Text Messaging May Improve Abnormal Mammogram Follow-Up in Latinas
Purpose/Objectives: To develop and pilot test a text message notification process to reduce follow-up time for women with abnormal mammograms.
Design: Formative analysis; randomized trial with delayed intervention control group.
Setting: Tiburcio Vasquez Health Clinic (TVHC), a federally qualified health center in Hayward, California.
Sample: 29 Spanish-speaking Latinas with abnormal mammograms.
Methods: A Spanish text message was developed based on findings from two focus groups and five interviews with TVHC healthcare providers. Thirteen women were assigned to receive text messages within 24 hours of receipt of abnormal mammogram by TVHC (intervention group) and 16 to receive text messages four weeks later (delayed intervention group).
Main Research Variables: Number of days between the abnormal mammogram and the return for follow-up appointment.
Findings: The median number of days from the abnormal mammogram report to the return for follow-up was 23 days for the intervention group and 59 days for the delayed intervention group (p = 0.0569).
Conclusions: This study successfully developed a text message that, in Latinas, may decrease the time from receipt of an abnormal mammogram report to attendance at a follow-up visit.
Implications for Nursing: This simple, low-cost approach could result in earlier detection of breast cancers, lowering morbidity and mortality among Latinas.
Jump to a section
The need exists for significantly improved follow-up care among Latina women who have received an abnormal mammogram. Although breast cancer incidence is lower for Latina women, they are more likely to be diagnosed with an advanced stage of breast cancer and are 20% more likely to die of breast cancer than non-Hispanic Caucasian women (American Cancer Society, 2012; Lantz et al., 2006). Foreign-born Hispanics are more likely than U.S.-born Hispanics to be diagnosed at an advanced stage (Keegan, Quach, Shema, Glaser, & Gomez, 2010), and women of Mexican origin were found to be at high risk for early onset, premenopausal breast cancer (Miranda et al., 2011). Latina Americans are more likely than European Americans, African Americans, or Asian Americans to report diagnostic delays (Ashing-Giwa et al., 2010), which is highly relevant because more than half of all women aged 50–69 years have an abnormal mammogram result (Karliner, Patricia Kaplan, Juarbe, Pasick, & Pérez-Stable, 2005). Timely initiation of diagnosis and treatment following abnormal mammography results has been shown to improve survival, and it may help to lessen the mortality differences among racial and ethnic groups (Gorin, Heck, Cheng, & Smith, 2006). The population growth of Latinas in the United States—to more than 128 million by 2060—makes diagnostic delays a significant public health concern (U.S. Census Bureau, 2012).
Follow-up of abnormal mammograms in specific populations is often poor for multiple reasons that may be based on system or individual barriers. Community health centers are often underfunded and overstretched, leading to as many as 34% of abnormal results without adequate documentation for follow-up (Chen, Eder, Elder, & Hickner, 2010). Key drivers of follow-up are a physician-documented plan and understanding of this plan by the patient (Poon et al., 2004). However, only 51% of women with a suspicious abnormality detected during mammography understood their results to be abnormal (Karliner et al., 2005). This percentage may be even lower among recent immigrants, as well as those with limited English skills and lower education levels. In particular, Hispanic ethnicity and low income have been shown to be associated with longer wait times between the abnormal mammogram result and diagnostic follow-up compared to non-Hispanic Caucasian women (Press, Carrasquillo, Sciacca, & Giardina, 2008). Among a group of 11,000 low-income women enrolled in a free statewide screening program, a retrospective case-control analysis revealed that of the 37% who required follow-up, 30% experienced delays of more than 60 days, and Hispanic and African American women were more likely than Caucasian women to experience delays (Wujcik et al., 2009). Another study of 970 minority women showed that the median time to diagnosis was 183 days for Breast Imaging-Reporting and Data System (BI-RADS) 3, and that income and an incomplete understanding of the mammogram results were associated with significant delays (Pérez-Stable et al., 2013). The medium of the message is also relevant; women notified in person or by telephone have been found to be more likely than women notified in writing to understand their results (Karliner et al., 2005). In particular, patients need clear messages about recommendations for abnormal screening follow-up when multiple healthcare providers are involved (Zapka et al., 2004); this is often the case in community care in which mammogram referrals may be made to outside facilities.
Reminder systems have been shown to enhance the likelihood of attendance at mammography examinations (Leirer, Tanke, & Morrow, 1992; Steele, 1999). In addition, text messages improve compliance with medical guidelines (McBride & Rimer, 1999; Stehr-Green, Dini, Lindegren, & Patriarca, 1993; Taplin et al., 2000), and the majority of Americans have a mobile phone (Dang, Estrada, Bresee, & Phillips, 2013; International Telecommunication Union, 2012; Price et al., 2013; Smith, 2011). However, no randomized trials testing interventions to increase follow-up of abnormal mammogram results have been reported in the literature (Bastani, Mojica, Berman, & Ganz, 2010).
This research was guided by a modified and condensed version of the Precede-Proceed model (Green & Kreuter, 1991). This model looks to change health behavior through a systematic planning process that empowers individuals with understanding, motivation, and skills and active engagement in community affairs to improve their quality of life. Multiple steps are involved in follow-up after an abnormal mammogram (Taplin, Yabroff, & Zapka, 2012; Zapka, Taplin, Price, Cranos, & Yabroff, 2010). The current authors’ pilot project intervened at the first point of result reporting and, because of community input, was designed to provide both study arms with an intervention.
Methods
Focus Groups
To assess the patient perspective on program acceptability, content, and methods of implementation, the current authors conducted two one-hour focus group meetings. Both groups were facilitated in Spanish by the Community Advisory Board (CAB) chair. Eight breast cancer survivors attended the first group meeting; all were members of an existing breast cancer support group. The second focus group meeting involved five women who had received an abnormal mammogram but had not been diagnosed with cancer. These women were referred by cancer survivors and the CAB. In addition to asking the women about linking their own behaviors to scheduling and attending an appointment to discuss their abnormal mammogram, the current authors asked them open-ended questions in the following categories: (a) response to abnormal mammogram, (b) attitudes toward cell phone messages, (c) content of cell phone messages, and (d) supporting materials. Focus group members were also asked if they were willing to become “rapid testers” to receive and evaluate test text messages. The focus group meetings were recorded, transcribed, and translated into English by a bilingual employee who also observed the meetings in person. Two of the current authors reviewed the transcripts, as well as coded the transcripts and identified themes.
Rapid Testers
Five text messages were developed and tested with six focus group participants who had signed a consent form to participate as rapid testers. Each rapid tester was contacted by telephone to remind her about the text message protocol. Subsequently, one text message was sent each day with specific instructions about providing feedback. After all text messages had been sent, each rapid tester was again contacted by telephone to provide verbal feedback in Spanish or English about the messages. The current authors also obtained input from the CAB and the Tiburcio Vasquez Health Clinic (TVHC) in Hayward, California, in regards to selecting the more effective of two messages identified by the rapid testers. This message was then translated into Spanish by one of the CAB members and back-translated by a bicultural and bilingual staff member of the Cancer Prevention Institute of California (CPIC) in Fremont.
Semistructured Interviews
The current authors completed five semistructured interviews with healthcare providers at TVHC who had referred Latina women for mammography. The same interviewer completed all of the interviews with three primary care providers, a medical assistant, and the supervising nurse. The interviews were conducted and recorded in English, and then transcribed. Two of the current authors reviewed and coded the transcripts to identify themes.
Randomized Pilot Test
The prospective randomized pilot test comparing the text message identified through the current authors’ formative research involved two groups: an intervention group and a delayed intervention group, the latter of which served as a pseudo-control group. All patients at TVHC clinics were offered informed consent for text messaging and clinical care as part of the general consent form used at patient intake. This consent process was reviewed and approved by the CPIC Institutional Review Board (IRB) upon which TVHC relied because TVHC did not have one in place. The CPIC IRB determined that obtaining additional consent for women who had an abnormal mammogram to participate in the study was not necessary because no personal health information was transmitted from TVHC to CPIC; in addition, the standard TVHC consent for treatment already included consent to receive text messages related to their medical care by TVHC as their healthcare provider, and current usual care would continue to be provided for all participants. The IRB and the CAB also felt that an additional consent process would serve as a reminder about the abnormal mammogram, potentially compromising the study because the consent itself could perhaps serve as an intervention.
Women eligible for the study needed to be Spanish speaking and Latina, have a signed clinic and medical care consent on file at TVHC, and have received an abnormal mammogram report. Abnormal mammograms were defined as BI-RADS 3 and above. No changes were made to the clinic’s methods for notifying patients of their abnormal mammogram or to their care, nor to any of the mammography facilities’ procedures for notifications. The text message was in addition to usual care notifications in place at the time of the study. Usual care notifications varied by practitioner; practitioners or their assistants attempted to call women but mentioned the difficulty of reaching their patients. An employee of TVHC checked daily for eligible women and assigned them a sequential study identification number (ID) according to the time of their abnormal report. This ID was used to assign women to either the intervention group (odd-numbered IDs) or the delayed intervention group (even-numbered IDs). The identical text message was sent as many as four times, except when a weekend or holiday intervened to avoid frustration on the part of recipients who attempted to respond to the message when the clinic was closed (see Figure 1). Messages ceased as soon as the recipient scheduled a follow-up appointment or called and requested that they stop.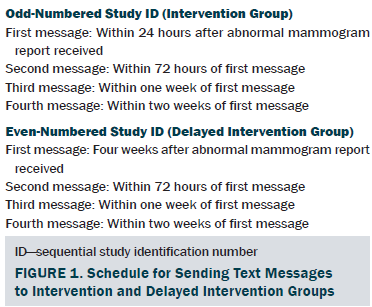
Data were transmitted from TVHC to CPIC with no personal health information included. CPIC data contained only study IDs, eligibility criteria, and the number of days from the receipt of the abnormal mammogram report at TVHC to each event, including the number of days to each message and the number of days to the follow-up appointment.
Results
Focus Groups: Breast Cancer Survivors or Women Who Had an Abnormal Mammogram
Both focus groups were conducted in November 2012. The first focus group, made up of breast cancer survivors, had eight participants. The average age of participants was 47.5 years. The average number of years of school completed was 7.9. The second focus group, consisting of women who had an abnormal mammogram with no subsequent cancer, consisted of five women, with an average age of 46.3 years. The average number of years of school completed was 10.8. The majority in both groups were monolingual Spanish speakers from Mexico. One member of each group was bilingual, and one member of each group was from a South or Central American country. Only three participants recalled receiving a letter from the mammography facility.
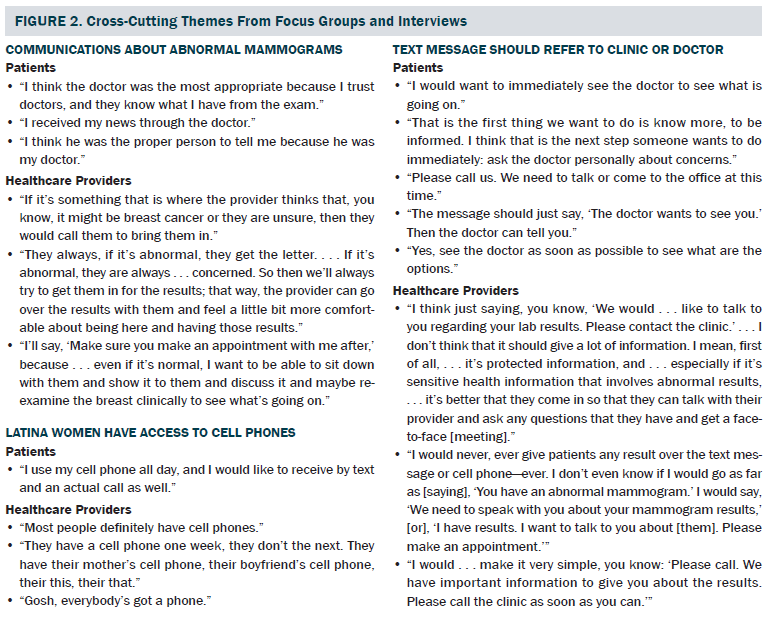
In both focus groups, 11 participants wanted the text message to tell them that the mammogram was abnormal, and 12 wanted to meet with their doctor for additional discussion about the abnormal results. As soon as they heard about the abnormal results, eight participants mentioned a fear of cancer, as well as a need for additional information in writing about an abnormal mammogram, including options for the next step.
Rapid Testers: Subset of Focus Group Participants
Six rapid testers were recruited from the focus groups for testing specific text messages. Three of these rapid testers had had breast cancer, and three had an abnormal mammogram but no cancer. The six rapid testers preferred two of the messages; to decide between the two, the CAB and TVHC provided their perspectives. One message (“The Tiburcio Vasquez clinic would like to speak with you about your exam results. Please call XXX-XXX-XXXX for an appointment”) was selected for use in the pilot test and approved for use by the CPIC IRB in July 2013. The message was translated into Spanish by a CAB member and back-translated by a bicultural, bilingual CPIC staff member for use in the pilot test.
Semistructured Interviews With Healthcare Providers
In October and November 2012, the current authors completed five semistructured interviews with healthcare providers at TVHC who had referred Latina women for mammography. All participants agreed that patients typically have access to cell phones and are familiar with how to use them, including retrieving text messages. Participants did warn that phone numbers may be changed frequently because patients often purchase inexpensive, “pay-as-you-go” phones and do not notify TVHC when they obtain a new phone with a different number. A majority (four out of five respondents) felt that the text message should provide minimal information; one respondent noted that the message could offer information about the importance of additional testing. In addition, healthcare providers responded that the message should include a specific phone number that patients could use to ask questions.
The current authors found that two of the three primary healthcare providers preferred to have women return to see them for a face-to-face discussion about their mammogram results, particularly if the abnormal result indicated the possibility of breast cancer. Another finding was that the existing process for notifying women of an abnormal mammogram varied. Some healthcare providers attempted to call patients themselves or have their medical assistants contact patients, but many noted difficulties in reaching patients, as well as in leaving a message that did not reveal personal health information. Healthcare providers noted that mammography facilities sometimes send letters directly to patients, but the timeliness, language, and literacy level of those letters vary by the facility where the patient received her mammogram (all TVHC patients are referred to other facilities for their actual mammogram).
Themes Identified in Focus Groups and Semistructured Interviews
Three major cross-cutting themes were identified from the focus groups with patients and the semistructured interviews with healthcare providers: (a) detailed communications about abnormal mammograms should be provided by the clinician, ideally in person; (b) Latina women have access to cell phones; and (c) the content of the text message should be very brief and should refer the woman to contact the clinic (see Figure 2). One unexpected result was the need for additional information about what an abnormal mammogram is, as expressed by most focus group members and discussed by several healthcare providers. The patients described the anxiety they felt, as well as the limited information they knew, from the time that they received the results of their abnormal mammogram to when they were able to complete their follow-up procedures. One focus group member elaborated on these feelings.
During that two-week period . . . the worry is so much. I think they should give some sort of follow-up—[offer] information, mail a brochure . . . [say], “Look, don’t worry because it could be this or this.” Like when you have pre-diabetes, they tell you, “These are the risks, do exercise, do this, do that.” They give you follow-up information, something you can actually do. With [an abnormal mammogram], they don’t. They don’t mail you anything. They just tell you to wait for the appointment. The worry is huge. I think they need to mail some sort of information, or at least if you have questions, [they should tell you to] go to this website or call this number. There should be a number that you can call to get informed because you do worry a lot, and you ask yourself a thousand questions.
Pilot Test
The current authors enrolled 31 Spanish-speaking Latina women with abnormal mammograms into the study. Of these women, 15 were assigned to receive text messages within 24 hours of when TVHC obtained the abnormal mammogram report (intervention group), and 16 were assigned to receive text messages four weeks later (delayed intervention group). The average age of women in the delayed intervention group was 51.9 years, compared to 53.1 years in the intervention group. No additional demographic information was collected from women enrolled in the study.
Two women in the intervention group had to be excluded from the study. One woman was excluded because she did not reapply for her health coverage and went elsewhere; the other woman was excluded because she had received adequate clinical input (she already understood that she only required a repeat mammogram in six months) at her original appointment, and no need existed for a follow-up visit. These exclusions resulted in a total of 13 women in the intervention group. Only one woman in each group was reached on a cell phone belonging to another member of the family; in both cases, the other family member was a daughter. In all other instances, the cell phone belonged to the woman herself.
On average, women in the intervention group returned for their follow-up appointment 23 days sooner than women in the delayed intervention group (see Table 1). The median number of days from receipt of the abnormal mammogram report to return for follow-up for the delayed intervention group was 59 days with an interquartile range (IQR) from 35.5 days at the 25th percentile to 69.5 days at the 75th percentile. The median number of days for the intervention group was 23 with an IQR from 16–46 days. The difference between the two groups in the median number of days to return for the follow-up appointment was 36 days (p = 0.0569). 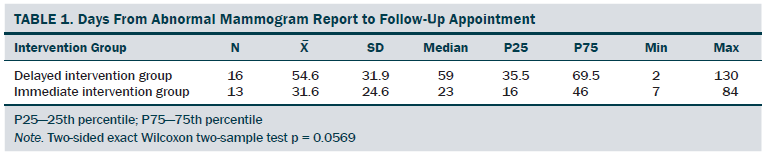
Discussion
To the current authors’ knowledge, this study is the first that uses Spanish text messages designed todecrease the delay from an abnormal mammogram report to follow-up. In this study, the current authors pilot tested text messages to Spanish-speaking Latina women with abnormal mammograms who were patients at TVHC, a federally qualified health center. The current authors found that Latina women had a high rate of individual cell phone ownership; however, they did not observe the concerns of healthcare providers that cell phones are shared by family members or that phone numbers change frequently. In agreement with other research (Davis & Oakley-Girvan, 2015), focus group members and healthcare providers felt that the text message should be short and refer the patient back to the clinic or doctor. The current authors also documented that focus group members were anxious about results in the interim from the receipt of mailed abnormal mammogram results to completion of their follow-up appointment; the lack of information was stressful. This may be a particularly relevant factor to consider in this population; a study by Molina, Beresford, Espinoza, and Thompson (2014) found that Latinas experienced greater psychological distress and social withdrawal compared to non-Latina Caucasians with receipt of an abnormal mammogram. In addition, a systematic literature review and meta-analysis found that Hispanic patients with cancer in the United States report significantly worse distress compared to Caucasians or other racial or ethnic groups (Luckett et al., 2011).
This study successfully developed a text message that, in a larger study of Latinas or with a control group that does not receive even delayed text messages, may show statistically significant decreases in the amount of time from receipt of an abnormal mammogram report to attendance at a follow-up visit with the healthcare provider. Although the current authors’ pilot study results did not achieve statistical significance, both intervention groups experienced a much shorter median delay (23 days for immediate intervention and 59 days for delayed intervention) compared with a median time to diagnosis of 183 days for BI-RADS 3 documented in another study (Pérez-Stable et al., 2013). Comparing the current authors’ results to those from another study of urban minority women with abnormal mammograms in which 22% (n = 11) members of the control group were still without a final diagnosis at 60 days (Ferrante, Chen, & Kim, 2008) provides reasonable indication that early intervention rather than delayed intervention is important. Although results in this pilot study were not statistically significant, they are encouraging given the small sample size and the large difference in mean and median days between the two groups. This study’s ability to use early intervention text messaging to move follow-up appointments forward is encouraging. Implementation of simple, low-cost text messaging may result in earlier detection of breast cancers, lowering morbidity and mortality among Latinas.
Strengths of the current study include formative analysis to increase understanding of concerns among Spanish-speaking women who have received an abnormal mammogram result and receipt of input to develop a text message for this population. The current authors included a CAB with representation of organizations serving this population and conducted the research at a federally qualified health center that provides medical services to a low-income and primarily Latino population. During the time period of the study, which was prior to the Patient Protection and Affordable Care Act, only one of the women experienced difficulties with health insurance.
Limitations
Several limitations exist with the study. This study was a pilot test of a text message, and the sample was limited to 29 Spanish-speaking Latina women who had received an abnormal mammogram result. Women eligible for the study had to have an abnormal mammogram, but no additional information was given about whether the mammogram was screening versus diagnostic. However, given the randomization scheme, differential distribution of diagnostic mammograms is unlikely. The current authors also used only one text message sent as many as four times instead of comparing approaches or messages. The text message did not mention anything about an abnormal mammogram because of feedback from healthcare providers who felt that other members of the family occasionally read text messages intended for someone else. Consequently, some women may not have understood to which examination the text message referred.
Because of limited funding and a basic phone system setup, the current authors were unable to obtain the date on which women called TVHC to make a follow-up appointment after receiving the text message. This information would have helped to determine the immediacy of response but was not available using the phone system in place at TVHC. Difficulties in scheduling an appointment could have been a major factor in delays, but the current authors have no reason to believe that a structural difference in scheduling between the immediate intervention and the delayed intervention group existed. The current authors would have liked to collect income and education data, as well as other variables (e.g., personal and family history of cancer) and comorbidities from the pilot test subjects, but Health Insurance Portability and Accountability Act confidentiality requirements and cost concerns prohibited this in the pilot design. The average age of participants in the intervention and control groups was not statistically different, and women were alternately assigned to the two groups, so the current authors expect that, in terms of other demographic variables, the groups were comparable.
Implications for Nursing
Latinas frequently experience delays in definitive diagnosis following an abnormal mammogram report (Ashing-Giwa et al., 2010; Chen et al., 2010; Press et al., 2008). They often do not understand what an abnormal mammogram means (Karliner et al., 2005); for perhaps this reason, Latinas experience levels of anxiety higher than other ethnic groups after receipt of an abnormal mammogram report (Molina et al., 2014). This pilot randomized study expands the understanding of Spanish-speaking Latinas who have received an abnormal mammogram report, as well as contributes to the limited interventional research in this population. Results demonstrate that most Latinas use cell phones (Dang et al., 2013; Price et al., 2013) and are willing to receive text messages from a federally qualified health clinic. For the first time, this study provides preliminary data that text messages may reduce the number of days from the receipt of the abnormal mammogram report to attendance at a healthcare provider-led follow-up visit. The current authors recommend evaluating the time to definitive resolution among larger samples with the statistical power to test for interaction among key variables. A need also exists to provide more education related to breast cancer prevention and early detection—more specifically, information about what an abnormal mammogram means in a culturally appropriate and linguistically acceptable manner. Healthcare providers’ adoption of text messaging for appointment reminders and prompts to follow up on abnormal examinations could eventually lead to decreases in breast cancer morbidity and mortality.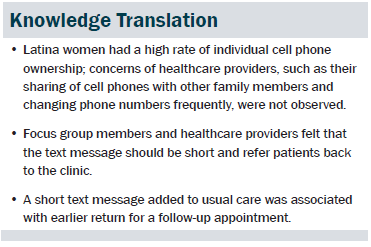
Conclusion
This research addresses the understudied topic of text messaging reminder systems for Latina patients to ensure high-quality and timely follow-up of abnormal mammogram results. This approach was built in conjunction with the needs of overburdened, understaffed, and underfunded health clinics, such as TVHC. The current authors hypothesized that harnessing the power of mobile applications to deliver reminder texts could reduce the observed healthcare gap and improve outcomes. Specifically, in this analysis, the current authors found that a short text message encouraged earlier return for follow-up physician appointment, suggesting that the message altered behavior and resulted in shorter time to discussion of medical results. These findings are similar to others described in a review of mHealth that text messages can improve compliance with medical recommendations (Davis & Oakley-Girvan, 2015). In this limited time frame pilot study, the current authors did not explore whether the text messaging program decreased time to definitive diagnosis. However, the results of this study provide encouraging support to investigate whether a tailored text messaging approach in a larger sample can reduce time to definitive diagnosis and, consequently, affect mortality. In this population, investigating tailored text messaging or other mobile health options may be beneficial in terms of improving education about breast cancer prevention and the meaning of abnormal mammograms.
The authors gratefully acknowledge the contributions of Anitha Mullangi, MD, for making the clinical aspects effective, the dedication of Sandra Espinoza for patient enrollment, and the Community Advisory Board for its perspective and insight.
References
American Cancer Society. (2012). Cancer facts and figures for Hispanics/Latinos 2012–2014. Retrieved from http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/docum…
Ashing-Giwa, K.T., Gonzalez, P., Lim, J.W., Chung, C., Paz, B., Somlo, G., & Wakabayashi, M.T. (2010). Diagnostic and therapeutic delays among a multiethnic sample of breast and cervical cancer survivors. Cancer, 116, 3195–3204. doi:10.1002/cncr.25060
Bastani, R., Mojica, C.M., Berman, B.A., & Ganz, P.A. (2010). Low-income women with abnormal breast findings: Results of a randomized trial to increase rates of diagnostic resolution. Cancer Epidemiology, Biomarkers, and Prevention, 19, 1927–1936. doi:10.1158/1055-9965.EPI-09-0481
Chen, E.T., Eder, M., Elder, N.C., & Hickner, J. (2010). Crossing the finish line: Follow-up of abnormal test results in a multisite community health center. Journal of the National Medical Association, 102, 720–725.
Dang, C.M., Estrada, S., Bresee, C., & Phillips, E.H. (2013). Exploring potential use of Internet, e-mail, and instant text messaging to promote breast health and mammogram use among immigrant Hispanic women in Los Angeles County. American Surgeon, 79, 997–1000.
Davis, S.W., & Oakley-Girvan, I. (2015). mHealth education applications along the cancer continuum. Journal of Cancer Education, 30, 388–394. doi:10.1007/s13187-014-0761-4
Ferrante, J.M., Chen, P.H., & Kim, S. (2008). The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: A randomized controlled trial. Journal of Urban Health, 85, 114–124. doi:10.1007/s11524-007-9228-9
Gorin, S.S., Heck, J.E., Cheng, B., & Smith, S.J. (2006). Delays in breast cancer diagnosis and treatment by racial/ethnic group. Archives of Internal Medicine, 166, 2244–2252. doi:10.1001/archinte.166.20.2244
Green, L.W., & Kreuter, M.W. (1991). Health promotion planning: An educational and ecological approach (2nd ed.). Mountain View, CA: Mayfield.
International Telecommunication Union. (2012). Measuring the information society 2012. Retrieved from http://www.itu.int/en/ITU-D/statistics/documents/publications/mis2012/m…
Karliner, L.S., Patricia Kaplan, C., Juarbe, T., Pasick, R., & Pérez-Stable, E.J. (2005). Poor patient comprehension of abnormal mammography results. Journal of General Internal Medicine, 20, 432–437. doi:10.1111/j.1525-1497.2005.40281.x
Keegan, T.H., Quach, T., Shema, S., Glaser, S.L., & Gomez, S.L. (2010). The influence of nativity and neighborhoods on breast cancer stage at diagnosis and survival among California Hispanic women. BMC Cancer, 10, 603. doi:10.1186/1471-2407-10-603
Lantz, P.M., Mujahid, M., Schwartz, K., Janz, N.K., Fagerlin, A., Salem, B., . . . Katz, S.J. (2006). The influence of race, ethnicity, and individual socioeconomic factors on breast cancer stage at diagnosis. American Journal of Public Health, 96, 2173–2178. doi:10.2105/AJPH.2005.072132
Leirer, V.O., Tanke, E.D., & Morrow, D.G. (1992). Automated telephone reminders for improving ambulatory care services. Journal of Ambulatory Care Management, 15, 54–62. doi:10.1097/00004479-199210000-00009
Luckett, T., Goldstein, D., Butow, P.N., Gebski, V., Aldridge, L.J., McGrane, J., . . . King, M.T. (2011). Psychological morbidity and quality of life of ethnic minority patients with cancer: A systematic review and meta-analysis. Lancet Oncology, 12, 1240–1248. doi:10.1016/S1470-2045(11)70212-1
McBride, C.M., & Rimer, B.K. (1999). Using the telephone to improve health behavior and health service delivery. Patient Education and Counseling, 37, 3–18. doi:10.1016/s0738-3991(98)00098-6
Miranda, P.Y., Wilkinson, A.V., Etzel, C.J., Zhou, R., Jones, L.A., Thompson, P., & Bondy, M.L. (2011). Policy implications of early onset breast cancer among Mexican-origin women. Cancer, 117, 390–397. doi:10.1002/cncr.25680
Molina, Y., Beresford, S.A., Espinoza, N., & Thompson, B. (2014). Psychological distress, social withdrawal, and coping following receipt of an abnormal mammogram among different ethnicities: A mediation model. Oncology Nursing Forum, 45, 523–532. doi:10.1188/14.ONF.523-532
Pérez-Stable, E.J., Afable-Munsuz, A., Kaplan, C.P., Pace, L., Samayoa, C., Somkin, C., . . . Pasick, R.J. (2013). Factors influencing time to diagnosis after abnormal mammography in diverse women. Journal of Women’s Health, 22, 159–166. doi:10.1089/jwh.2012.3646
Poon, E.G., Haas, J.S., Louise Puopolo, A., Gandhi, T.K., Burdick, E., Bates, D.W., & Brennan, T.A. (2004). Communication factors in the follow-up of abnormal mammograms. Journal of General Internal Medicine, 19, 316–323. doi:10.1111/j.1525-497.2004.30357
Press, R., Carrasquillo, O., Sciacca, R.R., & Giardina, E.G. (2008). Racial/ethnic disparities in time to follow-up after an abnormal mammogram. Journal of Women’s Health, 17, 923–930. doi:10.1089/jwh.2007.0402
Price, M., Williamson, D., McCandless, R., Mueller, M., Gregoski, M., Brunner-Jackson, B., . . . Treiber, F. (2013). Hispanic migrant farm workers’ attitudes toward mobile phone-based telehealth for management of chronic health conditions. Journal of Medical Internet Research, 15, e76. doi:10.2196/jmir.2500
Smith, A. (2011, August 15). Americans and their cell phones. Retrieved from http://www.pewinternet.org/2011/08/15/americans-and-their-cell-phones
Steele, A. (1999). Computer telephony solution reduces no-shows. Health Management Technology, 20, 8–10.
Stehr-Green, P.A., Dini, E.F., Lindegren, M.L., & Patriarca, P.A. (1993). Evaluation of telephoned computer-generated reminders to improve immunization coverage at inner-city clinics. Public Health Reports, 108, 426–430.
Taplin, S.H., Barlow, W.E., Ludman, E., MacLehos, R., Meyer, D.M., Seger, D., . . . Curry, S. (2000). Testing reminder and motivational telephone calls to increase screening mammography: A randomized study. Journal of the National Cancer Institute, 92, 233–242. doi:10.1093/jnci/92.3.233
Taplin, S.H., Yabroff, K.R., & Zapka, J. (2012). A multilevel research perspective on cancer care delivery: The example of follow-up to an abnormal mammogram. Cancer Epidemiology, Biomarkers, and Prevention, 21, 1709–1715. doi:10.1158/1055-9965.EPI-12-0265
U.S. Census Bureau. (2012, December 12). U.S. Census Bureau projections show a slower growing, older, more diverse nation a half century from now [Press release]. Retrieved from https://www.census.gov/newsroom/releases/archives/population/cb12-243.h…
Wujcik, D., Shyr, Y., Li, M., Clayton, M.F., Ellington, L., Menon, U., & Mooney, K. (2009). Delay in diagnostic testing after abnormal mammography in low-income women. Oncology Nursing Forum, 36, 709–715. doi:10.1188/09.ONF.709-715
Zapka, J., Taplin, S.H., Price, R.A., Cranos, C., & Yabroff, R. (2010). Factors in quality care—the case of follow-up to abnormal cancer screening tests—problems in the steps and interfaces of care. Journal of the National Cancer Institute. Monographs, 2010, 58–71. doi:10.1093/jncimonographs/lgq009
Zapka, J.G., Puleo, E., Taplin, S.H., Goins, K.V., Ulcickas Yood, M., Mouchawar, J., . . . Manos, M.M. (2004). Processes of care in cervical and breast cancer screening and follow-up—The importance of communication. Preventive Medicine, 39, 81–90. doi:10.1016/j.ypmed.2004.03.010
About the Author(s)
Oakley-Girvan is a research scientist II at the Cancer Prevention Institute of California in Fremont; Londono is the director of health education at the Tiburcio Vasquez Health Center in Hayward, CA; and Canchola is a biostatistician IV and Davis is a research associate IV, both at the Cancer Prevention Institute of California. This research was funded by a grant (No. I8AB-1500) from the California Breast Cancer Research Program at the University of California, donations to the Cancer Prevention Institute of California, and support paid to Oakley-Girvan’s investigator funds by the Stanford Cancer Institute. Oakley-Girvan, Londono, and Davis contributed to the study conceptualization and design. Oakley-Girvan and Londono completed the data collection. Canchola provided statistical support. Canchola and Davis contributed to the analysis. All of the authors contributed to the manuscript preparation. Oakley-Girvan can be reached at ingrid.oakley-girvan@cpic.org, with copy to editor at ONFEditor@ons.org. Submitted March 2015. Accepted for publication May 25, 2015.

