Improving Nurses’ Knowledge About Older Adults With Cancer
Purpose/Objectives: To assess nurses’ knowledge, attitudes, and perceptions of caring for older adults and to use that assessment data to develop a training program to improve skills in caring for older adults with cancer.
Design: Survey of oncology nursing staff conducted pre- and posteducation regarding geriatric care.
Setting: City of Hope, a comprehensive cancer center in southern California.
Sample: 422 (baseline) and 375 (postintervention) nursing staff in adult care areas.
Methods: The primary endpoint was the difference between baseline and postintervention knowledge. Secondary endpoints included differences in attitudes and perceptions of caring for older adults in an oncology setting. A two-sample t test was performed to compare the mean results between baseline and follow-up surveys.
Main Research Variables: Knowledge, attitudes, and perceptions of caring for older adults.
Findings: Survey comparisons from baseline to postintervention demonstrated statistically significant increases in nurses’ knowledge of geriatric care after the implementation of an educational program targeted at oncology nurses. Nurses’ attitudes remained the same pre- versus posteducation. A significant change reflecting a better perception was noted in the burden of behavioral problems; however, a worsening was noted in disagreements among staff; disagreements involving staff, patients, and families; and limited access to geriatric services. Both surveys highlighted the need to provide more education for staff about geriatric care issues and to make available more geriatric-specific resources.
Conclusions: Knowledge about caring for older adults is needed for oncology nurses, and a geriatric education program for oncology nurses can result in improved knowledge in a variety of domains. Surveying staff highlighted the positive attitude of nurses toward caring for older adults at the study institution. The use of this survey identified key issues facing older adults and ways to improve care.
Implications for Nursing: Additional knowledge about caring for older adults for oncology nurses and assistive staff is needed to prepare for the increasing population of older adults with cancer. Continuous learning is key to professional development, and more research is needed on how to best continue to integrate knowledge of geriatric concepts into oncology care.
Jump to a section
Life expectancy in the United States is increasing, and the number of baby boomers aged 65 years and older is expected to almost double, to 70 million or 20% of the U.S. population, by the year 2030 (Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine [HMD], 2008). The risk of developing cancer increases with age (Jemal et al., 2008), and data from the Surveillance, Epidemiology, and End Results database demonstrate that 57% of patients with cancer are aged 65 years and older (National Cancer Institute, n.d.). Because of the aging U.S. population and the association of cancer with aging, this number is estimated to grow to almost 70% by 2030 (Smith, Smith, Hurria, Hortobagyi, & Buchholz, 2009). In contrast, a relatively modest increase of 11% in cancer incidence among adults aged less than 65 years is expected.
These demographics reveal that most oncology professionals are caring for an older patient population. A recommendation from the HMD (2008) report Retooling for an Aging America: Building the Healthcare Workforce noted that, “to meet the health care needs of the next generation of older adults, the geriatric competence of the entire workforce needs to be enhanced . . . [and] innovative models need to be developed and implemented” (p. 6). This HMD (2008) report highlighted the conclusion that all members of the healthcare team will need to have specialized knowledge in geriatrics to meet the needs of the aging patient. Oncology nurses in particular must gain expertise in geriatric care. The HMD (2008) report called for a substantial focus in the healthcare infrastructure to provide skilled care to this vulnerable population. In addition, another HMD (2013) report, Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis, reinforced the recommendations to develop geriatric competence to improve the quality of cancer care.
Nurses play a key role in the care of older adults with cancer; consequently, most oncology nurses are working in geriatrics without training as geriatric nurses. Despite the rapid increase in the U.S. aging population, a shortage of healthcare specialists with geriatric training remains. The education of oncology nurses focuses primarily on oncology itself, rather than on geriatric information and training. A survey that measured knowledge, attitudes, and perceptions of geriatric care was conducted at a comprehensive cancer center to detect changes before and after implementing a geriatric educational program (Burhenn, Johnson, & Hurria, 2013). A major goal of the current project was to evaluate the efficacy of a geriatric-focused education program for oncology nurses. The primary goal of this study was to assess the attitudes, knowledge, and perceptions of caring for older adults among nurses and patient care assistants at City of Hope, a comprehensive cancer center in Duarte, California. Other objectives were to use the assessment data to develop a training program for nurses and assistants to improve skills in caring for older adults with cancer. The conceptual framework for this study was based on four domains described by Nurses Improving Care for Healthsystem Elders (NICHE), a nurse-driven organization with the goal of improving care of older adults, and six knowledge areas outlined by the Oncology Nursing Society (ONS) in the Caring for the Older Adult With Cancer course. The NICHE domains were (a) nurse knowledge of geriatric care, (b) nurse attitudes for caring for older adults, (c) perceptions of professional issues about caring for older adults, and (d) perceptions of the geriatric care environment (NICHE, n.d.). The educational course on geriatrics for the oncology nurse created by ONS contained geriatric knowledge content about the following six areas of care: (a) age- and disease-related changes, (b) comorbidities, (c) cognitive and neuropsychiatric disorders, (d) psychosocial issues, (e) other geriatric care issues (e.g., polypharmacy, fall reduction, caregiver support), and (f) resources and patient education. This framework guided the selection of the survey and the analysis of the results.
Methods
Design and Sample
Data for this analysis were obtained from a survey of nursing staff at this comprehensive cancer center that was administered at baseline in April 2012 (year 1) and one year later in April 2013 (year 2) to assess the attitudes, knowledge, and perceptions of caring for older adults. The aggregate data identify and summarize target areas for improvement in geriatric knowledge and care practices.
Study participants consisted of nurses and patient care assistants who were eligible to participate if they were permanently employed at the study institution and worked in adult care areas. Each time the survey was sent out, it went to the current database of employed staff that met those criteria. Because staffing changes year to year, this resulted in a sample of a different population of staff from year to year. Staff who took the survey were not required to have participated in the previous year or attend the intervention classes that were offered.
Procedures
The survey was sent to all qualifying staff members via an email from the chief nursing officer with a link to participate in the study by completing the survey. Alternatively, participants could complete a paper copy of the survey, which was distributed at nursing meetings and returned anonymously to the principal investigator via interoffice mail. The results from paper and computerized surveys were not identifiable to a specific staff member. Follow-up reminder emails were sent weekly for three weeks to encourage participation. Target accrual was 450 surveys per timepoint (pre- and posteducation). To encourage participation, survey respondents could enter a drawing for a $50 gift certificate. Participation in the study was voluntary, and nursing staff members were aware that this was a research study.
Intervention
A geriatric-focused educational initiative was implemented after the baseline Geriatric Institutional Assessment Profile (GIAP) was completed. This program consisted of a four-hour didactic presentation that was developed by ONS; the first author of the current study was an approved trainer for this program. This course was offered five times following the baseline survey in May, July, August, October, and December 2012 and was voluntarily attended by a total of 83 staff members. A 20-hour geriatric resource nurse course (the core curriculum for all NICHE sites) was also piloted on one unit during this time.
Instruments
The survey used the GIAP, which is a self-completed survey for healthcare professionals designed to quantify staff knowledge, attitudes, and perceptions in the care of older adult patients via the assessment of the four domains previously described (NICHE, n.d.). Demographic data (gender, age, years in the profession, years at the institution, race and ethnicity, position held) were also collected in the survey. This survey, developed by NICHE, has demonstrated good reliability and validity (for knowledge, the Cronbach alpha was greater than 0.85; for attitudes, the Cronbach alpha was greater than 0.7), is computer-based, and takes about 15 minutes to complete (Boltz, Capezuti, Kim, Fairchild, & Secic, 2009, 2010; Capezuti et al., 2013; NICHE, n.d.). For pre- and postsurvey, the scales used for knowledge and attitudes were scored using a scale of 0–10, with a higher score representing better results. However, responses for professional issues were scored from 0–10, with a lower score representing better perception of issues.
This research was conducted in compliance with federal and state of California requirements relating to protected health information (PHI). This survey was not a patient database and did not include any PHI or individually identifiable health information as defined by the Health Insurance Portability and Accountability Act privacy rule. The study was approved by the institutional review board at City of Hope.
Statistical Methods
Following completion of the survey period, GIAP data were analyzed by NICHE staff, and a report was provided that compared this institution’s staff responses against staff responses at other hospitals in the database. A comparison between initial GIAP (year 1) and post-intervention GIAP (year 2) for the institution was also offered. The survey benchmarking included healthcare staff of participating NICHE facilities across the United States and Canada who have completed the survey (N = 93,811). In a later analysis with more than 100,000 surveys in the database, a secondary data analysis was done, which reported the validity and reliability of the survey (Capezuti et al., 2013). A simple two-sample t test was performed to compare the means of the benchmark database and participants’ responses at this comprehensive cancer center (NICHE, n.d.).
Results
A total of 422 staff completed the survey in 2012 (year 1) and 375 in 2013 (year 2). This represented response rates of 44% and 41% of the nursing staff, respectively. Demographics of respondents were similar between years (see Table 1). The participants were primarily women (87% in year 1, 82% in year 2) who were staff nurses (69% in year 1, 67% in year 2) and had been in the profession for about 17 years and had worked at the study institution for about 10 years. Compared to the benchmark data, these demographics were similar, except in race and ethnicity. In particular, the institution in this study had a lower percentage of Caucasian and African American nursing staff and a higher percentage of Hispanic, Asian, and “declined to respond” participants.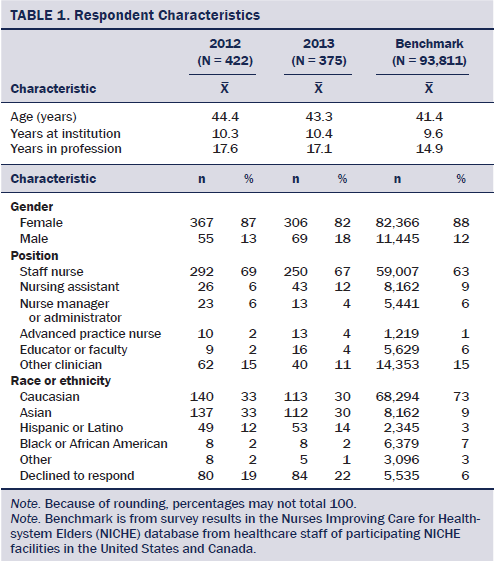
Knowledge was surveyed only for RN respondents, so the population is slightly lower than the overall number of respondents (N = 406, 96% in year 1; N = 360, 96% in year 2). The survey results demonstrated a statistically significant improvement in geriatric knowledge of the nurses between surveys (Burhenn et al., 2013) (see Table 2). Knowledge of geriatric conditions improved significantly from year 1 to year 2 in each area studied. A 16% increase in knowledge regarding restraints was noted, along with a 15% increase in knowledge regarding pressure ulcers, a 16% increase in knowledge regarding incontinence, a 16% increase in knowledge regarding sleep, and a 16% increase in total knowledge.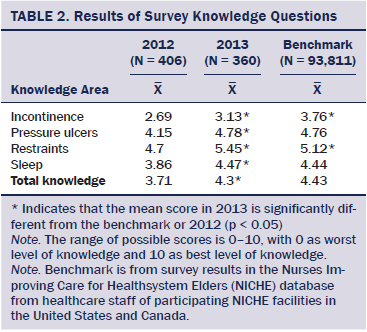
Attitudes regarding caring for the older adult, also answered only by RNs, were higher than the benchmark data at this institution in three areas; however, only one area reached significance (see Table 3). The total number of respondents varied because not all nurses answered all sections of the survey. No significant change in attitudes was noted from year 1 to year 2. Attitudes were measured for the same four parameters as knowledge (restraints, pressure ulcers, sleep, and incontinence). Scoring on attitudes from year 1 to year 2 revealed changes in the areas of incontinence, pressure ulcers, restraints, and sleep.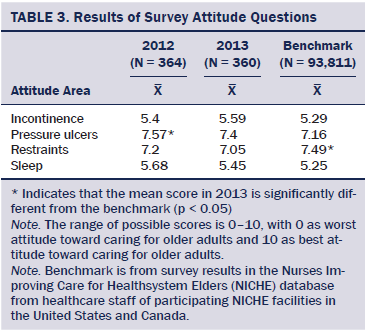
The professional issues scale includes questions about disagreements among staff or involving staff, patients, and family members about older adult treatment, access to geriatric services, perceived vulnerability to legal action, intensity of behavioral problems, and the burden of behavioral problems of older adults. No change was observed from year 1 to year 2 for perceived legal vulnerability or intensity of behavioral problems. A significant change reflecting a better perception was noted in the burden of behavioral problems; however, a worsening was found in disagreements among staff; disagreements involving staff, patients, and family members; and limited access to geriatric services. Compared to the benchmark data, the institution in this study was significantly poorer in the areas of disagreements among staff and involving staff, patients, and family members and perceived vulnerability to legal action, but better in the areas of limited access to geriatric services and intensity of behavioral problems. No difference was noted in the burden of behavioral problems (see Table 4).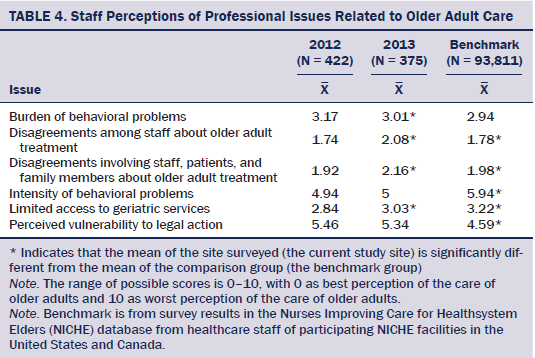
The final section of the questionnaire, the geriatric care environment, asks about the facilitators and barriers to care for the older adult. From year 1 to year 2, no change was observed in any of the categories described. However, compared to benchmark, the institution in this study scored significantly higher in the area of delivery of age-sensitive care but lower in the area of capacity for collaboration. No difference was noted in resource availability, the institution valuing the older adult, or the overall geriatric care environment (see Table 5). 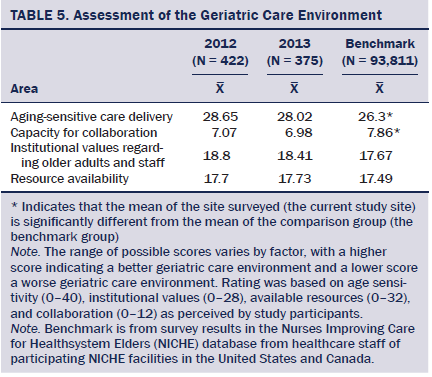
The survey included open-ended questions about pressing issues that staff face in caring for older adults, reaction to the survey, and what would improve care for older adults. These questions provided additional detail that drove the development of the educational program. The number of comments differs from the number of respondents because not all participants provided a comment (N = 241 in 2012, N = 174 in 2013). The qualitative data presented as “pressing issues” suggested five themes, which are outlined in Table 6. In the pre- and postintervention surveys, the main themes identified were family and caregiver support and patient safety. The top five suggested ways of improving care for older adult patients are listed in Table 7. Both surveys suggested providing education for staff and increasing the availability of geriatric-specific resources.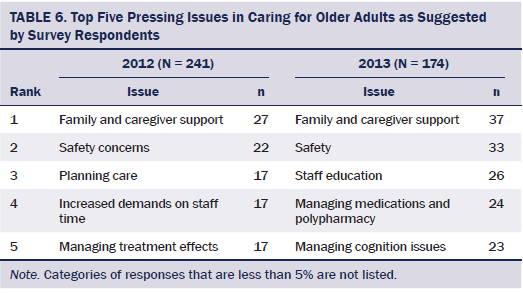
Discussion
This research demonstrated that improving geriatric knowledge at a comprehensive cancer center can be done through a directed educational program. The knowledge scores were lower than the attitude scores at this institution. High attitudes and low knowledge may indicate a desire to provide appropriate care to the older adult, and staff may need additional assistance in recognizing the need for this knowledge (NICHE, n.d.). An analysis of studies using the GIAP found mixed results regarding significant improvement in knowledge scores pre- and posteducation. However, four studies concluded that continuing education can improve knowledge and attitudes regarding geriatric care (Tavares & da Silva, 2013). Various sources have suggested that additional education is needed in geriatrics. 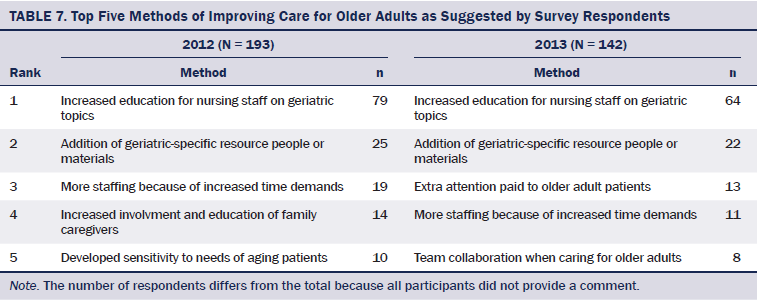
The HMD (2008) report focusing specifically on the healthcare needs of the aging population found that most healthcare workers are not adequately trained in geriatrics; it called for enhancing the competence of healthcare workers in this area. At the time of the report, only one-third of baccalaureate nursing programs contained geriatric content, and just 29% had faculty certified in geriatrics (HMD, 2008). A survey of 623 baccalaureate programs of nursing noted that 92% contained geriatric content in their curricula; of those programs, only 34% offered standalone geriatric content (Berman et al., 2005). Standalone content, or a separate course in geriatrics, as compared to the integration of geriatric content into the curriculum, was associated with a higher number of faculty with the American Nurses Credentialing Center’s gerontological certification. A study of 531 associate degree nursing programs also showed that a majority integrated geriatric content into the curricula and that it comprised 10%–25% of the content that was taught (Ironside, Tagliareni, McLaughlin, King, & Mengel, 2010). Only 5% of associate degree programs reported having standalone geriatric content. The authors have called for innovative clinical models to highlight the complexities of caring for the older adult. These complexities can be lost when infused into the general curriculum, and the specialized knowledge needed to care for the older adult can be diluted (Koroknay, 2015).
Title 16 of the California Code of Regulations states that theory and clinical practice should include geriatrics (Board of Registered Nursing, 2011). In addition, the National Council of State Boards of Nursing has recommended that geriatrics be included in the curriculum and that the content address patients across the lifespan (Russell, 2012). The American Association of Colleges of Nursing developed Recommended Baccalaureate Competencies and Curricular Guidelines for the Nursing Care of Older Adults (National Council of State Boards of Nursing, 2012) in which 19 competencies to help nurse educators infuse geriatric content into their programs are outlined because “the overwhelming majority of nurses practicing in this country today are, by default, geriatric nurses, but have not had enhanced preparation in caring for this population” (p. 9). Olson and Young (1992) reported that, to provide the most effective care for older adults, healthcare professionals must know and understand the complexities and special characteristics of health and illness in this population, suggesting that continuing education should address geriatric care and dispel myths about aging while assisting with integrating current research findings into practice. The assumption cannot be made that geriatric knowledge is consistent in nursing education and that all nurses are prepared to care for older adults postgraduation.
Results from the current study identified the institution’s nurses as being sensitive to the needs of the older adult and the institution as valuing the older patient; however, results also showed that resources for geriatric oncology education were limited. The results determined that nurses wanted more information about geriatric issues and resources. This program was initiated to educate oncology nurses in the principles of geriatric care. After this initiative and to further meet the needs identified by this analysis, a 16-member interdisciplinary team was formed; this team included 12 RNs from different patient care areas who were accepted after completing a competitive application. One team member from each of the disciplines of pharmacy, clinical nutrition, social work, and rehabilitation services was included. A curriculum was developed to teach key geriatric principles to the team regarding caring for older adults with cancer. The group met monthly to review key components of the educational modules, as well as to discuss patient cases and apply the lessons learned to real situations.
Limitations
The study used a voluntary, convenience sample, which could have affected the results and may not be reflective of the institution’s nursing staff as a whole. In addition, the target to survey 450 of the institution’s nursing staff in either year was not met. Demographic data for nonresponders were not available, making knowing if differences existed between responders and nonresponders impossible. However, an analysis using the GIAP in an emergency department setting did not find differences between respondents and nonrespondents (Boltz, Parke, Shuluk, Capezuti, & Galvin, 2013). A small portion of nurses at the study institution were educated using the intervention; however, the dissemination appeared to reach a broader cohort, as evidenced by the knowledge scores. The education did not address cultural competencies; given the institution’s diverse workforce and patient population, this is an area that should be addressed in future programs. The survey was not specific to oncology care, and benchmarking the results specifically to other oncology nurses was not possible. The current authors also acknowledged that a stronger design would have been to limit the pre- and postassessments to only those nurses given the educational intervention.
Implications for Practice and Research
Although educational programs can increase nurses’ knowledge, additional research is needed to determine if increased knowledge can improve patient care or outcomes and results in practice change, as well as if nurses who participate in education modify their plans of care for patients or change their practice behaviors. Models are needed to best integrate geriatric care into the oncology care of the future. Continuous learning is key to professional development, and more research is needed regarding how to best continue to integrate knowledge of geriatric concepts into oncology care. Older adults with cancer may have different needs than the general geriatric population, and a geriatric oncology–specific tool could be developed and tested.
Conclusion
Despite the high incidence of cancer in older adults, many oncology nurses have little training beyond nursing school in caring for this population. The current authors’ research documented that geriatric knowledge is needed for oncology nurses and that a geriatric education program for oncology nurses resulted in improved knowledge in a variety of geriatric domains. The survey also highlighted the positive attitude of nurses toward caring for older adults at the study institution. Through the survey, the current authors were able to identify key issues facing older adults and ways to improve care. This institution’s assessment uncovered the need for geriatric education and resources, which resulted in the development of a program to educate nurses and other healthcare professionals. The current authors subsequently developed a team to focus initiatives to improve the care of older adults with cancer at this institution. This project was an example of how institution-specific evidence can lead to targeted education aimed at improving the care of older adults with cancer.
The next steps include continuing to address the educational needs of the nursing population in caring for older adults. The number of geriatric resource nurses specifically trained in geriatrics will be expanded to serve as resources to other staff in patient care areas. Interdisciplinary staff will also continue to be included in future educational programs. The expanded team will meet quarterly for educational sessions and to discuss issues facing older adults with cancer at this institution. The RN class will be offered annually, and a similar class has been developed for patient care assistants and ancillary assistive staff (e.g., dietary aides, physical therapy assistants) to further the education of all staff caring for older adults with cancer. Geriatric knowledge for oncology nurses and assistive staff is needed to prepare for the predicted population expansion of older adults with cancer. Research shows that this knowledge can be gained through a systematic educational approach.
References
Berman, A., Mezey, M., Kobayashi, M., Fulmer, T., Stanley, J., Thornlow, D., & Rosenfeld, P. (2005). Gerontological nursing content in baccalaureate nursing programs: Comparison of findings from 1997 and 2003. Journal of Professional Nursing, 21, 268–275. doi:10.1016/j.profnurs.2005.07.005
Board of Registered Nursing. (2011). California Nursing Practice Act with regulations and related statutes. Sacremento, CA: State of California, Department of Consumer Affairs.
Boltz, M., Capezuti, E., Kim, H., Fairchild, S., & Secic, M. (2009). Test-retest reliability of the Geriatric Institutional Assessment Profile. Clinical Nursing Research, 18, 242–252. doi:10.1177/1054773809338555
Boltz, M., Capezuti, E., Kim, H., Fairchild, S., & Secic, M. (2010). Factor structure of the Geriatric Institutional Assessment Profile’s Professional Issues Scales. Research in Gerontological Nursing, 3, 126–134. doi:10.3928/19404921-20091207-98
Boltz, M., Parke, B., Shuluk, J., Capezuti, E., & Galvin, J.E. (2013). Care of the older adult in the emergency department: Nurses views of the pressing issues. Gerontologist, 53, 441–453. doi:10.1093/geront/gnt004
Burhenn, P., Johnson, S., & Hurria, A. (2013). Improving nurses’ geriatric knowledge at a comprehensive cancer center. Journal of Geriatric Oncology, 4 (Suppl. 1), S89.
Capezuti, E., Boltz, M.P., Shuluk, J., Denysyk, L., Brouwer, J.P., Roberts, M.C., . . . Secic, M. (2013). Utilization of a benchmarking database to inform NICHE implementation. Research in Gerontological Nursing, 6, 198–208. doi:10.3928/19404921-20130607-01
Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine. (2008). Retooling for an aging America: Building the healthcare workforce. Washington, DC: National Academies Press.
Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine. (2013). Delivering high-quality cancer care: Charting a new course for a system in crisis. Washington, DC: National Academies Press.
Ironside, P.M., Tagliareni, M.E., McLaughlin, B., King, E., & Mengel, A. (2010). Fostering geriatrics in associate degree nursing education: An assessment of current curricula and clinical experiences. Journal of Nursing Education, 49, 246–252. doi:10.3928/01484834-20100217-01
Jemal, A., Siegel, R., Ward, E., Hao, Y., Xu, J., Murray, T., & Thun, M.J. (2008). Cancer statistics, 2008. CA: A Cancer Journal for Clinicians, 58, 71–96. doi:10.3322/CA.2007.0010
Koroknay, V. (2015). Educating nurses in gerontology: We still have a way to go. Journal of Gerontological Nursing, 41, 3–4.
National Cancer Institute. (n.d.). Cancer stat fact sheets. Retrieved from http://seer.cancer.gov/statfacts
National Council of State Boards of Nursing. (2012). NCSBN model rules. Retrieved from http://bit.ly/1YgvCAf
Nurses Improving Care for Healthsystem Elders. (n.d.). Revised/updated GIAP offers higher reliability. Retrieved from http://bit.ly/1VOTRVn
Olson, E.A., & Young, R.F. (1992). Continuing education in geriatrics: An imperative for elderly care. Journal of Continuing Education in the Health Professions, 12, 25–32. doi:10.1002/chp.4750120106
Russell, K.A. (2012). Nurse practice acts guide and govern nursing practice. Journal of Nursing Regulation, 3, 36–42.
Smith, B.D., Smith, G.L., Hurria, A., Hortobagyi, G.N., & Buchholz, T.A. (2009). Future of cancer incidence in the United States: Burdens upon an aging, changing nation. Journal of Clinical Oncology, 27, 2758–2765. doi:10.1200/JCO.2008.20.8983
Tavares, J.P., & da Silva, A.L. (2013). Use of the Geriatric Institutional Assessment Profile: An integrative review. Research in Gerontological Nursing, 6, 209–220. doi:10.3928/19404921-20130304-01
About the Author(s)
Burhenn is a professional practice leader, Ferrell is a professor and director of the Division of Nursing Research and Education, Johnson is a chief nurse and patient care services officer, and Hurria is director of the Cancer and Aging Research Program, all at City of Hope in Duarte, CA. No financial relationships to disclose. All authors contributed to the conceptualization and design and manuscript preparation. Burhenn completed the data collection. All authors provided the statistical support and analysis. Burhenn can be reached at pburhenn@coh.org, with copy to editor at ONFEditor@ons.org. Submitted June 2015. Accepted for publication September 17, 2015.

