Implementation and Use of a Patient Symptom Diary During Chemotherapy: A Mixed-Methods Evaluation of the Nurse Perspective
Purpose/Objectives: To gain a deeper understanding of nurses’ experience working with a patient diary for tracking and treating side effects during chemotherapy.
Design: A mixed-methods design was used to learn about oncology nurses’ use and perceptions of a symptom diary.
Setting: Six oncology wards and two outpatient clinics at the University Hospitals Leuven, Belgium.
Sample: 79 nurses completed a survey, and 14 nurses participated in focus group discussions.
Methods: First, a survey sampled nurses’ use and perceptions of the diary. Next, focus group discussions were held with the aim of arriving at a deeper understanding of the survey results.
Main Research Variables: Use and perceptions of a symptom diary.
Findings: Most nurses reported performing diary-related behavior to some extent. The survey and focus groups indicated that many nurses strongly believed in the value of the diary, but some were still hesitant or had concerns about patients’ perceptions of the diary. The focus group results showed that nurses’ use of the diary in daily practice was influenced by their personal beliefs about the value of the diary, the team’s, and those of their patients.
Conclusions: Although a positive trend was noted, nurses’ use of the symptom diary was suboptimal six months after its implementation.
Implications for Nursing: This study highlights important issues that need to be addressed to advance the successful implementation of the symptom diary.
Jump to a section
Supportive care for patients with cancer is suboptimal (Henry et al., 2008; Johnsen, Petersen, Pedersen, Houmann, & Groenvold, 2013). Several barriers at the professional level (e.g., lack of time, focus on treatment) and at the patient level (e.g., misconceptions that symptoms are incurable, beliefs that good patients do not complain) impede adequate symptom detection and, ultimately, impair symptom management (Jakobsson, Ekman, & Ahlberg, 2008; Passik et al., 2002; Patrick et al., 2004; Sun et al., 2007, 2012).
To prevent professionals from overlooking or minimizing symptoms, the use of patient-reported outcomes (PROs) is being promoted (Atkinson et al., 2016; Judson et al., 2013). Evidence shows that routine attention to PROs improves quality of care, patient–clinician communication, and symptom management (Detmar, Muller, Schornagel, Wever, & Aaronson, 2002; Howell et al., 2015; Judson et al., 2013; Ruland et al., 2010; Velikova et al., 2004). In addition, using PROs in routine clinical practice has shown potential for reducing symptom burden (Judson et al., 2013; Ruland et al., 2010; Velikova et al., 2004). More frequent and better discussions about symptoms between patients and clinicians, together with intensified and improved symptom management in response to patient reports, are central mechanisms that can explain these clinical benefits (Basch et al., 2016). In addition to these positive effects on professional care, diaries contribute to patients’ self-management. Self-monitoring helps patients understand how their symptoms evolve and respond to medication or self-management strategies and helps them choose or continue appropriate actions (Lorig & Holman, 2003; Richard & Shea, 2011).
Several studies of the outcomes of a self-report instrument found that only in a minority of cases were the diary contents discussed with healthcare professionals (Hoekstra, de Vos, van Duijn, Schadé, & Bindels, 2006; Mills, Murray, Johnston, & Donnelly, 2008). Poor implementation of the interventions may explain the negative results in these studies (Blackwood, 2006; Hoekstra et al., 2006; Howell et al., 2015; Locklear et al., n.d.; Mills et al., 2008). Most importantly, these observations point to the need for research on the experiences of intervention receivers and providers. Insight into the users’ perceptions of the patient diary can contribute to the selection of adequate implementation strategies (Bartholomew, Parcel, Kok, Gottlieb, & Fernandez, 2011).
Concerns about time constraints, lack of training on how to use and respond to PROs, and doubts about their value and benefit have been raised as clinician-related barriers to the routine use of PROs (Howell et al., 2015; Kanatas, Mehanna, Lowe, & Rogers, 2009; Locklear et al., n.d.; Snyder, Jensen, Geller, Carducci, & Wu, 2010). Most of these studies included physicians, and only a few studies have evaluated the nursing perspective. Nurses seem concerned about the workload associated with these tools (Maguire, McCann, Miller, & Kearney, 2008; Miller, Taylor, Wells, et al., 2007). They also report feeling that such interventions can be valuable but a burden to patients (Kearney et al., 2006; Maguire et al., 2008). In a study by Cornbleet, Campbell, Murray, Stevenson, and Bond (2002), nurses and doctors believed the patient-held record to be more useful and relevant to patients than to healthcare professionals.
The aim of the current study was to arrive at a better understanding of nurses’ experiences with a paper patient diary for tracking symptoms during chemotherapy. The authors were interested in how nurses actually use the diary and in identifying key elements that facilitate or hinder nurses’ adoption of the diary in everyday clinical practice.
Methods
The study took place at six oncology wards and two outpatient clinics at the University Hospitals Leuven in Belgium. These wards represented the five medical departments prescribing chemotherapy: hematology, digestive oncology, respiratory oncology, gynecologic oncology, and general medical oncology. Therefore, the entire patient population being treated with chemotherapy at the hospital was represented, with the exception of pediatric patients. The study was approved by the Research Ethics Board of the Catholic University Hospitals.
Symptom Diary
The symptom diary in the current study is a paper tool that allows patients to self-report their chemo-therapy side effects at home on a daily basis. The diary formally tracks and grades 14 chemotherapy-related symptoms: nausea, vomiting, loss of appetite or taste changes, soreness of the mouth, diarrhea, constipation, fatigue, pain, rash, mental burden, fever/temperature, numbness of paresthesia in fingers or toes, tearing eyes, and hearing loss. It provides a blank space to describe other symptoms. The patient grades each symptom on a color-coded, four-level scale. Patients mark the grade they experience. The symptom grades in the diary are Dutch lay translations of the Common Toxicity Criteria for Adverse Events, version 4.0, except for mental burden, for which custom grades were developed in collaboration with three psychologists. The diary uses colors matching the severity of the symptoms: green for grade 0 (absent), yellow for grade 1, orange for grade 2, and red for grade 3 (most severe). The original English diary is available at www.uzleuven.be/sites/default/files/brochures/chemotherapy_diary_sympto….
The symptom diary is intended for patients treated with IV chemotherapy. At every new treatment cycle, patients were offered a symptom diary. Discussion of the diary contents at follow-up hospital visits allowed healthcare professionals to provide symptom management support. In the study hospital, oncology nurses discuss the diary contents with the patient and summarize the diary information in the electronic patient file. Doctors look at the “raw” paper diary or at the nurses’ summary report.
The diary was developed by two advanced nurse practitioners in oncology, in collaboration with a panel of oncologists and oncology nurses. Next, the diary was pilot tested and optimized in a group of patients with breast or lung cancer. After discussion with the head nurses and medical staff, lunch meetings were organized to introduce the diary to oncology nurses from eight wards. At the same time, the authors introduced a module to report on patients’ symptom burden at home (as discussed using the diary or asking questions) in the electronic patient file. After these lunch meetings, head nurses were encouraged to discuss local agreements for the implementation and use of the diary with their nursing teams. During the next few months, the advanced nurse practitioner closely monitored the diary use and nurse reactions, provided regular feedback on observed bottlenecks or positive examples via the head nurses, or participated in meetings in the wards. Posters summarizing the diary’s added value or evidence were displayed in the nursing wards. The nursing and patient evaluations were the next step to monitor the adoption and to plan necessary actions in response.
Survey of Nurses’ Experiences
A quantitative evaluation (in the form of a survey) took place about six months after diary initiation. This custom survey, constructed in-house, gathered information on the nurses’ use of the symptoms reported in the diary, as well as their opinions and perceptions of the diary. The survey content was informed by relevant themes in feasibility studies on symptom detection and management interventions (Kearney et al., 2006; Maguire et al., 2008; Miller, Taylor, Wells, et al., 2007), as well as nurses’ behavior and attitude toward the diary, as observed during the first months of diary use. The authors also included some items on symptom management to elicit nurses’ views on how the symptom diary fits into supportive cancer care. The multidisciplinary taskforce behind the development and implementation of the diary commented on the proposed content of the survey. Next, to improve the face validity of the survey, a pilot test was held with the head nurses of the participating wards. The 32-item survey consisted of 14 behavioral and 18 attitudinal statements to be graded by the nurses on a five-point Likert-type scale.
Because nonsurvey issues delayed implementation of the diary at one of the wards, that ward was excluded from participation in this part of the study. The authors invited all oncology nurses working at one of the other seven oncology wards to participate in the survey. Nurses who worked exclusively on night shifts were excluded. The authors attempted to attain a response rate of 70% from every ward and took extra measures to do this by sending email reminders or organizing an extra staff meeting, depending on the midterm response rate. The surveys were to be completed anonymously. SPSS®, version 20.0, was used for descriptive data analyses.
Focus Groups
Three focus groups—one for nurses working in the outpatient clinics and two for nurses working in the hospital wards—were organized with the aim of gaining richer insight into the nurses’ perspective of working with the symptom diary. The first attempt at identifying potential participants was made at the end of the survey. To ensure approximately equal representation of nurses having positive feelings and those having negative feelings toward the symptom diary, additional candidates were considered with input from the head nurses.
The topic list for the focus group discussions was inspired by the survey results and included diary use in daily practice, patient communication regarding the patient diary, and multidisciplinary collaboration. Focus group interviews were conducted by two researchers. One of them was also the driving force behind the implementation of the diary. Although the authors were aware that her participation could influence participants’ feedback, her presence was crucial because she had important experience in conducting qualitative interviews. At the beginning of the focus groups, open discussion (on positive and negative aspects of the symptom diary) was emphasized as fundamental to the purpose of the current study.
Focus group discussions were audio recorded and transcribed verbatim. Two researchers read and reread the transcripts to grasp the key concepts expressed in the nurses’ experiences with the symptom diary. Transcripts were coded using paper and pencil. Preliminary results were discussed within the research team.
Results
Survey
One hundred thirty-nine nurses received the survey, and 79 surveys were completed. Therefore, the overall response rate was 57%, ranging from 33%–88% across wards. The respondents’ mean age was 39 years (range = 21–61 years), and their mean years of experience as an oncology nurse was 12 years (range = 1–34 years). The behavioral questions of the survey and a descriptive summary of the nurses’ responses are presented in Table 1. Table 2 provides results of the attitudinal survey questions. 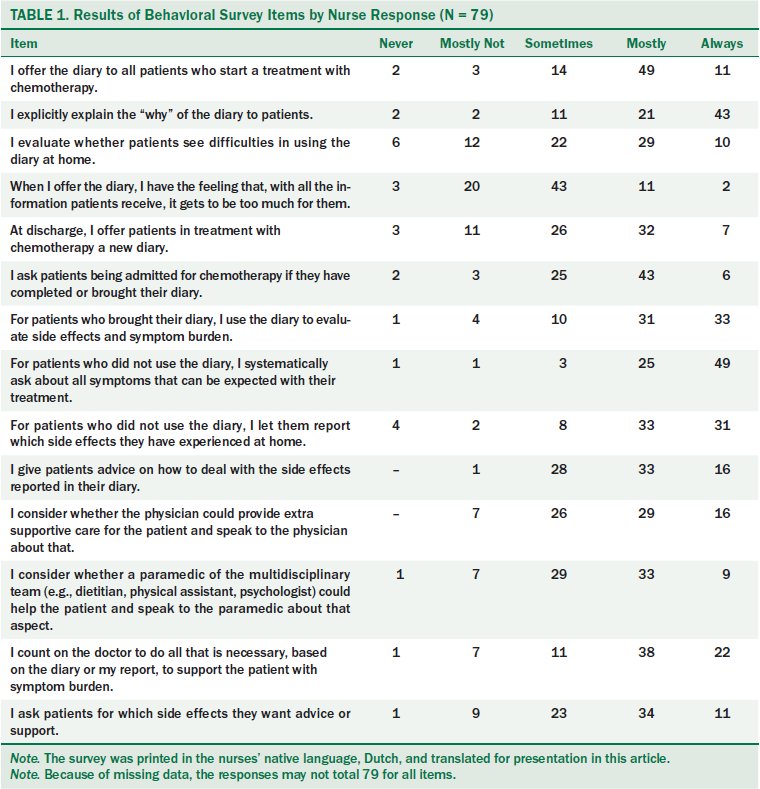
Diary Use
Forty-nine respondents reported that they mostly offered a diary to patients starting chemotherapy treatment, and 11 reported that they always did. At the patients’ next hospital visit, only 32 respondents mostly offered a diary and 7 always did. Forty-three respondents indicated that they always explained the rationale behind the diary to patients. Thirty-three always evaluated symptom burden by means of the diary; 31 mostly did. However, only 6 nurses reported that they always asked the patient for his or her diary, 43 indicated they mostly did, and 25 only sometimes did.
[[{"type":"media","view_mode":"media_original","fid":"34981","attributes":{"alt":"","class":"media-image","height":"882","typeof":"foaf:Image","width":"760"}}]]
Attitudes and Beliefs
Forty-three nurses reported that they sometimes felt that “it gets to be too much for the patient” to use the diary. At the same time, 46 nurses reported that patients who used the diary felt good about doing so. From their own perspective, 71 nurses agreed that the diary enabled them to gain quick information about the symptoms that patients experience. Sixty-three nurses found that the diary provided reliable information about symptoms experienced at home. Regarding their past practice of asking open-ended questions about side effects, 37 nurses said that this did not give them complete information on experienced symptoms, and 31 believed that it did. Of note, 54 nurses felt that the symptom diary motivated them to address reported symptoms rather than overlook them.
Use of the diary resulted in an increased workload, according to 44 nurses. Twenty-one nurses said that it did not. Forty-two nurses found using the diary in their daily practice reasonable, and 12 found that it was not.
Focus Group
Fourteen nurses (13 women, 1 man) participated in a focus group. Their mean age was 41 years (range = 27–61 years), and their mean experience as an oncology nurse was 12 years (range = 2–34 years). All focus groups lasted from 50–60 minutes.
The focus group results showed that nurses’ use of the diary was influenced by five factors: personal beliefs about the value of the diary, perceived views about patient perceptions of the diary, the nursing team’s attitude toward the diary, collaboration with doctors, and practical barriers or facilitators in adopting the tool.
Nurses’ Personal Beliefs
How nurses personally viewed the symptom diary (whether using it is advantageous to patient care) influenced how often they offered and used the symptom diary. One group of nurses seemed strongly convinced of the diary’s value. They believed that the diary prevented patients minimizing or forgetting symptoms. According to one nurse,
Before, when you just did the oral conversation and asked about their first days at home, I believe they sometimes already did not know anymore, or that it wasn’t fresh in their memory, and that they left things out of the conversation. As for now [with the diary], you can see everything. And then nothing gets forgotten.
Nurses also found that the diary helped them talk about symptoms with patients. The diary enabled them to address reported symptoms quickly and directly, instead of having to slowly discover which symptoms the patient experienced only after extensive questioning. One nurse said, “When, for example, fatigue is in red (i.e., red box or severe fatigue). You don’t go asking how tired he has been. You can immediately work further on that.”
Some explained that the diary made talking about symptoms, that would otherwise be easily left undisclosed by the patient, easier:
I am really glad about the psychological distress item . . . because it’s not easy to ask about that. . . . And when you see it in the diary, that motivates you to ask . . . “Are you OK? Because I see that you are worrying a lot,” for example.
However, other nurses expressed more doubts about the diary’s added value. They said they were often still relying on their old habits of simply asking questions orally. According to one nurse, “In a conversation, you can get to know a lot, too, you know, without actually using the diary. I think that view still stands a bit.”
Nurses’ Perceived Views About Patient Perceptions
How nurses perceived the patients’ response to the diary influenced their beliefs and behavior toward it. For example, when a patient was reluctant to use the diary, this seemed to discourage some nurses from offering it to subsequent patients.
In addition, based on some patients’ reactions or their own beliefs, some nurses assumed that the diary was “asking too much” or was “too confrontational.” The nurses’ presumed patient perceptions of the diary made them hesitant to actively use or promote it, shown by the following participant quotes:
I think they have so much on their mind already. Then, to have to go and write down all their problems. That, maybe, is a bit too much.
I believe that if I were sick, I wouldn’t use the diary either. I would rather go easy on it, rather than taking control. It’s a matter of personality.
Other nurses confirmed that not all patients found the diary to be helpful, but this did not seem to dissuade them from actively using the diary.
Nursing Team’s Attitude
Some nurses reported that use of the symptom diary had become routine in their ward, with most colleagues agreeing with the rationale and purpose of the symptom diary and the notion that the whole team should use it. One nurse said, “I think in our team, there’s only some individuals not working with the diary. But most of them [nurses] offer the diary, and so most people [patients] use it, yes.”
However, other nurses said that no consensus was reached within the team. Some colleagues made efforts to work with the diary, but others did not. Some nurses were resigned to the fact that some colleagues struggled to adopt new tools, and they did not seem to let this view discourage them from using the diary themselves. Other nurses stated that continuing to work with the diary was hard when the team did not seem to join in: “Well, after a while you go thinking, ‘Oh well, I’ll just quit making the effort, because I seem to be the only one doing so.’”
Some mentioned the discouraging effect on patients when not everyone in the nursing team was consistently using the diary: “And then patients get discouraged too, because I had someone [a patient] saying, ‘Well, I entered it completely, I really did my best and last time, nobody asked about it.’”
Nurses’ Collaboration With Doctors
All nurses agreed that doctors’ use of the diary was imperative to the success of the symptom diary. Some nurses shared positive experiences of doctors making use of the patients’ diary or electronic report to explore and manage symptoms: “I consequently ask about it [the diary]. And then it gets passed on [to the doctors], and it always gets managed. Luckily!”
However, several nurses expressed disappointment about doctors not seeming to care about the diary, or not even seeming to engage in supportive care. Nurses reported that doctors’ ignorance or neglect of the diary did not only discourage their own efforts but also those of the patient. In addition, it kept patients from receiving the symptom support they needed and asked for. According to one nurse,
I think it’s a real pity, because patients are actually enthusiastic about it and they really use it punctually. You get those diaries back and they are completed, and there’s things written, and they really put effort into using it. And then it really doesn’t get followed up. That discourages us [nurses] to continue with it, but patients, too.
Practical Barriers or Facilitators
From the focus group results, some nurses were clearly still struggling to adopt the diary in their daily practice. Some said they still easily forgot about the diary: “And to always think about it: ‘Oh, I have to offer the diary, too.’ At our ward, it’s all going so quickly. I find it hard. I admit, I often forget.”
Some nurses referred to the importance of reminders and said they saw that their head nurse played an important role in facilitating and encouraging implementation of the diary. Some explained arrangements that had been made in their ward to facilitate the use of the diary:
Our head nurse is really behind it. . . . She sometimes puts the diaries out for us. So it really gets encouraged.
At our ward, it doesn’t get talked about. That’s a real miss. It is not an issue. That’s too bad.
Time and the extra workload were other issues. On the busiest days, integrating the diary into daily practice was more difficult. However, nurses disagreed about how much time using the diary took. Some felt that it took extra time, and others believed it helped them quickly look over a patient’s symptom experience that otherwise would have been explored by asking questions.
Discussion
The aim of the current study was to evaluate the implementation of a patient symptom diary from the nurses’ perspective. Specifically, the authors wanted to get a better understanding of the factors that influence nurses’ attitudes toward symptom diaries and their use, or nonuse, in daily practice. Previous studies (Børøsund, Ruland, Moore, & Ekstedt, 2013; Hoekstra et al., 2006; Mills et al., 2008), as well as the current survey results, show that adequate application of symptom-report tools in routine practice is complex. Insight into the experience of healthcare professionals working with such tools can inform strategies that aim to ensure adoption, appropriate implementation, and maintenance of these interventions, and, consequently, to ensure their desired health outcomes (Bartholomew et al., 2011).
From the current results, many oncology nurses across a wide age range (21–61 years) and experience (1–34 years) seemed to be convinced about the relative advantage and compatibility of the diary, both of which are central attributes in the adoption rate of innovations (Grol, Wensing, Eccles, & Davis, 2015; van der Weide & Smits, 2004). Nurses reported that the diary enabled them to get quick and deeper insight into patients’ symptoms and helped them to give better symptom support. However, not all nurses were convinced, and some were still weighing the benefits and disadvantages of the diary six months after implementation. Some were convinced that their old practice of asking about symptoms was equally effective. More striking were the doubts some nurses had about patients’ perceptions of the diary. Some felt that the diary was too demanding, and this perception or assumption discouraged some nurses from using the diary. The estimated burden to patients was also suggested by Maguire et al. (2008), who said nurses felt that sometimes the diary was too much for patients to handle. Therefore, study of the patient perspective can be valuable in further encouraging nurses to develop positive attitudes toward using the symptom diary.
The ultimate aim of the diary (to improve supportive care) can be achieved only if symptoms are actually discussed adequately and managed. Of note, the majority of the participating nurses reported that the diary motivated them to better manage symptoms. Although this was a positive outcome, the focus groups raised another critical issue in successful implementation of the diary—namely, poor collaboration with the doctors. For success, nurses emphasized the importance of doctors using the diary or the electronically reported summary of it. Even more so, they emphasized that, for successful implementation, doctors needed to actually manage symptoms reported in the diary. Although oncologists were aware and supportive of the new practice, their specific role in the practical application of the diary could have been too loosely defined, or they may not have been convinced about the utility of the diary and its contribution. A study by Pereira et al. (2016) showed that the uptake and perceived value of systematic symptom assessment varied across disciplines and was lowest among physicians. Although the medical staff had approved the introduction of the diary into nursing practice, no clear discussion or consensus took place on its integration in the medical workflow. Daily medical practice was run by physicians in training, highlighting the need for clear actions and strategies to inform and engage physicians in the use of the diary in daily clinical practice (Wintner et al., 2016).
Time constraints and workload could affect whether nurses used the diary. Previous studies showed that nurses have mixed feelings about the extra workload associated with these kinds of interventions (Maguire et al., 2008; Miller, Taylor, Kearney, et al., 2007). Of note, a study by Velikova et al. (2004) on measuring quality of life in routine oncology practice showed a significant positive effect on discussion of symptoms without prolonging the encounters. The current study indicates that nurses believed that the diary saves time in detecting symptoms and, at the same time, it compels nurses to take the time to handle reported symptoms.
Lack of nursing skills to address symptoms and quality-of-life issues is reported as a barrier to using symptom-management tools (Maguire et al., 2008; Snyder et al., 2012). The current survey results indicate that the majority, but not all, of the participating nurses felt competent in providing self-care advice to patients. A lack of self-confidence in providing symptom assistance did not emerge as a concern during the focus groups.
The current study evaluated nurses’ experience with a paper diary completed by patients receiving chemotherapy. Several web-based and mobile symptom-report applications have been developed (Basch et al., 2016; Børøsund et al., 2013; Johnsen et al., 2013; Kearney et al., 2009). These offer the advantage of alerting clinicians about patients’ symptoms between clinic visits and perhaps allowing a more timely response. Although these applications are expected to be more important in the future, many patients lack access to a computer at home or a mobile telephone, or lack the necessary skills to use them (Judson et al., 2013; Wintner et al., 2015, 2016). Therefore, paper symptom-report tools remain a relevant alternative, and working with paper diaries may provide important, unique lessons for better implementation and application of electronic tools.
Limitations
The relatively poor response rate at some of the participating wards is the main limitation of the current study. Response rates were affected by major transitions at some wards at the time of the survey (e.g., implementation of an electronic health record). However, that poor response rates at some wards indicated poorer acceptance of the diary among those teams cannot be completely ruled out.
The evaluation took place about six months after the introduction. At this point, all nurses had the opportunity to use the diary. Frequency of diary use or familiarity were not taken into account during the sampling or analytical process. However, infrequent occasions to use the diary, because of their workplace (e.g., day care center versus hospitalization ward) or their motivation or resistance to change, may have influenced the perspective of nurses in the survey, as well as the focus group.
The risk of selection bias was possibly present in the focus groups, because nurses who volunteered for the groups seemed particularly motivated to participate in the group discussions. However, in selecting participants for the focus groups, the authors were careful to select nurses with positive, negative, or mixed feelings about the diary. This balance was reflected in the discussions during the focus groups.
Finally, one of the interviewers was the clinical nurse specialist responsible for the implementation of the diary, which could have led to participants giving socially desirable answers. However, from a close inspection of the data, the authors believe that this was unlikely; the participating nurses’ answers showed they were uninhibited in speaking out.
Implications for Nursing
The current findings on nurses’ perspectives of symptom-report tools indicate the need for implementation strategies that encourage developing and affirm positive attitudes toward the symptom diary. These include organizing discussions about implementation and involving key individuals and opinion leaders in the process (Grol et al., 2015). Additional motivation for nurses to integrate the diary into their daily routines may come from a better understanding of patients’ perspectives of diary usage. The authors’ evaluation of the patient perspective is underway and will be reported elsewhere.
Because the diary requires collective and coordinated symptom management from nurses and doctors, both groups should be engaged in all stages of implementation (Locklear et al., n.d.; Wintner et al., 2016). Although the diary was integrated in the nursing workflow, clear integration in the medical workflow is needed to engage physicians in the uptake of PRO into their clinical routine (Locklear et al., n.d.; Wintner et al., 2016). Flagging clinically important scores and linking PROs with clinical practice guidelines and interventions are possible ways to actively engage clinicians and, at the same time, make PROs actionable. Diary uptake and integration also may benefit from engaging physician and nurse champions to promote diary use (Locklear et al., n.d.; Wintner et al., 2016). Finally, long-term follow-up will be necessary to monitor the adoption and sustainability of the diary and take appropriate actions. Research is needed to inform effective implementation strategies and application of PROs.
Conclusion
Adequate application of patient symptom-report tools is crucial for achieving their desired outcome. However, the nurse perspective explored in the current study revealed that integrating a patient symptom diary into daily practice is complex. Several factors were uncovered that tended to impede adequate implementation. These factors inform new strategies, such as the engagement of physicians, that will improve implementation of symptom-report tools in daily practice.
About the Author(s)
Coolbrandt is a clinical nurse specialist and Bruyninckx is a nurse, both in the Department of Oncology Nursing; Verslype is a professor in the Department of Hepatology, all at University Hospitals Leuven; Steffens is a PhD candidate in the Department of Public Health and Primary Care at Katholieke Universiteit (KU) Leuven; Vanhove is an oncology nurse in the Department of Oncology Nursing, and Wildiers is an adjunct head of clinic in the Department of General Medical Oncology, both at University Hospitals Leuven; and Milisen is a professor in the Department of Public Health and Primary Care in the Academic Centre for Nursing and Midwifery at KU Leuven, all in Belgium. Verslype has previously consulted for Sirtex, Pfizer, Novartis, and Bayer, and has received support from Bristol-Myers Squibb, Bayer, and Ispen, as well as fees for participation in advisory or review activities from Bayer and Novartis. No other financial relationships to disclose. Coolbrandt, Bruyninckx, Steffens, Vanhove, and Wildiers completed the data collection. Coolbrandt, Bruyninckx, Steffens, and Wildiers provided statistical support. Coolbrandt, Bruyninckx, Steffens, Wildiers, and Milisen provided the analysis. All authors contributed to the conceptualization and design and manuscript preparation. Coolbrandt can be reached at annemarie.coolbrandt@uzleuven.be, with copy to editor at ONFEditor@ons.org. Submitted October 2016. Accepted for publication March 1, 2017.
References
Atkinson, T.M., Ryan, S.J., Bennett, A.V., Stover, A.M., Saracino, R.M., Rogak, L.J., . . . Basch, E. (2016). The association between clinician-based common terminology criteria for adverse events (CTCAE) and patient-reported outcomes (PRO): A systematic review. Supportive Care in Cancer, 24, 3669–3676. doi:10.1007/s00520-016-3297-9
Bartholomew, L.K., Parcel, G.S., Kok, G., Gottlieb, N.H., & Fernandez, M.E. (2011). Planning health promotion programs: An intervention mapping approach (3rd ed.). San Francisco, CA: Jossey-Bass.
Basch, E., Deal, A.M., Kris, M.G., Scher, H.I., Hudis, C.A., Sabbatini, P., . . . Schrag, D. (2016). Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. Journal of Clinical Oncology, 34, 557–565. doi:10.1200/JCO.2015.63.0830
Blackwood, B. (2006). Methodological issues in evaluating complex healthcare interventions. Journal of Advanced Nursing, 54, 612–622. doi:10.1111/j.1365-2648.2006.03869.x
Børøsund, E., Ruland, C.M., Moore, S., & Ekstedt, M. (2014). Nurses’ experiences of using an interactive tailored patient assessment tool one year past implementation. International Journal of Medical Informatics, 83(7), E23–E34. doi:10.1016/j.ijmedinf.2013.10.010
Cornbleet, M.A., Campbell, P., Murray, S., Stevenson, M., & Bond, S. (2002). Patient-held records in cancer and palliative care: A randomized, prospective trial. Palliative Medicine, 16, 205–212. doi:10.1191/0269216302pm541oa
Detmar, S.B., Muller, M.J., Schornagel, J.H., Wever, L.D., & Aaronson, N.K. (2002). Health-related quality-of-life assessments and patient-physician communication: A randomized controlled trial. JAMA, 288, 3027–3034.
Grol, R., Wensing, M., Eccles, M., & Davis, D. (Eds.). (2015). Improving patient care: The implementation of change in health care (2nd ed.). Hoboken, NJ: Wiley-Blackwell.
Henry, D.H., Viswanathan, H.N., Elkin, E.P., Traina, S., Wade, S., & Cella, D. (2008). Symptoms and treatment burden associated with cancer treatment: Results from a cross-sectional national survey in the U.S. Supportive Care in Cancer, 16, 791–801. doi:10.1007/s00520-007-0380-2
Hoekstra, J., de Vos, R., van Duijn, N.P., Schadé, E., & Bindels, P.J. (2006). Using the symptom monitor in a randomized controlled trial: The effect on symptom prevalence and severity. Journal of Pain and Symptom Management, 31, 22–30. doi:10.1016/j.jpainsymman.2005.06.014
Howell, D., Molloy, S., Wilkinson, K., Green, E., Orchard, K., Wang, K., & Liberty, J. (2015). Patient-reported outcomes in routine cancer clinical practice: A scoping review of use, impact on health outcomes, and implementation factors. Annals of Oncology, 26, 1846–1858. doi:10.1093/annonc/mdv181
Jakobsson, S., Ekman, T., & Ahlberg, K. (2008). Components that influence assessment and management of cancer-related symptoms: An interdisciplinary perspective. Oncology Nursing Forum, 35, 691–698. doi:10.1188/08.ONF.691-698
Johnsen, A.T., Petersen, M.A., Pedersen, L., Houmann, L.J., & Groenvold, M. (2013). Do advanced cancer patients in Denmark receive the help they need? A nationally representative survey of the need related to 12 frequent symptoms/problems. Psycho-Oncology, 22, 1724–1730. doi:10.1002/pon.3204
Judson, T.J., Bennett, A.V., Rogak, L.J., Sit, L., Barz, A., Kris, M.G., . . . Basch, E. (2013). Feasibility of long-term patient self-reporting of toxicities from home via the Internet during routine chemotherapy. Journal of Clinical Oncology, 31, 2580–2585. doi:10.1200/JCO.2012.47.6804
Kanatas, A.N., Mehanna, H.M., Lowe, D., & Rogers, S.N. (2009). A second national survey of health-related quality of life questionnaires in head and neck oncology. Annals of the Royal College of Surgeons of England, 91, 420–425. doi:10.1308/003588409X428306
Kearney, N., Kidd, L., Miller, M., Sage, M., Khorrami, J., McGee, M., . . . Gray, P. (2006). Utilising handheld computers to monitor and support patients receiving chemotherapy: Results of a UK-based feasibility study. Supportive Care in Cancer, 14, 742–752. doi:10.1007/s00520-005-0002-9
Kearney, N., McCann, L., Norrie, J., Taylor, L., Gray, P., McGee-Lennon, M., . . . Maguire, R. (2009). Evaluation of a mobile phone-based, advanced symptom management system (ASyMS) in the management of chemotherapy-related toxicity. Supportive Care in Cancer, 17, 437–444. doi:10.1007/s00520-008-0515-0
Locklear, T., Miriovsky, B.J., Willig, J.H., Staman, K., Bhavsar, N., Weinfurt, K., & Abernethy, A. (n.d.). Strategies for overcoming barriers to the implementation of patient-reported outcomes measures. Retrieved from https://www.nihcollaboratory.org/Products/Strategies-for-Overcoming-Bar…
Lorig, K.R., & Holman, H. (2003). Self-management education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine, 26, 1–7.
Maguire, R., McCann, L., Miller, M., & Kearney, N. (2008). Nurse’s perceptions and experiences of using of a mobile-phone-based Advanced Symptom Management System (ASyMS) to monitor and manage chemotherapy-related toxicity. European Journal of Oncology Nursing, 12, 380–386. doi:10.1016/j.ejon.2008.04.007
Miller, M., Taylor, A., Kearney, N., Paterson, G., Wells, M., Roe, L., . . . Maguire, R. (2007). Evaluation of the feasibility and acceptability of an oral care diary by patients during chemotherapy. International Journal of Nursing Studies, 44, 693–701. doi:10.1016/j.ijnurstu.2006.01.009
Miller, M., Taylor, A., Wells, M., Roe, L., Hagen, S., Parson, F., . . . Kearney, N. (2007). Health professionals’ views of the feasibility and acceptability of an oral care diary by patients during chemotherapy. European Journal of Oncology Nursing, 11, 82–84. doi:10.1016/j.ejon.2006.02.006
Mills, M.E., Murray, L.J., Johnston, B.T., & Donnelly, M. (2008). Feasibility of a standardised quality of life questionnaire in a weekly diary format for inoperable lung cancer patients. European Journal of Oncology Nursing, 12, 457–463. doi:10.1016/j.ejon.2008.06.003
Passik, S.D., Kirsh, K.L., Donaghy, K., Holtsclaw, E., Theobald, D., Cella, D., & Breitbart, W. (2002). Patient-related barriers to fatigue communication: Initial validation of the fatigue management barriers questionnaire. Journal of Pain and Symptom Management, 24, 481–493.
Patrick, D.L., Ferketich, S.L., Frame, P.S., Harris, J.J., Hendricks, C.B., Levin, B., . . . Vernon, S.W. (2004). National Institutes of Health state-of-the-science conference statement: Symptom management in cancer: Pain, depression, and fatigue, July 15–17, 2002. Journal of the National Cancer Institute Monographs, 32, 9–16. doi:10.1093/jncimonographs/djg014
Pereira, J.L., Chasen, M.R., Molloy, S., Amernic, H., Brundage, M.D., Green, E., . . . Klinger, C.A. (2016). Cancer care professionals’ attitudes toward systematic standardized symptom assessment and the Edmonton symptom assessment system after large-scale population-based implementation in Ontario, Canada. Journal of Pain and Symptom Management, 51, 662–672. doi:10.1016/j.jpainsymman.2015.11.023
Richard, A.A., & Shea, K. (2011). Delineation of self-care and associated concepts. Journal of Nursing Scholarship, 43, 255–264. doi:10.1111/j.1547-5069.2011.01404.x
Ruland, C.M., Holte, H.H., Røislien, J., Heaven, C., Hamilton, G.A., Kristiansen, J., . . . Ellison, M.C. (2010). Effects of a computer-supported interactive tailored patient assessment tool on patient care, symptom distress, and patients’ need for symptom management support: A randomized clinical trial. Journal of the American Medical Informatics Association, 17, 403–410. doi:10.1136/jamia.2010.005660
Snyder, C.F., Aaronson, N.K., Choucair, A.K., Elliott, T.E., Greenhalgh, J., Halyard, M.Y., . . . Santana, M. (2012). Implementing patient-reported outcomes assessment in clinical practice: A review of the options and considerations. Quality of Life Research, 21, 1305–1314. doi:10.1007/s11136-011-0054-x
Snyder, C.F., Jensen, R.E., Geller, G., Carducci, M.A., & Wu, A.W. (2010). Relevant content for a patient-reported outcomes questionnaire for use in oncology clinical practice: Putting doctors and patients on the same page. Quality of Life Research, 19, 1045–1055. doi:10.1007/s11136-010-9655-z
Sun, V., Borneman, T., Koczywas, M., Cristea, M., Piper, B.F., Uman, G., & Ferrell, B. (2012). Quality of life and barriers to symptom management in colon cancer. European Journal of Oncology Nursing, 16, 276–280. doi:10.1016/j.ejon.2011.06.011
Sun, V.C., Borneman, T., Ferrell, B., Piper, B., Koczywas, M., & Choi, K. (2007). Overcoming barriers to cancer pain management: An institutional change model. Journal of Pain and Symptom Management, 34, 359–369. doi:10.1016/j.jpainsymman.2006.12.011
van der Weide, M., & Smits, J. (2004). Adoption of innovations by specialised nurses: Personal, work and organisational characteristics. Health Policy, 68, 81–92. doi:10.1016/j.healthpol.2003.09.007
Velikova, G., Booth, L., Smith, A.B., Brown, P.M., Lynch, P., Brown, J.M., & Selby, P.J. (2004). Measuring quality of life in routine oncology practice improves communication and patient well-being: A randomized controlled trial. Journal of Clinical Oncology, 22, 714–724. doi:10.1200/JCO.2004.06.078
Wintner, L.M., Giesinger, J.M., Zabernigg, A., Rumpold, G., Sztankay, M., Oberguggenberger, A.S., . . . Holzner, B. (2015). Evaluation of electronic patient-reported outcome assessment with cancer patients in the hospital and at home. BMC Medical Informatics and Decision Making, 15, 110. doi:10.1186/s12911-015-0230-y
Wintner, L.M., Sztankay, M., Aaronson, N., Bottomley, A., Giesinger, J.M., Groenvold, M., . . . Holzner, B. (2016). The use of EORTC measures in daily clinical practice—A synopsis of a newly developed manual. European Journal of Cancer, 68, 73–81. doi:10.1016/j.ejca.2016.08.024

