Coming of Age With Cancer: Physical, Social, and Financial Barriers to Independence Among Emerging Adult Survivors
Purpose: To explore the transition to self-care among a sample of emerging adult cancer survivors after hematopoietic cell transplantation (HCT).
Participants & Setting: 18 HCT survivors who were aged 18–29 years at the time of HCT for a primary hematologic malignancy and were 8–60 months post-HCT participated in the study. The study took place in the hematology outpatient setting at City of Hope National Medical Center.
Methodologic Approach: The authors conducted in-depth semistructured interviews and analyzed interview transcripts using grounded theory methodology.
Findings: Health-related setbacks following HCT disrupted not only participants’ journey toward self-care, but also their overarching developmental trajectory toward adulthood. Physically, participants struggled with lack of personal space around caregivers, but felt unready to live on their own. Socially, they relied on multiple caregivers to avoid relying too much on any one person. Financially, participants worried about prolonged dependence and increased needs in the future.
Implications for Nursing: Nurses can support the transition to self-care among emerging adults after HCT by recognizing the broader developmental impact of their cancer experience.
Jump to a section
Emerging adulthood refers to a distinct life stage between adolescence and adulthood, specifically from age 18 years to the mid to late 20s. Building on the work of Erik Erikson and Daniel Levinson in developmental psychology, Arnett (2004) first proposed emerging adulthood and defined five key attributes: identity exploration, instability, self-focus, feeling in-between, and possibilities. According to this theory, profound demographic shifts, social revolutions, and economic realities have resulted in a protracted developmental trajectory (Arnett, 2014; Blatterer, 2007). Specifically, compared with previous generations, emerging adulthood in the contemporary era reflects delayed entry into the traditional spheres of adulthood, such as marriage, parenthood, and a steady career.
During this life stage, young people experiment with possibilities, particularly in the areas of love and work, to define their preferences and gain a clearer picture of who they are and what they want out of life. No longer adolescents, but not yet fully adults, emerging adults occupy an in-between space. As individuals progress through the stage, they become more serious in their life choices and commitments. The developmental goal of emerging adulthood is self-sufficiency, which lays the foundation for an independent adulthood. Across multiple studies, emerging adults consistently identify accepting responsibility for oneself, making independent decisions, and achieving financial independence—rather than marriage or parenthood—as the key signifiers of adulthood (Arnett, 2014).
In general, emerging adults are an exceptionally healthy group, with nearly all (96.3%) in the age 18–24 year range reporting excellent, very good, or good health (Mulye et al., 2009). This norm makes a cancer diagnosis during this stage unexpected, complex, and potentially alienating. From a life course perspective, the intersection of a cancer diagnosis with the developmental tasks of emerging adulthood may hinder social and emotional development and successful transition to adulthood (Katz, 2015; Zebrack, 2011). The “AYA paradox” refers to the conflict between the developmental tasks of emerging adulthood and the demands of a cancer diagnosis (Kent et al., 2012). For example, emerging adults with cancer must balance their needs for autonomy with increased dependence on family; attempts to maintain engagement in education or occupation with managing treatment effects; and the development of social and intimate relationships in the context of medically imposed isolation, the threat of infertility, alterations in body image, and uncertainty regarding the future.
Leukemia and lymphoma account for about 25% of cancers in emerging adults aged 15–29 years in the United States (Howlader et al., 2016). These hematologic malignancies often require hematopoietic cell transplantation (HCT) as part of treatment. HCT aims to restore hematopoietic function by infusing stem cells from oneself (autologous) or a donor (allogeneic) after an intense conditioning regimen of high-dose chemotherapy, and, in some cases, radiation (Wood & Lee, 2011). HCT typically requires prolonged hospitalization to receive supportive care, symptom management, and close monitoring for complications such as infections or graft-versus-host disease. Although HCT has provided tremendous promise as a lifesaving treatment, it is also associated with high toxicity. In the long-term, HCT survivors face substantial risk for physical and psychological morbidity, even 10 years or more beyond treatment (Baker, Armenian, & Bhatia, 2010; Majhail & Rizzo, 2013; Sun et al., 2010, 2011).
Adolescent and young adult (AYA) oncology has emerged as a distinct field of clinical practice and research. In 2006, the National Cancer Institute (NCI) convened the Adolescent and Young Adult Oncology Progress Review Group to address disparities observed in this cohort and defined AYAs as individuals diagnosed with cancer aged 15–39 years (NCI, 2015). Since this call to action, considerable progress has been made in recognizing AYAs as a unique patient population with specific needs, circumstances, and health risks. Recently, however, the scientific community has acknowledged the heterogeneity within this broad definition and the need to focus on AYA subgroups to account for variation in experiences (Phillips-Salimi, Lommel, & Andrykowski, 2012; Smith et al., 2016). The combined risks of AYA survivors and the toxicities associated with HCT make them a particularly vulnerable group with extensive survivorship needs for the remainder of life (Bukowinski, Burns, Parsons, Perentesis, & O’Brien, 2015). A paucity of research examines the HCT experience among AYAs and how the prospect of prolonged dependence, inherent in the HCT process, affects recovery and the developmental trajectory. Therefore, the purpose of this study was to explore the transition to self-care in the recovery phase following HCT among emerging adults.
Research Approach
The authors used a qualitative, inductive approach to gain in-depth understanding of the transition to self-care after HCT among a sample of emerging adults. The institutional review boards of City of Hope National Medical Center [COH] and University of California, Los Angeles, approved this research. Using clinical registry sources at COH, the authors identified potentially eligible participants who were aged 15–29 years when they received HCT for treatment of a primary hematologic cancer and were 6–60 months post-HCT at study enrollment. Those who were younger than 18 years at the time of study entry, had relapsed since HCT, received more than one HCT, could not speak English, or were cognitively impaired were excluded from this analysis. Additional details of recruitment have been described elsewhere (Brauer et al., 2017).
Methodologic Approach
Grounded theory methodology (Corbin & Strauss, 2015), influenced by constructivism (Charmaz, 2014), guided this study. After obtaining informed consent, the first author (EB) conducted intensive interviews with each participant in a private consultation room or via telephone, depending on the participant’s preference. The authors used a semistructured interview guide, developed by EB and MH from pilot work with an AYA population, to enhance consistency (see Figure 1). Open-ended questions regarding the transition to self-care, relationships with informal caregivers, and HCT recovery allowed for flexibility in examining the unique experiences of each participant. In this study, the term self-care includes activities and behaviors of self-management, such as adhering to a medication schedule, but also broader aspects of taking care of oneself and achieving independence. On average, interviews lasted 102 minutes (range = 56–164) and were digitally recorded, transcribed, and deidentified. Data collection also included a self-reported demographic questionnaire, abstraction of clinical variables from medical records, and detailed field notes written by the primary interviewer (EB) and discussed with other members of the research team. Participants received a $50 gift card at the completion of study procedures.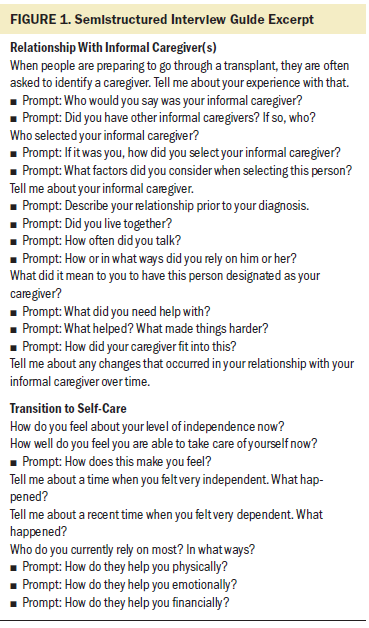
The authors engaged in data collection and analysis simultaneously to allow for constant comparison (Charmaz, 2014). They used a systematic coding process to link concrete description to theoretical insights. Beginning with initial coding, each transcript was studied and relevant action was identified while remaining close to participants’ words. Next, focused coding allowed the authors to group significant codes and form tentative categories. Through an iterative process, analysis of early interviews informed subsequent data gathering. Theoretical sampling was used to refine the interpretations and fill out properties and dimensions of categories. Using diagrams, memos, and mapping, the authors explored and tested relationships among major categories (Charmaz, 2014; Corbin & Strauss, 2015). This process continued until no new properties emerged, major theoretical categories were deemed robust, and saturation was reached (Charmaz, 2014). To enhance methodologic rigor, at least two members of the research team were engaged in analysis at each stage and met regularly to discuss and resolve issues.
Findings
The 18 participants were, on average, 26 years old (range = 19.8–34.6 years) and 32.8 months (range = 8–60 months) post-HCT at the time of the interview. See Table 1 for additional characteristics. Using emerging adulthood as a sensitizing concept (Blumer, 1954), or as a “[point] of departure for developing, rather than limiting, our ideas” (Charmaz, 2014, p. 31), the authors describe participants’ transition to self-care as a process within another broader process, the overall developmental stage of emerging adulthood. The presentation of results is focused on the interplay between these processes as they impact physical, social, and financial developmental domains. 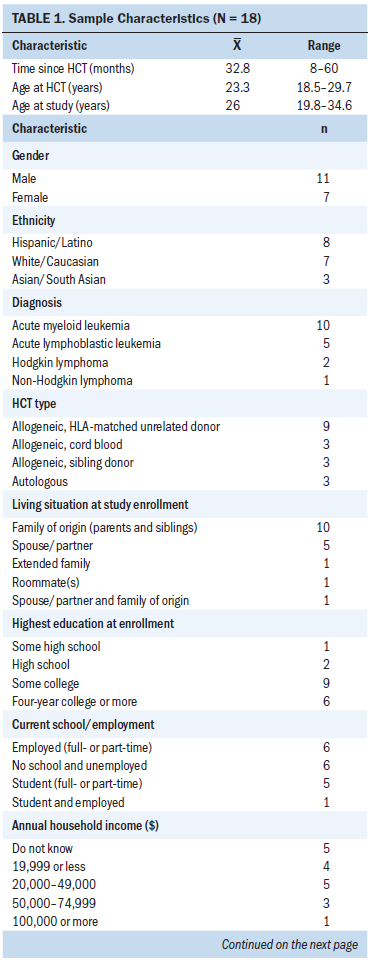
Lost Between Sick and Well
The post-HCT phase was a time of unexpected and lonely struggles during which participants felt lost somewhere between being sick and being well. This sample of survivors acknowledged being in remission from disease and described marked improvements in their health since the diagnostic and acute treatment periods. At the same time, most participants felt far from healthy, continued to spend significant time dealing with health issues, such as chronic graft-versus-host disease, and relied substantially on informal caregivers. Isolated from friends and social activities, participants equated this prolonged recovery period to “house arrest” and “prison,” with one elaborating by stating, “This is not the way I should be living.”
Self-care after HCT was a transitional process between sickness and wellness that occurred within the broader developmental phase between adolescence and adulthood. According to participants, independence and self-sufficiency were the major indicators of adulthood, but also inherent in health. As one participant stated, “Being healthy is just being able to function on your own.” Because participants associated health with self-sufficiency, the transition to self-care emerged as an important subprocess of an overarching developmental trajectory toward adulthood.
Most participants were in the early stages of emerging adulthood at cancer diagnosis. For example, some were finishing high school and headed to college, some were enrolled in college, and only two had graduated from college. Similarly, many were in intimate relationships of varying levels of commitment, but only one was married. Participants explained how a cancer diagnosis halted—and at times reversed—their developmental progress. One participant said,
Going off to college, I was like, “No. I don’t want my parents. I don’t need to talk to them.” I wanted freedom. I wanted adulthood. And then, getting the cancer, obviously I was like, “I want my mommy.”
For the emerging adults in this study, the notion of self-care was never removed from the developmental definition of independence.
Physical–Spatial Setbacks
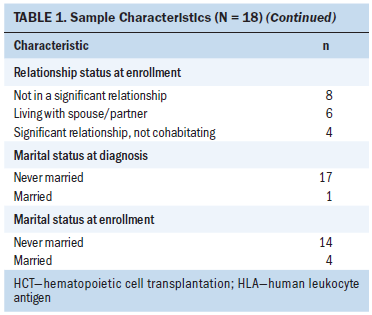
Progress toward self-care did not follow a linear trajectory of steady improvement over time. Instead, most participants reported an unpredictable recovery, punctuated with health-related setbacks, such as persistent issues or the emergence of late effects. Virtually all participants reported struggles with chronic health issues, including graft-versus-host disease, frequent infections, depression, anxiety, neurocognitive impairment, and cardiac, endocrine, and musculoskeletal dysfunction. One participant, who was 2.5 years post-HCT, had recently fractured her arm after falling at home and was “relying on [family] mostly 100% of the time now.” Another participant described the physical weakness that resulted after a five-week hospitalization for pneumonia requiring an induced coma. About five years post-HCT, one participant experienced avascular necrosis and underwent hip replacement. These unexpected, devastating digressions in their recovery directly contributed to feeling sicker and more dependent, creating physical barriers in their developmental progress toward independence.
Participants reported that an important aspect of independence related to personal space, as exemplified by moving out and living away from one’s family of origin—a common milestone during emerging adulthood. In this sample, at diagnosis, 11 participants were living with at least one parent, 5 lived near a college campus (typically with roommates), 1 lived with a spouse, and 1 lived alone but was considering cohabitation with his girlfriend. In most cases, participants’ parents paid for rent and living expenses. Following diagnosis and treatment, four participants described the necessity of moving back in with their families of origin for support, some bringing an intimate partner with them. Two participants were cohabitating with intimate partners but also had parents staying with them daily. According to participants, living with parents was helpful with respect to meal preparation, grocery shopping, housekeeping, and transportation, but involved trade-offs in control over their daily lives and the ability to make independent decisions.
Most participants accepted compromises in privacy during initial recovery related to their acute health needs. However, over time, the “hovering” of parents, the lack of alone time, and the infringement on personal space felt suffocating. One shared, “I was just getting frustrated with people being around me all the time. . . . I just felt like I was a child again.” Informal caregivers left for only brief periods, if at all, as one participant in her third year post-HCT described, “Probably like 30 minutes by myself, but they won’t leave me longer than that and they’re constantly calling me when they’re gone.” This confined existence left these AYAs with nowhere to vent, and many remarked that their typical outlets for stress, such as basketball, paintball, the shooting range, or socializing at happy hour, were off-limits because of disease-related restrictions. Despite the desire to move out on their own, most participants admitted that they still needed considerable support on a daily basis and did not feel ready for that step. A participant who requested “a weekend of alone time” in a hotel room panicked when she needed to take her medications and “ruined the whole thing by calling my dad at like 10 p.m. and being like, ‘Can you come sleep with me in the hotel room?’” Once participants moved back in with their parents, it became difficult to justify moving out again, both financially and in terms of health and safety.
Social Setbacks
The intensity of HCT required that participants rely on informal caregivers for support, but these interactions disrupted the social tasks of emerging adulthood, such as separating from their parents and exploring their identity through peer relationships. Participants engaged in a push-pull dynamic between accepting help and trying to retain aspects of autonomy they had established before diagnosis. Although participants understood that caregiver support was crucial to recovery, they felt highly uncomfortable relying so much on others, and many spoke of intentionally creating distance in their relationships.
Participants described various reasons for this reluctance to depend on people in their lives. They explained how relying on parents required sacrificing recent strides toward independence. However, they also admitted that parents offered more reliability, commitment, and perspective than other relationships, and, therefore, they found themselves depending on them even when relationship challenges existed. One participant blamed herself when her illness forced her divorced parents to interact, whereas another described how pre-illness conflicts with her mother intensified. Others struggled to overcome regressive behaviors once they needed less help. One participant explained how she reverted socially to her parents rather than friends when she resumed college.
On the other hand, entrusting caregiving responsibilities to friends, roommates, or intimate partners placed high demands on non-familial, less-committed relationships. These relationships were generally new and lighthearted, whereas a cancer diagnosis was a serious intrusion. One participant explained this excessive burden on his girlfriend, a graduate student who, he estimated, was spending 75% of her time caregiving; another described the disconnect between his concerns and those of his friends. In peer relationships, dependence created an uncomfortable imbalance and vulnerability that most participants wanted to avoid; as one remarked, “It’s not rainbows and lollipops.” Participants worried about intimate partners leaving them or staying with them out of pity or guilt. One participant offered her boyfriend an exit from the relationship, saying, “It’s okay if you want to break up with me. I totally understand. I don’t want to put any pressure on you.” In addition, peers were emerging adults themselves, and less able to provide financial support, insurance, or help in navigating the healthcare system.
Cognizant of the benefits and drawbacks to depending on parents and peers, most participants ultimately relied on multiple caregivers. As one explained, “It was a group effort.” This allowed participants to avoid relying totally on any single individual. Although these arrangements varied, participants depended on parents, relatives, intimate partners, and close friends in a collective fashion. One participant explained, “I can turn to one or the other based on my own needs.” Parents often traveled from other states to help; they tended to be most involved before and during acute HCT, handling practical, medical, and financial tasks. Meanwhile, intimate partners, siblings, close friends, and even a pet provided emotional support, distraction, and companionship, particularly in the post-HCT period.
Financial Setbacks
Financial independence is usually the final step in reaching adulthood. It was common for participants to have part-time jobs for spending money, but most relied financially on their parents to pay their living expenses before diagnosis and at the time of interviews. Participants perceived financial dependence on parents as normal for their age. One remarked, “I feel like I’m as independent now as anyone I know or as I would have been without my treatments.” Most participants had expected financial support from parents during college, but the added burden of substantial medical expenses set their circumstances apart from peers.
Participants identified the financial aspects of treatment, particularly out-of-pocket expenses and health insurance, as setbacks in their ability to achieve independence. Maintaining adequate health insurance was a significant stressor for almost all participants. One participant pointed out that the insurance offered by her employment did not cover laboratory costs, stating, “If I had to pay for labs out of pocket, I would have no money. There’s not enough money in the world to pay for that many labs.” Many differentiated the “good” insurance of their parents’ plans from basic coverage. Moving forward with a chronic illness, participants believed that good insurance was necessary for survival. They also connected the financial hardship of HCT to their life stage, explaining how the long-term consequences would impact their financial futures. One participant elaborated about how a cancer experience during emerging adulthood could result in financial ruin.
Key quotations that help to illustrate the health-related setbacks that are barriers to independence can be found in Figure 2.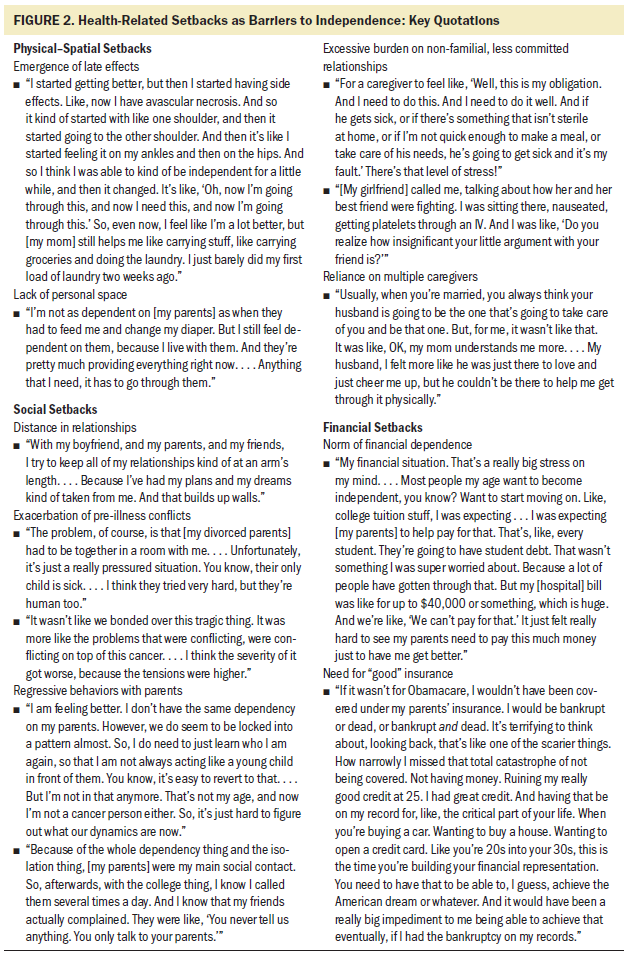
Discussion
The authors found that the transition to self-care after HCT among this sample of emerging adults was deeply connected to broader developmental processes. Persistent health needs after HCT resulted in physical, social, and financial setbacks that were perceived as threats to independence and self-sufficiency. These setbacks disrupted participants’ journey toward health and self-care, as well as the overarching developmental trajectory toward adulthood.
Emerging adults typically leave home and develop social connections outside of their family of origin (Arnett, 2014). Relationships with peers provide feelings of intimacy through support, companionship, and social activities, but often are carefree and exploratory in nature. For most participants, the intensity of HCT demanded that they remain or return to living with parents, contributing to feelings of extreme social isolation. Participants tended to grow closer to parents while struggling to connect with peers. The dynamics of caregiving after HCT have been fairly well-documented for younger and older groups. The pediatric literature has focused on parental caregivers (Forinder, Claesson, Szybek, & Lindahl Norberg, 2015; Lindahl Norberg, Mellgren, Winiarski, & Forinder, 2014; Rodday et al., 2012; Virtue et al., 2014); meanwhile, adult studies have reported on spousal caregivers (Cooke, Grant, Eldredge, Maziarz, & Nail, 2011; Langer, Yi, Storer, & Syrjala, 2010; Meehan et al., 2006; Sabo, McLeod, & Couban, 2013; Wilson, Eilers, Heermann, & Million, 2009). The current findings suggest that the strongly dyadic relationship portrayed in the pediatric and adult HCT research may not reflect the unique caregiving configurations of young adults. In contrast, the current sample saw dependence on caregivers as a threat to autonomy and tended to rely on multiple caregivers rather than any single person.
Although participants perceived financial dependence on parents as normal for their age, they expressed serious concerns about their future financial well-being. Young adults are particularly vulnerable to cancer-related financial toxicity, which is associated with adverse medical and psychosocial outcomes (Landwehr, Watson, Macpherson, Novak, & Johnson, 2016). Cancer during this life stage can threaten future employability, potential earnings, career development, and access to health insurance (Guy et al., 2014). In addition to high out-of-pocket costs, emerging adults with cancer face increased risk for bankruptcy (Ramsey et al., 2013) and are more likely to forego medical care related to cost when compared to older groups or age-matched peers (Kirchhoff, Lyles, Fluchel, Wright, & Leisenring, 2012; Weaver, Rowland, Bellizzi, & Aziz, 2010).
Much of this financial vulnerability can be attributed to the instability of health insurance opportunities in the U.S., particularly for individuals who are not employed and have a preexisting condition. Among AYAs with cancer, lack of insurance has been linked to delays in diagnosis (Martin et al., 2007), delays in receiving treatment (Burg et al., 2010), and decreased survival (Kent, Sender, Largent, & Anton-Culver, 2009). Prior to the passage of the Patient Protection and Affordable Care Act (ACA), young adults were the most underinsured age group and about two of five young adults were without health insurance (Collins, Robertson, Garber, & Doty, 2012). Recently, the ACA has enhanced opportunities for 5.7 million young adults to obtain health coverage through a consumer-based marketplace, expanding state Medicaid, prohibiting the denial of coverage for preexisting conditions, and extending eligibility of children on parental plans until age 26 (Guy et al., 2014; Landwehr et al., 2016). Consistent with preliminary evaluations of this policy, the findings suggest that the dependent care provision of the ACA was critical to accessing adequate insurance for emerging adults with cancer (Parsons, Schmidt, Tenner, Bang, & Keegan, 2016). Of note, the study coincided with the aftermath of the 2008 economic recession, which may have influenced the findings. Nevertheless, the tenuous position of the ACA in the current political climate has serious implications for young adults across the cancer continuum (Obama, 2017).
Implications for Nursing
The current findings have implications for clinical practice, future research, and policy. Health-related setbacks after HCT are common (Bhatia, 2014; Luskin, Banerjee, Del Percio, & Loren, 2015). It is critical for nurses and other clinicians to recognize that these setbacks can result in significant and prolonged developmental disruptions for emerging adults by threatening progress toward independence and successful attainment of adulthood. Nurses in a variety of settings may have contact with young adult survivors of HCT. In these interactions, an important aspect of patient-centered care may be prioritizing opportunities for independence when developing goals and care plans, such as advising on appropriate periods of alone time. A key finding from this study was participants’ reliance on multiple informal caregivers rather than single individuals. Recognizing that these caregiver arrangements may change over time as the young adult’s life circumstances evolve is necessary. Healthcare providers should also routinely screen for distress and assess for dysfunction in these relationships.
Young adults face significant financial hardship after HCT. In accordance with the National Comprehensive Cancer Network’s guidelines (Coccia et al., 2012), financial counseling is considered an essential component of AYA cancer care to address immediate medical expenses, avoid medical debt and bankruptcy, and prepare financially for the future. Financial counselors can function as part of an interprofessional AYA oncology team; in settings without specific AYA services, nurses and other providers should be able to initiate financial discussions with young adult patients and connect them to resources. For example, nurses can refer patients to websites such as Critical Mass Mission Control, a searchable, continuously updated database for young adults with cancer, to identify a wide range of local and national resources (https://criticalmass.org). Future research should focus on the development of interventions tailored to the needs of emerging adults to improve management of long-term and late effects and reduce the impact of these often unavoidable setbacks. In addition, longitudinal research is needed to track financial outcomes of young adult survivors and identify protective and risk factors. On a macro level, policies that ensure access to adequate and affordable health insurance and minimize the immense financial burden of cancer on AYA survivors should be prioritized.
Limitations
Although this study is among the first to explore the experiences of AYAs after HCT, several limitations exist. The generalizability of the study results to the larger population of AYAs after HCT is limited given the qualitative study design, purposive sampling technique, small sample size, the inclusion of participants who were less than one year post-HCT, and the fact that all participants had survived and were currently in remission. In addition, the findings are limited to the experiences of AYAs treated at a single, specialized institution.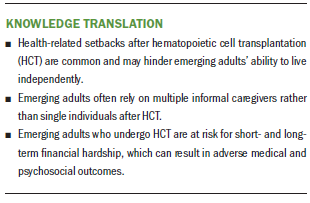
Conclusion
The interest in AYAs with cancer has increased, but major gaps in current research and clinical knowledge remain (Nass et al., 2015; Smith et al., 2016). In this article, the lens of emerging adulthood provided insight into the broader developmental impact of the cancer experience. Taking care of oneself—physically, socially, and financially—is at the crux of the definition of adulthood. However, young people requiring HCT during the transition to adulthood face substantial challenges in achieving this important developmental milestone. Better understanding of the consequences of health-related setbacks will help nurses and other clinicians support transition to self-care and enhance overall development among emerging adult HCT survivors.
The authors gratefully acknowledge Julie Wolfson, MD, MSHS, Saro Armenian, DO, MPH, Stephen Forman, MD, Lindsey Hageman, MPH, Alysia Bosworth, BA, and Laura Gustafson, BS, for their administrative support of this project.
About the Author(s)
Eden R. Brauer, PhD, RN, is a postdoctoral fellow in the School of Public Health and the Jonsson Comprehensive Cancer Center, Huibrie C. Pieters, PhD, DPhil, RN, is an associate professor in the School of Nursing, and Patricia A. Ganz, MD, is a professor in the Schools of Medicine and Public Health, all at the University of California, Los Angeles; Wendy Landier, PhD, CRNP, FAAN, is an associate professor in the School of Medicine at the University of Alabama in Birmingham; and Carol Pavlish, PhD, RN, FAAN, and MarySue V. Heilemann, PhD, RN, are associate professors in the School of Nursing at the University of California, Los Angeles. This research was funded by a dissertation research grant from the ONS Foundation and the National Institutes of Health/National Institute of Nursing Research Ruth L. Kirschstein National Research Service Award and Institutional Research Training Grant (T32 NR 07077). Brauer completed the data collection and provided statistical support. Brauer, Pieters, Ganz, Landier, and Heilemann provided the analysis. All authors contributed to the conceptualization and design and the manuscript preparation. Brauer can be reached at ebrauer@ucla.edu, with copy to ONFEditor@ons.org. (Submitted June 2017. Accepted August 3, 2017.)
References
Arnett, J.J. (2004). Emerging adulthood: The winding road from the late teens through the twenties. New York, NY: Oxford University Press.
Arnett, J.J. (2014). Emerging adulthood: The winding road from the late teens through the twenties. (2nd ed.). New York, NY: Oxford University Press.
Baker, K.S., Armenian, S., & Bhatia, S. (2010). Long-term consequences of hematopoietic stem cell transplantation: Current state of the science. Biology of Blood and Marrow Transplantation, 16(Suppl. 1), S90–S96. https://doi.org/10.1016/j.bbmt.2009.09.017
Bhatia, S. (2014). Caring for the long-term survivor after allogeneic stem cell transplantation. Hematology, 2014, 495–503. https://doi.org/10.1182/asheducation-2014.1.495
Blatterer, H. (2007). Contemporary adulthood: Reconceptualizing an uncontested category. Current Sociology, 55, 771–792. https://doi.org/10.1177/0011392107081985
Blumer, H. (1954). What is wrong with social theory? American Sociological Review, 18, 3–10.
Brauer, E.R., Pieters, H.C., Ganz, P.A., Landier, W., Pavlish, C., & Heilemann, M.V. (2017). “From snail mode to rocket ship mode”: Adolescents and young adults’ experiences of returning to work and school after hematopoietic cell transplantation. Journal of Adolescent and Young Adult Oncology, 6, 551–559. https://doi.org/10.1089/jayao.2017.0025
Bukowinski, A.J., Burns, K.C., Parsons, K., Perentesis, J.P., & O’Brien, M.M. (2015). Toxicity of cancer therapy in adolescents and young adults (AYAs). Seminars in Oncology Nursing, 31, 216–226. https://doi.org/10.1016/j.soncn.2015.05.003
Burg, M.A., Zebrack, B., Walsh, K., Maramaldi, P., Lim, J.W., Smolinski, K.M., & Lawson, K. (2010). Barriers to accessing quality health care for cancer patients: A survey of members of the association of oncology social work. Social Work in Health Care, 49, 38–52. https://doi.org/10.1080/00981380903018470
Charmaz, K. (2014). Constructing grounded theory (2nd ed.). London, UK: Sage.
Coccia, P.F., Altman, J., Bhatia, S., Borinstein, S.C., Flynn, J., George, S., . . . Shead, D.A. (2012). Adolescent and young adult oncology. Clinical practice guidelines in oncology. Journal of the National Comprehensive Cancer Network, 10, 1112–1150.
Collins, S.R., Robertson, R., Garber, T., & Doty, M.M. (2012). Young, uninsured, and in debt: Why young adults lack health insurance and how the Affordable Care Act is helping. Retrieved from http://www.commonwealthfund.org/Publications/Issue-Briefs/2012/Jun/Youn…
Cooke, L., Grant, M., Eldredge, D.H., Maziarz, R.T., & Nail, L.M. (2011). Informal caregiving in hematopoietic blood and marrow transplant patients. European Journal of Oncology Nursing, 15, 500–507. https://doi.org/10.1016/j.ejon.2011.01.007
Corbin, J., & Strauss, B.G. (2015). Basics of qualitative research: Techniques and procedures for developing grounded theory (4th ed.). Thousand Oaks, CA: Sage.
Forinder, U., Claesson, L., Szybek, K., & Lindahl Norberg, A. (2015). Exploring the content of post-traumatic stress symptoms among parents after paediatric stem cell transplant. PLOS ONE, 10, e0126905. https://doi.org/10.1371/journal.pone.0126905
Guy, G.P., Jr., Yabroff, K.R., Ekwueme, D.U., Smith, A.W., Dowling, E.C., Rechis, R., . . . Richardson, L.C. (2014). Estimating the health and economic burden of cancer among those diagnosed as adolescents and young adults. Health Affairs, 33, 1024–1031. https://doi.org/10.1377/hlthaff.2013.1425
Howlader, N., Noone, A.M., Krapcho, M., Miller, D., Bishop, K., Altekruse, S.F., . . . Cronin, K.A. (Eds.). (2016). SEER cancer statistics review, 1975–2013. Bethesda, MD: National Cancer Institute. Retrieved from http://seer.cancer.gov/csr/1975_2013/
Katz, A. (2015). Meeting the need for psychosocial care in young adults with cancer. Pittsburgh, PA: Oncology Nursing Society.
Kent, E.E., Parry, C., Montoya, M.J., Sender, L.S., Morris, R.A., & Anton-Culver, H. (2012). “You’re too young for this”: Adolescent and young adults’ perspectives on cancer survivorship. Journal of Psychosocial Oncology, 30, 260–279. https://doi.org/10.1080/07347332.2011.644396
Kent, E.E., Sender, L.S., Largent, J.A., & Anton-Culver, H. (2009). Leukemia survival in children, adolescents, and young adults: Influence of socioeconomic status and other demographic factors. Cancer Causes and Control, 20, 1409–1420. https://doi.org/10.1007/s10552-009-9367-2
Kirchhoff, A.C., Lyles, C.R., Fluchel, M., Wright, J., & Leisenring, W. (2012). Limitations in health care access and utilization among long-term survivors of adolescent and young adult cancer. Cancer, 118, 5964–5972. https://doi.org/10.1002/cncr.27537
Landwehr, M.S., Watson, S.E., Macpherson, C.F., Novak, K.A., & Johnson, R.H. (2016). The cost of cancer: A retrospective analysis of the financial impact of cancer on young adults. Cancer Medicine, 5, 863–870. https://doi.org/10.1002/cam4.657
Langer, S.L., Yi, J.C., Storer, B.E., & Syrjala, K.L. (2010). Marital adjustment, satisfaction and dissolution among hematopoietic stem cell transplant patients and spouses: A prospective, five-year longitudinal investigation. Psycho-Oncology, 19, 190–200. https://doi.org/10.1002/pon.1542
Lindahl Norberg, A., Mellgren, K., Winiarski, J., & Forinder, U. (2014). Relationship between problems related to child late effects and parent burnout after pediatric hematopoietic stem cell transplantation. Pediatric Transplantation, 18, 302–309. https://doi.org/10.1111/petr.12228
Luskin, M.R., Banerjee, R., Del Percio, S., & Loren, A.W. (2015). A pound of cure requires an ounce (or more) of prevention: Survivorship and complications of therapy for hematologic malignancies. Current Hematologic Malignancy Reports, 10, 225–236. https://doi.org/10.1007/s11899-015-0274-1
Majhail, N.S., & Rizzo, J.D. (2013). Surviving the cure: Long term followup of hematopoietic cell transplant recipients. Bone Marrow Transplantation, 48, 1145–1151. https://doi.org/10.1038/bmt.2012.258
Martin, S., Ulrich, C., Munsell, M., Taylor, S., Lange, G., & Bleyer, A. (2007). Delays in cancer diagnosis in underinsured young adults and older adolescents. Oncologist, 12, 816–824. https://doi.org/10.1634/theoncologist.12-7-816
Meehan, K.R., Fitzmaurice, T., Root, L., Kimtis, E., Patchett, L., & Hill, J. (2006). The financial requirements and time commitments of caregivers for autologous stem cell transplant recipients. Journal of Supportive Oncology, 4, 187–190.
Mulye, T.P., Park, M.J., Nelson, C.D., Adams, S.H., Irwin, C.E., Jr., & Brindis, C.D. (2009). Trends in adolescent and young adult health in the United States. Journal of Adolescent Health, 45, 8–24. https://doi.org/10.1016/j.jadohealth.2009.03.013
Nass, S.J., Beaupin, L.K., Demark-Wahnefried, W., Fasciano, K., Ganz, P.A., Hayes-Lattin, B., . . . Smith, A.W. (2015). Identifying and addressing the needs of adolescents and young adults with cancer: Summary of an Institute of Medicine workshop. Oncologist, 20, 186–195. https://doi.org/10.1634/theoncologist.2014-0265
National Cancer Institute. (2015). Adolescents and young adults with cancer. Retrieved from https://www.cancer.gov/types/aya
Obama, B.H. (2017). Repealing the ACA without a replacement—The risks to American health care. New England Journal of Medicine, 376, 297–299. https://doi.org/10.1056/NEJMp1616577
Parsons, H.M., Schmidt, S., Tenner, L.L., Bang, H., & Keegan, T.H. (2016). Early impact of the Patient Protection and Affordable Care Act on insurance among young adults with cancer: Analysis of the dependent insurance provision. Cancer, 122, 1766–1773. https://doi.org/10.1002/cncr.29982
Phillips-Salimi, C.R., Lommel, K., & Andrykowski, M.A. (2012). Physical and mental health status and health behaviors of childhood cancer survivors: Findings from the 2009 BRFSS survey. Pediatric Blood and Cancer, 58, 964–970. https://doi.org/10.1002/pbc.23359
Ramsey, S., Blough, D., Kirchhoff, A., Kreizenbeck, K., Fedorenko, C., Snell, K., . . . Overstreet, K. (2013). Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Affairs, 32, 1143–1152. https://doi.org/10.1377/hlthaff.2012.1263
Rodday, A.M., Pedowitz, E.J., Mayer, D.K., Ratichek, S.J., Given, C.W., & Parsons, S.K. (2012). Parental caregiving of children prior to hematopoietic stem cell transplant. Research in Nursing and Health, 35, 328–339. https://doi.org/10.1002/nur.21485
Sabo, B., McLeod, D., & Couban, S. (2013). The experience of caring for a spouse undergoing hematopoietic stem cell transplantation: Opening Pandora’s box. Cancer Nursing, 36, 29–40. https://doi.org/10.1097/NCC.0b013e31824fe223
Smith, A.W., Seibel, N.L., Lewis, D.R., Albritton, K.H., Blair, D.F., Blanke, C.D., . . . Zebrack, B.J. (2016). Next steps for adolescent and young adult oncology workshop: An update on progress and recommendations for the future. Cancer, 122, 988–999. https://doi.org/10.1002/cncr.29870
Sun, C.L., Francisco, L., Baker, K.S., Weisdorf, D.J., Forman, S.J., & Bhatia, S. (2011). Adverse psychological outcomes in long-term survivors of hematopoietic cell transplantation: A report from the Bone Marrow Transplant Survivor Study (BMTSS). Blood, 118, 4723–4731. https://doi.org/10.1182/blood-2011-04-348730
Sun, C.L., Francisco, L., Kawashima, T., Leisenring, W., Robison, L.L., Baker, K.S., . . . Bhatia, S. (2010). Prevalence and predictors of chronic health conditions after hematopoietic cell transplantation: A report from the Bone Marrow Transplant Survivor Study. Blood, 116, 3129–3139. https://doi.org/10.1182/blood-2009-06-229369
Virtue, S.M., Manne, S.L., Mee, L., Bartell, A., Sands, S., Gajda, T.M., & Darabos, K. (2014). Psychological distress and psychiatric diagnoses among primary caregivers of children undergoing hematopoietic stem cell transplant: An examination of prevalence, correlates, and racial/ethnic differences. General Hospital Psychiatry, 36, 620–626. https://doi.org/10.1016/j.genhosppsych.2014.08.010
Weaver, K.E., Rowland, J.H., Bellizzi, K.M., & Aziz, N.M. (2010). Forgoing medical care because of cost: Assessing disparities in healthcare access among cancer survivors living in the United States. Cancer, 116, 3493–3504.
Wilson, M.E., Eilers, J., Heermann, J.A., & Million, R. (2009). The experience of spouses as informal caregivers for recipients of hematopoietic stem cell transplants. Cancer Nursing, 32, E15–E23. https://doi.org/10.1097/NCC.0b013e31819962e0
Wood, W.A., & Lee, S.J. (2011). Malignant hematologic diseases in adolescents and young adults. Blood, 117, 5803–5815. https://doi.org/10.1182/blood-2010-12-283093
Zebrack, B.J. (2011). Psychological, social, and behavioral issues for young adults with cancer. Cancer, 117, 2289–2294. https://doi.org/10.1002/cncr.26056




