Differences in Coping Among African American Women With Breast Cancer and Triple-Negative Breast Cancer
Purpose/Objectives: To determine differences in psychological distress, symptoms, coping capacity, and coping abilities among African American (AA) women with triple-negative breast cancer (TNBC) and non-TNBC and to explore differences in relationships among these variables.
Design: A prospective, descriptive, comparative, and correlational design.
Setting: Johns Hopkins Hospital in Baltimore, Maryland.
Sample: 30 AA women with breast cancer.
Methods: Patients completed questionnaires during chemotherapy. The Transactional Model of Stress and Coping was used to guide the research.
Main Research Variables: Psychological distress, symptoms, coping capacity, and coping ability.
Findings: Patients with non-TNBC reported more intense present total pain, nausea and vomiting, better emotional functioning, lower cognitive functioning, use of significantly more prayer and hope, and more coping self-statements. A lower coping capacity score was associated with psychological distress in the TNBC group at midpoint and in both groups at completion of chemotherapy treatment. Patients in both groups used a higher level of positive religious coping.
Conclusions: AA women with TNBC and non-TNBC might benefit (reduced psychological distress and improved coping skills) from receiving a comprehensive psychological care program. The findings can be incorporated and tested in a comprehensive coping strategy program.
Implications for Nursing: Nurses should work closely with AA women with breast cancer undergoing chemotherapy to help them identify and consciously use coping strategies associated with increased coping capacity.
Jump to a section
Triple-negative breast cancer (TNBC) is a serious form of breast cancer that occurs more frequently in younger African American (AA) women (Susan G. Komen, 2012). Although women diagnosed with TNBC can be successfully treated, they have a poorer prognosis than women diagnosed with non-TNBC because metastasis is often involved (Dent et al., 2009; Foulkes, Smith, & Reis-Filho, 2010; National Cancer Institute, 2017). Breast cancer incidence rates are markedly higher in Caucasian women aged 60–84 years. However, AA women aged younger than 45 years have a higher rate of breast cancer and are more likely to die from it (American Cancer Society, 2015). In addition, AA women are more likely to die within seven years of TNBC diagnosis compared to non-Hispanic Caucasian and Asian women (Newman et al., 2006).
Researchers suggest that psychological distress (depression, anxiety, emotional and cognitive functioning) and symptoms (pain, fatigue, nausea and vomiting) are the most common distressing adverse effects experienced by women treated for breast cancer with IV chemotherapy (Henderson et al., 2012) and that coping strategies are beneficial to the emotional and spiritual well-being of these women (Helgeson, Snyder, & Seltman, 2004; Silva, Crespo, & Canavarro, 2012). Psychological distress and burdensome symptoms in AA women with breast cancer have negative effects on emotional and cognitive functioning (Gaston-Johanssonet al., 2015). The negative effects experienced by AA women with breast cancer during chemotherapy may be reduced by teaching them how to cope effectively and avoid poor or negative coping behaviors or strategies. Research has shown that a comprehensive coping strategy program (CCSP) composed of preparatory information, cognitive restructuring, broad coping strategies, and relaxation with guided imagery may be helpful to women dealing with breast cancer (Gaston-Johansson, Fall-Dickson, Nanda, Sarenmalm, Browall, & Goldstein, 2013). Given the higher incidence of TNBC and shorter life span (death at every age and within seven years of diagnosis) among AA women compared to non-Hispanic Caucasian and Asian women (American Cancer Society, 2015), AA women may benefit from learning how to increase their coping capacity, spiritual well-being, and use of helpful coping strategies, to descrease psychological distress and distressing symptoms.
However, no studies could be found that focused on a comprehensive psychological/coping approach to help AA women with TNBC improve coping capacity, spiritual well-being, and emotional and cognitive functioning to better cope with psychological distress and symptoms; or that examined the relationship between coping capacity and coping strategies, religious coping, and spiritual well-being associated with breast cancer and chemotherapy treatment (Huo et al., 2009; Stead et al., 2009). In addition, little is known about whether coping capacity and coping abilities during chemotherapy treatment differ among AA women diagnosed with TNBC versus AA women diagnosed with non-TNBC. Tailoring an already tested comprehensive coping strategy program to the needs of AA women with TNBC will assist them in dealing with breast cancer.
The purpose of this pilot study was to determine (a) differences in psychological distress (anxiety, depression, total distress, emotional and cognitive functioning), symptoms (pain, fatigue, nausea and vomiting), and coping capacity, and (b) differences in coping capacity and coping abilities (strategies, effectiveness, religious) and spiritual well-being among AA women with TNBC and non-TNBC.
Literature Review
Psychological Distress and Symptoms
Women diagnosed with breast cancer and treated with chemotherapy experience substantial psychological distress (depression, anxiety, emotional and cognitive functioning) and symptoms (pain, fatigue, nausea and vomiting) that can have lasting negative physiologic consequences (Jean-Pierre et al., 2007; Kenne Sarenmalm, Browall, & Gaston-Johansson, 2014; Paice & Ferrell, 2011). The psychological distress and burdensome symptoms experienced by AA women have negative effects on emotional and cognitive functioning (Gaston-Johanssson et al., 2015). A strong coping capacity has been associated with lower psychological distress and symptoms, and a weaker coping capacity may negatively affect a person’s ability to cope effectively with psychological distress (Anke, Damsgård, & Røe, 2013).
Coping Capacity
The Transactional Model of Stress and Coping describes the process in which individuals evaluate and respond to stress. An individual’s coping capacity (mechanisms used to deal with a stressful event or stressor) is strongly related to mental health and leads to the use of coping strategies and healthy behaviors (Antonovsky, 1987). According to Folkman and Lazarus (1980) and Lazarus and Folkman (1984), cognitive primary appraisal is used to evaluate a situation and its significance, such as how stressful a situation is. A secondary appraisal, an assessment of a person’s coping resources and options, addresses what one can do to resolve a stressful situation (Cohen, 1984). Coping is defined as the use of cognitive and behavioral efforts to lessen and control the effects of stress. According to Antonovsky (1987), sense of coherence is a person’s capacity to use coping mechanisms when faced with a stressor and is helpful in explaining how some people become ill under stress and others stay healthy. Sense of coherence is strongly related to mental health. Antonovsky’s (1987) definition of sense of coherence describes a person’s coping capacity. In the current study, “coping capacity” is used instead of “sense of coherence.” Antonovsky (1987) claimed that the way people relate to their life influences their health. Coping capacity has three components: (a) comprehensibility, defined as the belief that what happens in life is rational, predictable, and understandable; (b) manageability, defined as the belief that resources are adequate and at one’s disposal to help resolve difficulties as they arise; and (c) meaningfulness, defined as seeing adversity as a challenge that is worthy of engagement. Coping capacity is an adaptive response that may be important in the future development of tailored interventions. In this regard, a person’s coping capacity is more than just a coping approach; it leads a person to engage in coping strategies and healthy behaviors (Gaston-Johansson, Haisfield-Wolfe, Reddick, Goldstein, & Lawal, 2013), and people may potentially be taught to do so. According to Antonovsky (1987), individuals with a stronger coping capacity, despite extremely challenging circumstances, can effectively handle psychological stress (anxiety and depression) and symptoms and protect their health.
Coping capacity is hypothesized to be a stable trait (Antonovsky, 1987). However, longitudinal studies have yielded mixed results regarding coping capacity stability, with some studies showing a decrease in coping capacity following psychological distress (Ferguson, Brown, Taylor, & Davis, 2016; Snekkevik, Anke, Stanghelle, & Fugl-Meyer, 2003). Others have shown that mindfulness-based stress reduction can increase patients’ coping capacity and reduce distress (Matousek & Dobkin, 2010; Shapiro, Bootzin, Figueredo, Lopez, & Schwartz, 2003).
Coping Abilities
Many cognitive and behavior strategies are used to manage internal and external demands on the body (Lazarus & Folkman, 1984). Women with breast cancer are challenged to cope with a variety of stressors, such as anxiety, depression, and emotional distress and symptoms, during chemotherapy. AA women have been compared to Caucasian women, and some differences exist in the use of coping strategies. AA women have been found to use more coping strategies (Gaston-Johansson et al., 2013) and more catastrophizing, positive self-statements, praying, hoping, increased behavior activities, and diverting of attention (Henderson, Fogel, & Edwards, 2003). The current authors found no studies that compared the differences in coping capacity and the use of coping strategies among AA women diagnosed with TNBC versus non-TNBC.
Religious coping refers to aspects of organized activities, worship, or practice (Jenkins & Pargament,1988). Religious coping can influence adjustment to illness by providing emotional comfort, hope, and a sense of purpose and meaning (Johnson & Spilka, 1991) and has been associated with better quality of life (Tarakeshwar et al., 2006). In a study by Buck and Meghani (2012), AA women reported “that prayer was powerful, life changing, and signified a direct connection to God” (p. 8). Prayer helped AA women get through their illness, offered distraction from their pain, and brought them inner peace (Buck & Meghani, 2012). Gaston-Johansson, Haisfield-Wolfe, et al. (2013) found that AA women with breast cancer used a high level of positive religious coping and that negative religious coping was associated with increased anxiety and increased use of catastrophizing, as well as decreased use of positive self-statements and less spiritual well-being. To the current authors’ knowledge, no studies have explored the differences between AA women with TNBC and non-TNBC in regard to psychological distress, symptoms, and aspects of religious coping essential for an evidence-based CCSP (Gaston-Johansson, Fall-Dickson, et al., 2013) tailored to address the specific needs of AA women with TNBC.
Spiritual well-being has been defined as the way in which people understand their lives in view of their ultimate meaning and value (Koenig, McCullough, & Larson, 2001) and is an inner resource that is used to cope with major stressors associated with breast cancer. Coping capacity has been positively related to spiritual well-being, and studies suggest that a relationship with God provides a consistent and reliable source of support (Gallia & Pines, 2009; Gibson, 2003; Hamilton, Powe, Pollard, Lee, & Felton, 2007; Holt et al., 2009; Levine, Yoo, Aviv, Ewing, & Au, 2007; Mullen, Smith, & Hill, 1994). Faith in God has been reported by AA breast cancer survivors as an important coping mechanism; they felt that their breast cancer experience was guided by God (Torres, Dixon, & Richman, 2016). A study by Best et al. (2015) examining self-rated health in AA cancer survivors revealed that spirituality had positive effects on physical distress; greater peace in cancer survivors was significantly associated with lower physical and emotional distress in AAs. A qualitative study by Adams et al. (2017) showed that AA women with breast cancer viewed spirituality and religion as important contributors to acceptance and coping with cancer. The positive aspects of spiritual coping among AA women with breast cancer include enhanced coping, decision making, inner strength, and better psychological well-being (Gibson & Hendricks, 2006). A strong spiritual base is viewed as critical for survivorship among AA women with breast cancer (Davis, Myers, Nyamathi, Lewis, & Brecht, 2016).
Methods
Design and Sample
A prospective, descriptive, comparative, and correlational design was used in this pilot study to compare AA women with TNBC and AA women with non-TNBC. The Transactional Model of Stress and Coping by Lazarus and Folkman (1984) was used to guide this research. Institutional review board approval from Johns Hopkins Institutional Review Board was obtained, and participants were recruited consecutively from Johns Hopkins Hospital in Baltimore, Maryland; Johns Hopkins Bayview Medical Center in Baltimore; and Suburban Hospital in Bethesda, Maryland,after they were scheduled for chemotherapy. After consulting with comprehensive cancer centers (recruitment sites), a sample size of 30 participants was determined to be a realistic and achievable goal for recruiting and collecting data during a 12-month period. Data were collected from a convenience and consecutively selected sample of 30 adult AA women who met the following inclusion criteria: women aged 18 years or older diagnosed with breast cancer who were scheduled to receive chemotherapy of any combination. The only exclusion criterion was confusion or inability to follow the instructions to complete the questionnaire.
Instruments
Data were collected and documented on a demographic form. The authors used the Charlson Comorbidity Index, which assigns a score for the existence of comorbid conditions and one-year mortality, to collect information about the presence of specific diseases (Charlson, Szatrowski, Peterson, & Gold, 1994). Ratings were quantified according to the age of the patient if older than 40 years and associated disease, with scores ranging from 0–40. The demographic form took about three minutes to complete.
Psychological Distress
The Hospital Anxiety and Depression Scale (HADS) is a 14-item instrument developed to detect depression and anxiety symptoms (Bjelland, Dahl, Haug, & Neckelmann, 2002; Zigmond & Snaith, 1983). Of 14 items on the HADS, 7 are specific to anxiety and 7 are specific to depression. Each response is scored on a four-point Likert-type scale (0–3). Potential scores are also weighted on a subscale ranging from 0 (no symptoms) to 21 (numerous and severe symptoms). HADS scores for each subscale are defined as follows: 11–21 (cases), 8–10 (suggestive of possible cases), and 0–7 (non-cases). The HADS takes about two to five minutes to complete. Cronbach alphas are 0.93 for anxiety and for 0.9 for depression (Bjelland et al., 2002). In the current study, the Cronbach alphas were 0.89 for anxiety and 0.98 for depression.
Symptoms
Pain intensity was measured and described with the Pain-O-Meter (POM), which was developed and tested in patients with cancer to assess total present pain. The POM is a self-administered pain assessment tool. A list of 15 sensory and 11 affective word descriptors are used to describe the pain. Each word descriptor is assigned an intensity value that ranges from 1–5. A present pain intensity score is calculated for the sensory (0–36) and affective (0–34) components of pain according to the word descriptors that patients use to describe their present pain. The total present pain score is obtained by adding the sensory and affective scores. Completing the POM takes about two minutes. Test-retest reliability (0.84) and concurrent validity for the POM have been shown to have good results (Gaston-Johansson, 1996). The Cronbach alpha for the current study was 0.91.
Fatigue, nausea and vomiting, and emotional and cognitive functioning were measured using the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire–Core 30 (EORTC QLQ-C30). The QLQ-C30 is a 30-item, Likert-type scale that was developed and validated with patients with cancer by the European Organisation for Research and Treatment of Cancer. Participants were asked to rate each of the items on a converted scale ranging from 0–100. For symptom-related items, higher scores indicate worse symptoms. This instrument takes about 10 minutes to complete. The Cronbach alphas are 0.7 for nausea and vomiting and 0.8 for fatigue (Aaronson et al., 1993). In the current study, Cronbach alphas were 0.65 for nausea and vomiting, 0.89 for fatigue, 0.89 for emotional functioning, and 0.79 for cognitive functioning.
Coping
The sense of coherence (SOC) short form was used to measure coping capacity (Antonovsky, 1987; Eriksson, Lindström, & Lilja, 2007; Langius, Björvell, & Antonovsky, 1992). The SOC consists of 13 questions that are scored on a seven-point Likert-type scale ranging from 1 (weak) to 7 (strong). The SOC assesses patients’ comprehensibility of stressors (five items), manageability of stressors (four items), and meaningfulness of stressors (four items) (Antonovsky, 1987). Higher scores indicate a stronger coping capacity, with cumulative scores ranging from 13–91 (Antonovsky, 1987). A score of 13–63 points indicates low coping capacity, 64–79 indicates moderate coping capacity, and 80–91 indicates high coping capacity (Eriksson et al., 2007). The SOC takes about five minutes to complete. The Cronbach alpha for the current study was 0.85. Alpha coefficients have ranged from 0.74–0.93 (Antonovsky, 1987; Post-White, 1998).
The Coping Strategies Questionnaire (CSQ) was used to evaluate coping strategies (Keefe, 1982; Rosenstiel & Keefe, 1983). The CSQ consists of seven subscales for coping strategies: praying and hoping, reinterpreting pain, ignoring pain, coping self-statements, diverting attention, catastrophizing, and increased behavioral activities. Higher overall scores indicate more practical application of the strategy, with each subscale consisting of six items and possible scores ranging from 0–36. The Cronbach alpha for the CSQ in the current study was 0.86. The CSQ takes about seven minutes to complete. The alpha coefficient ranges from 0.71–0.89 (Culver, Arena, Antoni, & Carver, 2002), and construct validity has been demonstrated (Keefe, 1982). The Effectiveness Coping Subscale is part of the CSQ questionnaire, and scores range from 0–10.
The Brief Religious Coping Inventory (Brief RCOPE) was used to explore religious coping. The Brief RCOPE is a 14-item Likert-type scale with responses ranging from 1 (not at all) to 4 (a great deal). Positive and negative religious coping are measured using two subscales with seven items per subscale. The respective subscale scores range from 7–28. Positive religious coping correlates with compassionate or benevolent religious involvement. Conflicts in coping with a situation are reflected in negative religious coping. The Brief RCOPE takes about three minutes to complete. The Cronbach alpha coefficient is 0.87 for the positive religious coping scale and 0.69 for the negative religious coping scale (Pargament, Smith, Koenig, & Perez, 1998). In the current study, the Cronbach alphas were 0.87 for the positive scale and 0.84 for the negative scale.
The Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being (FACIT-Sp) was used to assess spiritual well-being. This consists of 12 indicators on a five-point Likert-type scale with subdomains of faith, peace, and meaning. Each subdomain score ranges from 0–16, with the total FACIT-Sp score ranging from 0–48. Higher scores indicate a greater sense of well-being. The FACIT-Sp takes about three minutes to complete. The Cronbach alpha is 0.87, and construct validity has been determined (Bredle, Salsman, Debb, Arnold, & Cella, 2011). In the current study, the Cronbach alpha was 0.94.
Procedure
Eligible participants were identified by the health-care provider, who asked them if they would be interested in participating in the study. The research nurse contacted women who expressed interest, and arrangements were made to meet in an outpatient center for an appointment. After discussion about the study, women who agreed to participate were asked to sign an informed consent form. Patients completed the demographic form and study instruments at baseline (prior to the start of first chemotherapy treatment). Data were collected at midpoint of the study and at the completion of chemotherapy. Participants were permitted to complete the instruments at home but were asked to return them within one week. The study research nurse assisted with the completion of the surveys and instruments as requested by participants while receiving chemotherapy or while at home via telephone. Clinical elements of the patients’ history were obtained from medical records.
Data Analysis
All analyses were performed using STATA statistical software, version 14.1. Summary statistics were used to describe demographic and clinical data. The Wilcoxon rank sum and Fisher’s exact tests were used to assess differences among patients with TNBC and non-TNBC. The relationships between (a) coping capacity, psychological distress, and symptoms, and (b) between coping capacity with coping ability and spirituality were examined using Spearman correlations. Statistical significance was set at p = 0.05.
Results
Demographic Variables
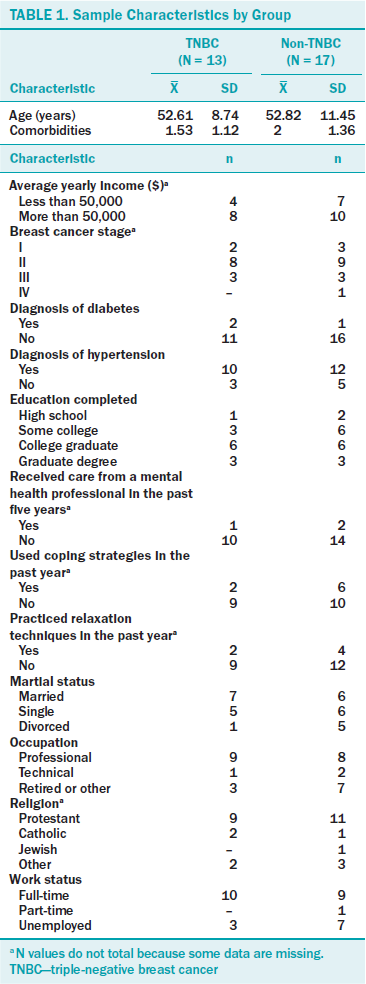
Sample characteristics are shown in Table 1. Thirty AA women participated in the study, and 13 were diagnosed with TNBC (estrogen receptor–negative, progesterone receptor–negative, and HER2eu marker–negative), with a mean age of 52.61 years. Seventeen participants were diagnosed with non-TNBC, with a mean age of 52.82 years. No significant differences existed between the groups in regard to demographic variables. Most participants reported full-time employment and Protestant religion. Twenty-two women reported hypertension as a comorbidity. Most women had stage II breast cancer. Only a few patients had practiced coping strategies and relaxation techniques or had consulted a mental health professional during the past five years.
Differences Between Psychological Distress and Symptoms During Chemotherapy
No significant differences in anxiety or depression existed between women diagnosed with TNBC versus non-TNBC. At midpoint of chemotherapy, nine participants in the total group had HADS scores indicative of anxiety, and five had scores indicative of depression (see Table 2). Of the total group, 17 had normal scores for anxiety and 21 patients had normal scores for depression.
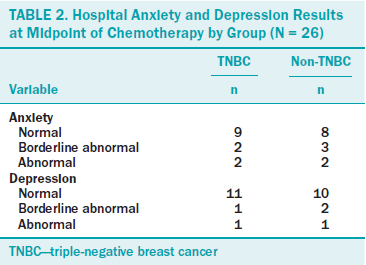
The mean score for anxiety in the non-TNBC group was 5.92 (SD = 4.15) compared to 7.3 (SD = 4.47) in the TNBC group. The mean score for depression in the non-TNBC group was 5.69 (SD = 5.6) compared to 4.38 (SD = 3.84) in the TNBC group. No significant differences in psychological distress existed between groups. The mean total for psychological distress (anxiety plus depression) was 11.61 (SD = 7.68) for the non-TNBC group and 11.69 (SD = 7.92) for the TNBC group.
At baseline, significant differences in emotional functioning were identified between women with TNBC (mean = 66.6, SD = 24.5) and women with non-TNBC (mean = 81.3, SD = 23.1), with the latter reporting greater emotional functioning (z = 2.1, p < 0.05). At completion of chemotherapy, women in the non-TNBC group reported lower cognitive functioning (mean = 71.42, SD =16.67) than women with TNBC (mean = 85, SD = 12.29, z = –2.04, p < 0.05). No significant group differences in catastrophizing existed.
In regard to symptoms, at completion of chemo-therapy, women with non-TNBC experienced significantly more intense present total pain (z = 2.02, p < 0.05) (measured by POM), and at midpoint, more nausea and vomiting (z = 2.01, p < 0.05) (measured by EORTC QLQ-C30) than the TNBC group.
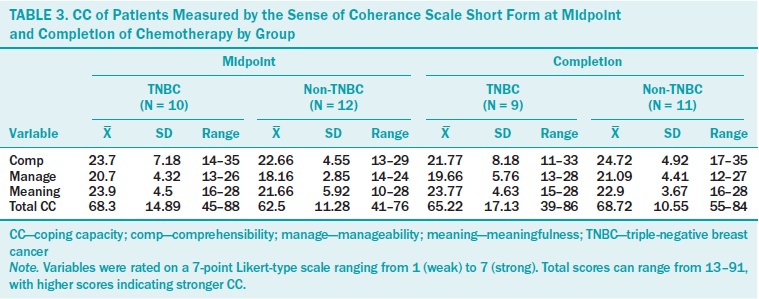
Coping Capacity and Abilities
No significant group differences regarding coping capacity existed in the total scores or subcategories at the midpoint or at the completion of chemotherapy. However, all values for coping capacity were low to moderate in both groups (see Table 3), indicating a need to increase coping capacity in both groups of patients.
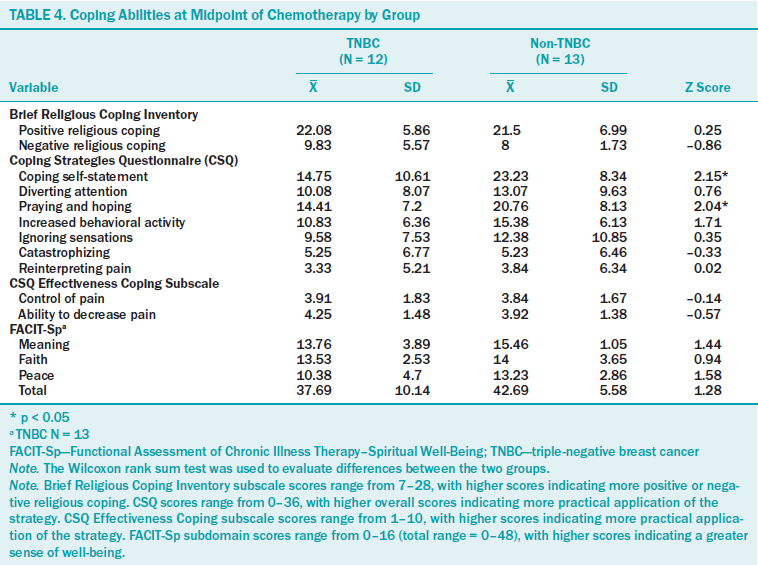
At midpoint of chemotherapy, women with non-TNBC prayed and hoped significantly more (z = 2.04, p < 0.05; “I pray to God it won’t last” and “I know someday someone will be here to help me and it will go away for a while”), as well as expressed more coping self-statements (z = 2.15, p ≤ 0.05; “No matter how bad it gets, I know I can handle it” and “I see it as a challenge and don’t let it bother me”) than the TNBC group. The mean scores for the remaining coping strategies ranged from 3.84–15.38 in the non-TNBC group and 3.33–10.08 in the TNBC group.The highest score possible for a coping strategy is 36, which means that the mean values for the five remaining coping strategies scores were low in both groups.
No significant group differences related to effectiveness ratings in control over pain and ability to decrease pain existed. The ratings for both groups were very low, with scores of 4 or less on a 10-point scale. In addition, no significant group differences in positive or negative religious coping were observed (see Table 4). Patients in both groups reported a high level of positive religious coping (“looked for a stronger connection with God”) compared to a lower level of negative religious coping. Analysis of spiritual well-being between groups revealed no significant differences.
Relationships Between Coping Capacity, Psychological Distress, and Symptoms
At midpoint of chemotherapy, significant inverse relationships were identified between coping capacity and anxiety (r = –0.69) in the TNBC group, as well as between coping capacity subcategories and total scores and depression (r ranged from –0.68 to –0.76). Lower coping capacity subcategories and total scores were related to significantly higher depression (–0.68 to –0.76) and total distress (r ranged from –0.66 to –0.75) in the TNBC group. No significant relationships existed between coping capacity and anxiety, depression, total distress, pain, and fatigue for the non-TNBC group at midpoint of chemotherapy.
A higher level of emotional functioning was related to a higher coping capacity (r = 0.62) in the non-TNBC group. Higher emotional functioning in the non-TNBC group was strongly and significantly related to a higher level of coping capacity subcategory meaningfulness (midpoint r =0.63, completion r = 0.82).
At completion of chemo-therapy, inverse relationships existed between (a) coping capacity subcategories (comprehensibility, manageability, meaningfulness) and total score and (b) between anxiety, depression, and total distress in both groups (see Table 5). Depression showed a significant, inverse relationship with all of the coping capacity subcategories and total coping capacity. Cognitive functioning was significantly and strongly related to a higher coping capacity for the meaningfulness subcategory (r =0.81) in the non-TNBC group.
[[{"type":"media","view_mode":"media_original","fid":"36606","attributes":{"alt":"","class":"media-image","height":"548","typeof":"foaf:Image","width":"1060"}}]]
Fatigue was the only symptom that was strongly and directly associated with stronger coping capacity subcategories (r ranged from 0.77–0.92) at midpoint of chemotherapy treatment in the TNBC group.
Relationships Among Coping Capacity, Coping Abilities, and Spiritual Well-Being
Among AA women diag-nosed with TNBC, at midpoint, a lower level of praying and hoping was related to two categories of higher coping capacity (comprehensibility r = –0.76 and total r = –0.62) (see Table 6). The current data also demonstrated an inverse relationship between catastrophizing and coping capacity among AA women diagnosed with TNBC (r ranged from –0.67 to –0.76). No significant relationships existed among any of the seven coping strategies and coping capacity at completion of chemotherapy for AA women diagnosed with TNBC.
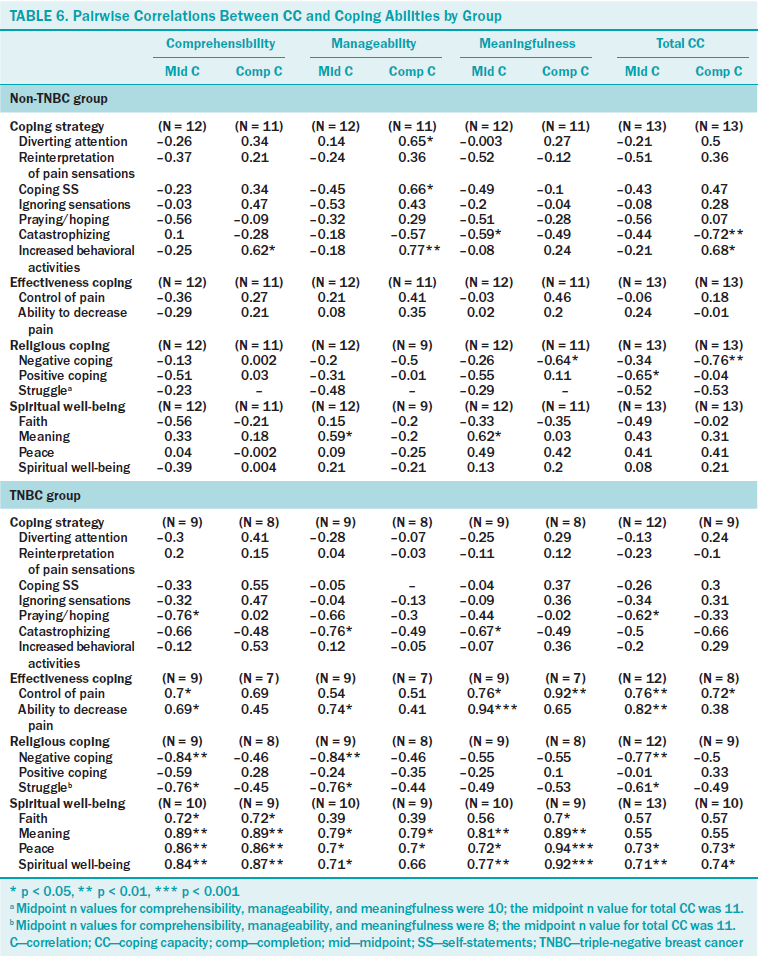
For AA women diagnosed with non-TNBC, at mid-point, significant inverse relationships existed between catastrophizing and coping capacity (meaningfulness, r = –0.59) and total coping capacity at completion (r = –0.72 ) of chemotherapy. At completion of chemotherapy, diverting attention, coping self-statements, and behavioral activities were directly related to coping capacity in the non-TNBC group (r ranged from 0.65–0.77).
Control of pain was directly related to coping capacity at midpoint (r ranged from 0.7–0.76) and at completion (r ranged from 0.72–0.92) of chemotherapy for patients with TNBC. Ability to decrease pain was also significantly related to a higher coping capacity at midpoint (r ranged from 0.69–0.94) but was not significant at completion for patients with TNBC. No significant relationships existed between coping capacity and control of pain or ability to reduce pain in patients with non-TNBC at midpoint or at the completion of chemotherapy.
At the midpoint of chemotherapy, negative religious coping and struggle were significantly and inversely related to coping capacity (comprehensibility and manageability) for patients with TNBC (r ranging from –0.61 to –0.84). Among AA women diagnosed with non-TNBC, at completion, inverse relationships existed between negative religious coping and meaningfulness and total coping capacity. The only significantly positive religious coping correlation related to a negative and weaker coping capacity was at midpoint for patients with non-TNBC.
Spiritual Well-Being
Among AA women diagnosed with TNBC, all subcategories of spiritual well-being were significantly and directly related to coping capacity categories at midpoint and at completion of chemotherapy, with correlation coefficients ranging from 0.7–0.94. Only one subcategory from spiritual well-being (meaning) was directly related to two coping capacity subcategories (manageability: r = 0.59; meaningfulness: r = 0.62), with significant correlations for patients with non-TNBC at midpoint.
In summary, no significant differences existed between the groups regarding demographic variables and psychological distress. Differences in cognitive and emotional functioning existed. Women with non-TNBC reported a greater emotional functioning and lower cognitive functioning than the TNBC group. The non-TNBC group also reported more intense pain (present total pain) and nausea and vomiting than the TNBC group. No differences regarding effectiveness ratings, religious coping, and coping capacity were observed between the groups, but all scores were low for both groups, indicating a need for improvement. In regard to coping strategies, the non-TNBC group used significantly more prayer, hope, and coping self-statements. The mean scores for the remaining coping strategies for both groups were low. The main findings revealed that an increased coping capacity was significantly associated with less anxiety and depression (total distress), as well as catastrophizing and fatigue, and an increase in emotional and cognitive functioning. A higher coping capacity was also associated with lower negative religious coping and struggle, as well as greater spiritual well-being.
Discussion
Thirteen of the participants were diagnosed with TNBC, of which 11 were diagnosed with stage II or III breast cancer and 10 were diagnosed with hypertension. Seventeen of the current sample was diagnosed with non-TNBC, of which 12 were diagnosed with stage II or III breast cancer and 12 were diagnosed with hypertension. Eleven of the total sample reported a household income of less than $50,000 per year. These sociodemographic, disease, and comorbidity results suggest that this sample represents a segment of a population experiencing health disparities (Gaston-Johansson, Hill-Briggs, Oguntomilade, Bradley, & Mason, 2007; O’Keefe, Meltzer, & Bethea, 2015). Enhanced and targeted research efforts and early treatment interventions are needed to help AA women cope with a breast cancer diagnosis and reduce hypertension. Given the evidence of poor outcomes among AA women diagnosed with TNBC and/or non-TNBC, there is an urgent need to develop and test targeted and culturally competent interventions to enhance psychological care, relaxation techniques, and coping strategies at diagnosis (Whitehead & Hearn, 2015). Relaxation training and visual imagery can be conceptualized as coping efforts directed at regulating the emotions, decreasing chemotherapy side effects (Burish & Jenkins 1992), and improving mood and quality of life (Walker et al., 1999).
Psychological Distress and Coping Capacity
An important finding from this study was the inverse relationship between coping capacity score and psychological distress (anxiety and depression) in the TNBC group at midpoint, as well as in both groups at completion of chemotherapy treatment, when symptoms have been reported as most severe (Gaston-Johansson et al., 2015). Similar results have been reported from studies of Caucasian samples (Eriksson et al., 2007; Ferguson et al., 2016; Haukkala et al., 2013; Kenne Sarenmalm, Browall, Persson, Fall-Dickson, & Gaston-Johansson, 2013). The current results suggest that routine screening for anxiety and depression prior to and during breast cancer treatment, as well as an intervention that provides strategies to enhance coping capacity, will help to recognize and diminish the adverse effects of a breast cancer diagnosis on depressive and anxiety symptoms.
Sheppard, Harper, Davis, Hirpa, and Makambi (2014) recommended routine distress screening during breast cancer care, particularly in AA women. Delivering such an intervention to people who are diagnosed with a depressive or anxiety disorder requires close consultation with a psychologist or psychiatrist. According to Winger, Adams, and Mosher (2016), few studies have examined intervention effects on coping capacity; however, research has suggested that mindfulness-based stress reduction can increase coping capacity and reduce distress in patients with cancer (Matousek & Dobkin, 2010; Shapiro et al., 2003).
The current research team found greater emotional functioning, lower cognitive functioning, more intense pain, and more nausea and vomiting in the non-TNBC group compared to the TNBC group. For the non-TNBC group, emotional functioning was strongly and directly related to coping capacity at midpoint and at completion of chemotherapy treatment. This finding suggests that improving emotional functioning with psychological care in the non-TNBC group and increasing cognitive functioning with appropriate medical and psychological treatment could benefit AA women diagnosed with breast cancer. A qualitative study by Rust and Davis (2013) recommended educating AA women with breast cancer pretreatment about potential effects on cognitive difficulties during and after chemotherapy treatment. In addition, providing patients with information on managing cancer-related side effects (American Cancer Society, 2017) to reduce anxiety, depression, pain, fatigue, and nausea and vomiting prior to chemotherapy treatment may delay the onset of and/or reduce the severity of symptoms that accompany breast cancer and its treatment.
Significant mean differences were reported, with the non-TNBC group reporting more use of the two coping strategies (coping self-statement and praying and hoping) than the TNBC group. Both groups had low mean values regarding the use of coping strategies, suggesting that the coping strategies were not appropriate or that they were not familiar with them.
A focus group of AA women with TNBC could review the coping strategies on the coping strategy questionnaire for appropriateness and, if found to be adequate, could receive education on how to use the them. More emphasis should be placed on teaching patients how to better recognize and consciously use coping strategies associated with increased coping capacity, such as coping self-statements, praying and hoping, and increased behavior activities. In addition, the results support more emphasis on recognizing and avoiding strategies, such as catastrophizing and negative religious coping, which are strongly and negatively related to coping capacity. Self-care information and methods of how to increase effective coping by controlling and decreasing pain could also be provided to patients in written materials, with appropriate, culturally orientated pictures to convey the information. A more tailored CCSP with fewer coping strategies could be used to teach women with TNBC. Women should be given examples of negative coping and catastrophizing and be taught how to recognize and avoid negative coping statements and thoughts.
AA women with TNBC should be involved in selecting, approving, and building spiritual coping aspects to be included in the CCSP. Finally, results from the current study suggest that AA women diagnosed with TNBC or non-TNBC could benefit from a comprehensive psychological care program, including a psychological health insurance package that covers the cost of care for this program, as a part of treatment of breast cancer.
Limitations
This pilot study used a small and nonprobability sample, so findings need to be considered with caution. Future studies should assess a larger sample of AA women to verify the findings from this study before incorporating the results into a CCSP. Knowledge gained from the current study could be used to enhance an already developed research-based CCSP directed at addressing the needs of AA women with TNBC (Gaston-Johansson et al., 2000; Gaston-Johansson,Fall-Dickson, et al., 2013; Gaston-Johansson, Haisfield-Wolfe, et al., 2013).
Implications for Nursing
Nurses should work closely with AA women with breast cancer undergoing chemotherapy to identify and consciously use coping strategies. Based on the findings of this study, coping strategies associated with increased coping capacity, such as coping self-statements, praying and hoping, and increased behavior activities, should be taught. AA women with breast cancer should also be educated on how to recognize and avoid the use of negative coping, such as catastrophizing and negative coping statements and thoughts. Also recommended are routine screening and risk assessments for psychological distress and psychosocial needs or deficits by clinic and inpatient nurses during follow-up visits, chemotherapy treatment, and inpatient stays. Patients in need of follow-up should be referred to a case management nurse or team. Case managers are in a unique position to facilitate the coordination of interprofessional care, referrals, and follow-up needed to improve quality of life and the breast cancer treatment experience.
Conclusion
CCSPs should be based partly on the meaningfulness component of coping capacity, encouraging individuals to engage in activities that improve emotional and cognitive functioning and use relaxation activities. Developing and incorporating the findings of this study into a CCSP could reduce psychological distress in AA women with breast cancer.
About the Author(s)
Watkins is the director of the Memory Clinic in Neuropsychiatry at the Sheppard Pratt Health System and an assistant professor in the Department of Psychiatry and Behavioral Health Sciences in the School of Medicine at Johns Hopkins University in Baltimore, MD; Kanu is a research nurse in the School of Nursing at Johns Hopkins University; Hamilton is an associate professor in the School of Nursing at Emory University in Atlanta, GA; and Kozachik is an associate professor and Gaston-Johansson is a professor emerita, both in the School of Nursing at Johns Hopkins University. Watkins is supported by the Women’s Hospital Foundation, the Sheppard Pratt Health System, the Mitsubishi Tanabe Corporation, and a Mosaic Award from the Johns Hopkins University School of Medicine. During the writing of this article, Kozachik was supported by a grant from the National Institute of Nursing Research and the National Institutes of Health. Watkins, Kanu, and Gaston-Johansson contributed to the conceptualization and design, completed the data collection, and provided statistical support and the analysis. All authors contributed to the manuscript preparation. Watkins can be reached at cwatkins@jhmi.edu, with copy to editor at ONFEditor@ons.org. Submitted November 2016. Accepted for publication April 11, 2017.
References
Aaronson, N.K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N.J., . . . de Haes, J.C. (1993). The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute, 85, 365–376.
Adams, N., Gisiger-Camata, S., Hardy, C.M., Thomas, T.F., Jukkala, A., & Meneses, K. (2017). Evaluating survivorship experiences and needs among rural African American breast cancer survivors. Journal of Cancer Education, 32, 264–271. https://doi.org/10.1007/s13187-015-0937-6
American Cancer Society. (2015). Breast cancer facts and figures, 2015–2016. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
American Cancer Society. (2017). Managing cancer-related side effects. Retrieved from https://www.cancer.org/treatment/treatments-and-side-effects/physical-s…
Anke, A., Damsgård, E., & Røe, C. (2013). Life satisfaction in subjects with long-term musculoskeletal pain in relation to pain intensity, pain distribution and coping. Journal of Rehabilitation Medicine, 45, 277–285. https://doi.org/10.2340/16501977-1102
Antonovsky, A. (1987). Unraveling the mystery of health: How people manage stress and stay well. San Francisco, CA: Jossey-Bass.
Best, A.L., Alcaraz, K.I., McQueen A., Cooper, D.L., Warren, R.C., & Stein, K. (2015). Examining the mediating role of cancer-related problems on spirituality and self-rated health among African American cancer survivors: A report from the American Cancer Society’s studies of cancer survivors-II. Psycho-Oncology, 24, 1051–1059. https://doi.org/10.1002/pon.3720
Bjelland, I., Dahl, A.A., Haug, T.T., & Neckelmann, D. (2002). The validity of the Hospital Anxiety and Depression Scale. An updated literature review. Journal of Psychosomatic Research, 52, 69–77.
Bredle, J.M., Salsman, J.M., Debb, S.M., Arnold, B.J., & Cella, D. (2011). Spiritual well-being as a component of health-related quality of life: The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp). Religions, 2, 77–94. https://doi.org/10.3390/rel2010077
Buck, H.G., & Meghani, S.H. (2012). Spiritual expressions of African Americans and Whites in cancer pain. Journal of Holistic Nursing, 30, 107–116. https://doi.org/10.1177/0898010111423420
Burish, T.G., & Jenkins, R.A. (1992). Effectiveness of biofeedback and relaxation training in reducing the side effects of cancer chemotherapy. Health Psychology, 11, 17–23.
Charlson, M., Szatrowski, T.P., Peterson, J., & Gold, J. (1994). Validation of a combined comorbidity index. Journal of Clinical Epidemiology, 47, 1245–1251.
Cohen, F. (1984). Coping. In J.D. Matarazzo, N.E., C.M. Weiss, J.A. Herd, N.E. Miller, & S.M. Weiss (Eds.), Behavioral health: A handbook of health enhancement and disease prevention (pp. 261–270). New York, NY: John Wiley and Sons.
Culver, J.L., Arena, P.L., Antoni, M.H., & Carver, C.S. (2002). Coping and distress among women under treatment for early stage breast cancer: Comparing African Americans, Hispanics and non-Hispanic Whites. Psycho-Oncology, 11, 495–504. https://doi.org/10.1002/pon.615
Davis, C.M., Myers, H.F., Nyamathi, A.M., Lewis, M., & Brecht, M.-L. (2016). The meaning of survivorship as defined by African American breast cancer survivors. Journal of Transcultural Nursing, 27, 277–285. https://doi.org/10.1177/1043659614561678
Dent, R., Hanna, W.M., Trudeau, M., Rawlinson, E., Sun, P., & Narod, S.A. (2009). Pattern of metastatic spread in triple-negative breast cancer. Breast Cancer Research and Treatment, 115, 423–428. https://doi.org/10.1007/s10549-008-0086-2
Eriksson, M., Lindström, B., & Lilja, J. (2007). A sense of coherence and health. Salutogenesis in a societal context: Åland, a special case? Journal of Epidemiology and Community Health, 61, 684–688. https://doi.org/10.1136/jech.2006.047498
Ferguson, S., Browne, J., Taylor, J., & Davis, D. (2016). Sense of coherence and women’s birthing outcomes: A longitudinal survey. Midwifery, 34, 158–165. http://doi.org/10.1016/j.midw.2015.11.017
Folkman, S., & Lazarus, R.S. (1980). An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior, 21, 219–239.
Foulkes, W.D., Smith, I.E., & Reis-Filho, J.S. (2010). Triple-negative breast cancer. New England Journal of Medicine, 363, 1938–1948. https://doi.org/10.1056/NEJMra1001389
Gaston-Johansson, F. (1996). Measurement of pain: The psychometric properties of the Pain-O-Meter, a simple, inexpensive pain assessment tool that could change health care practices. Journal of Pain and Symptom Management, 12, 172–181.
Gaston-Johansson, F., Fall-Dickson, J.M., Nanda, J., Ohly, K.V., Stillman, S., Krumm, S., & Kennedy, M.J. (2000). The effectiveness of the comprehensive coping strategy program on clinical outcomes in breast cancer autologous bone marrow transplantation. Cancer Nursing, 23, 277–285.
Gaston-Johansson, F., Fall-Dickson, J.M., Nanda, J.P., Sarenmalm, E.K., Browall, M., & Goldstein, N. (2013). Long-term effect of the self-management Comprehensive Coping Strategy Program on quality of life in patients with breast cancer treated with high-dose chemotherapy. Psycho-Oncology, 22, 530–539. https://doi.org/10.1002/pon.3031
Gaston-Johansson, F., Haisfield-Wolfe, M.E., Reddick, B., Goldstein, N., & Lawal, T.A. (2013). The relationships among coping strategies, religious coping, and spirituality in African American women with breast cancer receiving chemotherapy. Oncology Nursing Forum, 40, 120–131. https://doi.org/10.1188/13.ONF.120-131
Gaston-Johansson, F., Hill-Briggs, F., Oguntomilade, F., Bradley, V., & Mason, P. (2007). Patient perspectives on disparities in healthcare from African-American, Asian, Hispanic, and Native American samples including a secondary analysis of the Institute of Medicine focus group data. Journal of National Black Nurses’ Association, 18(2), 43–52.
Gaston-Johansson, F., Watkins, C.C., Kanu, I.K., Whitehouse, E., Sarenmalm, E.K., Brovall, M., & Kozachik, S.L. (2015). The effects of symptoms on quality of life during chemotherapy in African American women with breast cancer. Journal of National Black Nurses’ Association, 26(2), 7–16.
Gibson, L.M. (2003). Inter-relationships among sense of coherence, hope, and spiritual perspective (inner resources) of African-American and European-American breast cancer survivors. Applied Nursing Research, 16(4), 236–244. https://doi.org/10.1016/S0897-1897(03)00053-3
Gibson, L.M., & Hendricks, C.S. (2006). Integrative review of spirituality in African American breast cancer survivors. ABNF Journal, 17(2), 67–72.
Hamilton, J.B., Powe, B.D., Pollard, A.B., 3rd, Lee, K.J., & Felton, A.M. (2007). Spirituality among African American cancer survivors: Having a personal relationship with God. Cancer Nursing, 30, 309–316. https://doi.org/10.1097/01.NCC.0000281730.17985.f5
Haukkala, A., Konttinen, H., Lehto, E., Uutela, A., Kawachi, I., & Laatikainen, T. (2013). Sense of coherence, depressive symptoms, cardiovascular diseases, and all-cause mortality. Psychosomatic Medicine, 75, 429–435. https://doi.org/10.1097/PSY.0b013e31828c3fa4
Helgeson, V.S., Snyder, P., & Seltman, H. (2004). Psychological and physical adjustment to breast cancer over 4 years: Identifying distinct trajectories of change. Health Psychology, 23, 3–15. https://doi.org/10.1037/0278-6133.23.1.3
Henderson, P.D., Fogel, J., & Edwards, Q.T. (2003). Coping strategies among African American women with breast cancer. Southern Online Journal of Nursing Research, 3(4), 1–21.
Henderson, V.P., Clemow, L., Massion, A.O., Hurley, T.G., Druker, S., & Hébert, J.R. (2012). The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: A randomized trial. Breast Cancer Research and Treatment, 131, 99–109. https://doi.org/10.1007/s10549-011-1738-1
Holt, C.L., Caplan, L., Schulz, E., Blake, V., Southward, P., Buckner, A., & Lawrence, H. (2009). Role of religion in cancer coping among African Americans: A qualitative examination. Journal of Psychosocial Oncology, 27, 248–273. https://doi.org/10.1080/07347330902776028
Huo, D., Ikpatt, F., Khramtsov, A., Dangou, J.-M., Nanda, R., Dignam, J., . . . Olopade, O.I. (2009). Population differences in breast cancer: Survey in indigenous African women reveals over-representation of triple-negative breast cancer. Journal of Clinical Oncology, 27, 4515–4521. https://doi.org/10.1200/JCO.2008.19.6873
Jean-Pierre, P., Figueroa-Moseley, C.D., Kohli, S., Fiscella, K., Palesh, O.G., & Morrow, G.R. (2007). Assessment of cancer-related fatigue: Implications for clinical diagnosis and treatment. Oncologist, 12(Suppl. 1), 11–21. https://doi.org/10.1634/theoncologist.12-S1-11
Jenkins, R.A., & Pargament, K.I. (1988). Cognitive appraisals in cancer patients. Social Science and Medicine, 26, 625–633.
Johnson, S.C., & Spilka, B. (1991). Coping with breast cancer: The roles of clergy and faith. Journal of Religion and Health, 30, 21–33. https://doi.org/10.1007/BF00986676
Keefe, F.J. (1982). Behavioral assessment and treatment of chronic pain: Current status and future directions. Journal of Consulting and Clinical Psychology, 50, 896–911. http://doi.org/10.1037/0022-006X.50.6.896
Kenne Sarenmalm, E., Browall, M., & Gaston-Johansson, F. (2014). Symptom burden clusters: A challenge for targeted symptom management. A longitudinal study examining symptom burden clusters in breast cancer. Journal of Pain and Symptom Management, 47, 731–741. https://doi.org/10.1016/j.jpainsymman.2013.05.012
Kenne Sarenmalm, E., Browall, M., Persson, L.-O., Fall-Dickson, J., & Gaston-Johansson, F. (2013). Relationship of sense of coherence to stressful events, coping strategies, health status, and quality of life in women with breast cancer. Psycho-Oncology, 22, 20–27. https://doi.org/10.1002/pon.2053
Koenig, H.G., McCollough, M.E., & Larson, D.B. (2001). Handbook of religion and health. Oxford, England: Oxford University Press.
Langius, A., Björvell, H., & Antonovsky, A. (1992). The sense of coherence concept and its relation to personality traits in Swedish samples. Scandinavian Journal of Caring Sciences, 6(3), 165–171. https://doi.org/10.1111/j.1471-6712.1992.tb00146.x
Lazarus, R.S., & Folkman, S. (1984). Stress, appraisal, and coping. New York, NY: Springer.
Levine, E.G., Yoo, G., Aviv, C., Ewing, C., & Au, A. (2007). Ethnicity and spirituality in breast cancer survivors. Journal of Cancer Survivorship, 1, 212–225. https://doi.org/10.1007/s11764-007-0024-z
Matousek, R.H., & Dobkin, P.L. (2010). Weathering storms: A cohort study of how participation in a mindfulness-based stress reduction program benefits women after breast cancer treatment. Current Oncology, 17(4), 62–72. https://doi.org/10.3747/co.v17i4.572
Mullen, P.M., Smith, R.M., & Hill, E.W. (1994). Sense of coherence as a mediator of stress for cancer patients and spouses. Journal of Psychosocial Oncology, 11(3), 23–46. https://doi.org/10.1300/J077V11N03_02
National Cancer Institute. (2017). Genetics of breast and gynecologic cancers (PDQ®)–Health professional version. Retrieved from https://www.cancer.gov/types/breast/hp/breast-ovarian-genetics-pdq
Newman, L.A., Griffith, K.A., Jatoi, I., Simon, M.S., Crowe, J.P., & Colditz, G.A. (2006). Meta-analysis of survival in African American and White American patients with breast cancer: Ethnicity compared with socioeconomic status. Journal of Clinical Oncology, 24, 1342–1349. https://doi.org/10.1200/JCO.2005.03.3472
O’Keefe, E.B., Meltzer, J.P., & Bethea, T.N. (2015). Health disparities and cancer: Racial disparities in cancer mortality in the United States, 2000–2010. Frontiers in Public Health, 3, 51. https://doi.org/10.3389/fpubh.2015.00051
Paice, J.A., & Ferrell, B. (2011). The management of cancer pain. CA: A Cancer Journal for Clinicians, 61, 157–182. https://doi.org/10.3322/caac.20112
Pargament, K.I., Smith, B.W., Koenig, H.G., & Perez, L. (1998). Patterns of positive and negative religious coping with major life stressors. Journal for the Scientific Study of Religion, 37, 710–724. https://doi.org/10.2307/1388152
Post-White, J. (1998). Wind behind the sails: Empowering our patients and ourselves. Oncology Nurse Forum, 25, 1011–1017.
Rosenstiel, A.K., & Keefe, F.J. (1983). The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain, 17, 33–44.
Rust, C., & Davis, C. (2013). Chemobrain in underserved African American breast cancer survivors [Online exclusive]. Clinical Journal of Oncology Nursing, 17, E29–E34. https://doi.org/10.1188/13.CJON.E29-E34
Shapiro, S.L., Bootzin, R.R., Figueredo, A.J., Lopez, A.M. & Schwartz, G.E. (2003). The efficacy of mindfulness-based stress reduction in the treatment of sleep disturbance in women with breast cancer: An exploratory study. Journal of Psychosomatic Research, 54, 85–91.
Sheppard, V.B., Harper, F.W.K., Davis, K., Hirpa, F., & Makambi, K. (2014). The importance of contexual factors and age in association with anxiety and depression in Black breast cancer patients. Psycho-Oncology, 23, 143–150. https://doi.org/10.1002/pon.3382
Silva, S.M., Crespo, C., & Canavarro, M.C. (2012). Pathways for psychosocial adjustment in breast cancer: A longitudinal study on coping strategies and posttraumatic growth. Psychology and Health, 27, 1323–1341. https://doi.org/10.1080/08870446.2012.676644
Snekkevik, H., Anke, A.G.W., Stanghelle, J.K., & Fugl-Meyer, A.R. (2003). Is sense of coherence stable after multiple trauma? Clinical Rehabilitation, 17, 443–452. https://doi.org/10.1191/0269215503cr630oa
Stead, L.A., Lash, T.L., Sobieraj, J.E., Chi, D.D., Westrup, J.L., Charlot, M., . . . Rosenberg, C.L. (2009). Triple-negative breast cancers are increased in Black women regardless of age or body mass index. Breast Cancer Research, 11(2), R18. https://doi.org/10.1186/bcr2242
Susan G. Komen. (2012). Triple negative breast cancer—What do we know and where are we headed? Retrieved from http://ww5.komen.org/KomenPerspectives/Komen-Perspectives---Triple-Nega…
Tarakeshwar, N., Vanderwerker, L.C., Paulk, E., Pearce, M.J., Kasl, S.V., & Prigerson, H.G. (2006). Religious coping is associated with the quality of life of patients with advanced cancer. Journal of Palliative Medicine, 9, 646–657. https://doi.org/10.1089/jpm.2006.9.646
Torres, E., Dixon, C., & Richman, A.R. (2016). Understanding the breast cancer experience of survivors: A qualitative study of African American women in rural eastern North Carolina. Journal of Cancer Education, 31, 198–206. https://doi.org/10.1007/s13187-015-0833-0
Walker, L.G., Walker, M.B., Ogston, K., Heys, S.D., Ah-See, A.K., Miller, I.D., . . . Eremin, O. (1999). Psychological, clinical and pathological effects of relaxation training and guided imagery during primary chemotherapy. British Journal of Cancer, 80, 262–268. https://doi.org/10.1038/sj.bjc.6690349
Whitehead, N.E., & Hearn, L.E. (2015). Psychosocial interventions addressing the needs of Black women diagnosed with breast cancer: A review of the current landscape. Psycho-Oncology, 24, 497–507. https://doi.org/10.1002/pon.3620
Winger, J.G., Adams, R.N., & Mosher, C.E. (2016). Relations of meaning in life and sense of coherence to distress in cancer patients: A meta-analysis. Psycho-Oncology, 25, 2–10. https://doi.org/10.1002/pon.3798
Zigmond, A.S. & Snaith, R.P. (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67, 361–370.

