A Comparison of the Reactions of Caregivers of Patients With Cancer Versus Patients With Other Chronic Medical Conditions
Purpose/Objectives: To explore positive and negative aspects of the experiences of informal caregivers of patients with cancer and patients with other chronic medical conditions, to compare the reactions of caregivers of patients with cancer and patients with other chronic medical conditions, and to study the association of caregiver reactions with demographic factors.
Design: Descriptive, correlational.
Setting: A comprehensive cancer center and a community hospital, both in Philadelphia, PA.
Sample: 111 informal caregivers.
Methods: A survey that could be completed either in paper format or electronically was administered.
Main Research Variables: Self-esteem, impact on schedule, impact on finances, impact on health, lack of family support, positive aspects of caregiving.
Findings: For caregivers, offering emotional and psychological support was most challenging, whereas providing transportation was least challenging. Caregivers reported high self-esteem and moderately positive aspects of caregiving. Caregivers of patients with cancer identified more positive aspects of caregiving. Differences in the caregiving experience based on demographic factors (e.g., gender, race, ethnicity) were found.
Conclusions: Caregivers reported positive and negative aspects of caregiving. Reactions of informal caregivers to the caregiving experience vary more based on individual demographic factors than on the diagnosis of the patient. Differences exist in the caregiving experience based on race and ethnicity.
Implications for Nursing: Nurses need to be aware that positive and negative reactions to the caregiving experience exist. Assessment and care planning should include consideration for individual factors, such as gender, race, and ethnicity.
Jump to a section
The care of patients with chronic medical conditions, including cancer, often involves the assistance of informal caregivers, such as family members or friends. An estimated 40 million caregivers provide care to adults (individuals aged 18 years or older) with a disability or illness. Caregiver services were valued at $470 billion per year in 2013—an increase from $375 billion in 2007; with the aging population expected to double between 2000 and 2030, the impact of caregiving on health care will likely continue to grow (Family Caregiver Alliance, 2016).
Although the majority of caregivers are women, research suggests that the number of male caregivers is increasing and will continue to do so because of a variety of social demographic factors (Family Caregiver Alliance, 2016). Scarce research exists on how the experiences of caregivers may vary according to gender. Early studies of caregiving have identified that women tend to perceive caregiving as more negative than do men and report higher levels of psychological distress; younger women in particular seem to share this perception (Blood, Simpson, Dineen, Kauffman, & Raimondi, 1994; Zarit, Todd, & Zarit, 1986). Pearlin, Mullan, Semple, and Skaff (1990) found that the effects of gender, as well as other demographic factors, such as age, are threaded throughout the entire stress process and noted that gender deserved more attention in studies of caregiving and stress. A study using the Pearlin Stress Process Model (Schumacher, Dodd, & Paul, 1993) to explore the stress process in family caregivers of patients receiving chemotherapy found that male caregivers had higher caregiver strain than did female caregivers. Kim, Baker, and Spillers (2007) reported that, among participants in the American Cancer Society National Quality of Life Survey for Caregivers, male caregivers were more likely than female caregivers to appraise the caregiving experience as boosting their self-esteem. These somewhat conflicting findings identify a gap in knowledge of the caregiving experience and gender differences, and they support the need for additional study.
Background
The majority of caregiving research has focused on negative aspects of caregiving, such as caregiver burden, stress, psychological distress, depression, strain, and demands. Positive aspects include preparedness, confidence, benefits, esteem, and resilience. Nijboer, Triemstra, Tempelaar, Sanderman, & van den Bos (1999) pointed out that positive and negative aspects of caregiving merit additional study. This information may enhance or increase positive aspects of caregiving for caregivers. Pasacreta, Barg, Nuamah, and McCorkle (2000) found that caregiver perceptions of their own health increased after attending a family caregiver cancer education program. Kim, Schulz, and Carver (2007) identified six domains of benefit finding via factor analysis from the American Cancer Society National Quality of Life Survey for Caregivers. These domains were acceptance, empathy, appreciation, family, positive self-view, and reprioritization. Ross, Sundaramurthi, and Bevans (2013) looked at the influence of caregiving on health behaviors in a review of eight articles and found conflicting information, with some deleterious changes and some protective changes noted. Ross et al. (2013) observed that, as a result of their experience, some caregivers may take a more active role in the protection of their health (e.g., obtaining cancer screenings at a higher rate than noncaregivers). A need for additional research exists regarding the potential positive aspects of the caregiving experience; this research may provide healthcare professionals and caregivers with a full picture of the experience and help to target resources and services more appropriately.
A body of research on caregiving exists in the areas of oncology and Alzheimer disease, with less available in other chronic medical condition situations, such as stroke or pulmonary disease. Few studies have compared the caregiver experience in various chronic medical condition populations. Similarities and differences may exist in the experiences of caregivers of different populations of patients, and this information could assist healthcare professionals in providing optimal care to caregiver–patient dyads.
The purpose of this study was to explore positive and negative aspects of the experiences of informal caregivers of patients with cancer and patients with other chronic medical conditions. Specific objectives were to compare the reactions of caregivers of patients with cancer and those with other chronic medical conditions and to study the association of caregiver reactions with demographic factors, such as gender, race, and ethnicity.
Methods
Eligible study participants were unpaid personal caregivers who self-identified as the primary caregiver of a patient or were identified by hospital staff as caregivers. Eligible criteria included (a) being an adult caregiver aged 18 years or older, (b) caring for an adult patient aged 18 years or older, and (c) giving care in the home environment. Caregivers of patients living in assisted-living facilities or nursing homes were not eligible.
A survey was developed and completed by 111 caregivers accessed through Fox Chase Cancer Center, a National Cancer Institute–designated comprehensive cancer center, and Jeanes Hospital, a community hospital on the same campus and part of the same academic health system; both are located in Philadelphia, Pennsylvania. According to participant preference, the survey was completed either in paper format or electronically. In addition to the study instruments, the survey included 17 self-reported demographic variables and additional questions about caregiver age, gender, ethnicity, race, relationship to the patient, length of time in caregiving role, and outside employment (full-time, part-time, number of hours per week), as well as chronic medical conditions of the patient and any home care or community services used. Participants were also asked to identify what types of caregiving assistance they provided to the patient and what they found to be most challenging and least challenging about caregiving.
Instruments
Study instruments were the Caregiver Reaction Assessment (CRA) instrument (Given et al., 1992) and the Positive Aspects of Caregiving (PAC) scale (Boerner, Schulz, & Horowitz, 2004).
Caregiver Reaction Assessment: The CRA was developed for use with caregivers of patients with chronic physical and mental impairments. It consists of 24 items with a five-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). The CRA is made up of five subscales: impact on finances, impact on health, impact on schedule, lack of family support, and self-esteem. The CRA was selected for use in this study because it assesses negative and positive aspects of the caregiving experience. It also can be used for discovering differences in the reactions of various groups of caregivers (e.g., various medical conditions of care recipients). Reliability analyses showed the Cronbach alpha to be from 0.62–0.83 for the separate subscales, and construct validity was supported (Nijboer et al., 1999). Reliability for the CRA subscales in this study was analyzed using the Cronbach alpha with results as follows: impact on finances = 0.79, impact on health = 0.76, impact on schedule = 0.85, lack of family support = 0.87, self-esteem (of the caregiver) = 0.88.
Positive Aspects of Caregiving: The PAC (Boerner et al., 2004; Tarlow et al., 2004) consists of 11 items that were based on an earlier measure administered to caregivers of patients with a diagnosis of either physical or cognitive impairment. A five-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree) is used. The PAC was selected for this study because of its focus on positive aspects of caregiving. Overall reliability of the scale is high, with a Cronbach alpha of 0.89, and construct validity was supported. In this study, the Cronbach alpha of the PAC was found to be 0.88.
Statistical Analysis
Power analysis: The sample size was chosen as such to have sufficient power to detect medium effect sizes when comparing responses in caregivers of patients with cancer versus caregivers of patients with other chronic medical conditions. A medium-sized effect (i.e., difference in two means) is about 0.5 standard deviation (SD) units as per the recommendation of Cohen (1992), whereas a large-sized effect is about 0.8 SD units. The current authors designed the study to recruit at least 40 people per caregiver group (N = 80; caregivers of patients with cancer versus caregivers [n = 40] of patients with other chronic medical conditions [n = 40]). With 40 people per group, the current authors had 85% power to detect effects as small as 0.67 SD units using a t test. This assumed a 5% type I error rate (two sided). The detectable effect would become smaller as the sample size increased above 40 people per group.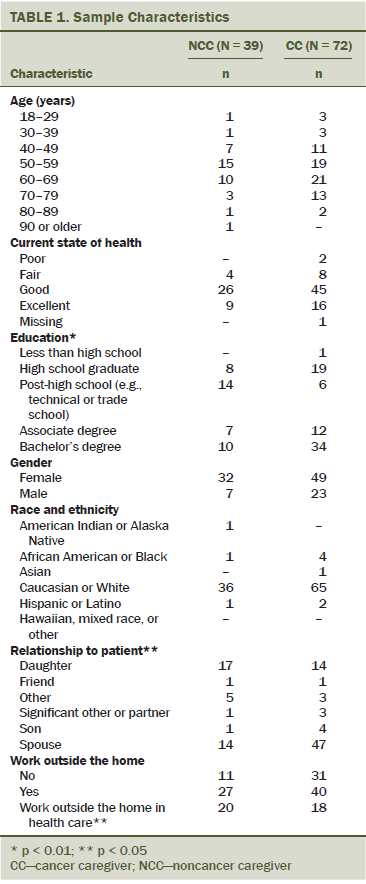
Analytic approach: The data were summarized using descriptive statistics, such as means, proportions, and SDs. For hypothesis testing, the authors used Fisher’s exact tests to compare two categorical variables, Spearman rank correlations to compare two continuous variables, t tests to compare continuous with binary variables, and analyses of variance to compare continuous with categorical variables. Multiple linear regressions of the CRA and PAC response variables were used to explore whether the effects of caring for a patient with cancer versus a patient with another chronic medical condition changed after controlling for potentially confounding demographic covariates. The authors adjusted for the following variables: length of time as caregiver, relationship to patient, education level, age, and gender. The choice of variables to include as covariates in the multiple linear regressions was based on those that were shown to be statistically significant in Tables 1 and 2, along with those that were considered to be scientifically relevant potential confounders (age, gender).
Results
Positive and negative aspects of the caregiving experience were identified in this study. Caregiver participants were asked to indicate the most challenging and least challenging aspects of the caregiving experience. Offering emotional or psychological support was identified as being most challenging (49%), whereas providing transportation was least challenging (19%). Of the five subscales of the CRA, self-esteem (of the caregiver) had the highest overall mean score (see Table 3). This subscale consisted of positive reactions to caregiving, such as enjoying caring, feeling privileged to care, wanting to care, and believing caring to be personally important to the caregiver. All of the subscales were strongly associated with one another, except impact on finances and self-esteem. The PAC yielded a mean score of 3.5 out of 5 (SD = 0.7, minimum = 1, maximum = 5), indicating moderately positive results.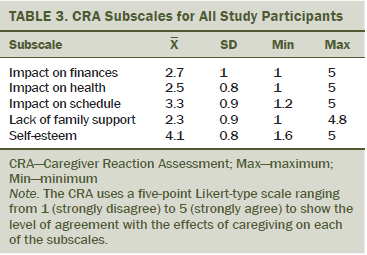
Differences in the caregiving experience (i.e., CRA and PAC variables) were explored with respect to the cancer versus noncancer diagnosis of the patient. Although lack of family support was associated with diagnosis in unadjusted analyses (higher Likert values in noncancer group), it was not statistically significant in the multiple linear regression adjusted analyses (mean = 2.6, SD = 0.9 in noncancer group; mean = 2.2, SD = 1 in cancer group; p = 0.021 unadjusted, p = 0.47 adjusted). This suggests that other factors are affecting feelings of lack of family support (e.g., education, the likely related income status differences between the two groups). PAC was marginally statistically significant in unadjusted analyses (cancer group has higher PAC). This effect became more pronounced and statistically significant when adjusting for other factors (mean = 3.3, SD = 0.6 in noncancer group; mean = 3.6, SD = 0.7 in cancer group; p = 0.054 unadjusted, p = 0.03 adjusted). No statistically significant unadjusted or adjusted differences were noted between the diagnosis groups with respect to impact on finance, impact on health, impact on schedule, or self-esteem.
Gender differences in the caregiving experience were identified. Men were more likely than women to find providing assistance with walking, personal care, and personal hygiene least challenging (12% of men versus 1% of women, p = 0.049). Men were less likely to indicate that their health was affected by caregiving (mean = 2.1, SD = 0.6) than women (mean = 2.7, SD = 0.8, p = 0.0002). Differences were also found regarding the relationship of the caregiver to the patient. Daughters identified the highest impact on schedule (mean = 3.4, SD = 0.8, p = 0.046) and were most likely to indicate lack of family support (mean = 2.8, SD = 1, p = 0.039).
Differences in the caregiving experience were identified based on the race and ethnicity of the caregiver. Caucasian caregivers (n = 101, mean = 4, SD = 0.8) had lower self-esteem than non-Caucasian caregivers (n = 10, mean = 4.4, SD = 0.5, p = 0.026) and were more likely to indicate that their health was affected (mean = 2.6, SD = 0.8 in Caucasian caregivers; mean = 2, SD = 0.6 in non-Caucasian caregivers; p = 0.025). Non-Caucasian caregivers had a higher score on the PAC instrument (mean = 4.1, SD = 0.5) than Caucasian caregivers (mean = 3.5, SD = 0.7, p = 0.002), indicating a more positive experience.
Other findings included that age was inversely related to lack of family support on the CRA. Older respondents were less likely to indicate lack of family support (Spearman correlation [rho] = –0.19, p = 0.047). Caregivers who worked outside of the home reported more impact on finances (mean = 2.8, SD = 1) than those who did not (mean = 2.4, SD = 1, p = 0.047). Those who worked more hours reported higher self-esteem (rho = 0.31, p = 0.013). Caregivers who worked outside of the home in a healthcare-related position found medical and nursing tasks to be least challenging (30% for those who worked outside of the home in a healthcare-related position versus 4% of others, p = 0.016). Caregivers with higher levels of health were less likely to indicate that caregiving affected their health (rho = –0.34, p = 0.0002) or finances (rho = –0.2, p = 0.038). Caregivers who did not live with the patient (mean = 2.8, SD = 1) were more likely to indicate lack of family support (mean = 2.2, SD = 0.9 for those who lived with the patient, p = 0.008).
Discussion
Informal caregivers play a role of growing importance in providing optimal health care to patients with cancer and other chronic medical conditions. Little information is available on how the experiences of caregivers are similar and different based on the chronic medical condition of the patient. Caregiving certainly is a challenging role; however, it can also potentially have positive aspects for the caregiver. Although the majority of informal caregivers are women, men are increasingly taking on the role of caregiver. Caregiving also has cultural implications, which have not been well explored in the research literature. This research was designed to expand knowledge about the informal caregiver experience and how this experience may vary based on the chronic medical condition of the patient, the gender of the caregiver, race and ethnicity, and other social demographic factors of the caregiver.
Study findings provide evidence that positive aspects, along with challenges, are part of the caregiving experience for informal caregivers. One of the major findings was that the caregiver experience can lend to a feeling of self-esteem for the caregiver. Acknowledging the potential positive aspects of the caregiving experience, as well as building on the caregiver’s self-esteem, could enhance patient education and support of caregivers. Challenges of the caregiving experience also need to be acknowledged, with soft needs, such as providing emotional and psychological support, potentially needing more intervention and assistance than more concrete needs, such as transportation. Nurses and social workers can work together to help identify, prioritize, and meet these needs.
Differences in the caregiving experience were found based on the cancer versus noncancer diagnosis of the patient, with study results suggesting the effects of confounding variables, such as education level of the caregiver. These findings support a need for additional study in this area, including the relationship of individual caregiver characteristics to the caregiving experience.
Study findings also provided evidence that variations exist in the caregiving experience based on gender. Male caregivers reported less impact on health, indicating that female caregivers may need more support in this area. These findings indicate a need for additional study related to gender, such as the perceptions of male caregivers related to the caregiving role. Daughters in a caregiving role may need help balancing their caregiver responsibilities with their personal lives (impact on schedule) and in eliciting more family support. Care planning, patient education, and support groups can be targeted accordingly.
Study results related to race and ethnicity were particularly interesting in light of some of the strong differences observed. Evidence was found that non-Caucasian caregivers may characterize the caregiving experience as more positive overall, have higher self-esteem, and report less impact on their health than Caucasian caregivers. This supports the importance of cultural aspects in the caregiving experience, an area that merits additional research. With the need for more cultural competency in all aspects of health care, these findings lend support to ongoing study and education in this area.
Limitations
This study had several limitations. A convenience sample was used so caregivers who chose to participate in the study may have different experiences or reactions than those who did not choose to participate. The study was conducted in a healthcare setting, and employees of the hospital who also were informal caregivers were not excluded from participating. The study was conducted in two institutions in the same geographic area, so generalization to other settings is limited.
Conclusion
Findings from the current study highlight the variations in the caregiving experience based on individual caregiver factors, such as gender, race, and ethnicity. These individual factors have more impact on the caregiving experience than the diagnosis of the patient. Although many challenging aspects of caregiving exist, caregivers also identified positive aspects, such as self-esteem.
Nurses can help to provide optimal care to caregiver–patient dyads by recognizing that, although physical tasks, such as assisting with activities of daily living or nursing and medical treatments, are common, other activities, such as providing emotional and psychological support, may be more challenging. With nursing involvement, a systematic caregiver assessment can address concerns of the patient and the caregiver and guide the development of interventions to reduce the negative aspects and enhance the positive aspects of the caregiving experience. Simply encouraging caregivers to talk about their experiences may be a helpful intervention. Additional interventions that allow for flexibility with caregiver responsibilities and schedules, such as Web-based interventions, merit additional study (Kaltenbaugh et al., 2015). Assessment and care planning should include consideration for individual factors, such as gender, race, and ethnicity. Oncology nurses and social workers possess the specialized knowledge and skills to work together to provide education and training about the caregiving process, determine appropriate support services, and enhance patient outcomes.
Informal caregivers are an integral part of health care and long-term services for the chronically ill. These study findings support the need for additional research on the multifaceted caregiving experience and ways in which nurses can partner with social workers and other members of the healthcare team to optimize the caregiving experience and positively affect patient outcomes. Specifically, research is needed regarding how the needs of caregivers can best be met based on individual factors, such as gender and education level. To support culturally competent practice, additional research is also needed regarding the cultural implications of the caregiving experience. As the science of caregiver health continues to grow, a need exists for more widespread implementation and evaluation of interventions that have shown effectiveness, as well as more longitudinal studies on the caregiver experience (Grady & Rosenbaum, 2015).
The authors gratefully acknowledge the following individuals employed as clinical nurses at Fox Chase Cancer Center at the time of this writing for their assistance with the current study: Lianne Doyle, RN, BSN, OCN®, Johanna Rochat, RN, BSN, Linda Regul, RN, MSN, OCN®, Jean Smith, RN, OCN®, and Catherine Toomey, RN, OCN®.
References
Blood, G.W., Simpson, K.C., Dineen, M., Kauffman, S.M., & Raimondi, S.C. (1994). Spouses of individuals with laryngeal cancer: Caregiver strain and burden. Journal of Communication Disorders, 27, 19–35.
Boerner, K., Schulz, R., & Horowitz, A. (2004). Positive aspects of caregiving and adaptation to bereavement. Psychology and Aging, 19, 668–675. doi:10.1037/0882-7974.19.4.668
Cohen, J. (1992). A power primer. Psychological Bulletin, 112, 155–159.
Family Caregiver Alliance. (2016). Caregiver statistics: Demographics. Retrieved from https://www.caregiver.org/caregiver-statistics-demographics
Given, C.W., Given, B., Stommel, M., Collins, C., King, S., & Franklin, S. (1992). The Caregiver Reaction Assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Research in Nursing and Health, 15, 271–283. doi:10.1002/nur.4770150406
Grady, P.A., & Rosenbaum, L.M. (2015). The science of caregiver health. Journal of Nursing Scholarship, 47, 197–199. doi:10.1111/jnu.12137
Kaltenbaugh, D.J., Klem, M.L., Hu, L., Turi, E., Haines, A.J., & Hagerty Lingler, J. (2015). Using Web-based interventions to support caregivers of patients with cancer: A systematic review. Oncology Nursing Forum, 42, 154–164. doi:10.1188/15.ONF.156-164
Kim, Y., Baker, F., & Spillers, R.L. (2007). Cancer caregivers’ quality of life: Effects of gender, relationship, and appraisal. Journal of Pain and Symptom Management, 34, 294–304. doi:10.1016/j.jpainsymman.2006.11.012
Kim, Y., Schulz, R., & Carver, C.S. (2007). Benefit-finding in the cancer caregiving experience. Psychosomatic Medicine, 69, 283–291. doi:10.1097/psy.0b013e3180417cf4
Nijboer, C., Triemstra, M., Tempelaar, R., Sanderman, R., & van den Bos, G.A. (1999). Measuring both negative and positive reactions to giving care to cancer patients: Psychometric qualities of the Caregiver Reaction Assessment (CRA). Social Science and Medicine, 48, 1259–1269. doi:10.1016/s0277-9536(98)00426-2
Pasacreta, J.V., Barg, F., Nuamah, I., & McCorkle, R. (2000). Participant characteristics before and 4 months after attendance at a family caregiver cancer education program. Cancer Nursing, 23, 295–303. doi:10.1097/00002820-200008000-00007
Pearlin, L.I., Mullan, J.T., Semple, S.J., & Skaff, M.M. (1990). Caregiving and the stress process: An overview of concepts and their measures. Gerontologist, 30, 583–594. doi:10.1093/geront/30.5.583
Ross, A., Sundaramurthi, T., & Bevans, M. (2013). A labor of love: The influence of cancer caregiving on health behaviors. Cancer Nursing, 36, 474–483. doi:10.1097/NCC.0b013e3182747b75
Schumacher, K.L., Dodd, M.J., & Paul, S.M. (1993). The stress process in family caregivers of persons receiving chemotherapy. Research in Nursing and Health, 16, 395–404. doi:10.1002/nur.4770160603
Tarlow, B.J., Wisniewski, S.R., Belle, S.H., Rubert, M., Ory, M.G., & Gallagher-Thompson, D. (2004). Positive aspects of caregiving: Contributions of the REACH Project to the development of new measures for Alzheimer’s caregiving. Research on Aging, 26, 429–453. doi:10.1177/016402750426449
Zarit, S.H., Todd, P.A., & Zarit, J.M. (1986). Subjective burden of husbands and wives as caregivers: A longitudinal study. Gerontologist, 26, 260–266.
About the Author(s)
Cobb is the director of professional development and practice innovation and Etkins is a social worker, both at Fox Chase Cancer Center; Nelson is a stroke program coordinator at Jeanes Hospital; and Egleston is an associate research professor and Sweeney is a clinical nurse, both at Fox Chase Cancer Center, all in Philadelphia, PA. This research was funded by a grant (P30CA006927) from the National Cancer Institute of the National Institutes of Health. Cobb, Etkins, Nelson, and Egleston contributed to the conceptualization and design. Cobb, Etkins, Nelson, and Sweeney completed the data collection. Egleston provided the statistical support and analysis. Cobb, Etkins, Nelson, Egleston, and Sweeney contributed to the manuscript preparation. Cobb can be reached at susan.cobb@fccc.edu, with copy to editor at ONFEditor@ons.org. Submitted May 2015. Accepted for publication June 28, 2015.

