Analysis of Age-Friendly Cancer Care Readiness
Objectives: Cancer care attuned to meeting the needs of older adults is imperative to ensure that they receive appropriate levels of treatment in accordance with their goals of care. Achieving age-friendly systems and geriatric-competent workforces require rethinking current models of cancer care delivery. This article reports on a descriptive study on the readiness of U.S. cancer programs to provide age-friendly cancer care.
Sample & Setting: A survey was sent to 567 ambulatory oncology leaders in the United States. Of the 81 respondents, 61 answered all questions.
Methods & Variables: The authors developed and administered an online survey assessing cancer programs’ age-friendly cancer care practices and readiness. Survey questions were based on the elements of the 4Ms framework. Results were analyzed using frequencies and percentages for categorically measured survey items and measures of central tendency for continuously scaled survey items.
Results: 67% of respondents reported that their program could deliver age-friendly cancer care within five years. Respondents less frequently indicated that they employed specific 4Ms elements: medications (41%), mobility (32%), mentation (14%), and what matters (11%).
Implications for Nursing: The results of this study suggest gaps in readiness to implement age-friendly cancer care. Recommendations to improve readiness include increasing awareness, expanding workforce preparation, and improving cancer program leadership engagement.
Jump to a section
The National Cancer Institute estimates that there will be 26.1 million cancer survivors in the United States by 2040, with the majority of survivors being aged 60 years or older (Shapiro, 2018). Cancer survivorship in older adults creates unique challenges, including management of multimorbidity and long-term effects of treatment, transitions in care settings that may include long-term care facilities, and ensuring older adults are fully included in shared decision-making (Guerard et al., 2016; Mohile et al., 2016). Patients risk being over- or undertreated when their providers exclude assessments of frailty or only focus on patients’ chronologic age (Lawler et al., 2014). Care directly attuned to the needs of older adults with cancer is a critical need within cancer healthcare systems to ensure that older adults receive appropriate levels of treatment in accordance with their goals of care.
The World Health Organization (WHO, 2004) defines active and healthy aging as “the process of optimizing opportunities for health, participation, and security in order to enhance quality of life as people age” (p. iv). Age-friendly health care is defined as a continuum of care that anticipates needs and engages older adults and their families in healthcare planning. Age-friendly cancer care can be defined as a person-centered approach to cancer care that focuses on quality and safety, engaging the older adult in goal-concordant care. Age-friendly cancer care focuses on the patient’s goals and values, improved outcomes, lower costs of care, and improved quality of care (American Hospital Association [AHA], 2018; Kagan, 2015). This model appreciates that older adults are sometimes invisible in society—even in their own healthcare decisions—and strives to ensure that the entire healthcare system adequately focuses on their needs (Lawler et al., 2014; Williams-Robert et al., 2018; Yao et al., 2018). 
The John A. Hartford Foundation partnered with the Institute for Healthcare Improvement (IHI) to create the Age-Friendly Health Systems initiative, with a goal of developing a model for health systems to address the gaps in current care of older adults, which preserves patients’ dignity and encourages independence (AHA, 2018). Specifically, the initiative addresses the 4Ms framework: what matters, medication, mentation, and mobility (see Figure 1 and Table 1). The 4Ms framework proactively addresses the complex needs of older adults, including the prevention of harm, improvement of communication, attention to physical needs, engagement of family caregivers, and improvement of care (Fulmer et al., 2018). Addressing these needs in a systematic way can demonstrate improved outcomes in many areas of focus for cancer programs and health systems, including the patient experience, unplanned readmissions, symptom management, inpatient mortality, falls risk, and appropriate site of care. This model has been implemented sporadically in cancer care and infrequently in the ambulatory setting. Limiting the reach of age-friendly care to the inpatient setting prevents those individuals treated in the outpatient setting—in which most cancer care occurs—from experiencing the benefits of age-friendly care. 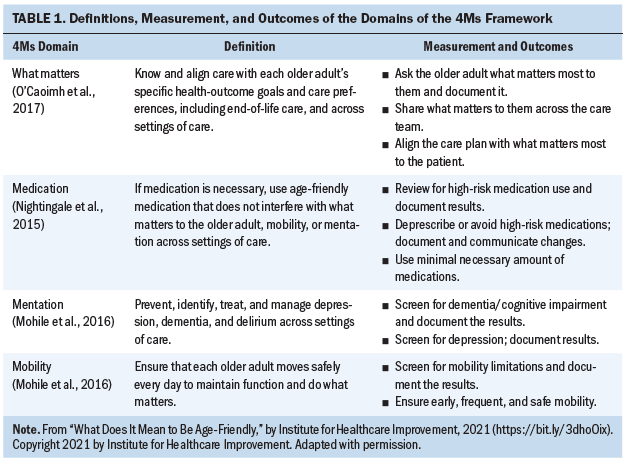
Since the 1990s, national and international organizations, such as the National Cancer Institute, the National Institute on Aging, the Oncology Nursing Society, and the International Society of Geriatric Oncology, have supported increased readiness for evidence-based care for older adults with cancer through position papers, focus groups, symposia, and educational programs. Despite these efforts, healthcare systems are not prepared to provide high-quality care for older adults with cancer. These organizations have called for oncology nursing, in partnership with colleagues in geriatric oncology, to provide leadership in advancing evidence-based care and promoting innovative change to enhance care for older adults with cancer (Bond et al., 2016; Bridges et al., 2016; Oncology Nursing Society, 2007). Oncology nursing faces challenges that include realignment of education, practice, and research to focus on demographic realities (Goldberg et al., 2018; Kagan, 2016). In the current study, the authors aim to identify opportunities to improve age-friendly readiness in U.S.-based cancer programs.
The majority of cancer care is delivered in the ambulatory setting; however, there is little description of age-friendly care in non-hospital settings. Many oncology nurses are also not prepared to offer age-friendly cancer care because basic nursing education programs provide limited content related to geriatrics. Much of the age-friendly literature focuses on creating age-friendly health systems (Chiou & Chen, 2009; Huang et al., 2011; Parke et al., 2014; Pearce et al., 2011), but there is little evidence regarding its application to cancer care delivery. To date, best practice models of workforce preparation to implement age-friendly cancer care are not well understood.
Identifying the current state of the readiness of the oncology workforce to provide age-friendly cancer care is an important next step in achieving the goal of age-friendly cancer care and developing recommendations for future directions. The purpose of this descriptive study was to develop and conduct a national survey of cancer program leaders to assess their readiness for age-friendly ambulatory cancer care, with the goal of developing recommendations to prepare for and implement age-friendly cancer care.
Methods
The authors developed a Qualtrics survey with cross-sectional design using Dillman’s tailored design method (Dillman et al., 2009), an evidence-based method for survey delivery. The 4Ms framework provided an outline from which to assess readiness (AHA, 2018; Fulmer et al., 2016). This self-developed survey was submitted to five experts in geriatric oncology for review and revision, as well as ethical review. The survey consisted of 24 items with a mix of multiple choice and open-ended questions. The authors estimated that most respondents would require about 10 to 15 minutes to complete the survey. Sample questions include the following:
• Is your program on track to deliver age-friendly care within the next five years?
• Is your workforce specifically educated/trained in the care of older adults?
• What do you consider the top barriers to age-friendly cancer care in your institution?
• How does your program engage the older adult as an active participant in their care?
• Approval to conduct the study was obtained from the Human Research Protection Office at the University of Pittsburgh in Pennsylvania.
Potential participants were recruited through the membership of professional organizations, including the Oncology Nursing Society, the Association of Community Cancer Centers, and nursing directors of National Cancer Institute–designated cancer programs. Although the age-friendly movement is international, this survey focused specifically on cancer programs in the United States. The survey was emailed to 567 ambulatory oncology leaders, including nursing directors, cancer program administrators, cancer service line directors, chief medical officers, practice administrators, and directors. The survey was open for 90 days. Email reminders were sent at 10 days and 30 days to those who did not complete the survey upon receipt. The survey results were analyzed using frequencies and percentages for categorically measured survey items and descriptive statistics for survey items answered with continuous measures.
Results
The survey achieved a 10.7% response rate with 81 participants; however, only 61 participants completed all questions. The majority of participants were nurse leaders (48%, n = 32), followed by cancer service line and program administrators (29%, n = 19). Survey participants’ roles are listed in Table 2. The largest setting of respondents was community cancer programs (43%, n = 29), followed by academic medical centers (21%, n = 14), NCI-designated cancer centers (19%, n = 13), and free-standing cancer centers (12%, n = 8). Fifty-two percent of respondents (n = 35) indicated that their patients traveled between 30 and 60 minutes, 37% (n = 25) traveled less than 30 minutes, and 10% (n = 7) traveled more than 60 minutes. 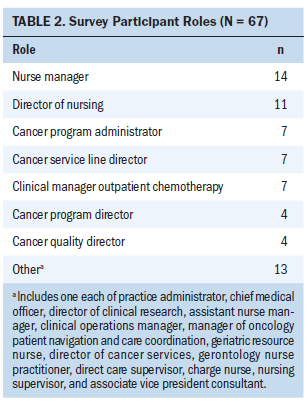
The primary question asked about their program’s readiness to deliver age-friendly cancer care within the next five years. Sixty-seven percent (n = 44) agreed that their program was on track, but responses to subsequent questions did not substantiate the assessment of readiness (see Table 3). Seventy-seven percent (n = 51) of respondents indicated that their workforce was not specifically trained or educated in the care of older adults. Table 4 lists geriatric education and training programs that were used by respondents. Respondents indicated that processes to measure the 4Ms were implemented as follows: medications (41%, n = 27), mobility (32%, n = 21), mentation (14%, n = 9), and what matters (11%, n = 7). Responses did not differ by role. 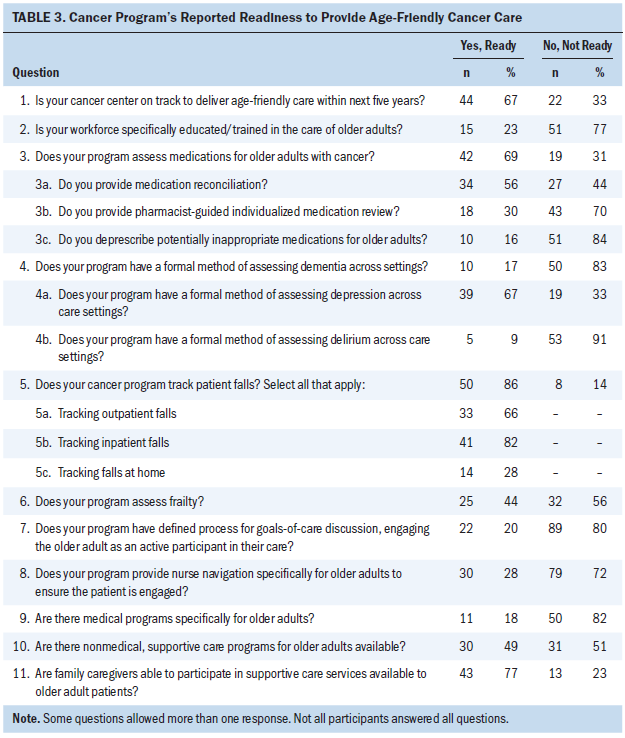
If the respondent reported that screening did occur, further questions assessed the type of screening. Medication reconciliation was reported as the most commonly used medication screening (56%, n = 34), followed by pharmacist-guided individualized medication review (30%, n = 18), and deprescribing of potentially inappropriate medications for older adults (16%, n = 10). Mentation was most frequently assessed through depression screening (67%, n = 39); however, delirium (9%, n = 5) and dementia (17%, n = 10) screening were rarely reported. Mobility can be measured through a frailty screening test, and 44% (n = 25) of programs were screening for frailty; however, falls tracking did not occur in all settings. Falls were most frequently measured in the inpatient setting (82%, n = 41), followed by the outpatient setting (66%, n = 33) and in the home (24%, n = 14). Falls were not tracked in 14% of programs (n = 8). 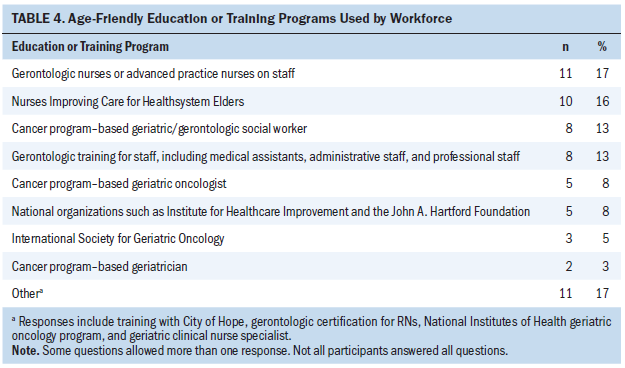
The authors assessed what matters readiness by reporting how the cancer program engaged the older adult as an active participant in his or her care. Responses included a defined process for goals-of-care discussions (20%, n = 22), referrals to supportive care programs (27%, n = 30), provision of nurse navigation to ensure patient is engaged (27%, n = 30), and provision of geriatric-specific nurse navigation (4%, n = 4). Twenty percent (n = 21) had no defined process to engage older adults in their care.
Respondents indicated that leadership engagement in age-friendly cancer care was limited. When asked about their perceptions of their cancer program leadership toward age-friendly cancer care, only 12% (n = 7) described their leadership as fully engaged. An equal percentage (26%, n = 15) of respondents indicated that their leadership was either unaware or they were aware but not yet engaged in age-friendly care. The highest percentage item related to leaders who were aware and partially engaged but focused on other priorities (36%, n = 21). Table 5 lists the perceived top barriers to age-friendly cancer care, which included financial burden, access to professionals with geriatric experience, workforce availability, and coordination of care among inpatient, outpatient, and home settings. 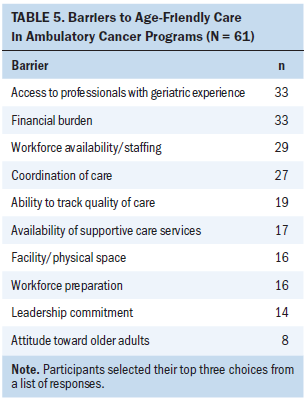
Discussion
The results of this survey are discordant, with the majority of program respondents reporting that they are on track to implement age-friendly cancer care in five years, but not reporting workforce preparation or processes to assess key elements of age-friendly care. Age-friendly cancer care is a critical need as healthcare providers prepare for and embrace healthy aging and strive for supportive, proactive approaches to the increasing number of older adult patients with cancer and survivors. This survey shows that most cancer programs are not prepared for this challenge. The primary issues identified by this descriptive study were readiness for age-friendly cancer care, low leadership engagement, and poor workforce preparation.
Workforce preparation is essential to ensuring age-friendly cancer care in the United States. Existing training programs, such as the American Geriatric Society’s Hospital Elder Life Program (HELP) and Nurses Improving Care for Healthsystem Elders (NICHE), have improved care for hospitalized older adults, but training programs focused on outpatient and home care must be developed and disseminated, with a focus on competency verification for all levels of staff and providers. Use of an evidence-based framework, such as the 4Ms, can guide the content and structure of novel workforce training. Engaging older adults and their families through programs, such as the Serious Illness Care Program (Paladino et al., 2019) and Vital Talk (www.vitaltalk.org), offers initial training in assessing the what matters domain of the 4Ms framework, helping to engage them as partners in their care. Additional research and evidence-based practice to develop best practices for the other aspects of the framework, including medication assessment, frailty screening, and cognitive screening, are needed. Figure 2 lists age-friendly resources for nurses. 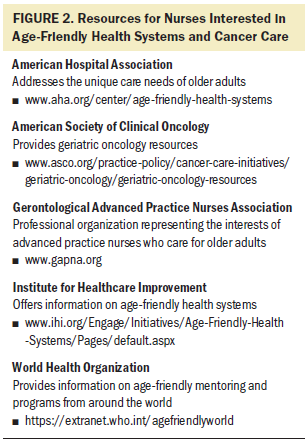
Financial burden was cited as one of the top barriers for age-friendly program development. Identifying the specific dimensions, such as a patient-related financial burden or, more likely, an institutional burden from competing operating and capital budget initiatives, is essential to advancing age-friendly cancer care. Other issues that program leaders can address include age-friendly facilities, as physical space was noted as a barrier. The lack of accessible entrances and restrooms, particularly in older buildings and facilities, is a barrier to an age-friendly experience.
The issue of ageism cannot be overlooked in developing age-friendly cancer care. Rather, ageism must be identified and eliminated through education and role modeling. Ageism is prejudice or discrimination on the grounds of a person’s age. The WHO (2020) notes that ageism is widespread and that it has harmful effects on the health of older adults. Oncology advocacy and professional groups are important allies in promoting awareness and action. Although ageism was not specifically addressed in this study, it nevertheless is important to identify how institutionalized as well as individual ageism plays a part in readiness for age-friendly cancer care. Institutional assessment, such as the Geriatric Institutional Assessment Program (GIAP) from the NICHE program, offers an important tool for cancer centers in this regard.
This study is limited in several ways. Critically, the initial question asked about preparedness before identifying the elements of readiness in subsequent questions. If that question had been asked at the end of the survey, fewer leaders may have indicated their program was ready to provide age-friendly care. Inter-rater reliability was not calculated on the self-developed survey. The response rate is low, which could indicate a lack of awareness of the topic of workforce preparation for the care of older adults with cancer. However, the response rate is on par with other studies that engaged this population of respondents. The findings are not generalizable given the low response rate. The scope of this project was limited to the 4Ms framework, and some readiness unrelated to this model, such as ageism, may have been missed. Nonetheless, the 4Ms framework provides a useful and practical path through which to assess and implement age-friendly readiness.
Implications for Nursing
Oncology nurses are well positioned to lead the changes needed to ensure readiness for age-friendly cancer care. Nurse educators can improve workforce readiness through expansion of nursing program curriculum to include awareness of ageism and more older adult nursing content. Nurse managers and administrators can advocate for inclusion of advanced practice gerontologic nurses as part of their clinical teams. Nurse executives can provide strategic planning, advocate for financial resources, ensure program development, and provide support for implementation of a framework for age-friendly cancer care, such as the 4Ms framework. 
Conclusion
The results of this survey do not conclusively indicate whether cancer programs in the United States are ready for the large numbers of older adults who will be seeking cancer care in the coming years. This survey will hopefully raise awareness of the steps that may need to be taken. Workforce preparation is needed, facilities need to be updated, and most centers do not have an evidence-based framework to develop programs. Recommendations for developing age-friendly cancer care include increasing awareness of the need, expanding workforce preparation for care of older adult patients with cancer, and improving cancer program leadership engagement. Important next steps include linking awareness of the need for age-friendly cancer care to workforce preparation, education, and access to geriatric oncology experts. Clear, replicable, efficient, and cost-effective recommendations for age-friendly cancer care are needed to prepare the oncology workforce to deliver age-friendly cancer care, focusing on the dignity, values, and participation of older adults.
About the Author(s)
Mary Pat Lynch, DNP, CRNP, AOCN®, NEA-BC, is a cancer service line administrator in the Abramson Cancer Center, and Sarah H. Kagan, PhD, RN, AOCN®, FAAN, is the Lucy Walker Honorary Term Professor of Gerontological Nursing in the School of Nursing and a gerontological clinical nurse specialist in the Abramson Cancer Center, both in the Pennsylvania Hospital at Penn Medicine at the University of Pennsylvania in Philadelphia; and Teresa Hagan Thomas, PhD, RN, is an assistant professor and Laura Fennimore, DNP, RN, NEA-BC, FAAN, is a professor, both in the School of Nursing at the University of Pittsburgh in Pennsylvania. Lynch was supported by a graduate scholarship in cancer nursing practice (GSCNP-19-211-10) from the American Cancer Society. All authors contributed to the conceptualization and design and manuscript preparation. Lynch completed the data collection and statistical support. Lynch, Kagan, and Thomas provided the analysis. Lynch can be reached at marypat.lynch@pennmedicine.upenn.edu, with copy to ONFEditor@ons.org. (Submitted August 2020. Accepted December 12, 2020.)




