Perceived Benefits and Barriers of Cervical Cancer Screening Among Chinese American Women
Purpose/Objectives: To explore the perceived benefits and barriers to cervical cancer screening among Chinese American women using stages of the Transtheoretical Model of Change.
Design: Cross-sectional design with self-report surveys.
Setting: Chinese communities (e.g., churches, supermarkets, restaurants) in Northern California and Northern Nevada.
Sample: 121 Chinese women aged 21–65 years living in Northern California and Northern Nevada.
Methods: A snowball sampling technique using personal contacts was used.
Main Research Variables: Stages of change and perceived benefits and barriers to cervical cancer screening.
Findings: Participants in the action/maintenance stage were most likely to believe that cervical cancer was treatable if caught early. Women in the contemplation/preparation stage were more likely to state that they worried about or feared screening, that it was too expensive, and that they would want to use Chinese medicine to cure an illness before trying Western medicine. Women in the precontemplation/relapse stage were most likely to report that they did not know where to get screened and that their partner would not want them to be screened.
Conclusions: Perceived benefits and barriers to screening were differentially associated with the stages of change. Results may support culturally sensitive and theory-based programs to improve screening rates among Chinese American women.
Implications for Nursing: The results suggest the importance of cultural sensitivity among nursing providers when working with Chinese Americans to provide more relevant, holistic care.
Jump to a section
Cervical cancer is the world’s second most common cancer among women in less developed regions, with an estimated 445,000 new cases in 2012 (World Health Organization, 2016). Cervical cancer was once a leading cause of death among American women in the United States; currently, it ranks 14th in the causes of female cancer mortality (National Institutes of Health [NIH], 2010). The rates of cervical cancer have greatly decreased in the United States since the introduction of Papanicolaou (Pap) screening in the 1950s, which identifies abnormal cells prior to the development of cervical cancer (NIH, 2010).
Despite the recognized benefits of regular Pap screening, Asian American women aged 18 years and older have the lowest Pap smear screening rate (68%) among U.S. racial and ethnic groups (compared to African Americans [78%], Hispanics [74%], non-Hispanic Caucasians [73%], and American Indians/Alaska Natives [73%]) (Centers for Disease Control and Prevention [CDC], 2016b). According to the 2010 Census, the Chinese American population grew 40% from 2000 to 2010 and comprised the largest Asian American population in the United States (U.S. Census Bureau, 2012). Despite the increased number of Chinese Americans, national data on cervical cancer specific to Chinese American women are scarce. One early study completed in 1999 of 432 Chinese American women aged 20 years and older who resided in Seattle revealed that 81% had received a Pap screening (Taylor et al., 2002). Similarly, another study of 100 Chinese American women aged 40 years or older in Portland reported that 84% had received a Pap screening (Lee-Lin et al., 2007). Three other studies of Chinese American women aged 18 years or 50 years and older in the eastern region of the United States (N = 96, 473, and 507, respectively) showed that 15% had never received a Pap screening (Robison et al., 2014; Strong & Liang, 2009), 76% had never had a Pap screening (Robison et al., 2014), and only 45%–50% currently received regular Pap screenings (Ji, Chen, Sun, & Liang, 2010; Strong & Liang, 2009). Another study found that Pap screening rates did not significantly change over time among Chinese American women aged 21 years and older in California, and about 75% reported adherence to recommendations for cervical screening (Chawla, Breen, Liu, Lee, & Kagawa-Singer, 2015). These studies indicate that screening rates for cervical cancer have not improved since 1999 (Chawla et al., 2015; Ji et al., 2010; Lee-Lin et al., 2007; Robison et al., 2014; Strong & Liang, 2009; Taylor et al., 2002). In addition, the data reported on Chinese American women who had received a Pap screening were below the Healthy People 2020 national objective of at least 93% of women aged 21–65 years receiving a Pap screening (Office of Disease Prevention and Health Promotion, 2015).
The few studies that have examined the factors associated with Pap screening among Chinese American women have reported that demographic characteristics (e.g., age, marital status, education levels, insurance) and other factors, such as perceived benefits and barriers, have been related to screening behavior (Ji et al., 2010; Lee-Lin et al., 2007; Ma et al., 2009, 2013; Strong & Liang, 2009; Taylor et al., 2002). Although some barriers to cancer screening are common across cultural groups (e.g., health insurance, health literacy, fear, pain, embarrassment), other factors are unique to certain groups. For example, gender and language concordance (Thompson et al., 2014; Zhang, Rose, Foster, Pullon, & Lawton, 2014), provider understanding of different cultural conceptions or perceptions of health and illness (Zhang et al., 2014), and trust (Wong et al., 2013) have been reported to be barriers to screening among Chinese and Asian American populations. Chinese American women have also reported barriers of fatalistic views of cancer and fear (Gor, Chilton, Camingue, & Hajeck, 2010; Ji et al., 2010; Strong & Liang, 2009; Taylor et al., 2002). Little research has been conducted on specific perceived benefits of cervical cancer screening among Chinese American women.
The purpose of this study was to discover differences in Chinese American women’s perceived benefits of and barriers to obtaining Pap screening by using the Transtheoretical Model (TTM) of Change as a conceptual framework. The TTM (Prochaska, Redding, & Evers, 2015) hypothesizes that people progress through a series of stages of readiness toward changing a behavior. These stages are (a) precontemplation, not intending to take action within the next six months; (b) contemplation, intending to take action within the next six months; (c) preparation, intending to take action in the next 30 days; (d) action, change in the past six months; and (e) maintenance, behavior change for six months or more. Relapsers are those who have not maintained the behavior change over time and may or may not be contemplating taking action again. According to this model, people in later stages (i.e., the action and maintenance stages) of the TTM demonstrate higher levels of perceived benefits and fewer barriers than people in earlier stages (i.e., the precontemplation and contemplation stages).
The TTM highlights the importance of designing stage-based interventions to help people move through the stages. Interventions incorporating the TTM components have demonstrated effectiveness in promoting Pap screening among Latina women living in Texas and Washington (Byrd, Wilson, Smith, Coronado, et al., 2012; Byrd, Wilson, Smith, Heckert, et al., 2012). Only a limited number of descriptive studies have used TTM as a framework for assessing an individual’s readiness of change for cervical screening among Chinese Americans (Strong & Liang, 2009). The study results may provide strategies for designing evidence-based and culturally sensitive programs that focus on specific benefits of and barriers to Pap screening among Chinese American women.
Methods
Approval for the study was obtained from the University of Nevada’s Institutional Review Board. A snowball sampling technique using personal contacts (e.g., face-to-face interaction, emails, telephone calls), which has proven to be highly successful in collecting data from immigrant groups, was used to recruit Chinese American women (Hasnain, Menon, Ferrans, & Szalacha, 2014). The Chinese authors of the current study recruited the first group of study participants individually, face-to-face, from Chinese communities(e.g., churches, supermarkets, restaurants) in Northern California and Northern Nevada in March 2015. After verbal informed consent was obtained, participants were asked to complete an anonymous self-report survey and return it to the recruiting investigator immediately or within two weeks in a prepaid, preaddressed envelope. The investigator also asked the women to contact friends and family members who met inclusion criteria to fill out surveys. Study packets, including study information, Chinese and English translations of the questionnaire, and a prepaid and preaddressed envelope, were provided for recruiting study participants. Prior to collecting data about cervical cancer screening behaviors, the investigators or data collectors explained the current cervical screening guidelines to the women.
According to the cervical cancer guidelines from the American Cancer Society (ACS) (2014) and the CDC (2016c), women aged 21–65 years should receive a Pap screening every three years, and women aged 30–65 years should receive a combination of Pap screening and human papillomavirus testing every five years. The U.S. Preventive Services Task Force (2012) recommends against screening for cervical cancer in women aged older than 65 years who have had adequate prior screening and are not otherwise at high risk for cervical cancer. Eligibility criteria for this study included women aged 21–65 years who self-identifiedas Chinese American and were able to read English, simplified Chinese, or traditional Chinese. Women with total hysterectomies were excluded because Pap screening is not recommended in women who have had hysterectomies for noncancerous conditions (e.g., fibroids) (ACS, 2014; CDC, 2016c).
Instruments
Participants had the option of responding to the questionnaire in English, simplified Chinese, or traditional Chinese. All participants chose to complete the survey in simplified or traditional Chinese. The survey instrument included three sections, a demographic section, a Cervical Cancer Screening Stage Questionnaire (CCSSQ), and a Benefits/Barriers Scale (BBS). Demographic questions assessed age, marital status, education, employment status, and health insurance coverage. The average time reported to complete the questionnaire was 10–15 minutes.
Cervical Cancer Screening Stage Questionnaire: The CCSSQ, including a four-item algorithm incorporating the time descriptors from the TTM (Prochaska et al., 2015), was used to assess participants’ stages of change related to Pap screening use. First, participants were asked if they received Pap screenings on a regular basis, and were provided with the definition and different response options. Those who obtained regular Pap screenings were asked if they planned to continue receiving them on a regular schedule. Respondents who had received one or more Pap screenings but not on a regular basis were asked when they had received their last screening and whether they planned to continue having screenings on a regular schedule. Respondents who had never received a Pap screening were asked if they were considering having one, and responded either (a) yes, in the next month; (b) yes, in the next six months; (c) no; or (d) other (please specify). Based on the TTM stages of change and the current screening guidelines, respondents’ answers were classified into one of the following stages: (a) precontemplation, (b) contemplation, (c) preparation, (d) action, (e) maintenance, (f) relapse with intention to continue screening, or (g) relapse without intention to continue screening.
Benefits/Barriers Scale: This scale consists of a 3-item benefits subscale and a 12-item barriers subcale, adapted from Byrd, Peterson, Chavez, and Heckert (2004), which evaluates women’s perceptions of the benefits and barriers to receiving Pap screenings. The original BBS scale developed by Byrd et al. (2004) consisted of nine questions measuring barriers. The authors of the current study added three items related to traditional Chinese medicine to the scale to assess the potential barriers preventing women’s participation in cervical screening. Each item was scored on a four-point Likert-type scale from 1 (strongly disagree) to 4 (strongly agree), with higher scores indicating greater levels of beliefs in each subscale. In the current study, Cronbach alpha coefficients were computed to test internal consistency reliability of the Chinese version of the BBS and indicated reliable alphas of 0.81 and 0.8.
Translation Process
A committee fluent in Chinese and English translated the CCSSQ and BBS into simplified and traditional Chinese, and two bilingual and bicultural individuals back translated the Chinese instruments into English. Three professional experts in women’s health, instrument development, and health behavior reviewed the linguistic appropriateness and clarity of the Chinese version of the CCSSQ and BBS to ensure face validity. Prior to the initiation of data collection, the translated CCSSQ and BBS were pilot tested in seven Chinese women who did not participate in the main study. Minor amendments were made to make questions more easily understood.
Statistical Analyses
Summary statistics were used to characterize demographic variables and perceived benefits and barriers scores. Multiple linear regression models were applied to compare individual values of perceived benefits and barriers among TTM stages, after controlling for confounding variables, including age and education. Post hoc multiple comparisons were applied to detect the differences between specific pairs of changes in individual levels of perceived benefits and barriers. Level of significance was set at p ≤ 0.05. The level of significance for multiple comparisons was adjusted by Bonferroni correction. SAS®, version 9.3, was used for data management and analysis. 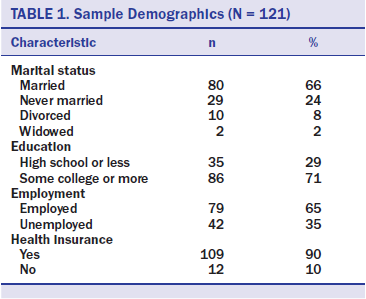
Results
The sample size for this survey was 121, and the average age of the sample was 44.8 years (SD = 11.9, range =21–65 years). As shown in Table 1, the majority of the women were married, had some college education or higher, were employed, and had health insurance.
Distribution of Participants
Most participants were categorized in the maintenance stage (n = 67), followed by the relapse without intention to continue screening (n = 19), precontemplation (n = 12), action (n = 12), contemplation (n = 10), and preparation stages (n = 1). None were classified in the relapse with intention to continue screening stage. Because of the low number of participants in the relapse without intention to continue screening, precontemplation, contemplation, preparation, and action stages, the authors condensed the TTM stages into a three-stage structure based on the women’s behaviors and intentions to obtain a Pap screening, including:
• Precontemplation/relapse without intention (N = 31): Women who had Pap screenings in the past or never had a Pap screening and did not intend to have one within the next six months
• Contemplation/preparation (N = 11): Women who had never received a Pap screening but intended to have one within the next six months
• Action/maintenance (N = 79): Women who had one Pap screening in the past year or who had regular Pap screenings and intended to continue to do so
Difference in Perceived Benefits and Barriers
As presented in Table 2, after controlling for potential confounding variables (age, education), multiple linear regressions and multiple comparisons with Bonferroni correction revealed that participants in the action/maintenance stage reported significantly higher scores than those in contemplation/preparation stage in the perceived benefits item: If cervical changes are found early, they are treatable (mean = 3.35, SD = 0.48 versus mean = 2.9, SD = 0.3, p = 0.0092). For perceived barriers, women in the contemplation/preparationstage exhibited significantly higher scores than those in the action/maintenance stage in the following items: (a) Getting a Pap screening would only make me worry (mean = 2.63, SD = 0.5 versus mean = 2.03, SD = 0.58, p = 0.0063); (b) It is too expensive to have a Pap screening (mean = 2.63, SD = 0.5 versus mean = 2.06, SD = 0.4, p = 0.0031); (c) I will experience fear of the results if I have a Pap screening (mean = 2.72, SD = 0.64 versus mean =2.07, SD = 0.47, p = 0.0041); and (d) I would choose traditional Chinese medicine to cure an illness before trying Western medicine (mean = 2.9, SD = 0.7 versus mean = 2.25, SD = 0.49, p = 0.0004).
In addition, respondents in the precontemplation/relapse without intention stage showed significantly higher scores than those in the action/maintenance stage in the following items: (a) I do not know where I could go if I wanted a Pap screening (mean = 2.54, SD = 0.62 versus mean = 1.96, SD = 0.43, p < 0.0001) and (b) My partner (boyfriend/husband) would not want me to have a Pap screening (mean = 2.06, SD = 0.51 versus mean = 1.79, SD = 0.43, p = 0.0008).
Discussion
The authors of the current study investigated the perceived benefits and barriers to cervical cancer screening among Chinese American women with the TTM stages of change. Significant associations existed between TTM stages and one perceived benefit theme and six barrier items. Respondents in the TTM contemplation/preparation stage were less likely to endorse cervical cancer as treatable if found early through screening than women in the action/maintenancestage. This finding suggests that, even among those with intentions to change, participants may be unaware of the benefits of screening and early detection. Culturally sensitive and linguistically appropriate educationprograms designed for improving knowledge of cervical cancer and awareness of early detection practices (Chawla et al., 2015; Fang, Ma, & Tan, 2011; Gor et al., 2010; Ji et al., 2010) may move these participants into the action/maintenance stage.
Six perceived barrier items were significantly associated with the TTM stages of change: (a) feelings of worry about getting a Pap screening, (b) perceptions of Pap screening being too expensive, (c) not knowing where to go for a Pap screening, (d) partners’ negative attitudes toward screening, (e) fear of screening results, and (f) preferences for traditional Chinese medicine over Western medicine. More specifically, compared to women in the action/maintenance stage, women in the contemplation/preparation stage perceived more barriers to obtaining Pap screenings, particularly in relation to worry about getting a Pap screening, that screening would be too expensive, that they would get bad results, and that they would rather try traditional Chinese medicine before Western medicine. Intervention efforts should address these perceptions to decrease the barriers and move participants into the action/maintenance stage. 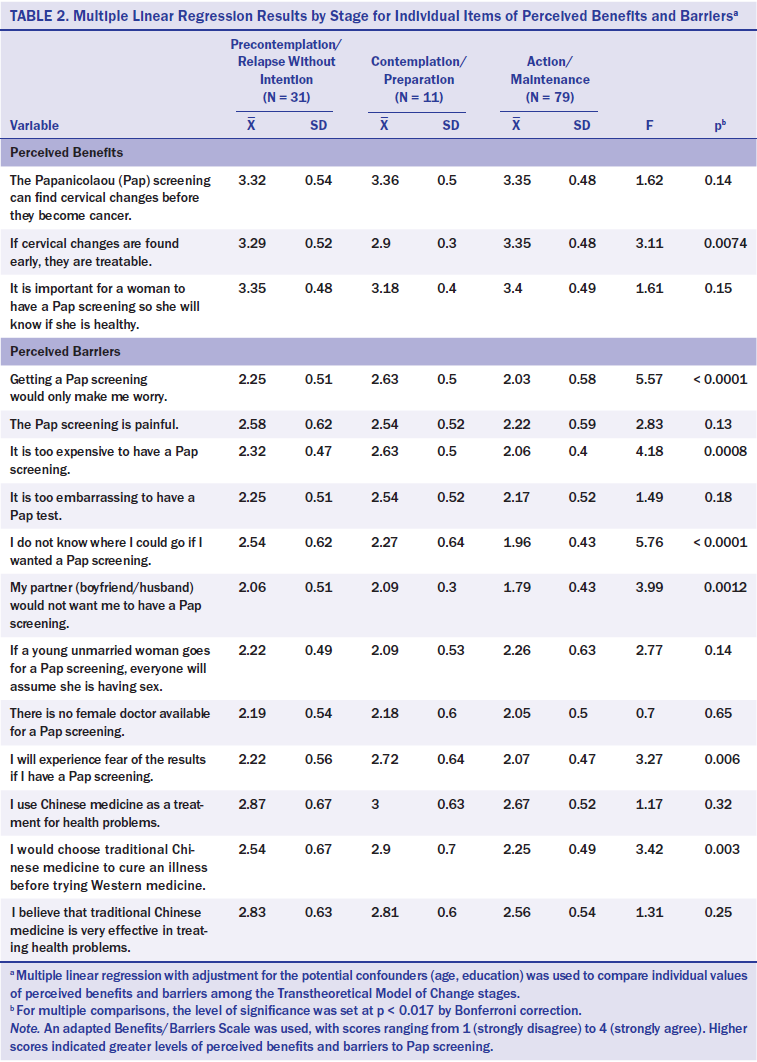
These results are consistent with previous studies that have indicated that Chinese American women were less likely to undergo Pap screenings because of fatalistic views of cancer and fear (Gor et al., 2010; Ji et al., 2010; Strong & Liang, 2009; Taylor et al., 2002). Strategies for overcoming these concerns include identifying women’s fears and worries and educating them about the Pap screening procedure to reduce anxiety associated with the test. In addition, concerns about the cost of Pap screenings in the current study were similar to concerns among Chinese American women in other studies who lacked health insurance coverage and/or were of low-income status (Chawla et al., 2015; Lee-Lin et al., 2007; Ma et al., 2009, 2013; Strong & Liang, 2009; Taylor et al., 2002). Although 90% of participants in the current study had health insurance, they still reported concerns about the costs of testing. Women may or may not be aware that their insurance plans cover Pap screenings, or they may have concerns about possible deductible or copay costs. Deeply rooted in Chinese culture, some Chinese women may rather save money for supporting their family rather than pay for their own health care out of pocket. A number of assistance programs provide free or low-cost cervical cancer screenings (e.g., National Breast and Cervical Cancer Early Detection Program) (CDC, 2016a), but Chinese American women may be unaware of these services or face other complications, such as language barriers and difficulty navigating complex healthcare systems.
In addition, Chinese American women may prefer Chinese medicine over Western medicine because it is affordable and culturally appropriate, or because they lack trust in Western medicine (Chang, Woo, Yau, Gorzalka, & Brotto, 2013). One study indicated that Chinese American women with more traditional Chinese cultural views of healthcare practices were less likely to adhere to cervical cancer screening guidelines (Ji et al., 2010). Chinese healthcare providers can be valuable and culturally appropriate resources for Chinese American women, providing navigation assistance on cervical screening. Western medical providers should establish collaborative relationships with traditional practitioners. Other barriers that have been cited in the literature but have not been deemed significant in the current study include embarrassment and pain associated with Pap screenings (Gor et al., 2010; Taylor et al., 2002). Continued research on the potential barriers and cultural factors associated with Pap screening is needed.
Women in the precontemplation/relapse without intention stage perceived more barriers to getting a Pap screening related to concerns of where to have a Pap screening and lack of support from their partner. One study of Asian American populations documented that male partners may pose barriers to cervical screening (Gor et al., 2010). In traditional Chinese culture, men make most decisions, so some Chinese women may need to obtain permission from their husbands or partners to seek gynecologic care. As Pap screening behaviors among Chinese American women are influenced by spouses and significant others, intervention strategies should be developed to inform spouses and significant others of the importance of adhering to regular Pap screenings. Because participants in precontemplation do not think about getting a Pap screening and participants in relapse fail to maintain routine Pap screenings, culturally appropriate interventions may help women overcome the barriers to maintaining routine Pap screenings and progress to later TTM stages.
Limitations
Although the questionnaire was offered in English and Chinese, all participants completed the survey in Chinese. Therefore, the results may differ from the screening behaviors of English-speaking Chinese American women. The small sample of Chinese American respondents were recruited mainly from Northern California and Northern Nevada through a snowball sampling method, limiting the generalizability of the results. Future research with a larger and more diverse random sample (geographically and linguistically) may provide a more representative pattern of Chinese American women’s screening behaviors.
Second, the study did not include measures of birth country, age at immigration, length of time living in the United States, generation, proficiency in English and/or other languages, or risk factors for cervical cancer (e.g., multiple full-term pregnancies, intrauterine device use, being overweight) (ACS, 2016), which may play important roles in Chinese American screening behaviors. Future work could benefit from the inclusion of these variables.
Third, current cervical screening guidelines were provided verbally to the participants, and information was self-reported. Participants’ understanding or compliance with guidelines cannot be determined with certainty. Future study designs could incorporate medical record data to improve accuracy.
Fourth, only three items assessed participants’ perceived benefits of obtaining a Pap screening. The instrument may need to be further developed by adding culturally relevant questions (e.g., Pap screening can detect cervical cancer early so I can take care of my family) to provide more comprehensive and culturally appropriate measures of Chinese women’s perceived benefits of cervical cancer screening.
Last, the current study used a quantitative research methodology that limited the authors’ ability to understand the depth or benefits of the results. A mixed-method design is recommended to explore the complex issues related to cervical screening behaviors.
Implications for Nursing
The specific perceived benefits of and barriers to Pap screening identified in the current study may be useful in developing culture-specific interventions for Chinese American women to increase their screening behaviors. Culturally sensitive and linguistically appropriate interventions should focus on partners and family members as well as women in the precontemplation/relapse without intention stage and the contemplation/preparation stage. Providing information about the procedure, benefits, availability, and affordability of Pap screenings may also be beneficial. The results also suggest the significance of cultural sensitivity among nursing providers when working with Chinese Americans to provide more relevant, holistic care.
Study participants in the earlier TTM stages perceived fewer benefits and more barriers than those in the later TTM stages, consistent with prior TTM research on Pap screenings, emphasizing that the progression of stages is based on an increase in the perception of benefits and decrease in the perceptions of barriers to participating in Pap screening (Strong & Liang, 2009). More TTM studies using theory-based interventions are needed to improve adherence to cervical cancer screening guidelines among Chinese American women. 
Finally, policy changes could support increased screening. For example, policies to increase health literacy and availability of interpreters could enhance women’s understanding and willingness to be screened. Efforts to increase nursing providers’ cultural sensitivity and understanding of Chinese conceptions of health and illness through training or continuing education may enhance trust and communication as well. Although Pap screenings are covered by most insurance plans with no out-of-pocket costs, policymakers should assess out-of-packet expenses for Chinese Americans without medical insurance. Availability of free and low-cost cervical screening services could help address access issues for underinsured or uninsured people.
Conclusion
Addressing Chinese American women’s perceived benefits and barriers to Pap screening is critical in helping them progress through the TTM stages of change and participate in regular Pap screening. The current study also provided guidance to healthcare professionals in the development of effective theory-based programs to improve screening rates among Chinese American women and highlighted the importance of cultural beliefs in cancer screening decision making.
About the Author(s)
Tung is an associate professor in the Orvis School of Nursing and Lu and Granner are associate professors in the School of Community Health Sciences, all at the University of Nevada in Reno. No financial relationships to disclose. Tung contributed to the conceptualization and design, provided statistical support and analysis, and completed the data collection. Lu contributed to the data analysis and results. All of the authors contributed to the manuscript preparation. Tung can be reached at wctung@hotmail.com, with copy to editor at ONFEditor@ons.org. Submitted April 2016. Accepted for publication June 4, 2016.




