Parental Decision Making Regarding the Disclosure or Nondisclosure of a Mutation-Positive BRCA1/2 Test Result to Minors
Purpose/Objectives: To gain insight into parental decision making regarding the disclosure or nondisclosure of a mutation-positive BRCA1/2 test result to minors.
Research Approach: A qualitative study based on Heidegger hermeneutic phenomenology was undertaken to explore the lived experience of parental decision making regarding high-risk BRCA1/2 disclosure.
Setting: The study’s recruitment site was a western Canadian hereditary breast and ovarian cancer clinic.
Participants: Fifteen female mutation-positive BRCA1/2 carriers who had at least one child aged 6–18 years.
Methodologic Approach: The use of a demographic questionnaire, semistructured interviews, and conversation summaries were employed to gain an understanding of participants’ lived experience. van Manen’s selective approach was used to conduct a thematic analysis.
Findings: Collectively, parents wanted clinicians to discuss implications of disclosing and not disclosing a mutation-positive BRCA1/2 test result to minors in greater detail. The findings were categorized under the following emergent themes: influential factors, parental decision making, supportive resources, the inner circle, knowledge deficit, and parental recommendations.
Conclusions: Participants’ stories identified the need for auxiliary support pertaining to the decision-making process and suggested ways in which parental support may be coordinated.
Interpretation: Oncology nurses with advanced genetics training should assist mutation-positive BRCA1/2 carriers in meeting their genetic risk information needs; this requires nurses to stay informed about a multitude of issues that affect this population of patients.
Jump to a section
About 23,800 cases of breast cancer and 2,600 cases of ovarian cancer are diagnosed each year in Canada (Canadian Cancer Society’s Advisory Committee on Cancer Statistics, 2013). Roughly 5%–10% of these two groups combined are at high risk for hereditary breast, ovarian, and other cancers; consequently, genetic services are offered to high-risk individuals (Patenaude et al., 2013; Seenandan-Sookdeo & Sawatzky, 2010). The proband (family member who initiates genetic testing) is then responsible for sharing the test result with family members. This action has the potential to affect individuals physically, psychologically, and socially (Bradbury et al., 2007, 2012).
A review of the BRCA1/2 peer review literature was conducted using the CINAHL® and PubMed databases from 2005–2015. The key word searches included hereditary breast and ovarian, BRCA1/2 parental decision making, and disclosure of genetic test results to minors. The literature search revealed that studies have assessed the psychological impact of and barriers to genetic testing with female participants (Braithwaite, Emery, Walter, Prevost, & Sutton, 2006; Crotser & Boehmke, 2009; Hamilton, Lobel, & Moyer, 2009; Meiser & Halliday, 2002; O’Neill et al., 2015). In addition, communication of a test result to sisters has been extensively researched (Howard, Balneaves, & Bottorff, 2009; MacKenzie, Patrick-Miller, & Bradbury, 2009; Schlich-Bakker, ten Kroode, & Ausems, 2006). However, a gap exists in the exploration of the needs of male mutation-positive BRCA1/2 carriers; this is partly attributable to the limited uptake of high-risk men consenting to genetic testing (Hallowell et al., 2005). Collectively, the aforementioned studies support fathers’ preference for a shared parental decision-making process and paternal feelings of guilt and blame associated with a deleterious BRCA1/2 test result (Finlay et al., 2008; Hallowell et al., 2005, 2006). The need for study also exists in the area of parental disclosure or nondisclosure of a mutation-positive BRCA1/2 test result to younger offspring (Clarke, Butler, & Esplen, 2008; Peshkin, DeMarco, & Tercyak, 2010; Rowland & Metcalfe, 2013). Research in the area of parental BRCA1/2 disclosure or nondisclosure will help clinicians understand how best to assist parental decision making.
BRCA1/2 testing is available to eligible individuals who are aged at least 18–25 years (Bradbury et al., 2009, 2012). Each offspring of a parent diagnosed with a mutation-positive BRCA1/2 has a 50% chance of inheriting the deleterious gene (Patenaude et al., 2013). The research literature acknowledges that the majority of parents share genetic test results with children aged younger than 18 years, despite admissions of feeling unprepared to engage in complex conversations (Rowland & Metcalfe, 2013). Nevertheless, parents conveyed that they were ideal individuals to initiate genetic conversations with offspring, but they requested the development of appropriate resources (O’Neill et al., 2015).
Extant research literature indicated that parents’ decisions to disclose or not disclose a mutation-positive BRCA1/2 test result to minors are influenced by various factors (Patenaude et al., 2013; Rowland & Metcalfe, 2013). The emotional readiness of parents and minors is taken into consideration (Bradbury et al., 2007; Clarke et al., 2008; Metcalfe, Plumridge, Coad, Shanks, & Gill, 2011; O’Neill et al., 2015). Nondisclosing parents supported disclosure during adulthood because they believed that minors are not emotionally ready to understand complex genetic health information (Bradbury et al., 2012; Clarke et al., 2008; Segal et al., 2004). Clarke et al. (2008) maintained that parents worried about the premature divulgence of genetic information by other family members before parental readiness, which caused decisional conflicts that contributed toward parents’ disclosure regret. Rowland and Metcalfe’s (2013) systematic review of nine qualitative studies concluded that age-appropriate disclosure was positively associated with the well-being of parents and offspring. Discrepancies exist in the literature regarding the impact of a child’s gender on decision making (Segal et al., 2004; Tercyak, Peshkin, DeMarco, Brogan, & Lerman, 2002) and children’s early knowledge of a family’s genetic history on healthy lifestyle choices, as well as body and health advocacy awareness (Bradbury et al., 2007; Rowland & Metcalfe, 2013). In addition, intrafamilial oncology experiences were shown to act as a disclosure barrier for some mutation-positive BRCA1/2 carriers (Bradbury et al., 2007). Although an open style of family communication was associated with disclosure, a lack of male partner involvement in the decision-making process was linked to nondisclosure (Segal et al., 2004).
Minimal published research exists regarding parental disclosure or nondisclosure processes regarding sharing mutation-positive BRCA1/2 test results with minors (Patenaude et al., 2013; Tercyak et al., 2013). Consequently, the current study sought to understand parental perceptions regarding the disclosure or nondisclosure of mutation-positive BRCA1/2 test results to minors, as well as to better comprehend parental decision making, parent–child communication, and information- and support-seeking needs. Systematic exploration of parents’ decision making, communication, and personal and family needs will inform clinicians in understanding parents’ needs and how best to assist parents during the decision-making process (Patenaude et al., 2013; Tercyak et al., 2013).
Methods
Hermeneutic phenomenology, an interpretive approach rooted in the study of the lived human experience (van Manen, 1990), was selected for this study because it considers human beliefs, culture, relationships, and context to answer research questions that address the social experience and meaning of human life (Lopez & Willis, 2004). Ethics approval was obtained from the research ethics board at the University of Manitoba in Winnipeg, Canada, before initiating recruitment and data collection protocols in the province’s genetics department. A genetic counselor from the provincial clinical genetics department identified 47 eligible participants. Seventeen agreed to participate, which accounted for a 36% response rate. However, because of participants’ circumstances, the final sample consisted of 15 female participants. Men and women were invited, but no male parents expressed an interest to participate.
Procedures
A purposive sample selection was guided by the study’s inclusion and exclusion criteria (see Figure 1), which resulted in a small sample size. However, data obtained were information-rich and reflected data saturation. The genetic counselor offered eligible participants recruitment packages. Interested participants contacted the principal investigator (PI) directly by telephone to review the study’s eligibility criteria and their role in the study. In accordance with hermeneutic phenomenology, participants engaged in the research process by choosing the method of communication (telephone or in person) and a date, time, and place convenient to them (van Manen, 1990). During the initial telephone contact (initiated by potential participants), the PI reviewed the study criteria, answered questions, and instructed interested participants to forward signed consent forms and completed demographic information (see Table 1) to the PI’s office. 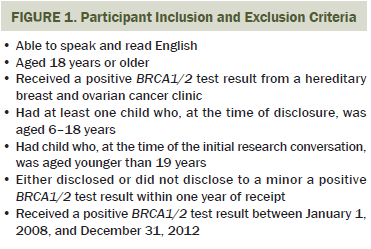
Data Collection and Measures
A conversation script consisting of open-ended questions (see Figure 2) was informed by the literature review and the PI’s previous clinical interactions with the mutation-positive BRCA1/2 population. Consequently, the script elicited parents’ decision-making processes, experiences, and perceptions regarding the disclosure or nondisclosure of mutation-positive BRCA1/2 test results to minors. The PI digitally recorded all conversations and, in a reflective log, documented her insights, response patterns, reflections on past log entries, and personal scripts. van Manen (1990) conveyed that lived human experiences are understood through the engagement of meaningful conversations that are mutually interpreted. Interactive conversations employing open-ended questions, patience, silence, respectful tones, paraphrasing, and close observations (captured in the reflective log) permitted participants to express their lived experience and allowed the PI to be objective and subjective to the shared experience. This engaging process between the PI and the participant allowed for the exploration of the parts and the whole of personal stories (Streubert & Carpenter, 2011; van Manen, 1990). In addition, interactive dialogue between the PI and the participant continued with the use of conversation summaries that were sent to each participant after the initial interview. In advance of the second conversation, participants reflected on the textual summary of the first conversation, which allowed for a continued interactive process between the PI and the participant for the purpose of gaining a rich understanding of the lived experience (van Manen, 1990). 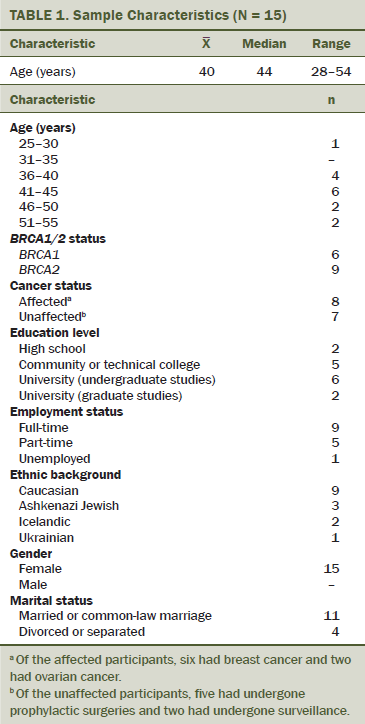
Data Analysis and Methodologic Rigor
According to van Manen (1990), lived human experiences are understood by uncovering and interpreting the structures of experience (themes). The process is not rule-bound; consequently, various methods may be embraced to understand the phenomenon (van Manen, 1990). A professional transcriptionist transcribed all digitally recorded conversations verbatim, and the PI reviewed each transcription for accuracy. A coding guide was constructed (based on the first three interviews) that was mutually agreed upon among the PI and two doctoral-prepared professionals (a psychosocial clinician and a nurse). After multiple readings of each transcript, the PI composed conversation summaries, which were sent to the appropriate participant for review.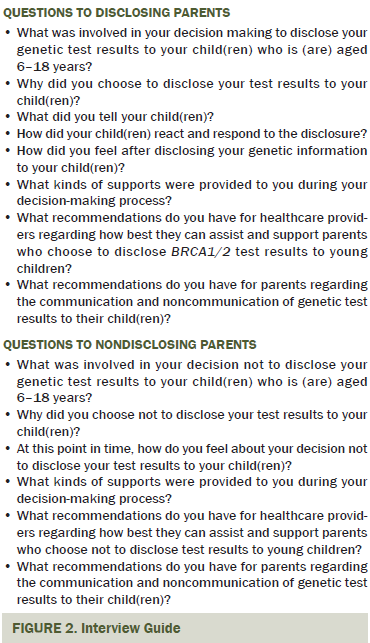
van Manen’s (1990) selective approach was used for data analysis because it reflects the underpinnings of hermeneutic phenomenology. The PI read each text as a whole to gain a deep understanding of the lived experience. Key phrases, sentences, and examples that best described the experience were isolated and transcribed onto a master spreadsheet. This process allowed for essential themes and subthemes to unfold. A second collaborative conversation ensued between the PI and the participant to offer additional insights and to assess the accuracy of conversation summaries. This collaborative back-and-forth process, known as the hermeneutic circle, verified each individual’s lived experience. The next step identified patterns among participants’ text transcripts for the identification of patterns as a whole. The final step was the interpretation of the whole, which involved reflecting on all documents (demographic forms, transcribed conversations, PI’s reflective log, and conversation summaries) to ensure a holistic reflection of participants’ lived experiences (van Manen, 1990).
Guba and Lincoln’s (1994) credibility, dependability, confirmability, and transferability were applied to establish methodologic rigor. Credibility in findings is supported by prolonged engagement (multiple conversations between the PI and the participant) and member checks, which allowed participants an opportunity to correct, clarify, and question interpretations. Periodic debriefings between the PI and the thesis advisor provided insight from an expert psychosocial clinician and researcher. Dependability is assessable through an audit trail of the study’s activities over time, which leads to confirmability (Streubert & Carpenter, 2011). The audit trail includes demographic forms, transcriptions of conversations, a detailed reflective log, the PI’s workbook, a thematic spreadsheet, and the preservation of all text that relates to the analysis process. The transferability may be assessed in the study’s contribution to the limited published research specific to the topic (Guba & Lincoln, 1994).
Findings
Fifteen parents, with a mean age of 40 years and an age range of 28–54 years, participated in the study. All parents received a mutation-positive BRCA1/2 test result from 2008–2012, and they either disclosed the result to an offspring within 36 months of receiving the test result or chose not to disclose by the first study conversation. The 15 participants had a total of 22 children (aged 6–18 years), with a mean age of 12.4 years. The event age (the age of children at the time of disclosure or the time when the parent was given the test result) range of the eligible children was 7–16 years. Nine parents disclosed, and seven did not disclose. One parent was categorized to both groups because she disclosed to the eldest child but not to the younger children. See Table 2 for the age characteristics of the participants’ children at various time points.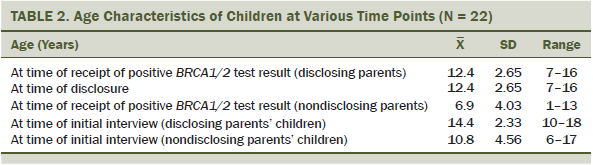
Following van Manen’s (1990) selective approach, the holistic reflection of the lived experience of parental perceptions regarding the disclosure or nondisclosure of a mutation-positive BRCA1/2 test result to minors was a parental desire for clinicians to engage parents in the decision-making process by taking the conversation a step further. Eight disclosing parents and four nondisclosing parents communicated the need to take it a step further. Parents described clinicians as being supportive and informative in their explanations about the BRCA1/2 test result, pathology reports, and available surgical and surveillance options. However, parents requested supplementary clinical support specific to the decision to disclose or not disclose a mutation-positive BRCA1/2 test result to their minor child. One disclosing parent with a mutation-positive BRCA2 discovered in 2011, an unaffected cancer status, and two children aged 11 years and 14 years at the time of disclosure elaborated on this need for additional assistance.
I mean, any healthcare provider or doctor in explaining to somebody that they have this genetic result should take it a step further. If you want to share the information with [your children], but you’re not sure how to do it, you know, maybe there could be some assistance in that regard.
One nondisclosing parent with a mutation-positive BRCA1 diagnosed in 2011, a breast cancer diagnosis, and one child aged 15 years at the time of the parental test result also discussed the importance of healthcare providers sharing this information.
I think that, even though it may be a difficult topic for some individuals . . . it’s an important one for healthcare professionals to raise—not to push information on people, but I think [it’s] just a topic that has to sort of be out there. And then, hopefully, there’ll be some resources that you can refer them to or make an offer to meet again to discuss this at whatever point in time.
The themes that emerged based on participants’ lived experiences were influential factors, parental decision making, supportive resources, the inner circle, knowledge deficit, and parental recommendations.
Influential Factors
Age, cognition, and maturity: Age, cognition, and maturity of children were factors that influenced parental decision making. A total of nine of the study participants disclosed mutation-positive BRCA1/2 test results to a minor because they felt these children were old enough and mature enough to handle that information. One disclosing parent with a mutation-positive BRCA2 discovered in 2010, an ovarian cancer diagnosis, and a child aged 7 years at the time of disclosure explained that “obviously our conversations will be changed over the years to match his comprehension of what’s actually happening and what it means.”
Nondisclosing parents also cited age, cognition, and maturity as their rationale for deferring initial genetic conversations with children until they were aged 18–30 years. The mean age of children at the time that nondisclosing parents received a mutation-positive BRCA1/2 test result was 6.9 years of age, with the average age of children from disclosing families being 12.4 years of age. Like disclosing parents, nondisclosing parents emphasized that with age comes maturity, the ability to think abstractly, and advanced problem-solving skills. Nondisclosing parents decided to postpone the conversation rather than initiate tailored age-appropriate discussions, as explained by one nondisclosing parent with a mutation-positive BRCA1 discovered in 2011, a breast cancer diagnosis, and one child aged 15 years at the time of the parental test result.
He’s not mature in the way he thinks of responsibility. He’s very egotistical right now. He’s kind of not really interested in anybody else but himself and his friends. I just don’t think he’d be interested in it or, again, would understand.
Emotional readiness: Participants took into consideration their emotional readiness and that of their children; parents identified this emotional readinesss of the parent and the child as including psychological well-being, family dynamics, familial experiences with cancer, and a desire to prepare minors for future self-health roles. One disclosing parent with a mutation-positive BRCA2 discovered in 2011, an unaffected cancer status, and two children aged 16 years and 20 years (the latter was not eligible) at the time of disclosure said, “Emotionally, she’s got a good head on her shoulders, and [she’s] very aware of her surrounding[s] and what’s going on and stuff like that. . . . I just felt it would be very beneficial to her.”
Gender: The study’s demographic form did not capture the gender of participants’ children. However, the PI identified the gender of children as a result of detailed assessments of participants’ word choices (e.g., he/she, male/female, son/daughter) in the transcripts. Study participants believed that their family’s genetic health history would not place stress onto male offspring because a man’s cancer risk is adult in onset, and surveillance options could be implemented. Parents did not voice any concerns related to vulnerabilities of a mutant BRCA1/2 gene to their daughters, but parents acknowledged an understanding that the associated risk for cancer related to a mutant BRCA1/2 gene was higher for women compared to men. One nondisclosing parent with a mutation-positive BRCA1 discovered in 2009, a breast cancer diagnosis, and one child aged 15 years at the time of the parental test result explained.
I think the fact that he’s a male and it’s BRCA1, and with BRCA1, what I’ve been told is that the risk for prostate and pancreatic cancers are . . . not that significantly elevated as they are with BRCA2. You know that fact that he doesn’t have, or I mean that there’s not the same urgency similarly as a girl.
Timing: Although most parents noted that their decision making involved a contemplation of preparing children for the future, several parents differed regarding the rationale for their decision about childhood preparation. For disclosing parents, childhood preparation was equated to family health history education, which they believed would foster engagement by the child in future health decision making. Nondisclosing parents associated the child’s preparation with implementing children’s insurance policies before the initiation of a disclosure conversation. These parents also delayed disclosure conversations to prevent children from making impulsive decisions early in life because they presumed prophylactic options could change. Consequently, a deferral in disclosure was viewed as allowing appropriate time for parental planning and time for the natural sequence of age-appropriate developmental stages to unfold.
Honesty: Exclusive to disclosing parents’ decision-making factors was a commitment to having honest relationships with children, other family members, and the community. Parents acknowledged that the decision to disclose a BRCA1/2 test result was affected by their child’s awareness of parental BRCA1/2 testing and of a parent’s or extended family member’s cancer diagnosis, as well as life-altering decisions that commenced with a mutation-positive test result. One disclosing parent with a mutation-positive BRCA2 discovered in 2012, an ovarian cancer diagnosis, and two children aged 11 years and 13 years at the time of disclosure explained, “[My children] had been such an active part of the cancer journey . . . and so I felt that it was important to be very honest and up front with them about what we were dealing with.”
Parental Decision Making
The second theme, parental decision making, captured parents’ assessments of their decision-making patterns. The majority of disclosing parents acknowledged that dialogue occurred between parents regarding their decision to disclose, as exemplified in the following example:
PI: What kind of support systems, if any, were involved to help prepare you for your discussion about your genetic test result with your children?
Participant (disclosing parent with a mutation-positive BRCA1 discovered in 2009, a breast cancer diagnosis, and two children aged 9 years and 12 years at the time of disclosure): I don’t know if I looked for any. My only support system would have been my husband. We had a discussion ourselves [about] how much information we were going to give them.
One disclosing parent with a mutation-positive BRCA2 discovered in 2009, a breast cancer diagnosis, and three children at the time of disclosure (aged 18 months [not eligible], 6 years [not disclosed], and 9 years [disclosed]) shared similar thoughts.
I think that, when we [the parents] talked about going for testing, it was kind of agreed between the two of us that it was something that the children would know the results of. . . . I mean, if, for some reason, they heard something on the news or read something and had a question, we would not have any problem discussing anything with them. We try to be open.
The PI’s assessment of study transcripts revealed that the presence of a supportive partner may have influenced disclosing parents’ decisions because the majority of nondisclosing parents made independent disclosure or nondisclosure decisions, as in the following example:
PI: Was your decision to disclose influenced by anyone, such as your family, friends, healthcare providers, [or] your child’s father?
Participant (nondisclosing parent with a mutation-positive BRCA2 discovered in 2008, a breast cancer diagnosis, and one child aged 15 years at the time of parental test result): No. Maybe a little bit— again with the life insurance. I did inquire [to an insurance agent] a little bit about that, asking the questions about how insurance companies might respond to that knowledge. I was really quite firm in my mind that it’s just way too young right now.
One nondisclosing parent with a mutation-positive BRCA2 discovered in 2008, a breast cancer diagnosis, and one child aged 13 years at the time of parental test result noted that the maturity of the individual child affects whether or not to disclose.
We’ve always had a very good relationship. I have made time with him to sit down and talk, and I try to listen. I’ve always been the one that would sit and talk to him. I think he feels comfortable sharing things with me. He has shared some pretty personal things as a teenager with me. . . . I absolutely think you should disclose at some point, but it depends on their maturity and what they’re going to do with that information.
Supportive Resources
Collectively, parents agreed that members of the genetics team provided valuable mutation-positive BRCA1/2 risk information. One disclosing parent with a positive BRCA1 discovered in 2011, an unaffected cancer status, and two children aged 14 years and 18 years at the time of disclosure elaborated.
The most support we got when we went through for the testing was . . . [name of member of genetics team]. So, I could have asked any questions that I wanted. They were very informative. . . . The support was good. They have a lot of information for me, and they were good to me. . . . When I went home, I went to see my family doctor, and we’re very close. . . . I really trust him, and we had a long talk, and he was a big support to me. . . . I don’t think anybody really asked me . . . if I was going to share that with my children or not. . . . Maybe I would have gotten some different ideas. I don’t know. I probably would have done the same things. . . . I think it would have been helpful.
As noted in the previous example, when asked if clinicians initiated the topic of disclosure or nondisclosure of mutation-positive BRCA1/2 test results to minors, the majority of parents stated that clinicians did not.
PI: You mentioned a little while ago that no healthcare provider approached you regarding the topic of disclosure [or] nondisclosure.
Participant (nondisclosing parent with a mutation-positive BRCA2 discovered in 2008, a breast cancer diagnosis, and one child aged 13 years at the time of parental test result): No. I’ve never heard anybody ask about this.
PI: Do you think they should have? Would it have been helpful?
Participant: I think they could bring it up. Like, “Have you thought about whether or not you’ll talk to your children at some point about this?”
Eight disclosing parents and two nondisclosing parents acknowledged that beneficial support came from family and friends, professional colleagues, family doctors, mental health professionals, surgical oncology physicians, and the families’ faith communities. One nondisclosing parent with a mutation-positive BRCA2 discovered in 2008, a breast cancer diagnosis, and one child aged 13 years at the time of parental test result emphasized the omnipresent support.
Support was always there through [name of member of genetics team], my family doctor, and my sisters. I mean, I had that. I just had made up my mind and didn’t think it was a big deal at the time. . . . I’ve never heard anybody ask about [disclosure]. . . . I think they could bring it up, like, “Have you [thought] about whether or not you’ll talk to your children at some point about this?”
A local program (Kids Can Cope) was cited as an excellent resource for children. However, this program was only accessible to children of parents diagnosed with cancer. The children who attended the program could transfer the skills learned in the program to other emotional life events. The program’s workbook, the American Cancer Society’s Because . . . Someone I Love Has Cancer: Kids’ Activity Book, was described as an excellent resource tool. Other tools identified as beneficial were a limited number of books and movies borrowed from a healthcare facility’s library. Parents stated that they adapted generalized information from the books, videos, and programs to meet the unique needs of children.
The Inner Circle
The third theme examined disclosing parents’ reflections on the parent–child disclosure conversations. Generally, conversations were described as unscheduled, nonstructured, casual, and delivered in a positive manner with the sharing of basic genetic information.
Similarities existed among the conversations. For example, the parent who was the mutation-positive BRCA1/2 carrier presented as the lead conversationalist. One disclosing parent with a mutation-positive BRCA1 discovered in 2011, an unaffected cancer status, and three children aged 13 years, 15 years, and 15 years at the time of disclosure explained further.
[I] just let them know that I would be having surgery. I was having surgery, but for them to know that I wasn’t sick. That when you have prophylactic surgery, it’s kind of different because you’re well. We said that it was related to the fact that I had a gene from my family.
One disclosing parent with a mutation-positive BRCA2 discovered in 2012, an ovarian cancer diagnosis, and two children aged 11 years and 13 years at the time of disclosure detailed the steps she took to share the test results with her children.
We just sat down and explained to them what the results or findings were and . . . risk-wise, what that meant for me personally and then, risk-wise, what that meant for them being male, [and] how I was going to proceed with this information and and what a positive, really positive bit of news it is in that we have the ability then to take that information and be proactive about it. So, we very much viewed this information as a positive in our lives.
Another disclosing parent with a mutation-positive BRCA2 discovered in 2011, an unaffected cancer status, and one child aged 14 years at the time of disclosure echoed these thoughts.
I told her we have cancer in our family, and I was glad to have the information. I said that people who are BRCA2 positive don’t necessarily get cancer, that most people who get cancer have no genetic reason for it. I was lucky in some ways because I can be proactive by having surgeries to lower my cancer incidence. I talked about eating healthy, not smoking or drinking. They were things she could do now to limit her chances of having cancer, heart disease, diabetes. They were all good things to do anyways. That there was no reason to worry, and she didn’t have to make any decisions now about testing. The conversation was in the car, where all deep conversations take place.
Knowledge Deficit
An assessment of the 15 study participants’ transcripts revealed that some parents lacked knowledge regarding specific BRCA1/2 information. Five of the study participants self-identified the need for additional information about a specific topic or were unconscious of the existence of a knowledge deficit. Of these five study participants, two disclosing parents and three nondisclosing parents were classifed as having a knowledge deficit in the following areas: BRCA1/2 risk factors, the risk of inheritance, the impact of a defective BRCA1/2 gene on men, screening recommendations for men, considerations regarding insurance, and BRCA1/2 genetic testing eligibility. A knowledge deficit in the aforementioned areas may have influenced parental decision making one way or another, with the consequence of disclosing parents sharing misinformation with minors. Parental knowledge deficit reinforces the need for additional parental education and supplemental resources.
A disclosing parent with mutation-positive BRCA2 discovered in 2009, a breast cancer diagnosis, and three children at the time of disclosure (aged 18 months [not eligible], 6 years [not disclosed], and 9 years [disclosed]) said she was “saddened a bit just in knowing” that, if she carries the gene, “then, out of three children, [it is] very likely at least one of them will carry.” A nondisclosing parent with a mutation-positive BRCA1 discovered in 2011, a breast cancer diagnosis, and one child aged 15 years at the time of parental test result said she was uncertain of how to proceed with the information with a male child.
It does become sort of less clear to me with a male. I mean, obviously, a son, if they marry and have children . . . they have the potential to have daughters. I’m not sure at what point it sort of becomes more important for him to have this information because how would it change what medical follow-up he has at this point?
Parental Recommendations
Despite feeling comfortable with the decision to disclose or not to disclose, the majority of parents requested clinicians’ guidance with if, when, what, and how to disclose; referrals to allied healthcare professionals; a list of reliable Internet sites, and a helpline for children. Parents also requested reading materials that were specific to disclosure or nondisclosure, age and language appropriate, and targeted to mutation-positive BRCA1/2 carrier parents and minors. The following dialogue exemplifies a few of these ideas:
PI: What kind of supports do you think would help other families regarding disclosing genetic test results to minors?
Participant (disclosing parent with a mutation-positive BRCA2 discovered in 2011, an unaffected cancer status, and two children aged 11 years and 14 years at the time of disclosure): I think it would be really good for the parents who choose to share it with their minor children, if they did have some kind of education forum, a workshop in kid-friendly language, graphics, and charts. Even if they had an information package for kids, saying, “This is what it means, and it doesn’t mean that your parent is going to have this.” . . . I think brochures, pamphlets, and even a kids help phone that they can call if they have questions. . . . If you need tips or guidelines, or this is how you could discuss it with your kid; maybe there could be some assistance in that regard.
One disclosing parent with a mutation-positive BRCA2, a breast cancer diagnosis, and two children aged 9 years and 12 years at the time of disclosure suggested having some way to explain the information to children: “Is there some type of place you could go to help you choose your words for them to understand at their level? Or some type of visual [on the] Internet where you can go for a visual presentation for them to understand at their level?” One nondisclosing parent with a mutation-positive BRCA1 discovered in 2011, a breast cancer diagnosis, and one child aged 15 years at the time of parental test result wanted to know “the pros and the cons of disclosure.”
Aside from the insurance pieces, are there other kinds of cons to knowing this information? What are other people concerned about? What are people’s experiences . . . when they sort of give this information to their family? What about males—what sort of impact does it have? Are there certain tests and things that they should be having? I’m not sure about that because, again, the information I’ve gotten has been a little bit inconsistent.
As part of the decision-making process, participants recommended that other parents with mutation-positive BRCA1/2 consider each child’s individual characteristics, family needs, and life situations. As one disclosing parent with a mutation-positive BRCA2 discovered in 2012, an unaffected cancer status, and two children aged 9 years and 11 years at the time of disclosure noted, “Go at your own pace, and, before you jump in, be mindful of what you’re doing.” Collectively, study participants encouraged parents to be honest and to prepare to engage in a series of discussions. One nondisclosing parent with a mutation-positive BRCA2 diagnosed in 2011, an unaffected cancer status, and one child aged 6 years at the time of parental test result touched on a number of these points.
It’s ultimately your decision to make. It’s your child, and nobody knows that child better than yourself and how they’re going to react. I think withholding it completely is not very good either. I mean, she deserves to know.
One nondisclosing parent with a mutation-positive BRCA1 discovered in 2012, a breast cancer diagnosis, and one child aged 6 years at the time of parental test result said the decision is an individual one.
Whatever you do is the right thing for you to do. It’s not right or wrong. It’s not a one-time conversation. Kids usually process it in little bits and pieces, so they will come back two weeks later or two months later with a little follow-up question. You have to be prepared that the conversation is not over. You’ve opened the conversation. If you present it in a way the kids feel safe to approach this topic, it will be an ongoing conversation.
Discussion
This study’s research question assessed parental perceptions regarding the disclosure or nondisclosure of a mutation-positive BRCA1/2 test result to minors. The research question was derived based on the PI’s personal assessment of what appeared to be a gap in clinical services specific to the mutation-positive BRCA1/2 population. A review of the literature also uncovered a research gap specific to parental decision making regarding the disclosure or nondisclosure of mutation-positive BRCA1/2 test results to minors.
The findings from this study are consistent with those from other studies (Bradbury et al., 2012; Segal et al., 2004; Tercyak et al., 2013). For example, a majority (n = 9) of study participants disclosed a mutation-positive test result to at least one or more offspring within one or two months of a confirmed status, and nondisclosing parents believed that disclosure should occur during adulthood. In addition, for disclosing parents, the mutation-positive BRCA1/2 carrier was the lead conversationalist during disclosure discussions, which often occurred as unscheduled conversations in the company of core family members. Clarke et al.’s (2008) findings indicated that parents may mislead children in unplanned disclosure situations; however, disclosing parents in this study responded truthfully when minors questioned them about BRCA1/2 testing, despite some feelings of decisional conflict. Similar to Rowland and Metcalfe (2013), these parents presented BRCA1/2 information in a series of positive, relaxed, and reassuring conversations that mirrored an age-appropriate developmental approach. Nondisclosing and disclosing parents encouraged other parents to take a step-by-step, age-appropriate developmental approach during their disclosure conversations with minors. Both categories of parents advocated for disclosure because they felt strongly that genetic risk information belonged to the entire family. Parents’ overall assessment was that genetic clinicians offered satisfactory education and supportive care. However, similar to other study findings, parents expressed that clinicians’ information sharing specific to the topic of mutation-positive BRCA1/2 disclosure or nondisclosure and referrals to professional counseling and community programs were limited (O’Neill, 2015; Rowland & Metcalfe, 2013). Subsequently, parents needed to independently seek out resources and encouraged clinicians to take the mutation-positive BRCA1/2 conversation a step further by initiating dialogue regarding if, when, what, and how to disclose or not to disclose to minors.
Factors that influenced parental decision making regarding disclosure or nondisclosure included the gender, age, maturity, and cognitive developmental stage of the offspring. In addition, the family’s psychological welfare, the offspring’s early involvement regarding the initiation of genetic testing, and familial experiences with cancer were taken into consideration. However, for the most part, parents were concerned about children’s emotional health because they did not want to negatively affect their psychological state. Parents also realized that their own emotional preparation at the time of disclosure would play a role in the children’s response. Rowland and Metcalfe (2013) reported a positive association between disclosure and parent–child well-being. In addition, disclosing parents were committed to the principle of honesty. Clarke et al. (2008) documented disclosing parents’ pledge to honesty that was tempered by their instinct to protect children. These conflicting beliefs led some parents to misrepresent information when children unexpectedly approached the topic with parents (Clarke et al., 2008). In this study, participants reported no parental misrepresentations.
Children’s gender was not collected as part of the study’s demographic information. However, detailed assessments of study transcripts identified a predominance of male offspring. The research literature has documented parental concerns specific to female offspring that included cancer screening, prophylactic options, and relationship issues (Clarke et al., 2008). Parents in this study did not voice any concerns pertaining to their daughters. In addition, they verbalized that the male offspring would readily adapt to familial risk information that is tempered by their knowledge of a low incidence of breast cancer in males and the availability of surveillance options. The predominance of male offspring may have influenced disclosure rates by parents in this study; all participants were female mutation-positive BRCA1/2 carriers with male offspring dominance. Future studies that compare the impact of offspring gender on dynamics around disclosure or nondisclosure are warranted.
Consistent with other findings, disclosing and nondisclosing parents perceived mutation-positive BRCA1/2 testing to be a positive healthcare tool, despite complex issues associated with genetic testing (Clarke et al., 2008; Ratnayake et al., 2011). In this study, life-altering decisions rested solely on single parents’ shoulders, which may have contributed toward their lower rates of disclosure. Consequently, single-parent status may be an indicator for additional support and educational assistance from clinicians. Disclosing parents believed that discussions with minors about their family’s genetic health history would encourage children’s self-health advocacy roles in adulthood and promote body awareness and healthy lifestyle choices, which has been supported in studies (Bradbury et al., 2012; Rowland & Metcalfe, 2013). In this study, nondisclosing parents equated preparing minors for the future with obtaining information from clinicians that detailed insurance discrimination issues. To better address parents’ and minors’ need for information, study participants suggested clinicians offer parents a list of easy-to-navigate Internet sites, informative group sessions, take-home educational materials, and follow-up clinician consultations.
A mutation-positive test result and medical confirmation of a cancer diagnosis within a close time frame influenced parents’ decision making as they faced their own mortality. Parents’ disclosure was also affected by their or an extended family member’s cancer journey or the child’s early participation in genetic testing discussions. Mortality-related life stressors may have affected parents’ cognitive understanding and critical-thinking skills, which could have contributed to parental knowledge deficits. In addition, parental recall bias may be influenced by a delayed disclosure time of two to three months after a mutation-positive BRCA1/2 test result confirmation. These issues, coupled with clinicians’ limited involvement in parental decision making, may have negative consequences on parents’ coping styles, core and extended family interactions, and parental understanding of risk information and critical thinking (Daly et al., 2001; O’Neill et al., 2015). Consequently, these factors could have contributed to the inaccurate knowledge transfer from parent to child, which was identified by the study’s PI. A holistic approach to health care is paramount to supporting the lived experiences of study participants’ perceptions regarding parental decision making. The implementation of genetic consultation recordings could assist parental information recall by preserving the content shared during mutation-positive BRCA1/2 consultations, which may foster accurate communication of risk information to minors (Hack, Ruether, Weir, Grenier, & Degner, 2013). This clinical recommendation is based on the lived experience of the PI with the use of consultation recordings with individuals and families in breast oncology consultations. A holistic healthcare process would also include conducting an initial family psychosocial assessment and initiating early psychosocial referrals. Ongoing psychosocial assessments along the genetic pathway would be critical.
Limitations
Several study limitations warrant acknowledgement. The retrospective nature of the study design may introduce participant recall bias. In addition, study participants’ recommendations for clinicians to take the consultation conversations a step further may no longer be valid as a result of the implementation of clinical changes since the time of the study participants’ genetic testing and data collection. Study findings are limited because of a focus on the lived experience specific to the mutation-positive BRCA1/2 population; in addition, data were collected at one point in time from a relatively small sample size. The study population was also homogenous because it primarily reflected the views of an educated Caucasian female population of middle to higher socioeconomic status who were mutation-positive BRCA1/2 parents of mainly male offspring. Based on these limitations, study findings cannot be generalized to the population at large (Streubert & Carpenter, 2011).
Implications for Nursing
Clinicians in genetic counseling are encouraged to take their mutation-positive BRCA1/2 test result consultations a step further by engaging parents in conversations that are specific to decision making about disclosure or nondisclosure to minors. In addition, follow-up consultation visits should be offered and appropriate referrals should be facilitated to allied clinicians. As the use of genomics in health care increases, genetics interprofessional teams (clinical physicians, nurses, and psychosocial clinicians) need to collaborate in the development of resources specific to the needs of mutation-positive BRCA1/2 carriers faced with disclosure or nondisclosure to minors.
Oncology nurses affiliated with genetics departments are positioned to offer genetics teams support with high-risk individuals in the BRCA1/2 population. These specialized nurses are encouraged to conduct personalized assessments specific to parent–child risk information and psychosocial needs. Personalized assessments should take unique personalities, characteristics, learning requirements, and life issues into consideration when, in conjunction with the parent, nurses construct a decisional and parental teaching guide. Personalized assessments may help nurses to identify appropriate parent–child resources, such as topic-specific education sessions, literature, reliable Internet sites, and referrals to community programs and services. Oncology nurses are encouraged to review research literature on hereditary breast and ovarian education, join genetics journal clubs, attend genetics meetings and conferences, and attain certification in advanced oncology programs, such as those offered by the Oncology Nursing Certification Corporation.
A need exists for future qualitative, quantitative, and mixed-methods design studies that provide greater depth of understanding about parental disclosure or nondisclosure of mutation-positive BRCA1/2 test results to male and female minors. Specifically, studies assessing the perceptions of mutation-positive BRCA1/2 men, individuals from the gay community, individuals from lower socioeconomic statuses, and diverse ethnic communities are warranted. A gap exists regarding mutation-positive BRCA1/2 communication between fathers and minors. In addition, perceptions of the genetic and oncology clinicians’ information needs warrant investigations.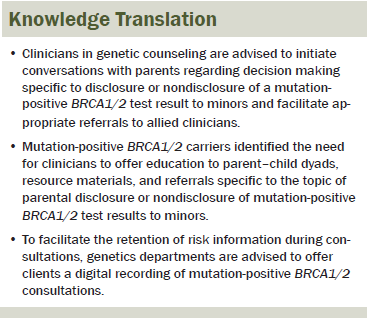
Conclusion
This study contributes to the published research gap specific to parental decision making related to the disclosure or nondisclosure of a mutation-positive BRCA1/2 test result to minors. Study findings corroborate international evidence specific to parental decision making regarding influential factors. Parents in this study collectively voiced the need for clinicians to take the mutation-positive BRCA1/2 conversation a step further by directly acknowledging the topic with parents. Clinicians are encouraged to structure conversations that directly assess parental decision making regarding the disclosure or nondisclosure of a mutation-positive BRCA1/2 to minors, as well as offer follow-up consultations, educational resources, and appropriate referrals. Ongoing research is required to better develop the evidence base for practice guidelines in support of parental decision making regarding the disclosure or nondisclosure of mutation-positive BRCA1/2 test results to minors.
The authors gratefully acknowledge the study participants for sharing their stories and the western Canadian hereditary breast and ovarian cancer clinic used as a recruitment site in this study for its support.
References
Bradbury, A.R., Dignam, J.J., Ibe, C.N., Auh, S.L., Hlubocky, F.J., Cummings, S.A., . . . Daugherty, C.K. (2007). How often do BRCA mutation carriers tell their young children of the family’s risk for cancer? A study of parental disclosure of BRCA mutations to minors and young adults. Journal of Clinical Oncology, 25, 3705–3711. doi:10.1200/jco.2006.09.1900
Bradbury, A.R., Patrick-Miller, L., Egleston, B.L., Olopade, O.I., Daly, M.B., Moore, C.W., . . . Daugherty, C.K. (2012). When parents disclose BRCA1/2 test results: Their communication and perceptions of offspring response. Cancer, 118, 3417–3425. doi:10.1002/cncr.26471
Bradbury, A.R., Patrick-Miller, L., Pawlowski, K., Ibe, C.N., Cummings, S.A., Hlubocky, F., . . . Daugherty, C.K. (2009). Learning of your parent’s BRCA mutation during adolescence or early adulthood: A study of offspring experiences. Psycho-Oncology, 18, 200–208. doi:10.1002/pon.1384
Braithwaite, D., Emery, J., Walter, F., Prevost, A.T., & Sutton, S. (2006). Psychological impact of genetic counseling for familial cancer: A systematic review and meta-analysis. Familial Cancer, 5, 61–75. doi:10.1007/s10689-005-2577-1
Canadian Cancer Society’s Advisory Committee on Cancer Statistics. (2013). Canadian cancer statistics 2013. Retrieved from http://bit.ly/25Vf8Rg
Clarke, S., Butler, K., & Esplen, M.J. (2008). The phases of disclosing BRCA1/2 genetic information to offspring. Psycho-Oncology, 17, 797–803. doi:10.1002/pon.1344
Crotser, C.B., & Boehmke, M. (2009). Survivorship considerations in adults with hereditary breast and ovarian cancer syndrome: State of the science. Journal of Cancer Survivorship, 3, 21–42. doi:10.1007/s11764-008-0077-7
Daly, M.B., Barsevick, A., Miller, S.M., Buckman, R., Costalas, J., Montgomery, S., & Bingler, R. (2001). Communicating genetic test results to the family: A six-step, skills-building strategy. Family and Community Health, 24, 13–26. doi:10.1097/00003727-200110000-00004
Finlay, E., Stopfer, J.E., Burlingame, E., Evans, K.G., Nathanson, K.L., Weber, B.L., . . . Domchek, S.M. (2008). Factors determining dissemination of results and uptake of genetic testing in families with known BRCA1/2 mutations. Genetic Testing, 12, 81–91. doi:10.1089/gte.2007.0037
Guba, E.G., & Lincoln, Y.S. (1994). Competing paradigms in qualitative research. In N.K. Denzin & Y.S. Lincoln (Eds.), Handbook of qualitative research (pp. 105–117). Thousand Oaks, CA: Sage.
Hack, T.F., Ruether, J.D., Weir, L.M., Grenier, D., & Degner, L.F. (2013). Promoting consultation recording practice in oncology: Identification of critical implementation factors and determination of patient benefit. Psycho-Oncology, 22, 1273–1282. doi:10.1002/pon.3135
Hallowell, N., Arden-Jones, A., Eeles, R., Foster, C., Lucassen, A., Moynihan, C., & Watson, M. (2006). Guilt, blame and responsibility: Men’s understanding of their role in the transmission of BRCA1/2 mutations within their family. Sociology of Health and Illness, 28, 969–988. doi:10.1111/j.1467-9566.2006.00515.x
Hallowell, N., Ardern-Jones, A., Eeles, R., Foster, C., Lucassen, A., Moynihan, C., & Watson, M. (2005). Men’s decision-making about predictive BRCA1/2 testing: The role of family. Journal of Genetic Counseling, 14, 207–217. doi:10.1007/s10897-005-0384-3
Hamilton, J.G., Lobel, M., & Moyer, A. (2009). Emotional distress following genetic testing for hereditary breast and ovarian cancer: A meta-analytic review. Health Psychology, 28, 510–518. doi:10.1037/a0014778
Howard, A.F., Balneaves, L.G., & Bottorff, J.L. (2009). Women’s decision making about risk-reducing strategies in the context of hereditary breast and ovarian cancer: A systematic review. Journal of Genetic Counseling, 18, 578–597. doi:10.1007/s10897-009-9245-9
Lopez, K.A., & Willis, D.G. (2004). Descriptive versus interpretive phenomenology: Their contributions to nursing knowledge. Qualitative Health Research, 14, 726–735. doi:10.1177/1049732304263638
MacKenzie, A., Patrick-Miller, L., & Bradbury, A.R. (2009). Controversies in communication of genetic risk for hereditary breast cancer. Breast Journal, 15(Suppl. 1), S25–S32. doi:10.1111/j.1524-4741.2009.00800.x
Meiser, B., & Halliday, J.L. (2002). What is the impact of genetic counselling in women at increased risk of developing hereditary breast cancer? A meta-analytic review. Social Science and Medicine, 54, 1463–1470. doi:10.1016/s0277-9536(01)00133-2
Metcalfe, A., Plumridge, G., Coad, J., Shanks, A., & Gill, P. (2011). Parents’ and children’s communication about genetic risk: A qualitative study, learning from families’ experiences. European Journal of Human Genetics, 19, 640–646. doi:10.1038/ejhg.2010.258
O’Neill, S.C., Mays, D., Patenaude, A.F., Garber, J.E., DeMarco, T.A., Peshkin, B.N., . . . Tercyak, K.P. (2015). Women’s concerns about the emotional impact of awareness of heritable breast cancer risk and its implications for their children. Journal of Community Genetics, 6, 55–62. doi:10.1007/s12687-014-0201-5
Patenaude, A.F., DeMarco, T.A., Peshkin, B.N., Valdimarsdottir, H., Garber, J.E., Schneider, K.A., . . . Tercyak, K.P. (2013). Talking to children about maternal BRCA1/2 genetic test results: A qualitative study of parental perceptions and advice. Journal of Genetic Counseling, 22, 303–314. doi:10.1007/s10897-012-9549-z
Peshkin, B.N., DeMarco, T.A., & Tercyak, K.P. (2010). On the development of a decision support intervention for mothers undergoing BRCA1/2 cancer genetic testing regarding communicating test results to their children. Familial Cancer, 9, 89–97. doi:10:1007/s10689-009-9267-3
Ratnayake, P., Wakefield, C.E., Meiser, B., Suthers, G., Price, M.A., Duffy, J., & Tucker, K. (2011). An exploration of the communication preference regarding genetic testing in individuals from families with identified breast/ovarian cancer mutations. Familial Cancer, 10, 97–105. doi:10.1007/s10689-010-9383-0
Rowland, E., & Metcalfe, A. (2013). Communicating inherited genetic risk between parent and child: A meta-thematic synthesis. International Journal of Nursing Studies, 50, 870–880. doi:10.1016/j.ijnurstu.2012.09.002
Schlich-Bakker, K.J., ten Kroode, H.F., & Ausems, M.G. (2006). A literature review of the psychological impact of genetic testing on breast cancer patients. Patient Education and Counseling, 62, 13–20. doi:10.1016/j.pec.2005.08.012
Seenandan-Sookdeo, K.I., & Sawatzky, J.V. (2010). Risk assessment for hereditary breast cancer: BRCA1 and BRCA2. Canadian Oncology Nursing Journal, 20, 107–115. doi:10.5737/1181912x203107110
Segal, J., Esplen, M.J., Toner, B., Baedorf, S., Narod, S., & Butler, K. (2004). An investigation of the disclosure process and support needs of BRCA1 and BRCA2 carriers. American Journal of Medical Genetics, 125A, 267–272. doi:10.1002/ajmg.a.20485
Streubert, H.J., & Carpenter, D.R. (2011). Qualitative research in nursing: Advancing the humanistic imperative (5th ed.). Philadelphia, PA: Lippincott Williams and Wilkins.
Tercyak, K.P., Mays, D., DeMarco, T.A., Peshkin, B.N., Valdimarsdottir, H.B., Schneider, K.A., & Patenaude, A.F. (2013). Decisional outcomes of maternal disclosure of BRCA1/2 genetic test results to children. Cancer Epidemiology, Biomarkers, and Prevention, 22, 1260–1266. doi:10.1158/1055-9965.EPI-13-0198
Tercyak, K.P., Peshkin, B.N., DeMarco, T.A., Brogan, B.M., & Lerman, C. (2002). Parent-child factors and their effect on communicating BRCA1/2 test results to children. Patient Education and Counseling, 47, 145–153. doi:10.1016/s0738-3991(01)00192-6
van Manen, M. (1990). Researching lived experience: Human science for an action sensitive pedagogy. Albany, NY: State University of New York Press.
About the Author(s)
Seenandan-Sookdeo is an adjunct nursing faculty member in the Faculty of Nursing at Minneapolis Community and Technical College in Minnesota; Hack is a professor in the College of Nursing, Lobchuk is an associate professor and Manitoba Research Chair in Caregiver Communication in the College of Nursing and Faculty of Health Sciences, and Murphy is a professor in the Department of Biochemistry and Medical Genetics, all at the University of Manitoba in Winnipeg, Canada; and Marles is a clinical geneticist at the Health Sciences Centre in Winnipeg, Manitoba, Canada. This research was funded by Hack’s Canadian Breast Cancer Foundation (Prairies/NWT) Chair in Psychosocial and Supportive Care Oncology Research, the Foundation for Registered Nurses of Manitoba, Inc., Graduate Award, the Marion Saydak Memorial Scholarship, and Lesley F. Degner’s Chair in Evidence-Based Nursing Practice Graduate Studies Tuition Award from the Canadian Institute of Health Research, all awarded to Seenandan-Sookdeo. Seenandan-Sookdeo contributed to the conceptualization and design, data collection, and analysis. Seenandan-Sookdeo, Hack, Lobchuk, Murphy, and Marles contributed to the manuscript preparation. Seenandan-Sookdeo can be reached at kendraanniss@gmail.com, with copy to editor at ONFEditor@ons.org. Submitted January 2015. Accepted for publication July 11, 2015.

