Effects of a Web-Based Pediatric Oncology Legacy Intervention on Parental Coping
Objectives: To examine the effects of a legacy intervention for children with advanced cancer and their parents on parental coping strategies.
Sample & Setting: The authors recruited 150 children with advanced cancer and their parents via Facebook.
Methods & Variables: Child–parent dyads were randomly assigned to the intervention or usual care. Children in the intervention group created electronic digital storyboards to assist in documenting their legacies. Parents completed the Responses to Stress Questionnaire at baseline/preintervention (T1) and postintervention (T2). Linear regressions were used to test for differences between the groups in the amount of change from T1 to T2 for each parent coping score.
Results: Although not statistically significant, the legacy intervention showed trends toward increasing use of primary control and disengagement coping strategies in parents over time relative to usual care.
Implications for Nursing: Nurses can help to facilitate opportunities for parents to use adaptive coping strategies. More work is needed to determine how legacy interventions in pediatric oncology can facilitate adaptive coping strategies for parents of children with cancer.
Jump to a section
The diagnosis of advanced (i.e., recurrent or refractory) childhood cancer can foster uncertainty and emotional distress for parents. Parents may experience symptoms of depression and anxiety, lower self-competence, and social isolation, and have high levels of stress (Neu et al., 2014; Olagunju et al., 2016; Rosenberg et al., 2013; Sherief et al., 2015). These consequences can lead to parental distress (Masa’deh & Jarrah, 2017), marital disruptions (Wiener et al., 2017), family financial strain (Lindahl Norberg et al., 2017), and job loss (Hovén et al., 2017; Lindahl Norberg et al., 2017). Parents must cope with their own emotional distress while focusing on their role of meeting their child’s physical, spiritual, and emotional needs (Hinds et al., 2009). Parental coping toward those challenges makes significant impacts on children’s well-being and entire family integrity (Darlington et al., 2018; Isokääntä et al., 2019). In addition, there is a growing need for supportive interventions for both parents and children with cancer as they share distress (Robb & Hanson-Abromeit, 2014).
Legacy-making, or actions or behaviors aimed at being remembered, is one strategy that may help to decrease suffering of patients with serious, advanced conditions and their family members (Akard et al., 2013; Akard, Wray, et al., 2020; Foster et al., 2009). Although legacy interventions have attracted attention in palliative care fields in various forms, such as dignity therapy, life review, and personal narrative interventions, these methods have been mainly used in adults with life-threatening conditions (Brożek et al., 2019; Kittelson et al., 2019; Roikjær et al., 2019; Vuksanovic et al., 2017). Outcomes of adult legacy interventions have included improved dignity, meaning and purpose, will to live, and generativity, and decreased suffering and depressive symptoms (Chochinov et al., 2005; Dose et al., 2018; Vuksanovic et al., 2017). Legacy artwork used with bereaved parents before their children’s death from cancer has improved family bonding and communication, sense of meaning, and coping (Schaefer et al., 2019, 2020). Children’s hospital staff have reported that legacy interventions benefit patients and families, including as a coping strategy for ill children, parents of ill children, and bereaved parents (Foster et al., 2012). However, few studies have examined the effects of legacy interventions on ill children or their parents.
Based on components of Chochinov et al.’s (2005) digital therapy model and stakeholder feedback from children with advanced cancer, bereaved parents, and bereaved siblings (Akard et al., 2013; Foster et al., 2009), the authors previously developed a pediatric legacy intervention via digital storytelling. Pilot work showed promise to improve child quality of life, expression of feelings, coping, and feeling better emotionally (Akard et al., 2015). Parents reported that the legacy intervention improved their coping, emotional comfort, and parent–child communication. The authors expanded their intervention format to include web-based delivery (Akard, Wray, et al., 2020). The purpose of the current study was to examine effects of the web-based legacy intervention on parental coping. The authors hypothesized that compared to usual care, the legacy intervention would increase use of secondary control coping strategies (strategies used to adapt to a stressor [Compas et al., 2012]) among parents across time.
Methods
Conceptual Approach
Chochinov et al.’s (2005) dignity model has provided a framework for legacy interventions in adults but has not been tested with children. The continuing bonds theory proposes that bereaved individuals maintain connections with the deceased that can facilitate coping; however, this theory applies to bereaved individuals rather than children living with cancer or their family members (Klass et al., 1996). Therefore, the authors used components of these existing theories to develop the conceptual framework in Figure 1 to guide the current study. Briefly, this conceptual framework provided a basis for examining the effects of a legacy intervention on outcomes for children living with refractory or relapsed cancer and their parent caregivers. This article reports results related to parent coping outcomes only. Specifically, coping is defined as “conscious volitional efforts to regulate emotion, cognition, behavior, physiology, and the environment in response to stressful events or circumstances” (Compas et al., 2001, p. 89). Coping strategies include the following (Connor-Smith et al., 2000):
• Primary control coping, defined as direct attempts to influence the stressor or one’s emotions as a stress response
• Secondary control coping, defined as adapting to the stressor
• Disengagement, defined as efforts to distance oneself from the stressor emotionally, cognitively, and physically 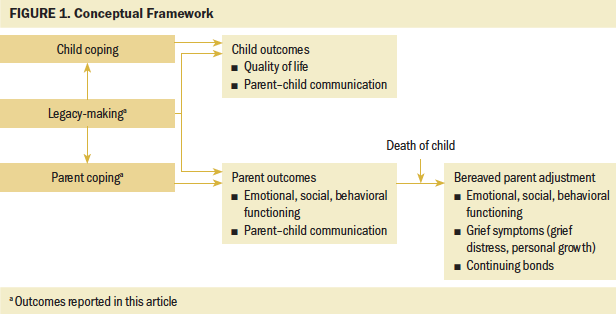
Procedures
This research was part of a randomized controlled trial examining the effects of a legacy intervention on child and parent coping and adjustment. Following institutional review board (IRB) approval from Vanderbilt University in Nashville, Tennessee, recruitment took place via Facebook advertising over three years. Details of Facebook recruitment are described elsewhere (Akard, Wray, et al., 2020; Cho et al., in press). Eligible participants were (a) patients aged 7–17 years and their primary parent caregiver; (b) patients with relapsed or refractory cancer determined by parent self-report; (c) able to speak, understand, read, and type English; (d) with Internet access; and (e) without cognitive impairment as determined during the consent process. Written consent was not required per IRB waiver. Parental consent was shown by completion of REDCap surveys.
Legacy Intervention
After consent, child–parent dyads were randomly assigned to the web-based intervention (n = 75) or to the control (n = 75) group using a computer-generated randomization approach with a permuted block scheme. The project coordinator emailed an electronic link to a password-protected intervention website to parents in the intervention group within one week after parents completed baseline (T1) measures. Each child–parent dyad created a username and password to access the website and created an electronic digital storyboard (Akard, Wray, et al., 2020). The web program directed children to create digital stories about themselves by guiding them to (a) answer guiding questions to document their legacies (e.g., questions about their personal traits, things they like to do, and connections with other people); (b) upload pictures, particularly photographs that may further depict story content; (c) upload video to incorporate the child’s favorite activities, crafts, or locations (e.g., their room), family members, pets, or special messages to loved ones; and (d) upload music, such as a favorite song. Children could select which guiding questions they wanted to answer to include in their story, or they could create content of their own. They were given the option to independently create stories or seek assistance from others. Participants were encouraged to finalize their stories within two weeks. The coordinator emailed a link of the child’s final story.
The waitlist control group participants received care as usual and could receive the intervention after completing postintervention (T2) measures.
Data Collection
Parents completed T1 baseline and T2 postintervention questionnaires online via REDCap. Although T2 was planned at two months post-baseline for all participants, the median time between T1 and T2 was 68 days (range = 7–176) because of flexible scheduling allowed for intervention and T2 completion based on the vulnerable population. Parents also completed a T3 satisfaction survey at the end of the study (see Akard, Wray, et al., 2020 for T3 results). This article presents T1 and T2 parent coping data. Additional results are published elsewhere (Akard, Dietrich, Friedman, Gerhardt, et al., 2020; Akard, Dietrich, Friedman, Wray, et al., 2020; Akard, Wray, et al., 2020).
Measures
Demographic characteristics: Parents provided family background information on a demographic questionnaire. Parents also reported child disease, treatment, and end-of-life care characteristics.
Coping: Parents completed the Response to Stress Questionnaire (Connor-Smith et al., 2000) to measure coping. Parents first completed a checklist of stressors related to childhood cancer, rating how often each stressor has occurred in the recent past. The questionnaire then asks participants to keep those stressors in mind while responding to the rest of the items. Items are rated from 1 (not at all) to 4 (a lot), indicating frequency of responses to stress, resulting in the following five factors:
• Primary control coping (problem solving, emotional expression, emotional modulation)
• Secondary control coping (cognitive restructuring, positive thinking, acceptance, distraction)
• Disengagement coping (avoidance, denial, wishful thinking)
• Involuntary engagement (emotional arousal, physiological arousal, rumination, intrusive thoughts, impulsive action)
• Involuntary disengagement (cognitive interference, emotional numbing, inaction, escape)
The first three factors reflect voluntary coping, and the latter two reflect involuntary stress responses. Because this analysis focused on parent coping strategies, only the three voluntary coping scales are reported. The reliabilities of the scores in this study were 0.63 (T1) and 0.69 (T2) for primary control coping, 0.74 (T1) and 0.76 (T2) for secondary control coping, and 0.82 (T1) and 0.85 (T2) for disengagement coping. This measure was chosen not only because of its strong psychometrics but also its unique ability to measure and differentiate between the three types of coping strategies described.
Analysis
Analyses were conducted using IBM SPSS Statistics, version 26.0. Descriptive statistics summarized demographic characteristics and parental coping scores. To allow for variability in the coping scores at T1, initially the change in each coping score (T1 to T2) was generated for each parent respondent. Because little to no change can be because of high scores at T2 (ceiling effects) or low scores at T1 (floor effects), generalized linear regressions that included the parents’ respective T1 score as a covariate were used to test for group differences in change in each coping score. The beta coefficients for the group effect on change from these regressions were transformed to Cohen’s d effect size indices for ease of interpretation. Conclusions regarding statistical significance used a criterion of p less than 0.05.
Results
Participants
The authors screened 273 child–parent dyads (see Figure 2). Of 250 eligible dyads (23 were excluded because of death or ineligibility), 150 (60%) enrolled in the study. Forty-two (28%) dyads dropped out prior to completing T2. The analysis sample included 97 eligible parents who completed both T1 and T2 within six months of baseline. Summaries of the demographic and clinical characteristics related to attrition have been published elsewhere (Akard, Dietrich, Friedman, Gerhardt, et al., 2020; Akard, Dietrich, Friedman, Wray, et al., 2020; Akard, Wray, et al., 2020). 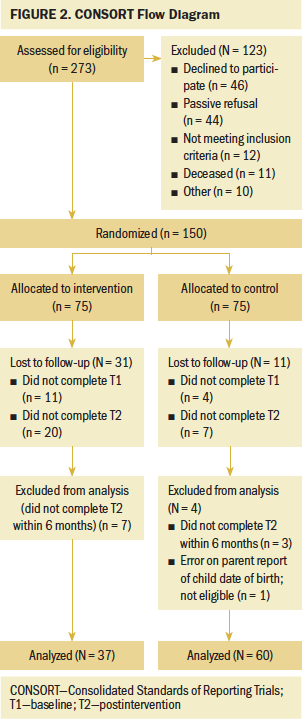
Parents were primarily White (n = 88, 93%), female (n = 88, 93%), married (n = 49, 52%), and college educated (n = 64, 67%), with incomes under $50,000 per year (65%). Their children averaged 10 years of age and were mostly female (n = 57, 59%) with relapsed cancer (n = 69, 71%). Median time since initial diagnosis was 4.1 years. As shown by the summaries presented in Table 1, after controlling for baseline values, none of the differences between the groups in change from T1 from T2 was statistically significant. However, small to moderate effects in the direction of increased use of primary control (Cohen’s d = 0.18) and disengagement (Cohen’s d = 0.31) coping were noted. 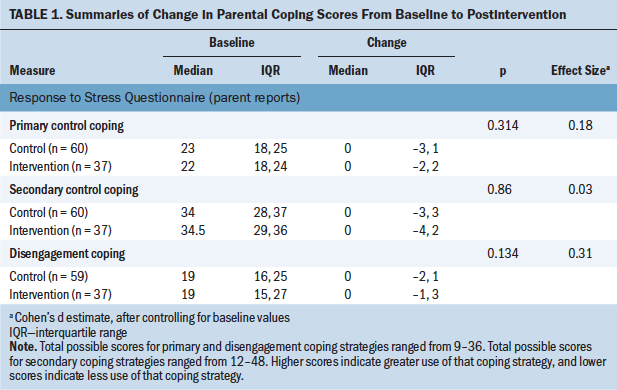
Discussion
This pioneering study examined parental coping effects of a web-based legacy intervention for children with advanced cancer and their parents. Compared to usual care, parents in the intervention group demonstrated a small effect for increased use of primary control coping strategies. The legacy intervention increasing use of parental primary control coping strategies could be explained, in part, by one component of primary control coping being emotional expression. Most parents reported on the T3 concluding satisfaction survey that the intervention improved their coping (n = 36, 46%) and facilitated communication between them and their child (n = 57, 72%) (Akard, Wray, et al., 2020). Hospital staff (n = 57, 74%) have similarly reported that legacy activities provided opportunities for children and families to discuss death and express themselves (Foster et al., 2012).
Parents in the intervention group demonstrated very little effect for increased use of secondary control (Cohen’s d = 0.03). These results suggest that this legacy intervention may be better suited to promote parental use of primary control coping strategies (i.e., seeking out information, taking steps to help the family deal with stress [Compas et al., 2015]) rather than secondary control coping strategies. Although both are considered adaptative, secondary control coping strategies (adapting to the stressor of cancer) are reportedly best suited for uncontrollable stressors, such as cancer and its treatment, and primary control coping strategies (direct attempts to influence the cancer) are better suited for controllable stressors (Compas et al., 2012). Primary and secondary control coping have been strongly associated with lower depressive symptoms in parents of children with cancer (Compas et al., 2015).
Parents in the intervention group compared to usual care demonstrated increased use of disengagement coping (Cohen’s d = 0.31). Disengagement coping strategies are typically reported as maladaptive and include avoidance, denial, and wishful thinking (Compas et al., 2015). However, some studies suggest that disengagement coping is adaptive when combined with primary and secondary control coping strategies (Compas et al., 2015), which could partly explain these results. Previous studies have reported effects of legacy interventions on disengagement coping strategies in patients, such as distraction for adult patients with life-limiting disease (Hesse et al., 2019). Children may share future plans, even though those plans are unlikely to occur (Viola et al., 2018), which may represent wishful thinking. Legacy interventions may contribute to similar thoughts for parents of children with cancer; however, more work is needed to determine if and how disengagement coping strategies can promote parental adaptive coping.
This large parent sample was willing to commit their ill child to a web-based intervention, with 72% completing both pre- and postintervention assessments. This speaks to the applicability of remotely delivered and conducted clinical trials, including computer and mobile intervention delivery of legacy interventions, for these families. Remote delivery methods could expand the reach of such interventions for parents of children with cancer. However, more research is needed to determine if and how these interventions can promote more use of adaptive parental coping strategies.
Results are limited to parents of children aged 7–17 years with relapsed or refractory cancer. One study limitation that strongly speaks to the challenges of this kind of important but difficult work is the higher attrition in the intervention group compared to controls, which limited power. This differential dropout was largely because of technological barriers related to the user friendliness of the intervention web program during the first year. Attrition between groups was similar after these issues were resolved. Attrition rates included deaths; however, the exact number of deaths is unknown because the authors did not access medical records because of Facebook recruitment. Another limitation is the homogeneity of respondents to Facebook advertisements. Study results emphasize the need for strategies to increase sample size and diversity, while continuing to address the changing technologies available to researchers and families.
Implications for Nursing
Future research should qualitatively explore parent perceptions about why they may or may not have had a change in coping strategies following exposure to legacy interventions. More data are needed regarding parents’ perceptions of reasons for change in coping to better understand mechanisms of legacy interventions. Additional parent input for how they could be involved in their child’s legacy-making to facilitate adaptive coping is also warranted. Researchers should examine if legacy interventions are more beneficial for parents with high distress or poor coping strategies. Such data would inform the development of future interventions.
Nurses are in ideal roles to help communicate with parents regarding the support they need to cope with their child’s illness. Nurses can help to facilitate opportunities for parents to use adaptive coping strategies, such as being available to parents who actively seek support or medical information. Nurses should recognize that some parents may need to disengage or engage in wishful thinking at times but be aware that some of these behaviors may indicate that these parents need additional resources and support. Nurses can offer suggestions or refer parents to resources for families who may be interested in legacy activities, while recognizing that such activities may not be appropriate for all children and their parents. Although this web-based intervention is currently undergoing modifications and is not yet available for public use, components of the intervention, as described in Akard, Wray, et al. (2020), can be used and incorporated into clinical practice. 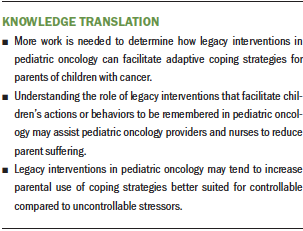
Conclusion
The current study examined the effects of a web-based legacy intervention on parental coping for children with recurrent or refractory cancer and their parents. Increased use of primary control coping following the legacy intervention was consistent with parent reports of improved communication (Akard, Wray, et al., 2020). Although secondary coping is thought to be more commonly associated with uncontrollable stressors such as cancer, primary control coping may be beneficial in reducing depressive symptoms and enhancing communication. Disengagement coping may even be beneficial when combined with primary or secondary coping. Future research will increase understanding about parental coping during childhood cancer and how suffering can be reduced for these vulnerable children and their parents.
The authors gratefully acknowledge the children and parents who generously participated in this study. The authors also gratefully acknowledge Sodium Halogen for their design and hosting of the intervention website and Paramore Digital for assisting in Facebook recruitment.
About the Author(s)
Terrah Foster Akard, PhD, RN, CPNP, FAAN, is an associate professor of nursing and medicine and the director of graduate studies for the PhD in Nursing Science Program and Mary S. Dietrich, PhD, MS, is a professor of biostatistics and measurements, both in the School of Nursing and in the School of Medicine at Vanderbilt University in Nashville, TN; Debra L. Friedman, MD, MS, is the E. Bronson Ingram Chair in Pediatric Oncology, an associate professor of pediatrics, the leader of the Vanderbilt-Ingram Cancer Center Cancer Control and Prevention Program, and the director of the Division of Hematology-Oncology at Vanderbilt University Medical Center and Vanderbilt-Ingram Cancer Center, both in Nashville, TN; Sarah Wray, MSN, RN, CPNP, is a research project coordinator in the School of Nursing at Vanderbilt University; Cynthia A. Gerhardt, PhD, is a professor of pediatrics and psychology at the Ohio State University and the director of the Center for Biobehavioral Health in the Abigail Wexner Research Institute at Nationwide Children’s Hospital, both in Columbus, OH; Barbara Given, PhD, RN, FAAN, is the university distinguished professor emerita and interim associate dean for research in the College of Nursing at Michigan State University in Lansing, MI; Verna L. Hendricks-Ferguson, PhD, RN, FPCN, FAAN, is the Irene Riddle Endowed Professor in the School of Nursing at Saint Louis University in Missouri; Pamela S. Hinds, PhD, RN, FAAN, is the William and Joanne Conway Chair in Nursing Research, the executive director of the Department of Nursing Science, Professional Practice, and Quality Outcomes, and a research integrity officer, all at Children’s National Health System, and a professor in the Department of Pediatrics at George Washington University, both in Washington, DC; Eunji Cho, PhD, RN, is a postdoctoral fellow in the School of Nursing at Vanderbilt University; and Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, is a professor of nursing and a professor of medicine in the School of Nursing and in the School of Medicine at Vanderbilt University. This work was supported by the National Institute of Nursing Research (grant number RO1 NR015353; ClinicalTrials.gov number NCT04059393; principal investigator: Akard) and National Institutes of Health/National Center for Advancing Translational Sciences (grant number UL1 TR000445). In addition, this project was conducted in collaboration with the Palliative Care Research Cooperative Group funded by the National Institute of Nursing Research (grant number U24 NR014637). Akard, Friedman, Gerhardt, Hendricks-Ferguson, Hinds, and Gilmer contributed to the conceptualization and design. Akard, Friedman, and Wray completed the data collection. Akard and Dietrich provided statistical support. Akard, Dietrich, Friedman, Given, Hendricks-Ferguson, and Hinds provided the analysis. Akard, Dietrich, Friedman, Gerhardt, Given, Hendricks-Ferguson, Hinds, Cho, and Gilmer contributed to the manuscript preparation. Akard can be reached at terrah.akard@vanderbilt.edu, with copy to ONFEditor@ons.org. (Submitted May 2020. Accepted November 18, 2020.)

