Prevalence of Smoking and Obesity Among U.S. Cancer Survivors: Estimates From the National Health Interview Survey, 2008–2012
Purpose/Objectives: To describe smoking and obesity prevalence among male and female cancer survivors in the United States.
Design: Cross-sectional survey.
Setting: Household interviews.
Sample: 9,753 survey respondents who reported ever having a malignancy, excluding nonmelanoma skin cancers.
Methods: Data from the National Health Interview Survey (2008–2012) were used to calculate weighted smoking status prevalence estimates. Cross-tabulations of smoking and weight status were produced, along with Wald chi-square tests and linear contrasts.
Main Research Variables: Cancer history, smoking status, obesity status, gender, age, and age at diagnosis.
Findings: Seventeen percent of cancer survivors reported current smoking. Female survivors had higher rates of current smoking than males, particularly in the youngest age category. Male survivors who currently smoked had lower obesity prevalence rates than males who previously smoked or never smoked. Among female survivors, 31% were obese and no significant differences were seen in obesity prevalence by smoking status for all ages combined.
Conclusions: The findings highlight the variation in smoking status and weight by age and gender. Smoking interventions may need to be targeted to address barriers specific to subgroups of cancer survivors.
Implications for Nursing: Nurses can be instrumental in ensuring that survivors receive comprehensive approaches to address both weight and tobacco use to avoid trading one risk for another.
Jump to a section
Among cancer survivors, smoking increases the risk of all-cause mortality, cancer-specific mortality, and secondary cancers related to smoking. Conversely, smoking cessation after a diagnosis improves cancer prognosis (U.S. Department of Health and Human Services, 2014). Population-based estimates of smoking prevalence among cancer survivors in the United States range from 9%–18% (Tseng, Lin, Martin, Chen, & Partridge, 2010; Underwood et al., 2012; Westmaas, Alcaraz, Berg, & Stein, 2014). Effective smoking cessation interventions exist for cancer survivors (de Moor, Elder, & Emmons, 2008), and research shows that many cancer survivors are motivated to quit after diagnosis (Berg, Carpenter, Jardin, & Ostroff, 2013; Hawkins et al., 2010). Leading organizations recommend tobacco use assessment and cessation support as part of cancer survivorship care planning (Hewitt & Ganz, 2007; Hewitt, Greenfield, & Stovall 2005; Toll, Brandon, Gritz, Warren, & Herbst, 2013). Despite motivation to quit and support from leading survivorship authorities, tobacco cessation can be extremely difficult for individuals to achieve. A study by Westmaas et al. (2015), which was guided by theories of health behavior, found evidence that long-term survivors were more likely to have quit smoking given greater perceived smoking risks and benefits to quitting and lower barriers to quitting.
To avoid potential increased risk of cancer recurrence and overall mortality, survivors are also advised to maintain their normal weight or to lose weight if they are overweight or obese (Hewitt & Ganz, 2007; Rock et al., 2012). Recommendations related to smoking and weight loss might be difficult to achieve in tandem because, although the mechanisms are not fully understood, smoking cessation is associated with weight gain (Aubin, Farley, Lycett, Lahmek, & Aveyard, 2012). Potential weight gain is consistently reported as a barrier to smoking cessation in the general population (Levine, Bush, Magnusson, Cheng, & Chen, 2013; Rosenthal et al., 2013). The authors are only aware of one study that estimates on the prevalence of obesity by smoking status in the survivor population, which did not stratify by age or gender (Tseng et al., 2010). Survivors might perceive smoking cessation and weight loss as conflicting goals, but this issue has not received much attention in the survivorship literature. The purpose of this study is to determine whether patterns of the distribution of obesity and smoking among cancer survivors differ by age and gender.
Methods
Data Source and Study Population
Data were obtained from the National Health Interview Survey (NHIS), an annual survey of a nationally representative sample of households conducted by the National Center for Health Statistics, Centers for Disease Control and Prevention (CDC) (Parsons et al., 2014). Five years of survey data (2008–2012) were included in this analysis. Data were collected from interviews with one randomly selected adult from each household. Key variables of interest included cancer history, smoking status, weight measures, age, gender, and age at first cancer diagnosis.
The adult response rates varied across survey years from 61%–66% (CDC, 2016). The authors defined survivors as individuals aged 18 years and older who reported having ever been told by a doctor or health professional that he or she had a malignancy of any kind. Respondents with only a diagnosis of nonmelanoma skin cancer were excluded (n = 2,721), resulting in the study sample size of 9,753.
Smoking Measures
Respondents were asked if they had ever smoked at least 100 cigarettes in their lifetime and if they currently smoked every day, some days, or no days. Individuals were classified as never smokers if they had not ever smoked at least 100 cigarettes. Past smokers were individuals who reported ever smoking at least 100 cigarettes, but no current smoking. Current smokers were individuals who reported smoking every day or some days. Individuals whose ever smoking status was unknown (n = 103), and individuals who reported ever smoking but whose current smoking status was not ascertained (n = 5), were excluded from comparisons between smokers and nonsmokers. Current smokers who reported smoking regularly at least one year before their diagnosis were considered to smoke prior to their diagnosis. For past smokers, the difference between years since first cancer diagnosis and reported time in years since quitting was calculated. If the difference was 0 or greater, it was assumed they smoked prior to their diagnosis.
Obesity Measures
Based on self-reported height and weight, body mass index (BMI) in kilograms per square meter was calculated. Respondents with a BMI of 30 or greater were classified as obese. The number of underweight individuals (BMI less than 18.5) (n = 224) was too small to support comparisons with other weight categories.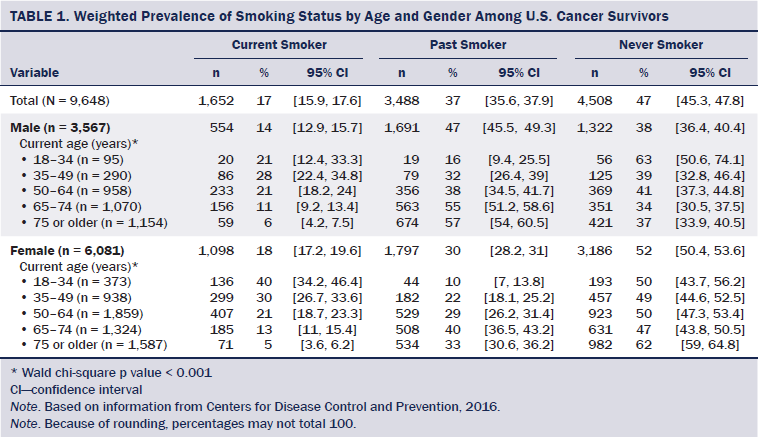
Demographic Characteristics
Demographic factors of interest included current age, gender, age at cancer diagnosis, and cancer type. Current age in years and age at first cancer diagnosis were uniquely assigned to five categories (see Table 1 and Figure 1). The reported most recent site of cancer was used to determine cancer type.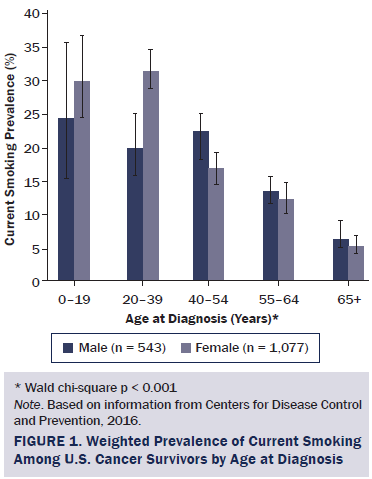
Statistical Analysis
SUDAAN, a statistical software package, was used to calculate all weighted prevalence estimates, including demographics, and to account for the complex sample design. Smoking status prevalence estimates were calculated for men and women, stratified by age and age at first cancer diagnosis. Cross-tabulations of smoking and weight status were produced for each gender by age. Respondents with unknown or missing responses were excluded from analyses (n = 105 for smoking status, n = 651 for obesity status, n = 190 for age of diagnosis, and n = 351 for cancer type). Wald chi-square tests were used to determine bivariate associations. Linear contrasts of differences between specific categories within variables were assessed using t tests.
Results
The study sample represented 14.4 million cancer survivors in the United States from 2008–2012. This population was equally split between those younger than age 65 years and those 65 years or older. A majority was female (60%) and non-Hispanic Caucasian (83%). Forty-eight percent were aged 55 years or older at the time of diagnosis, and 30% were obese.
Smoking Rates
Forty-seven percent of all survivors reported never smoking. Smoking status differed significantly by age and age at diagnosis among men and women (p < 0.001). Females had higher current smoking rates than males (p < 0.001). Younger female survivors (aged 18–34 years) were almost twice as likely to smoke as men of the same age (p = 0.002). Current smoking rates were highest at ages 18–34 years for women and ages 35–49 for men. Women diagnosed at ages 20–39 had higher smoking rates than their male counterparts (p < 0.001). Among those diagnosed at ages 40–54, men had higher smoking rates than women (p = 0.013).
Many of these gender differences appeared to be driven by cervical cancer survivors. When they were excluded from the analysis, significant gender differences in current smoking rates were no longer evident overall (14% in women), among those aged 18–34 years (23% in women), or among those diagnosed at ages 20–39 (24% in women). Among all survivors, 24% reported smoking immediately prior to their cancer diagnosis, and, of those, 11% quit within one year after their diagnosis. Men were more likely than women to quit within one year (14% versus 10%, p = 0.033).
Smoking and Obesity
Male survivors had an obesity prevalence of 28% (95% confidence interval [CI] [25.9, 29.4]) compared to 31% of female survivors (95% CI [29.6, 32.5]) (p = 0.005). Men who reported current smoking had lower overall rates of obesity (22%) than those who previously smoked (28.5%, p = 0.015) or never smoked (29.4%, p = 0.007). However, when stratified by age, this pattern held true only among men aged 35–49 (14% current versus 40% past, p = 0.004, and versus 45% never, p < 0.001) and 65–74 years (23% current versus 32% past, p = 0.031, and versus 35% never, p = 0.017) (see Figure 2).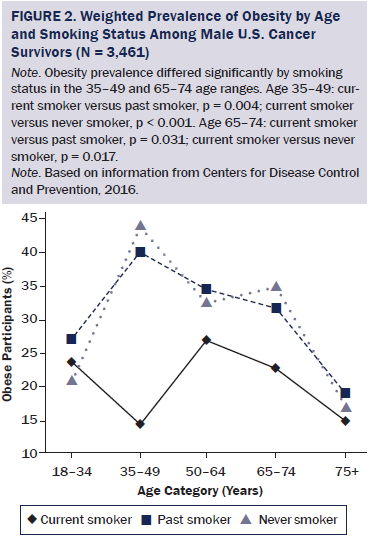
The overall prevalence of obesity among female survivors did not differ significantly by smoking status. Of women who reported current smoking, 30% were obese. When stratified by age, women 35–49 who currently smoked had significantly lower rates of obesity (27%) than those who previously smoked (36%, p = 0.006) and never smoked (37%, p < 0.001) (see Figure 3). Women aged 65–74 years who currently smoked had a significantly lower prevalence of obesity (26%) than those who previously smoked (37%, p = 0.016) or never smoked (32%, p = 0.031). For both men and women, no differences were noted in obesity prevalence by smoking status among the 18–34, 50–64, and 75 or older age groups.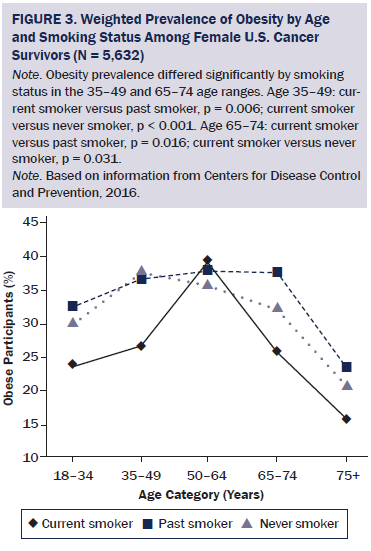
Discussion
This study provides population-based, gender-specific estimates of smoking status by age group and age at diagnosis among cancer survivors in the United States. Female survivors who were aged 18–34 and those who were diagnosed at age 20–39 had higher rates of current smoking than their male counterparts. The overall prevalence of obesity differed by gender and by smoking status in men, but not women. Among cancer survivors aged 35–49 and 65–74, current smokers had a lower prevalence of obesity than did previous or never smokers.
Smoking prevalence in this study was comparable to that in the general U.S. population (Agaku et al., 2014) and to estimates reported in the U.S. cancer survivor population (Tseng et al., 2010; Underwood et al., 2012). The smoking estimates in the current study were higher than the 9% reported in a study of U.S. cancer survivors from 2010–2011 (Westmaas et al., 2014). In older studies of cancer survivors using data from before 2007, current smoking prevalence estimates were as high as 23% (Bellizzi, Rowland, Jeffery, & McNeel, 2005; Mayer et al., 2007). The more recent data in the current study are consistent with research showing an overall decline in cigarette smoking in the general population, from 21% in 2005 to 18% in 2012 (Agaku et al., 2014). Specifically, among younger survivors, smoking prevalence was lower than past estimates (Bellizzi et al., 2005; Tseng et al., 2010).
The current study estimated that immediately prior to their cancer diagnosis, 24% of survivors reported smoking. A study by Westmaas et al. (2015) estimated that 31% of smokers quit two years after a cancer diagnosis, compared to estimates in the current study of 11% of survivors who quit within one year after diagnosis.
Data in the current study show that female survivors have a higher smoking prevalence than men, particularly among women who were younger (younger than 35 years) or had a diagnosis at 20–39 years. This gender difference was driven by a higher smoking prevalence among cervical cancer survivors. Cervical cancer is associated with smoking (U.S. Department of Health and Human Services, 2014) and has been shown to be more inaccurately reported compared to other cancers, possibly related to inaccurate reports of precancerous cervical lesions as cancer (Zajacova, Dowd, Schoeni, & Wallace, 2010).
Overall, a high prevalence of obesity was noted in both male and female survivors. These findings underscore the importance of addressing potential weight gain as a barrier to smoking cessation and supporting smoking cessation interventions along with weight management for survivors. Smoking cessation interventions are known to benefit from addressing barriers (Fiore et al., 2008) and have been shown to be more effective in women when weight gain issues or concerns are addressed (Torchalla et al., 2012). Prospective research is needed to determine when to deliver interventions and how to encourage maintenance of weight control among cancer survivors. Substantial weight gain in cancer survivors can adversely affect health and has been associated with increased risk of recurrence, as well as overall and breast cancer–specific mortality (McTiernan, Irwin, & Vongruenigen, 2010).
The CDC’s National Comprehensive Cancer Control Program (NCCCP) is uniquely positioned to help communities plan and implement evidence-based interventions to address smoking and weight control among cancer survivors (www.cdc.gov/cancer/ncccp/index.htm). NCCCP programs have successfully implemented initiatives to reduce risks, increase access to quality care, and improve quality of life for cancer survivors. Many NCCCP coalitions work with other partners to institutionalize the use of survivorship care plan standards. These plans provide descriptive follow-up instructions to address post-treatment care, including specific recommendations about diet, exercise, healthy weight, and smoking cessation. NCCCP coalitions can work with clinical and community partners to ensure survivors have access to medical homes and community programs to facilitate smoking cessation and weight management. Future efforts could be made to emphasize the pairing of weight management support whenever tobacco cessation support is recommended.
Limitations
The limitations of this study include the cross-sectional survey design of the NHIS. The findings relied on self-reported data, which might not accurately capture cancer prevalence and is likely to underestimate BMI (Klein, Lee, Moss, Trentham-Dietz, & Klein, 2010; Scribani et al., 2014). Data on BMI status over treatment time was not available, and, therefore, it was not possible to examine how treatment might have affected BMI. For respondents who had received more than one diagnosis, only the date of the first diagnosis was used as the time point in the analyses. Length of time since diagnosis was not examined and may have had an effect on some findings. For the calculation of smokers who smoked prior to and quit after their diagnosis, the authors did not have exact start and quit dates or diagnosis dates, only years. For those who quit less than two years after their first cancer diagnosis, the reason why they quit is unknown because the question was not asked in the NHIS. Because of limited sample sizes, analyses were primarily descriptive, and comparisons did not adjust for covariates.
Implications for Nursing
Nurses are in a unique position to facilitate comprehensive approaches to follow-up care through survivorship care plans. Oncology nurses and oncology nurse navigators should be aware of the significant prevalence of smoking and obesity in the survivorship population. Survivorship care plans that emphasize maintaining a healthy weight and not smoking can help survivors avoid trading one health risk for another. Nurses and patient navigators can consult individuals on perceived barriers to quitting, including concerns about weight gain. The authors’ data found that female cancer survivors who smoke had comparable rates of obesity to past and never smokers, suggesting that smoking status is not the only factor to influence high BMI. Healthcare providers should communicate the benefits of smoking cessation and weight management, such as improved survival, as supported by the low prevalence of smoking and obesity found in survivors aged 75 years or older. In addition, nurses can provide tobacco use assessment along with referrals to quit smoking help lines and cessation and weight management programs. Recommendations to survivors about physical activity could be beneficial as well, given the important role it plays in weight management.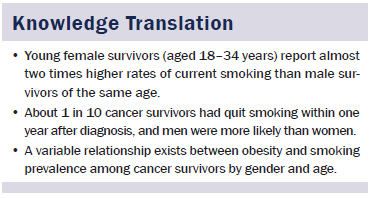
Conclusion
Cancer survivors in the United States are in need of tobacco use assessment and cessation support that incorporate weight management components in survivorship care plans. This study found a variable relationship between obesity and smoking prevalence among cancer survivors by gender and age. Interventions could be tailored for different groups of cancer survivors. Comprehensive approaches in survivorship care plans that address both weight and tobacco use could avoid trading one risk for another. In addition, smoking cessation interventions are particularly needed for young female survivors, given their high rates of current smoking.
The authors gratefully acknowledge Steve Leadbetter, MS, for his helpful statistical consultation on this analysis.
References
Agaku, I.T., King, B.A., Husten, C.G., Bunnell, R., Ambrose, B.K., Hu, S.S., . . . Day, H.R. (2014). Tobacco product use among adults—United States, 2012–2013. Morbidity and Mortality Weekly Report, 63, 542–547.
Aubin, H.J., Farley, A., Lycett, D., Lahmek, P., & Aveyard, P. (2012). Weight gain in smokers after quitting cigarettes: Meta-analysis. BMJ, 345, e4439. doi:10.1136/bmj.e4439
Bellizzi, K.M., Rowland, J.H., Jeffery, D.D., & McNeel, T. (2005). Health behaviors of cancer survivors: examining opportunities for cancer control intervention. Journal of Clinical Oncology, 23, 8884–8893. doi:10.1200/jco.2005.02.2343
Berg, C.J., Carpenter, M.J., Jardin, B., & Ostroff, J.S. (2013). Harm reduction and cessation efforts and interest in cessation resources among survivors of smoking-related cancers. Journal of Cancer Survivorship, 7, 44–54. doi:10.1007/s11764-012-0243-9
Centers for Disease Control and Prevention. (2016). National Health Interview Survey: Questionnaires, datasets, and related documentation 1997 to the present. Retrieved from http://www.cdc.gov/nchs/nhis/quest_data_related_1997_forward.htm
de Moor, J.S., Elder, K., & Emmons, K.M. (2008). Smoking prevention and cessation interventions for cancer survivors. Seminars in Oncology Nursing, 24, 180–192. doi:10.1016/j.soncn.2008.05.006
Fiore, M.C., Jaen, C.R., Baker, T.B., Bailey, W.C., Benowitz, N.L., & Curry, S.J. (2008). Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services.
Hawkins, N.A., Smith, T., Zhao, L., Rodriguez, J., Berkowitz, Z., & Stein, K.D. (2010). Health-related behavior change after cancer: Results of the American Cancer Society’s studies of cancer survivors (SCS). Journal of Cancer Survivorship, 4, 20–32. doi:10.1007/s11764-009-0104-3
Hewitt, M., & Ganz, P.A. (2007). Implementing cancer survivorship care planning. Washington, DC: National Academies Press.
Hewitt, M., Greenfield, S., & Stovall, E. (2005). From cancer patient to cancer survivor: Lost in transition. Washington, DC: National Academies Press.
Klein, B.E., Lee, K.E., Moss, S.E., Trentham-Dietz, A., & Klein, R. (2010). Self- and registry-reported cancer in a population-based longitudinal study. Wisconsin Medical Journal, 109, 261–266.
Levine, M.D., Bush, T., Magnusson, B., Cheng, Y., & Chen, X. (2013). Smoking-related weight concerns and obesity: Differences among normal weight, overweight, and obese smokers using a telephone tobacco quitline. Nicotine and Tobacco Research, 15, 1136–1140.
Mayer, D.K., Terrin, N.C., Menon, U., Kreps, G.L., McCance, K., Parsons, S.K., & Mooney, K.H. (2007). Health behaviors in cancer survivors. Oncology Nursing Forum, 34, 643–651.
McTiernan, A., Irwin, M., & Vongruenigen, V. (2010). Weight, physical activity, diet, and prognosis in breast and gynecologic cancers. Journal of Clinical Oncology, 28, 4074–4080.
Parsons, V.L., Moriarity, C., Jonas, K., Moore, T.F., Davis, K.E., & Tompkins, L. (2014). Design and estimation for the National Health Interview Survey, 2006–2015. Vital and Health Statistics, Series 2, 165, 1–53.
Rock, C.L., Doyle, C., Demark-Wahnefried, W., Meyerhardt, J., Courneya, K.S., Schwartz, A.L., . . . Gansler, T. (2012). Nutrition and physical activity guidelines for cancer survivors. CA: A Cancer Journal for Clinicians, 62, 242–274. doi:10.3322/caac.21142
Rosenthal, L., Carroll-Scott, A., Earnshaw, V.A., Sackey, N., O’Malley, S.S., Santilli, A., & Ickovics, J.R. (2013). Targeting cessation: Understanding barriers and motivations to quitting among urban adult daily tobacco smokers. Addictive Behaviors, 38, 1639–1642.
Scribani, M., Shelton, J., Chapel, D., Krupa, N., Wyckoff, L., & Jenkins, P. (2014). Comparison of bias resulting from two methods of self-reporting height and weight: A validation study. JRSM Open, 5(6), 2042533313514048. doi:10.1177/2042533313514048
Toll, B.A., Brandon, T.H., Gritz, E.R., Warren, G.W., & Herbst, R.S. (2013). Assessing tobacco use by cancer patients and facilitating cessation: An American Association for Cancer Research policy statement. Clinical Cancer Research, 19, 1941–1948.
Torchalla, I., Okoli, C.T., Bottorff, J.L., Qu, A., Poole, N., & Greaves, L. (2012). Smoking cessation programs targeted to women: A systematic review. Women and Health, 52, 32–54.
Tseng, T.S., Lin, H.Y., Martin, M.Y., Chen, T., & Partridge, E.E. (2010). Disparities in smoking and cessation status among cancer survivors and non-cancer individuals. Journal of Cancer Survivorship, 4, 313–321. doi:10.1007/s11764-010-0127-9
Underwood, J.M., Townsend, J.S., Stewart, S.L., Buchannan, N., Ekwueme, D.U., Hawkins, N.A., . . . Fairley, T.L. (2012). Surveillance of demographic characteristics and health behaviors among adult cancer survivors—Behavioral Risk Factor Surveillance System, United States, 2009. Morbidity and Mortality Weekly Report, 61(SS01), 1–23.
U.S. Department of Health and Human Services. (2014). The health consequences of smoking—50 years of progress: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
Westmaas, J.L., Alcaraz, K.I., Berg, C.J., & Stein, K.D. (2014). Prevalence and correlates of smoking and cessation-related behavior among survivors of ten cancers: Findings from a nationwide survey nine years after diagnosis. Cancer Epidemiology, Biomarkers and Prevention, 23, 1783–1792.
Westmaas, J.L., Newton, C.C., Stevens, V.L., Flanders, W.D., Gapstur, S.M., & Jacobs, E.J. (2015). Does a recent cancer diagnosis predict smoking cessation? An analysis from a large prospective US cohort. Journal of Clinical Oncology, 33, 1647–1652.
Zajacova, A., Dowd, J.B., Schoeni, R.F., & Wallace, R.B. (2010). Consistency and precision of cancer reporting in a multiwave national panel survey. Population Health Metrics, 8, 20.
About the Author(s)
Shoemaker is a research fellow, White is chief of the Epidemiology and Applied Research Branch, Hawkins is a behavioral scientist, and Hayes is chief of the Comprehensive Cancer Control Branch, all in the Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion, at the Centers for Disease Control and Prevention in Atlanta, GA. This research was funded, in part, by an appointment (Shoemaker) to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the Centers for Disease Control and Prevention. The National Health Interview Survey and preparation of the manuscript were entirely funded by the U.S. government. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Shoemaker and White contributed to the conceptualization, design, and analysis. All authors contributed to the manuscript preparation. Shoemaker can be reached at xhr1@cdc.gov, with copy to editor at ONFEditor@ons.org. Submitted July 2015. Accepted for publication September 8, 2015.

