of oral chemotherapy. Oncology Nursing Forum, 40, 225–233. https://doi.org/10.1188/13.ONF.40-03AP2
Partridge, A.H., Sepucha, K., O’Neill, A., Miller, K.D., Motley, C., Swaby, R.F., . . . Sledge, G.W., Jr. (2015). Effect of unblinding on participants’ perceptions of risk and confidence in a large double-blind clinical trial of chemotherapy for breast cancer. JAMA Oncology, 1, 369–374. https://doi.org/10.1001/jamaoncol.2015.0246
Pellegrini, I., Sarradon-Eck, A., Soussan, P.B., Lacour, A.C., Largillier, R., Tallet, A., . . . Julian-Reynier, C. (2010). Women’s perceptions and experience of adjuvant tamoxifen therapy account for their adherence: Breast cancer patients’ point of view. Psycho-Oncology, 19, 472–479. https://doi.org/10.1002/pon.1593
Salgado, T.M., Davis, E.J., Farris, K.B., Fawaz, S., Batra, P., & Henry, N.L. (2017). Identifying socio-demographic and clinical characteristics associated with medication beliefs about aromatase inhibitors among postmenopausal women with breast cancer. Breast Cancer Research and Treatment, 163, 311–319. https://doi.org/10.1007/s10549-017-4177-9
Saratsiotou, I., Kordoni, M., Bakogiannis, C., Livadarou, E., Skarlos, D., Kosmidis, P.A., & Razis, E. (2011). Treatment adherence of cancer patients to orally administered chemotherapy: Insights from a Greek study using a self-reported questionnaire. Journal of Oncology Pharmacy Practice, 17, 304–311. https://doi.org/10.1177/1078155210380292
Stiggelbout, A.M., De Haes, J.C. Kiebert, G.M., Kievit, J., & Leer, J.W. (1996). Tradeoffs between quality and quantity of life: Development of the QQ questionnaire for cancer patient attitudes. Medical Decision Making, 16, 184–192. https://doi.org/10.1177/0272989X9601600211
Tariman, J.D., Berry, D.L., Cochrane, B., Doorenbos, A., & Schepp, K.G. (2012). Physician, patient, and contextual factors affecting treatment decisions in older adults with cancer and models of decision making: A literature review [Online exclusive]. Oncology Nursing Forum, 39, E70–E83. https://doi.org/10.1188/12.ONF.E70-E83
Thuné-Boyle, I.C., Myers, L.B., & Newman, S.P. (2006). The role of illness beliefs, treatment beliefs, and perceived severity of symptoms in explaining distress in cancer patients during chemotherapy treatment. Behavioral Medicine, 32, 19–29. https://doi.org/10.3200/BMED.32.1.19-29
Vioral, A., Leslie, M., Best, R., & Somerville, D. (2014). Patient adherence with oral oncolytic therapies. Seminars in Oncology Nursing, 30, 190–199. https://doi.org/10.1016/j.soncn.2014.05.007
Voogt, E., van der Heide, A., Rietjens, J.A., van Leeuwen, A.F., Visser, A.P., van der Rijt, C.C., & van der Maas, P.J. (2005). Attitudes of patients with incurable cancer toward medical treatment in the last phase of life. Journal of Clinical Oncology, 23, 2012–2019. https://doi.org/10.1200/JCO.2005.07.104
Whittemore, R., & Knafl, K. (2005). The integrative review: Updated methodology. Journal of Advanced Nursing, 52, 546–553. https://doi.org/10.1111/j.1365-2648.2005.03621.x




