Resistance Exercise Reduces Body Fat and Insulin During Androgen-Deprivation Therapy for Prostate Cancer
Purpose/Objectives: To determine whether exercise could reduce biomarkers of cancer progression in prostate cancer survivors (PCSs) on androgen-deprivation therapy (ADT).
Design: Randomized, controlled trial.
Setting: Oregon Health and Science University School of Nursing.
Sample: 51 PCSs randomized to one year of resistance and impact training or a stretching control group.
Methods: The authors investigated changes in body composition and cancer-related biomarkers, and the influence of age and fat loss on changes in biomarkers.
Main Research Variables: Body composition (total fat, trunk fat, and lean mass), insulin, insulin-like growth factor-1, and sex hormone–binding globulin.
Findings: In the 36 PCSs with baseline and 12-month data, total fat (p = 0.02) and trunk fat (p = 0.06) mass decreased in the training group compared to gains in controls. Loss of total and trunk fat each mediated the relationship between groups and one-year change in insulin (p < 0.05). Age moderated the insulin response to exercise where insulin reductions were smaller with increasing age (p = 0.03).
Conclusions: Resistance and impact exercise may reduce body fat among PCSs undergoing ADT, in turn exerting an insulin-lowering effect.
Implications for Nursing: Nurses should counsel PCSs to exercise to reduce the risk of obesity and associated conditions, including cancer progression.
Jump to a section
Among prostate cancer survivors (PCSs), inactivity, increased adiposity, and weight gain have been associated with poorer survival outcomes. Overweight and obese PCSs have lower survival rates and an increased risk of cancer progression compared to men who weigh less (Gong, Agalliu, Lin, Stanford, & Kristal, 2007). Adiposity may worsen prognosis for PCSs because it can lead to hyperinsulinemia and chronic inflammation, which worsens insulin resistance, and these states are associated with an increased risk of prostate cancer recurrence, as well as prostate cancer and overall mortality (Cao & Ma, 2011; Prins et al., 2012). Two large, observational studies suggested that PCSs who report regular physical activity have a lower risk of disease progression and cancer-specific mortality than sedentary survivors (Kenfield, Stampfer, Giovannucci, & Chan, 2011; Richman et al., 2011). The mechanisms that underlie this observed relationship between physical activity and survival have yet to be substantiated through controlled trials, but because exercise is an accepted weight-control strategy, the protective effect of exercise against cancer recurrence may act through this mechanism (McTiernan, 2008). Some studies in non-cancer populations report that exercise-induced reductions in cytokines or sex hormones only occur in the presence of weight loss and that, among people who exercise, fat loss is directly associated with reductions in inflammation (Kohut et al., 2006; Kraemer et al., 1999). Whether or not changes in adiposity must occur to shift biomarkers of cancer progression in PCSs remains unknown.
About one-third of all PCSs are treated with androgen-deprivation therapy (ADT) to reduce tumor androgen exposure. PCSs undergoing ADT experience significant increases in adiposity, including subcutaneous and visceral fat deposits that could further increase their risk of cancer progression (Haseen, Murray, Cardwell, O’Sullivan, & Cantwell, 2010). In addition to concerns about disease prognosis, PCSs undergoing ADT face additional threats to survival because of the effects of aging or cancer treatment, including osteoporosis, cardiovascular disease, and diabetes (Keating, O’Malley, Freedland, & Smith, 2010). The authors of the current article developed a resistance and impact exercise program, Prevent Osteoporosis With Impact and Resistance (POWIR), that reduces risk factors for fracture in female cancer survivors (Winters-Stone et al., 2011, 2012, 2013) and slowed bone loss, reversed muscle weakness, and lessened mobility disability in PCSs undergoing ADT (Winters-Stone et al., 2014, 2015). In the latter study, the authors also measured body composition and collected serum samples for analysis of select biomarkers associated with cancer progression (i.e., insulin, insulin-like growth factor [IGF]-1, and sex hormone–binding globulin [SHBG]). The purpose of this article is to determine whether the benefits of POWIR extend to improved body composition and biomarker profiles in PCSs undergoing ADT. The authors also explored whether changes in body fat influenced (i.e., mediated) changes in biomarkers of cancer progression and whether age or ADT dosing regimen moderated the influence of exercise on body composition and biomarkers (see Figure 1).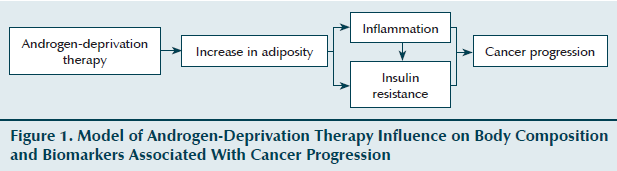
Methods
Design
The authors conducted a 12-month single-blind randomized, controlled trial comparing two parallel groups receiving progressive, supervised exercise: (a) POWIR (experimental) and (b) FLEX (short for “flexibility,” placebo control). Outcomes were measured at baseline, 6 months, and 12 months. Testing and exercise training took place at Oregon Health and Science University (OHSU).
Recruitment methods for the trial were reported elsewhere (Winters-Stone et al., 2014). Inclusion criteria were having a diagnosis of prostate cancer, currently receiving ADT, no concurrent chemotherapy, no known bone metastases in the hip or spine, no detectable osteoporosis, no regular (more than twice per week with 30 minutes per session) participation in moderate-to-vigorous resistance training, and no contraindications for exercise. Physician clearance for exercise training was obtained for each participant before training commenced. The study was approved by the institutional review board at OHSU, and informed consent was obtained prior to baseline testing.
Sample size was estimated from an a priori power analysis to detect differences in the primary aim of the study, bone mineral density, resulting in 25 participants per group (Winters-Stone et al., 2014). Using the same approach based on a 2 x 3 mixed-design analysis of variance and using initial and change values for body fat from a prior study (Winters & Snow, 2000), 25 participants per group would provide power of greater than 0.8 to detect a 6% decrease in fat mass with a Cronbach alpha of less than 0.05.
Interventions
A detailed description of the interventions, including program progression, is provided elsewhere (Winters-Stone et al., 2014). Participants in both groups were prescribed an exercise program consisting of two one-hour supervised classes and one 30- to 45-minute home-based session per week for 12 months. POWIR was based on prior interventions in people without cancer (Winters & Snow, 2000) and followed American College of Sports Medicine’s recommendations for preserving bone health and muscle strength in older adults (Chodzko-Zajko et al., 2009; Kohrt, Bloomfield, Little, Nelson, & Yingling, 2004). Resistance training used free weights (e.g., dumbbells, barbells, weighted vest) for 1–3 sets per exercise at a weight that could be lifted for 8–12 repetitions (about 60%–80% of one repetition maximum [RM]). Impact exercises were included to place a load on the skeleton by generating ground reaction forces and consisted of 50 two-footed jumps from the ground with weighted vests. An exercise session consisted of wall-sits, squats, dead lifts, lunges, rows, chest presses, lateral raise, push-ups, and two-footed jumps. Participants in the control group (FLEX) performed whole-body stretching and relaxation exercises in a seated or prostrate position to minimize muscle forces and energy expenditure. Aside from FLEX, participants in this group were encouraged to maintain habitual physical activity levels throughout the intervention.
Procedures
At the baseline visit, blood was drawn following 12-hour fasts, body composition measurements were taken, and participants completed questionnaires. Tests were administered by trained technicians blinded to group assignment and were repeated at 6 and 12 months. Randomization was stratified by length of ADT use (greater than one year or one year or less) and current aerobic activity (90 minutes per week or more versus less than 90 minutes per week).
Demographic, clinical history, and medication use was obtained by self-report at each visit. Chronic medical conditions were assessed by self-report using the Charlson Comorbidity Index (Charlson, Pompei, Ales, & MacKenzie, 1987). To consider whether physical activity and diet changed during the intervention, the authors used valid and reliable instruments to measure current physical activity energy expenditure with the Community Health Activity Model Program for Seniors (CHAMPS) physical activity questionnaire for older adults (Bennett, Young, Nail, Winters-Stone, & Hanson, 2008; Stewart et al., 2001) and energy intake with the Block Food Frequency Questionnaire (Block, Thompson, Hartman, Larkin, & Guire, 1992). Answers to select questions on CHAMPS were also used to screen for eligibility. Body height (in meters) was measured without shoes using a wall-mounted stadiometer, and body weight (in kilograms) was measured on a balance-beam scale.
Bone-free lean and fat mass (in kilograms) of the whole body were assessed by dual-energy x-ray absorptiometry (DXA). The authors also determined fat mass in the trunk region from the whole-body scan to estimate central adiposity. DXA scans were performed by licensed technicians blinded to participant group and were analyzed by a single technician. The authors’ in-house coefficients of variation (CVs) for DXA-measured soft tissue are less than 1.5% (Winters & Snow, 2000).
From stored and batched serum samples, insulin (mcIU/ml), IGF-1 (ng/ml), and SHBG (nmol/ml) were analyzed by chemiluminescent assay, and total testosterone (ng/dl) was analyzed by radioimmunoassay, all using commercial kits. Inter-assay and intra-assay CVs for insulin, IGF-1, SHBG, and testosterone were 7.1% and 5.7%, 6.4% and 3.6%, 8% and 6.9%, and 6% and 10%, respectively.
Statistical Analysis
The intent-to-treat (ITT) analysis was performed using a linear mixed-effects modeling approach implemented in the lme package for the R statistical computing environment. The approach uses full information maximum likelihood estimation for handling missing data and performs on par with multiple imputation for generating unbiased parameter estimates. In addition to ITT analysis, data from participants in both groups with complete baseline and 12-month data were considered to evaluate intervention effects in participants who completed the study (completers) using separate 2 (group) x 3 (time) mixed-design analysis of covariance for each outcome. Age and time since diagnosis were included as covariates to account for any influence of these variables on exercise tolerance and adaptations. To examine the influence of ADT dosing regimen (e.g., continuous versus intermittent) or age on the efficacy of POWIR, linear mixed-effects modeling was repeated to examine for potential moderator effects. To explore whether changes in biomarkers of cancer progression from POWIR were mediated by changes in body composition parameters, mediation analyses were performed using the RMediation package using the distribution-of-the-product method (Tofighi & MacKinnon, 2011). Mediation tests were conducted using mediator (total fat mass, trunk fat mass, or percent body fat) and biomarker change scores (from baseline to 12 months). The authors evaluated all hypotheses using an alpha significance level of 0.05.
Results
Sample
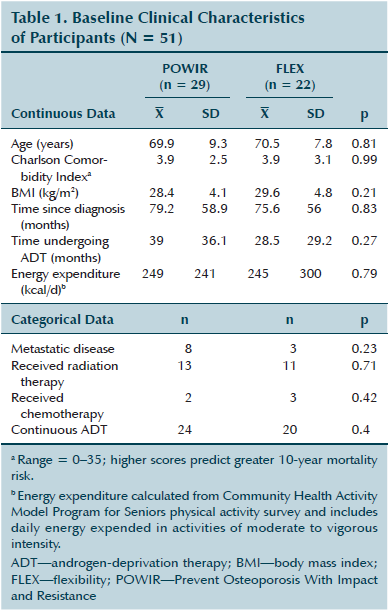
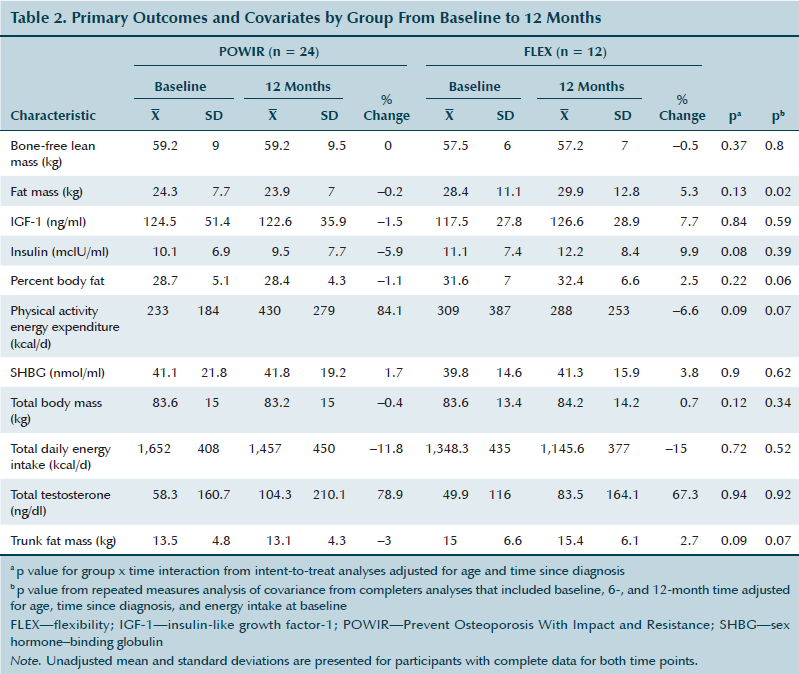
Of 467 men expressing interest, 51 were eligible and enrolled in the trial. Participants were randomized to POWIR (n = 29) or FLEX (n = 22) (see Figure 2). On average, participants were older, overweight men with multiple comorbidities (see Table 1). Less than 25% of men had metastatic disease, and few had received chemotherapy prior to enrollment. Participants were an average of six years past diagnosis and had been undergoing ADT for more than two to three years. Intervention groups were not different at baseline on any demographic, clinical characteristic, or outcome measure when considering the full sample; however, among completers, groups differed for baseline energy intake, which was then considered as a covariate for analyses in this sample (see Table 2). 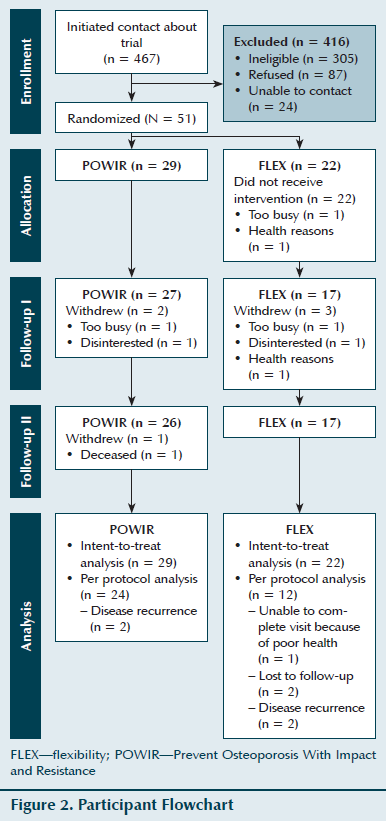
Adherence and Compliance
Retention of men in the one-year study was 84% and was slightly higher, but not significantly so, within POWIR (90%) than FLEX (77%). The median attendance for supervised classes was 84% for POWIR and 74% for FLEX, and median attendance to home-based sessions was 43% for POWIR and 51% for FLEX. Attendance did not significantly differ between groups. No injuries or adverse events were reported.
Body Composition
A significant group x time interaction for fat mass was noted when considering completers and including all covariates in the model (p = 0.02); significance weakened when considering the ITT sample (p = 0.13). Similar patterns were found for percent body fat and trunk fat mass where group x time interactions were almost significantly different in completers (p = 0.07 for percent body fat; p = 0.06 for trunk fat mass) but weakened somewhat in the ITT sample. Men in the POWIR arm lost weight and decreased percent body fat because of a reduction in fat mass, whereas men in the FLEX arm gained weight and increased percent body fat because of a disproportionate increase in fat relative to lean mass.
Biomarkers
Circulating insulin and IGF-1 levels decreased slightly among men in the POWIR arm compared to increases in both biomarkers among men in the FLEX arm. A trend toward significance for insulin was found among the ITT sample (Coefficient for group x time = –1.34, standard error [SE] = 0.76, t(73) = –1.76, p = 0.08). Despite increases in testosterone during the intervention period, changes were similar between the POWIR and FLEX arms, but SHBG was unchanged. Testosterone increases were greater among men receiving intermittent ADT (n = 6), with mean increases of 161.2 ng/dl (SD = 252.4 ng/dl) during one year compared to mean increases of 21 ng/dl (SD = 180 ng/dl) among men receiving continuous ADT (n = 30); however, group x time interactions for testosterone were not significant when considering men on intermittent or continuous ADT separately.
Moderation and Mediation Analyses
Neither age nor ADT dosing regimen moderated the effects of exercise on body composition. There was no effect of ADT dosing regimen on changes in any biomarker; however, there was a significant effect modification by age on group x time differences for insulin (Coefficient for age x group x time = 0.19, SE = 0.09, t(71) = 2.20, p = 0.03) where differences between the POWIR and FLEX arms were greatest among younger PCSs and narrowed with increasing age of participants (see Figure 3). Mediation analyses revealed significant indirect effects of loss of total fat mass (indirect effect = –1.96; 95% CI [–0.19, –3.83]; p = 0.04) and loss of trunk fat mass (indirect effect = –1.38; 95% CI [–0.23, –2.61]; p = 0.03) on group differences in insulin from baseline to 12 months. 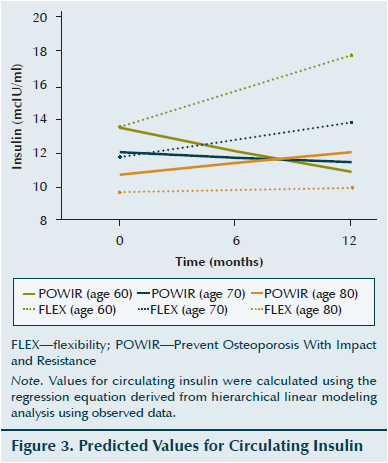
Discussion
The authors’ study is the first to show that a one-year resistance and impact training program (POWIR) that was designed to combat ADT-related bone loss may also have a favorable influence on body composition that reduces circulating insulin. POWIR has shown preliminary efficacy for preventing bone loss (Winters-Stone et al., 2014) and lessening disability (Winters-Stone et al., 2015) and now also appears to prevent gains in body fat, including central fat deposits that are typical with ADT. A trend occurred for POWIR to lower insulin compared to increases experienced in the control group, and these group differences were influenced by age and fat loss during the study period. POWIR training was more likely to lower insulin levels among men in the younger age range of the sample compared to older-aged men, and POWIR appears to have exerted an insulin-lowering effect through changes in body fat.
The ability of exercise to favorably shift body composition among PCSs undergoing ADT has only been examined in three controlled trials that used short-term training programs and machine-based resistance exercise. Segal et al. (2003) failed to detect any influence of a 12-week machine-based, moderate-intensity resistance training program on body weight or composition among PCSs undergoing ADT. Other investigations of a 12-week program of machine-based resistance and aerobic training in PCSs undergoing ADT reported consistent effects on lean body mass but prevention of fat gain only in men just beginning ADT (Cormie et al., 2015; Galvão, Taaffe, Spry, Joseph, & Newton, 2010). The authors of the current study expected POWIR to improve lean body mass, but the intensity of training actually performed by men in the trial may have been insufficient to induce muscle hypertrophy. The energy deficit among men in the POWIR arm could have limited the ability to gain lean body mass, but might also suggest that POWIR preserved muscle during energy restriction (Miller et al., 2013). Men in this trial were undergoing ADT two to three times longer than participants in other trials, so it also is possible that exercise becomes a less effective countermeasure to ADT-induced lean body mass loss as duration of treatment extends. POWIR participants who completed the trial maintained body fat and even lost trunk fat in contrast to control participants who gained fat in the total body and trunk region. POWIR likely limited fat gain because it increased physical activity by an average of 200 kcal/day. Participation in POWIR would contribute to this energy expenditure, estimated at about 350 kcal/session (Ainsworth et al., 2011), but it may also reflect an increase in participation in additional physical activity outside of the intervention. The effectiveness of POWIR to improve body composition was not influenced by age or ADT dosing regimen and, therefore, could be an effective countermeasure to fat gain across a wide age range of men and under varied management strategies.
The authors observed a trend for an insulin-lowering effect for men in the POWIR arm but no effect on other biomarkers. Two controlled exercise trials in PCSs undergoing ADT found no influence of aerobic and resistance training on insulin levels (Cormie et al., 2014; Galvão et al., 2010). Compared to the three-month combined programs in other trials, the POWIR program was of similar intensity (resistance workloads of 8–12 RM for POWIR and 6–12 RM for other trials) but included a greater amount of muscle-loading (resistance) exercise (50 minutes in POWIR versus 30 minutes in other trials) and was three times longer in duration. Controlled trials in older adults without cancer have demonstrated an insulin-lowering effect of resistance training alone (Flack et al., 2010); therefore, the length of a training program may be a more important feature of an exercise prescription than the duration of resistance exercise within a single session. Moderator analyses did not show any influence of ADT regimen on changes in biomarkers; however, age had a significant influence. POWIR appeared to be most effective at preventing increases in insulin among men in the younger age range of the sample, but this effect diminished with increasing age. Although physiologic aging could underlie the dampened insulin-lowering effect of POWIR, it also is reasonable to consider that older men were not training at the same level of effort as younger men. Age was not correlated with class attendance, but inspection of the strength data showed a significant inverse correlation between age and change in maximum strength (r = –0.48, p < 0.01; unpublished data). To achieve consistent benefits from exercise training across men of all ages, strategies to ensure that older men can maintain training volume, particularly intensity, over time will be important.
The authors explored a potential mediating effect of changes in body fat on changes in biomarkers across the intervention and found that the insulin-lowering effect of POWIR was exerted through loss of body fat, particularly through decreases in trunk fat mass, a measure indicative of central adiposity. Several potential mechanisms have been proposed to explain the link between physical activity and prostate cancer survival including decreased adiposity and associated decreases in systemic inflammatory cytokines and metabolic hormones (McTiernan, 2008). Adiposity can create low-level systemic inflammation that stimulates insulin resistance and hyperinsulinemia, promoting an environment for cancer progression (Ballard-Barbash et al., 2012). Increases in body fat and central adiposity with age are associated with hyperinsulinemia and glucose intolerance (Coon, Rogus, Drinkwater, Muller, & Goldberg, 1992). Although weight loss was not a primary aim of the study, resistance training can result in loss of body fat and reductions in central adiposity (Deschenes & Kraemer, 2002). Resistance training is a recommended form of exercise to prevent or manage diabetes because it is an effective training modality to reduce abdominal fat and improve glucose tolerance (Flack et al., 2010). Although preliminary, the finding that loss of total and central body fat mediated reductions in circulating insulin from resistance training provides beginning insight about one potential mechanism by which physical activity could affect prostate progression and should be considered in the design of future trials that address biobehavioral approaches to extend cancer survival.
Strengths and Limitations
The current study had notable strengths and limitations. This study was the first to examine the additional potential benefits of an exercise program that was designed to combat ADT-related bone loss in PCSs. More than 75% of PCSs fail to achieve recommended amounts of aerobic exercise, and only 4% engage in any resistance exercise (Bellizzi, Rowland, Jeffery, & McNeel, 2005; Coups & Ostroff, 2005; Richman et al., 2011). Therefore, PCSs, most of whom are older, are unlikely to engage in multiple types of exercise programs to achieve different benefits. By exploring whether or not a single exercise modality can affect multiple outcomes that are relevant to quality of life and disease progression, clinicians could more easily prescribe exercise to patients, and patients may be more likely to comply. The current study is one of few controlled trials to examine moderators and mediators of exercise-induced changes in biomarkers of cancer progression. Identifying moderators of the exercise response provides knowledge about whether or not benefits are independent of influences, such as age or ADT dosing regimen, or whether benefits are more likely in certain subgroups or conditions. By exploring a mediating effect of body fat on exercise-induced insulin changes, the authors found preliminary evidence for a mechanism by which exercise might reduce insulin among men undergoing ADT and could suggest that designing exercise programs for weight loss may be particularly effective at reducing biomarkers of disease progression. In addition, the POWIR program was of sufficient length to explore changes in response to longer-term (i.e., greater than three months) exercise and may explain why other, shorter programs failed to favorably shift insulin levels. Retention and adherence to the 12-month program was good, particularly among older men with multiple comorbidities, demonstrating that POWIR could be a sustainable exercise program for PCSs undergoing ADT. However, the study also had notable limitations. The sample size, although similar to those in comparable exercise trials, was not large. The authors enrolled the minimum sample size to detect group differences in body fat and, despite a low dropout rate, this may explain why differences between the groups only approached significance on several outcomes. Therefore, the findings should be considered preliminary and need to be confirmed by a properly powered, controlled trial that is also designed to examine potential mediator and moderator effects. The authors of the current study only explored a limited number and type of biomarkers associated with prostate cancer progression. Other markers, such as inflammatory cytokines, adipokines, and myokines, have been posited as potential mechanisms that explain the link between physical activity and cancer survival (Basaria & Bhasin, 2012; McTiernan, 2008; Neilson, Friedenreich, Brockton, & Millikan, 2009). Future trials should include a more comprehensive set of biomarkers that might better capture the mechanism through which exercise affects cancer progression.
Implications for Nursing
Oncology nurses are an influential member of the care team for PCSs and can make important recommendations for lifestyle modification for cancer survivors. Nurses caring for PCSs, who are mostly older, should counsel their patients on the benefits of exercise, particularly resistance training, that could extend to prolonging survival from cancer and from other causes, such as comorbid conditions, fractures, and disability. In conjunction with other healthcare professionals (e.g., physical therapists, exercise physiologists) nurses can create an exercise prescription that considers PCSs’ needs, preferences, abilities, and limitations. Nurses can then monitor and support PCSs to maintain a long-term exercise program.
Conclusions
The findings from this study provide preliminary evidence that POWIR, a 12-month exercise program of resistance and impact training, can reduce body fat and central adiposity that lowers circulating insulin levels in PCSs undergoing ADT. Because evidence of the benefits of exercise for cancer survivors extends to consider a potential influence on disease progression, the mechanisms that underpin such benefits must be identified to substantiate the link between exercise and survival from observation studies. This study suggests that POWIR could be a specific and effective exercise program that addresses multiple consequences of ADT because of its feasibility and its potential to become a routine component of the care of men with advanced prostate cancer.
References
Ainsworth, B.E., Haskell, W.L., Herrmann, S.D., Meckes, N., Bassett, D.R., Jr., Tudor-Locke, C., . . . Leon, A.S. (2011). 2011 Compendium of Physical Activities: A second update of codes and MET values. Medicine and Science in Sports and Exercise, 43, 1575–1581. doi:10.1249/MSS.0b013e31821ece12
Ballard-Barbash, R., Friedenreich, C.M., Courneya, K.S., Siddiqi, S.M., McTiernan, A., & Alfano, C.M. (2012). Physical activity, biomarkers, and disease outcomes in cancer survivors: A systematic review. Journal of the National Cancer Institute, 104, 815–840. doi:10.1093/jnci/djs207
Basaria, S., & Bhasin, S. (2012). Targeting the skeletal muscle-metabolism axis in prostate-cancer therapy. New England Journal of Medicine, 367, 965–967. doi:10.1056/NEJMcibr1203160
Bellizzi, K.M., Rowland, J.H., Jeffery, D.D., & McNeel, T. (2005). Health behaviors of cancer survivors: Examining opportunities for cancer control intervention. Journal of Clinical Oncology, 23, 8884–8893. doi:10.1200/JCO.2005.02.2343
Bennett, J.A., Young, H.M., Nail, L.M., Winters-Stone, K., & Hanson, G. (2008). A telephone-only motivational intervention to increase physical activity in rural adults: A randomized controlled trial. Nursing Research, 57, 24–32. doi:10.1097/01.NNR.0000280661.34502.c1
Block, G., Thompson, F.E., Hartman, A.M., Larkin, F.A., & Guire, K.E. (1992). Comparison of two dietary questionnaires validated against multiple dietary records collected during a 1-year period. Journal of the American Dietetic Association, 92, 686–693.
Cao, Y., & Ma, J. (2011). Body mass index, prostate cancer–specific mortality, and biochemical recurrence: A systematic review and meta-analysis. Cancer Prevention Research, 4, 486–501. doi:10.1158/1940-6207.CAPR-10-0229
Charlson, M.E., Pompei, P., Ales, K.L., & MacKenzie, C.R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40, 373–383. doi:10.1016/0021-9681(87)90171-8
Chodzko-Zajko W.J., Proctor, D.N., Fiatarone Singh, M.A., Minson, C.T., Nigg, C.R., Salem, G.J., & Skinner, J.S. (2009). American College of Sports Medicine position stand. Exercise and physical activity for older adults. Medicine and Science in Sports and Exercise, 41, 1510–1530. doi:10.1249/MSS.0b013e3181a0c95c
Coon, P.J., Rogus, E.M., Drinkwater, D., Muller, D.C., & Goldberg, A.P. (1992). Role of body fat distribution in the decline in insulin sensitivity and glucose tolerance with age. Journal of Clinical Endocrinology and Metabolism, 75, 1125–1132.
Cormie, P., Galvão, D.A., Spry, N., Joseph, D., Chee, R., Taaffe, D.R., & Newton, R.U. (2015). Can supervised exercise prevent treatment toxicity in patients with prostate cancer initiating androgen-deprivation therapy: A randomised controlled trial. BJU International, 115, 256–266. doi:10.1111/bju.12646
Coups, E.J., & Ostroff, J.S. (2005). A population-based estimate of the prevalence of behavioral risk factors among adult cancer survivors and noncancer controls. Preventive Medicine, 40, 702–711. doi:10.1016/j.ypmed.2004.09.011
Deschenes, M.R., & Kraemer, W.J. (2002). Performance and physiologic adaptations to resistance training. American Journal of Physical Medicine and Rehabilitation, 81(Suppl.), S3–S16. doi:10.1097/00002060-200211001-00003
Flack, K.D., Davy, K.P., Hulver, M.W., Winett, R.A., Frisard, M.I., & Davy, B.M. (2010). Aging, resistance training, and diabetes prevention. Journal of Aging Research, 2011, 127315.
Galvão, D.A., Taaffe, D.R., Spry, N., Joseph, D., & Newton, R.U. (2010). Combined resistance and aerobic exercise program reverses muscle loss in men undergoing androgen suppression therapy for prostate cancer without bone metastases: A randomized controlled trial. Journal of Clinical Oncology, 28, 340–347. doi:10.1200/JCO.2009.23.2488
Gong, Z., Agalliu, I., Lin, D.W., Stanford, J.L., & Kristal, A.R. (2007). Obesity is associated with increased risks of prostate cancer metastasis and death after initial cancer diagnosis in middle-aged men. Cancer, 109, 1192–1202. doi:10.1002/cncr.22534
Haseen, F., Murray, L.J., Cardwell, C.R., O’Sullivan, J.M., & Cantwell, M.M. (2010). The effect of androgen deprivation therapy on body composition in men with prostate cancer: Systematic review and meta-analysis. Journal of Cancer Survivorship, 4, 128–139. doi:10.1007/s11764-009-0114-1
Keating, N.L., O’Malley, A.J., Freedland, S.J., & Smith, M.R. (2010). Diabetes and cardiovascular disease during androgen deprivation therapy: Observational study of veterans with prostate cancer. Journal of the National Cancer Institute, 102, 39–46.
Kenfield, S.A., Stampfer, M.J., Giovannucci, E., & Chan, J.M. (2011). Physical activity and survival after prostate cancer diagnosis in the health professionals follow-up study. Journal of Clinical Oncology, 29, 726–732. doi:10.1200/JCO.2010.31.5226
Kohrt, W.M., Bloomfield, S.A., Little, K.D., Nelson, M.E., & Yingling, V.R.(2004). American College of Sports Medicine position stand: Physical activity and bone health. Medicine and Science in Sports and Exercise, 36, 1985–1996. doi:10.1249/01.MSS.0000142662.21767.58
Kohut, M.L., McCann, D.A., Russell, D.W., Konopka, D.N., Cunnick, J.E., Franke, W.D., . . . Vanderah, E. (2006). Aerobic exercise, but not flexibility/resistance exercise, reduces serum IL-18, CRP, and IL-6 independent of beta-blockers, BMI, and psychosocial factors in older adults. Brain, Behavior, and Immunity, 20, 201–209. doi:10.1016/j.bbi.2005.12.002
Kraemer, W.J., Häkkinen, K., Newton, R.U., Nindl, B.C., Volek, J.S., McCormick, M., . . . Evans, W.J. (1999). Effects of heavy-resistance training on hormonal response patterns in younger vs. older men. Journal of Applied Physiology, 87, 982–992.
McTiernan, A. (2008). Mechanisms linking physical activity with cancer. Nature Reviews. Cancer, 8, 205–211. doi:10.1038/nrc2325
Miller, C.T., Fraser, S.F., Levinger, I., Straznicky, N.E., Dixon, J.B., Reynolds, J., & Selig, S.E. (2013). The effects of exercise training in addition to energy restriction on functional capacities and body composition in obese adults during weight loss: A systematic review. PLoS One, 8, e81692. doi:10.1371/journal.pone.0081692
Neilson, H.K., Friedenreich, C.M., Brockton, N.T., & Millikan, R.C. (2009). Physical activity and postmenopausal breast cancer: Proposed biologic mechanisms and areas for future research. Cancer Epidemiology, Biomarkers and Prevention, 18, 11–27. doi:10.1158/1055-9965.EPI-08-0756
Prins, R.C., Rademacher, B.L., Mongoue-Tchokote, S., Alumkal, J.J., Graff, J.N., Eilers, K.M., & Beer, T.M. (2012). C-reactive protein as an adverse prognostic marker for men with castration-resistant prostate cancer (CRPC): Confirmatory results. Urologic Oncology, 30, 33–37. doi:10.1016/j.urolonc.2009.11.012
Richman, E.L., Kenfield, S.A., Stampfer, M.J., Paciorek, A., Carroll, P.R., & Chan, J.M. (2011). Physical activity after diagnosis and risk of prostate cancer progression: Data from the cancer of the prostate strategic urologic research endeavor. Cancer Research, 71, 3889–3895. doi:10.1158/0008-5472.CAN-10-3932
Segal, R.J., Reid, R.D., Courneya, K.S., Malone, S.C., Parliament, M.B., Scott, C.G., . . . Wells, G.A. (2003). Resistance exercise in men receiving androgen deprivation therapy for prostate cancer. Journal of Clinical Oncology, 21, 1653–1659. doi:10.1200/JCO.2003.09.534
Stewart, A.L., Mills, K.M., King, A.C., Haskell, W.L., Gillis, D., & Ritter, P.L. (2001). CHAMPS physical activity questionnaire for older adults: Outcomes for interventions. Medicine and Science in Sports and Exercise, 33, 1126–1141. doi:10.1097/00005768-200107000-00010
Tofighi, D., & MacKinnon, D.P. (2011). RMediation: An R package for mediation analysis confidence intervals. Behavior Research Methods, 43, 692–700. doi:10.3758/s13428-011-0076-x
Winters, K.M., & Snow, C.M. (2000). Detraining reverses positive effects of exercise on the musculoskeletal system in premenopausal women. Journal of Bone and Mineral Research, 15, 2495–2503. doi:10.1359/jbmr.2000.15.12.2495
Winters-Stone, K.M., Dobek, J., Nail, L., Bennett, J.A., Leo, M.C., Naik, A., & Schwartz, A. (2011). Strength training stops bone loss and builds muscle in postmenopausal breast cancer survivors: A randomized controlled trial. Breast Cancer Research and Treatment, 127, 447–456. doi:10.1007/s10549-011-1444-z
Winters-Stone, K.M., Dobek, J.C., Bennett, J.A., Maddalozzo, G.F., Ryan, C.W., & Beer, T.M. (2014). Skeletal response to resistance and impact training in prostate cancer survivors. Medicine and Science in Sports and Exercise, 46, 1482–1488. doi:10.1249/MSS.0000000000000265
Winters-Stone, K.M., Dobek, J.C., Bennett, J.A., Maddalozzo, G.F., Ryan, C.W., & Beer, T.M. (2015). Resistance training reduces disability in prostate cancer survivors on androgen deprivation therapy: Evidence from a randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 96, 7–14. doi:10.1016/j.apmr.2014.08.010
Winters-Stone, K.M., Dobek, J., Bennett, J.A., Nail, L.M., Leo, M.C., & Schwartz, A. (2012). The effect of resistance training on muscle strength and physical function in older, postmenopausal breast cancer survivors: A randomized controlled trial. Journal of Cancer Survivorship, 6, 189–199. doi:10.1007/s11764-011-0210-x
Winters-Stone, K.M., Dobek, J., Nail, L.M., Bennett, J.A., Leo, M.C., Torgrimson-Ojerio, B., . . . Schwartz, A. (2013). Impact + resistance training improves bone health and body composition in prematurely menopausal breast cancer survivors: A randomized controlled trial. Osteoporosis International, 24, 1637–1646. doi:10.1007/s00198-012-2143-2
About the Author(s)
Kerri M. Winters-Stone, PhD, is a research professor in the School of Nursing in Knight Cancer Institute and Nathan Dieckmann, PhD, is an assistant professor in the School of Nursing, both at Oregon Health and Science University (OHSU) in Portland; Gianni F. Maddalozzo, PhD, is a senior instructor in the Department of Exercise and Sport Science at Oregon State University in Corvallis; and Jill A. Bennett, PhD, RN, is a professor in the School of Nursing, and Christopher W. Ryan, MD, and Tomasz M. Beer, MD, are professors in the School of Medicine, all in Knight Cancer Institute at OHSU. No financial relationships to disclose. Winters-Stone can be reached at wintersk@ohsu.edu, with copy to editor at ONFEditor@ons.org. (Submitted November 2014. Accepted for publication January 16, 2015.)

