Feasibility Pilot Study of a Virtual Intervention for Survivors With Decreased Perceived Cognitive Function After Cancer Treatment
Objectives: Many cancer survivors report issues with cognitive function following diagnosis and treatment. The purpose of this single-arm pilot study was to test the feasibility and acceptability of virtual delivery of a cognitive rehabilitation intervention for participants in virtual groups.
Sample & Setting: 37 adult cancer survivors reporting impaired cognitive function following primary treatment were enrolled from Cedars-Sinai Medical Center and affiliates, the University of Kansas Cancer Center, and the Masonic Cancer Alliance.
Methods & Variables: Two cohorts attended six weekly virtual sessions and completed pre- and postintervention patient-reported outcome questionnaires designed to measure perceived cognitive function, loneliness, and determinants of behavior change for exercise, sleep, and mindfulness.
Results: Postintervention scores for perceived cognitive function, determinants of behavior change, and loneliness ratings significantly improved.
Implications for Nursing: Evidence continues to build in support of cognitive rehabilitation interventions for cancer survivors. Nurses play an important role in terms of patient identification, participation, and facilitation.
Jump to a section
About 75% of cancer survivors report significant decreases in cognitive function (CF) during and following treatment for non–central nervous system (CNS) malignancies (Janelsins et al., 2014). These cognitive effects may persist for years in a subset of survivors (about 35%) and have a significant negative impact on many aspects of quality of life, including home, work, and social functioning (Koppelmans et al., 2014; Myers, 2012; Von Ah et al., 2013). Research indicates that some behavioral lifestyle factors may potentiate cancer-related cognitive impairment, such as level of physical activity, disturbed sleep, and loneliness (Hartman et al., 2015; Jaremka et al., 2014; Myers et al., 2020). Hartman et al. (2015) were the first to explore the relationship between physical activity, sleep disturbance, and CF in cancer survivors. Using a computerized battery of neurocognitive tests and linear regression, Hartman et al. (2015) demonstrated significant relationships between physical activity and cognitive performance in the domains of executive function, attention, and visuospatial ability. Jaremka et al. (2014) reported the results of three studies conducted with breast cancer survivors and individuals without cancer indicating that loneliness was associated with both self-report of cognitive issues and worse performance on neurocognitive tests. The current authors’ previous pilot work (Myers et al., 2020) further demonstrated a correlation between loneliness and cancer survivors’ increased reports of changes in CF. Postintervention improvements in loneliness correlated with improvement in self-report of CF. Mindfulness practices also have shown promise in enhancing CF in the general population and in cancer survivors. Proposed mechanisms for the impact of physical activity, undisturbed sleep, and reduction in loneliness all include reduction in inflammatory products (cytokines) and the stress response (Asher & Myers, 2015). Exercise also is postulated to increase products and processes associated with improvement of brain health, such as brain-derived neurotrophic factor, neurogenesis, and angiogenesis (Asher & Myers, 2015).
The search for effective interventions to prevent or mitigate cancer-related cognitive impairment is ongoing. One promising area is the study of cognitive rehabilitation, a multifaceted intervention inclusive of psychoeducation, cognitive training, and cognitive behavioral training (Myers et al., 2020). Results were previously published of a prospective, waitlist-controlled study of a six-week, multidimensional psychoeducational cognitive rehabilitation intervention, Emerging From the HazeTM (Haze), for women with breast cancer who reported decreased perceived CF (PCF) (Myers et al., 2020). PCF is a subjective measure obtained by self-report of one’s thinking skills, memory, and concentration. Haze is comprised of didactic and experiential content and provides participants with a toolbox of adaptive strategies designed to enhance attention and short-term memory, as well as to cope with deficits in CF. Three components of the lifestyle-related content include information regarding increasing exercise, improving sleep, and implementing mindfulness techniques. Statistically significant improvement in PCF that appeared to be durable was demonstrated for the intervention group. However, data were not collected on participants’ likelihood of behavioral change as a result of attending the program.
Haze is a regular component of the cancer survivorship program at Cedars-Sinai Medical Center in Los Angeles, California, and has been delivered in person since 2010 to groups of cancer survivors. Results from a retrospective analysis of a mixed sample of 110 cancer survivors receiving the Haze intervention (54% with breast cancer, 15% with gynecologic cancer, 14% with hematologic cancer, 8% with gastrointestinal cancer, and 11% with another cancer type) also demonstrated a significant improvement in self-reported CF and health-related quality of life (Asher et al., 2019). Haze also has been delivered remotely to in-person groups in other institutional locations (Myers et al., 2020). Since the advent of the COVID-19 pandemic, Haze has not been administered to in-person groups. The purpose of this single-arm pilot study was to test the feasibility and acceptability of a purely virtual delivery of Haze to groups of participants via password-protected teleconferencing. Results from this study will be used to inform a larger, confirmatory, multisite study.
The primary aim of this study was to demonstrate the feasibility of the complete virtual delivery of the Haze intervention by recruiting 30 participants and achieving a retention rate of at least 70%. The second aim was to demonstrate the feasibility and acceptability of measures assessing determinants of behavior change for exercise, sleep, and mindfulness postintervention (missing data of less than 25% and Cronbach’s alpha of 0.7 or greater). The third aim was to explore the impact of Haze on patient-reported outcomes for PCF, determinants of behavior change, and loneliness.
Methods
Theoretical Framework
The theory of planned behavior was used as a framework to explore behavior change following participation in the Haze intervention (Azjen, 2019). This theory proposes four constructs that influence behavior: instrumental and affective attitudes toward the behavior, perceived behavioral control, subjective norms, and intentions to engage in the behavior.
Variables
Haze is delivered in six weekly sessions by an interprofessional team and consists of a combination of didactic and experiential content, as well as participant–presenter engagement. A cancer rehabilitation physician and a neuropsychologist facilitated the Haze intervention. Specific details of the interventional content have been published previously (Liang et al., 2019; Myers et al., 2020). For this pilot study, the intervention was delivered in real time via secure teleconferencing technology from Cedars-Sinai Medical Center to participants in two virtual cohort groups in fall 2020 and spring 2021 (N = 21 and N = 16, respectively).
REDCap, a secure, web-based software platform, was used for electronic consent and study questionnaire completion (Harris et al., 2009). Data were collected electronically at baseline, or within one week prior to the first session of the intervention (time 1 [T1]), and within two weeks of completing the six-week intervention (T2).
Participants completed a demographics questionnaire; the Patient-Reported Outcomes Measurement Information System (PROMIS) eight-item short forms for CF and CF abilities, version 2.0; and the 20-item University of California, Los Angeles, Loneliness Scale, version 3.0. These instruments are validated for use with cancer survivors (Lai et al., 2014; Russell, 1996).
Based on the theory of planned behavior, four determinants of health behavior were evaluated (Azjen, 2019). These four determinants were instrumental (one item) and affective attitudes (four items), perceived behavioral control (three items), subjective norms (one item), and intentions (two items) (Ajzen, 1991, 2019; Rhodes & Courneya, 2004; Rhodes & Rebar, 2017). Items were ranked on a seven-point Likert-type scale ranging from 1 to 7, with higher scores indicating increased likelihood of behavior adaptation. Scores were obtained by summing the item totals and dividing by the number of items for each construct. The four constructs were measured across the three behaviors highlighted in the intervention: exercise, sleep, and mindfulness. These construct items are well validated in exercise studies, including those with populations of patients with cancer. Data were collected and analyzed to further assess reliability for sleep and mindfulness behavior. In addition, participants rated their satisfaction with 11 items related to session and overall course length, specific weekly content, and quality of homework on a scale of 0 (not satisfied) to 5 (exceptionally satisfied).
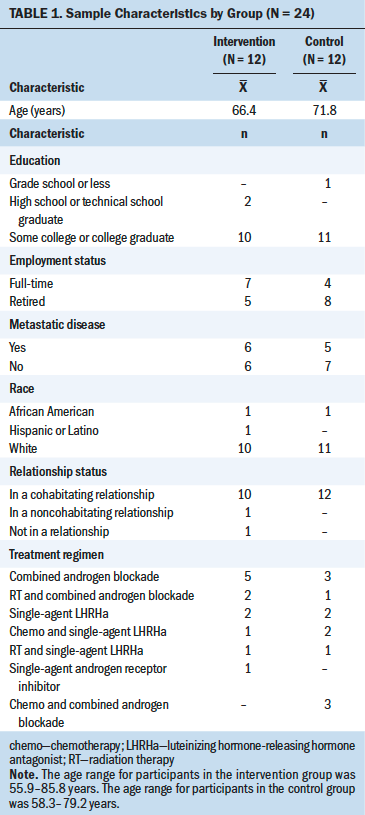
Descriptive statistics were used to quantify demographics and calculate percentages for attrition rate, attendance adherence, and participant satisfaction ratings. Because of non-normal distribution of data, Wilcoxon signed rank testing was used to compare pre- and postintervention scores on the study instruments. Reliability of the measures of determinants of behavior change was assessed by Pearson’s correlation (single items) and Cronbach’s alpha (multiple items). As a result of the small sample size and the primary objective of feasibility, the authors did not control for type of cancer, previous treatment regimen, or ongoing endocrine therapy.
Sample and Setting
English-speaking adults (aged 21 years or older) who reported decreased PCF following completion of primary treatment for non-CNS cancer were enrolled in the study. This self-report was operationalized as any report of change in CF to their healthcare provider(s). Because the current authors’ objective was to demonstrate the feasibility of virtual intervention delivery, participation was not restricted by tumor type, time since completion of primary therapy, or specific treatment regimen. Ongoing endocrine, anti-HER2, or other stable maintenance therapies were allowed, despite endocrine therapy’s potential contributions to cognitive issues. Participants were excluded for CNS involvement or concurrent treatment with chemotherapy or radiation therapy.
Participants were recruited from Cedars-Sinai Medical Center and affiliates, the University of Kansas Cancer Center, and the Masonic Cancer Alliance. Recruitment efforts included providing study flyers in survivorship clinic areas, presenting information about the study to local cancer support groups, and having rehabilitation specialists and nurse practitioners discuss the study during survivorship clinic visits. Access to the internet and a device that would accommodate teleconferencing were required for participation in this pilot study.
Results
Thirty-nine individuals provided informed consent. Of these, two dropped out prior to data collection or program attendance (one because of advancing disease and one because of work conflicts). The remaining 37 individuals completed baseline assessments and were included in the data analyses. Thirty-two participants completed all T2 data. One participant partially completed T2 data because of personal issues. Overall, the retention rate was 85%, and 89% for those initiating the intervention.
Ages ranged from 30 to 73 years, with a mean of 56.7 years (SD = 11.1). Years of education ranged from 12 to 20 years, with a mean of 16 years (SD = 1.8). Most participants were diagnosed with breast cancer (n = 26), and other disease types included gastrointestinal cancer (n = 3), gynecologic cancer (n = 3), lymphoma (n = 3), and head and neck cancer (n = 2). Most participants had completed chemotherapy (n = 34) and/or radiation therapy (n = 29). Seventeen participants were receiving endocrine therapy; one of these participants also was receiving anti-HER2 therapy. One participant was receiving rituximab. Fourteen participants were more than 12 months out from completion of primary therapy. The remainder were 6–12 months out (n = 7) or less than 6 months out (n = 16) from completion of primary therapy. Most participants were female (n = 34), postmenopausal (n = 29), non-Hispanic (n = 35), White (n = 32), and married (n = 20). Ten participants were retired, eight were unemployed, and four were on medical leave; 10 were working full-time, and five were working part-time. A total of 24 participants attended all six sessions. Weekly attendance ranged from 30 to 32 participants. Participant satisfaction ratings were high for the overall length of the program and for the weekly content.
Adequate reliability (Cronbach’s alpha of greater than 0.7) was demonstrated for each behavioral construct (instrumental and affective attitudes, perceived behavioral control, subjective norms, and intentions) at both time points (T1 and T2) and all three behaviors (exercise, sleep, mindfulness), with one exception (sleep intention construct at T2, with a Cronbach’s alpha of 0.688). Data were missing for only two participants at T2.
Participants’ scores significantly improved for both measures of PCF, as well as for loneliness. Likewise, significant postintervention increases were demonstrated for exercise perceived behavioral control and intention, as well as for mindfulness intention (see Table 1). Significant positive correlation was noted for changes in PCF (PROMIS-CF) and mindfulness affective attitudes (r = 0.452, p = 0.008). Significant inverse correlation was noted for change in loneliness and both measures of PCF at T2 (r = –0.376, p = 0.031 for PROMIS-CF; r = –0.452, p = 0.008 for PROMIS–CF abilities). Changes in loneliness scores were significantly inversely correlated with changes in exercise intention (r = –0.544, p = 0.001).
Discussion
The significant postintervention improvement in PCF is commensurate with the current authors’ previous prospective controlled study involving breast cancer survivors and retrospective analyses of data collected from a mixed sample of 110 cancer survivors who experienced the in-person delivery of Haze (Asher et al., 2019). Results from this small single-arm pilot study provide further evidence of the feasibility and potential effectiveness of the Haze intervention across a variety of types of cancers. As with the breast cancer survivor pilot, the current study results indicate a significant decrease in participants’ rating of loneliness between baseline and completion of Haze. Of note, changes in loneliness scores appeared to be inversely correlated with change in determinants of health behavior for exercise. Loneliness has been associated with increased risk of inactivity in older adults (Schrempft et al., 2019). Feelings of social isolation may have impaired intentions for behavioral change in addition to magnifying participants’ perceptions of impaired CF. Despite evidence of successful recruitment and retention for this and previous studies, one limitation of either in-person or live virtual group delivery of Haze relates to restrictions for participant access because of time zone and work-related schedule constraints. The ability of individual cancer centers to virtually host a prerecorded version of Haze content is of significant interest and would broaden dissemination of the intervention to a larger, and potentially more diverse, population. An additional research question to be explored is the potential contribution of the group effect as a mechanism for validating the experience of cognitive changes for participants. Future research is needed to compare delivery of the Haze intervention in a group setting versus in an individual setting. Additional investigation of the Haze intervention for cancer survivors of diverse malignancies and treatment regimens will help identify potential predictors of a positive response.
Implications for Nursing
The literature is replete with evidence highlighting the importance of attending to cognitive changes (subjective and objective), psychological distress, and lifestyle behavioral alterations in individuals with cancer. Evidence continues to build in support of cognitive rehabilitation interventions for cancer survivors reporting cognitive issues. Nurses are crucial for identifying patients who may benefit from cognitive rehabilitation, encouraging participation in clinical trials, and facilitating accessibility to resources. Assessment of available cognitive rehabilitation programs or ongoing research studies is important for nurses providing care to cancer survivors.
Conclusion
The study results indicate that virtual delivery of a cognitive rehabilitation intervention is feasible and acceptable to cancer survivors reporting issues with PCF following primary cancer treatment. These results will be used to inform a randomized controlled trial comparing real-time virtual delivery of Haze to virtual delivery of a facilitator-hosted, prerecorded adaptation of the intervention.
The authors gratefully acknowledge Bin McLaurin, BS, for facilitating participant communication and access to the telehealth platform.
About the Author(s)
Jamie S. Myers, PhD, RN, AOCNS®, FAAN, is a research associate professor in the School of Nursing at the University of Kansas in Kansas City; and Celina H. Shirazipour, PhD, is an assistant professor in the Cancer Research Center for Health Equity, Jeffrey C. Wertheimer, PhD, ABPP-CN, is the associate director of Physical Medicine and Rehabilitation and chief of Psychology and Neuropsychology Services, and Arash Asher, MD, is the director of Cancer Rehabilitation and Survivorship at the Samuel Oschin Cancer Center, all at Cedars-Sinai Medical Center in Los Angeles, CA. This research was supported by the Larry and Helen Hoag Foundation. Myers, Shirazipour, and Asher contributed to the conceptualization and design. Myers completed the data collection and provided statistical support. All authors provided the analysis and contributed to the manuscript preparation. Myers can be reached at jmyers@kumc.edu, with copy to ONFEditor@ons.org. (Submitted June 2021. Accepted August 4, 2021.)

