Symptoms and Self-Management Strategies Identified by Children With Cancer Using Draw-and-Tell Interviews
Purpose: This cross-sectional study described how school-aged children with cancer represent their symptoms and associated characteristics using draw-and-tell interviews.
Participants & Setting: 27 children aged 6–12 years receiving treatment for cancer at the Cancer Transplant Center at Primary Children’s Hospital, a tertiary pediatric hospital in Salt Lake City, Utah.
Methodologic Approach: Children participated in draw-and-tell interviews while completing drawings depicting days when they felt well and days when they felt sick. Children’s drawings and accompanying explanations were analyzed qualitatively.
Findings: Children’s drawings related symptoms and the strategies children used to self-manage those symptoms. Nausea, fatigue, pain, and sadness were the most frequently reported symptoms. Strategies to manage symptoms most often included physical and psychosocial care strategies.
Implications for Nursing: Children with cancer were able to relate detailed descriptions of their symptoms and symptom self-management strategies when presented with developmentally sensitive approaches. Healthcare providers are well positioned to integrate arts-based approaches to symptom assessment and to support children in implementing their preferred strategies to alleviate symptoms.
Jump to a section
More than 10,000 children aged younger than 15 years are diagnosed with cancer in the United States each year (Siegel, Miller, & Jemal, 2018). These children are developmentally diverse, ranging from pre-verbal infants to young adolescents with the capacity to think abstractly. Children’s developmental abilities also influence the manner in which they articulate and respond to their symptoms (Linder, 2008). Although children as young as four years old are recognized as being capable of providing self-report their symptoms, resources to support children in relating their symptom experiences are limited.
Elementary school–aged children, those aged 6–12 years, are developing the ability to represent events mentally and symbolically. Maturing reasoning abilities allow children to form relationships between things and ideas, as well as to think through actions and anticipated consequences (Rodgers, 2011). In contrast to adults, who tend to use external, verbal cues to recall information, children tend to recall and communicate information through internal cues, which are supported through activities that involve the use of the senses. The majority of resources for eliciting children’s self-report, including self-report of symptoms, however, are based on adult versions of tools that rely on external, verbal prompts for recall of information. In addition, these self-report tools provide limited opportunity to explore children’s perspectives of the context in which they are experiencing symptoms and the meanings they attach to their symptoms. Alternative approaches to obtain an understanding of children’s experiences to inform clinical interventions are needed.
Symptoms in Children With Cancer
Challenges in understanding children’s symptom experiences are evident in qualitative and quantitative studies. Many of these studies have included relatively small sample sizes of children and adolescents, limiting the opportunity to delineate experiences and perspectives of younger children from those of adolescents.
Qualitative interviews have allowed children as young as four years old to relate their cancer experiences (Woodgate & Degner, 2003). Children frequently described the presence of multiple symptoms as “I feel really weird” or “I feel sore and hurting” (Woodgate, 2008). Such descriptions, which align with children’s developmental abilities, may be difficult for healthcare providers—and even parents—to interpret. Younger children also related frustration with multiple quantitative rating scales. Allowing children to relate their symptoms within the larger experience of cancer facilitated greater understanding of the meaning children attached to their symptoms (Woodgate, Degner, & Yanofsky, 2003).
Quantitative studies involving self-report scales also limit a full understanding of the child’s experience, particularly that of children aged younger than 10 years. Although validated tools for assessing fatigue (Hinds et al., 2010; Hockenberry et al., 2003), nausea (Dupuis, Taddio, Kerr, Kelly, & MacKeigan, 2006), and pain (von Baeyer, 2006) are available for children as young as seven years old, multisymptom assessment scales are limited.
The nine-item Memorial Symptom Assessment Scale in children aged 7–12 years (Collins et al., 2002) has facilitated the recruitment of younger children. Children and adolescents using this scale, however, reported fewer symptoms (Linder, Al-Qaaydeh, & Donaldson, 2018; Walker, Gedaly-Duff, Miaskowski, & Nail, 2010) than those using more extensive multisymptom scales (Baggott et al., 2010; Miller, Jacob, & Hockenberry, 2011; Williams et al., 2012). Regardless of the scale used, however, the most frequently reported symptoms included nausea, fatigue, pain, and changes in appetite. Of note, Linder et al. (2018) found that about one-third of participants reported a response to the item “Did anything else make you feel bad or sick?” on at least one occasion during a three-day data collection period. Responses were varied and included psychosocial aspects of hospitalization, the hospital environment, physical symptoms, and aspects of physical care and treatment. These “other” symptoms were among the top five most severe and most distressing symptoms, highlighting the importance of providing developmentally meaningful mechanisms for children to communicate aspects of the symptom experience that are of priority to them.
Symptom Self-Management
Self-management is a dynamic, iterative process by which individuals with chronic illness integrate strategies that allow them to cope with their illness and its symptoms in the context of their day-to-day lives (Miller, Lasiter, Bartlett Ellis, & Buelow, 2015). Self-management requires individuals to evaluate their health status and then implement interventions. The changing nature of children’s symptoms further adds to the challenge of self-management. Coping, a related aspect of illness and symptom experiences, emphasizes internal management, including thoughts and behaviors individuals use to respond to stressors (Audulv, Packer, Hutchinson, Roger, & Kephart, 2016).
Symptom self-management strategies reported by children themselves include sleeping, both for rest and to provide a mental reprieve, and taking medicine (Woodgate & Degner, 2003). School-aged children reported more frequent use of active coping strategies, including distraction, emotional regulation, and problem solving, rather than passive strategies to manage chemotherapy-induced nausea and vomiting (Rodgers et al., 2012). Active strategies were also perceived as more effective. In contrast, passive strategies, such as avoidant or emotion-focused strategies, may support coping with medical procedures (Aldridge & Roesch, 2007). More research is needed to understand the context in which children use specific strategies and long-term outcomes of those strategies.
Arts-Based Approaches
Arts-based approaches, including drawing, provide an alternative to traditional paper-and-pencil–based tools and support recall of information in a developmentally meaningful manner (Driessnack & Furukawa, 2012). Drawing-based approaches with children have been widely used in research and clinical settings by psychology and child life professionals (Gross & Hayne, 1998; Malchiodi, 1998). Drawing supports not only children’s description of the experience, but also their larger interpretation and explanation of the context in which the experience is occurring. Children with sickle cell disease and asthma have used drawings to communicate their symptoms (Gabriels, Wamboldt, McCormick, Adams, & McTaggart, 2000; Stefanatou & Bowler, 1997). Children’s drawings have also demonstrated sensitivity to change over time in relating headache symptoms (Stafstrom, Goldenholz, & Dulli, 2005). More recently, drawing-based approaches have been used in children with cancer to explore existential challenges during treatment (Woodgate, West, & Tailor, 2014) and to reduce anxiety during hospitalization (Altay, Kilicarslan-Toruner, & Sari, 2017).
Purpose
The purpose of this study was to describe how school-aged children with cancer perceive and represent their symptoms and their associated characteristics using draw-and-tell interviews, an arts-based approach (Driessnack, 2006). The study was grounded in a developmental science framework that recognizes a continuous interaction of multiple aspects of the individual’s development (e.g., biologic, physiologic, behavioral, emotional, cognitive, perceptual) in the context of his or her environment (Magnusson, 2000; Miles & Holditch-Davis, 2003). As the study proceeded, the study team found that many children not only related their symptoms, but also depicted the strategies they used to manage their symptoms.
Methods
Design
This cross-sectional, exploratory, descriptive study used participatory methods guided by the contextual inquiry phase of the cooperative inquiry process (Druin, 1999). Results of this study are part of a larger study that is engaging school-age children with cancer and pediatric oncology healthcare providers in the co-design of a mobile technology–based resource for symptom assessment. The cooperative inquiry process engages users as participants in the design process. The first phase of the cooperative inquiry process is contextual inquiry, which is grounded in field research and supports active participation of research participants throughout the study process. This phase also emphasizes the role of the research team in observing and analyzing participants’ responses and patterns of activity.
Sample and Setting
Participants were recruited from an inpatient oncology unit and ambulatory oncology clinic of the Cancer Transplant Center at Primary Children’s Hospital, a tertiary free-standing children’s hospital in Salt Lake City, Utah. Eligible children were aged 6–12 years and receiving treatment for cancer. Children receiving treatment for either a primary diagnosis of cancer or relapsed/refractory disease were eligible. Children were required to speak and understand English and be physically and cognitively capable of completing study-related activities. Children with major cognitive developmental disabilities were excluded. Because the study was exploratory in its scope, children were heterogeneous with regard to diagnosis and stage of treatment.
Procedure
Institutional review board approval was granted by the University of Utah. Participants were recruited from March 2015 to January 2016. Eligible patients and families were initially approached by an oncology team member to elicit interest in the study. A research team member then met with families to explain study procedures. Written parental permission was obtained for all participants. Children aged 7–12 years provided written assent; children aged six years provided verbal assent. Research team members reviewed the medical records of enrolled participants to identify demographic and clinical data to describe the study sample.
The draw-and-tell interview is a developmentally sensitive approach to data collection (Driessnack, 2006). This approach emphasizes the drawing and what the child says about the drawing. By drawing first and then relating their accompanying explanations, this process fosters children’s recall and communication of their experiences, which supports a greater understanding of the child’s associated interpretation and meaning, including the context of the experience, that cannot be obtained from interviews or traditional quantitative measures (Butler, Gross, & Hayne, 1995; Gross, Hayne, & Drury, 2008).
Children participated in draw-and-tell interviews during the course of a scheduled ambulatory clinic visit or inpatient admission. They received a packet of art supplies with a sketch tablet, crayons, colored pencils, markers, pencils, and stickers that they were permitted to keep at the conclusion of the interview. Parents were allowed to remain with the child during the interviews. Parents’ presence did not interfere with study-related activities.
Participants provided pictures of themselves to relate days when they were feeling well and days when they were feeling sick. As children completed the pictures, research team members used a semistructured interview guide to facilitate participants’ explanation of their pictures and to record detailed notes of the interview. Participants were first asked to explain each picture. Specific attention was given to commonly reported symptoms based on published literature while allowing participants to relate other symptoms that were of priority to them. Research team members also asked clarifying follow-up questions based on participants’ responses to validate understanding of the children’s response and to clarify the meaning of the language children used in describing a given symptom or feeling associated with that symptom. For example, one participant was able to further articulate that the expression that his “tummy feels sick” could relate to either pain or nausea; whereas other children were not able to further describe expressions of “stomachache.”
With the exception of one participant, children completed study-related activities without difficulty during the course of a routinely scheduled ambulatory clinic visit or afternoon of a scheduled inpatient admission. Because of progressive tiredness during the course of the clinic visit, one participant provided only brief explanations of her drawings.
Data Management
Demographic and clinical data were entered electronically using REDCap (Research Electronic Data Capture) tools hosted at the University of Utah (Harris et al., 2009). Data were then exported into IBM SPSS Statistics for analysis. Qualitative data were organized into Microsoft® Excel and IBM SPSS Statistics files to support descriptive summaries and content analysis procedures.
Analysis Procedures
Demographic and clinical data were summarized using descriptive statistics. Symptoms and self-management strategies were also summarized descriptively. Independent samples t tests explored differences in the number of reported symptoms and self-management strategies based on gender and age (i.e., younger [aged 6–8 years] versus older [aged 9–12 years] children).
Qualitative content analysis procedures were used to organize symptoms and self-management strategies into common categories and themes (Elo & Kyngäs, 2008). Participants’ drawings and accompanying interview notes were reviewed independently by at least two research team members to identify symptoms and symptom self-management strategies reported by each child. Pictures depicting days when children were feeling well and when children were feeling sick were reviewed. Team members then met to resolve discrepancies. Symptoms and self-management strategies that were depicted in participants’ drawings and reported in the interviews were included.
A coding scheme was developed to organize reported symptoms into categories using participants’ expressions and associated explanations of their symptoms. For example, the expression “feeling tired” was categorized as “fatigue,” and “feeling queasy” was categorized as “nausea.” Categories were then organized into subthemes and themes. This analytical process was also applied to participants’ self-management strategies. Participants’ drawings and accompanying explanations were further examined with regard to the context in which symptoms were occurring and the impact of symptoms on day-to-day life.
Results
Participants
Demographic characteristics are summarized in Table 1. The study sample consisted of 27 children receiving treatment for cancer. Participants were a mean age of 9.16 years (SD = 1.9, range = 6.33–12.83) and were a median of 9 months from their initial diagnosis of cancer (range = 1–93). The accrual rate for the study was 90%, with three children declining to participate. Reasons for non-participation included “don’t feel like it” and “really don’t want to.” 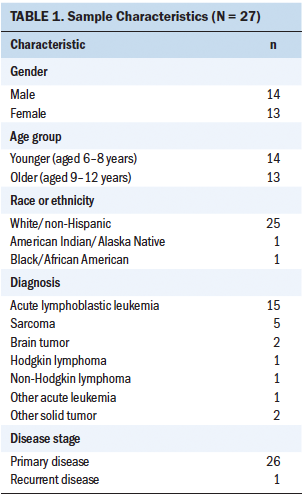
Symptoms
Table 2 summarizes symptoms reported by children through their drawings and accompanying explanations. This table also presents the reported frequencies of each symptom category and their organization into subthemes. 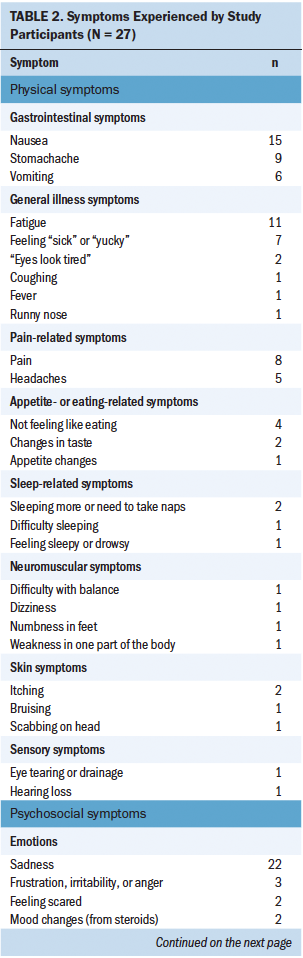
Participants identified 26 different physical symptoms and 11 different psychosocial symptoms. Three children also related challenges with taking oral medications. Participants reported a median of four symptoms (range = 2–11). This included a median of three physical symptoms (range = 1–7) and one psychosocial symptom (range = 0–4). Independent samples t tests did not identify differences in the total number of symptoms reported based on gender (t = –0.73, p = 0.47). Likewise, the total number of symptoms reported by younger children (aged 6–8 years) did not differ from the number reported by older children (aged 9–12 years) (t = –0.73, p = 0.47). The number of physical and psychosocial symptoms also did not differ based on gender or age group. Although all children included symptoms on their drawings depicting days they were feeling sick, two girls included symptoms on days they were feeling well.
Among physical symptoms, gastrointestinal symptoms (i.e., nausea and stomachache) predominated, followed by general illness symptoms (i.e., fatigue and “feeling yucky”). Pain-related symptoms were reported by 12 children. Of note, the experience of headaches (n = 5) was distinguished from other sources of pain. Appetite-related symptoms (n = 7) and sleep-related symptoms (n = 4) were also among the most common physical symptoms.
Emotions predominated as psychosocial symptoms, with sadness (n = 22) being most frequently depicted. Children’s pictures also depicted a sense of isolation (n = 3) and self-esteem changes (n = 2).
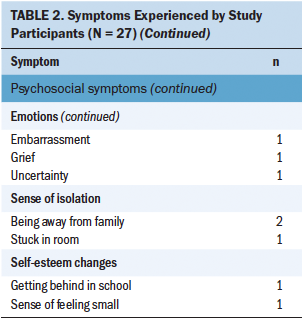
Symptom Self-Management Strategies
Twenty-two children related 21 different strategies (see Table 3) that they used to manage their symptoms. These children related a median of three symptom self-management strategies (range = 1–6). The number of reported strategies did not differ based on gender (t = –0.33, p = 0.75) or age group (t = –0.45, p = 0.66). All children described symptom self-management strategies specific to days when they were not feeling well; however, six children (four girls and two boys) also drew symptom self-management strategies specific to days when they were feeling well. 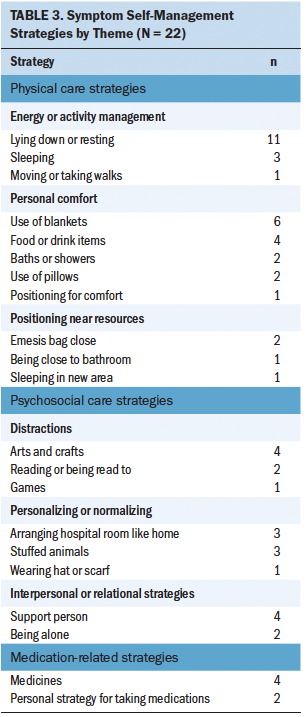
Children’s symptom self-management strategies were further organized into six subthemes and three themes. Themes included physical care strategies, psychosocial care strategies, and medication-related strategies. Physical care strategies predominated, with efforts to manage their energy balance (n = 15) and personal comfort strategies (n = 15) most often depicted. Lying down and resting was the most frequently reported strategy overall (n = 11). The most frequently depicted psychosocial care strategies included children’s use of distractions (n = 7) and their efforts to personalize and normalize their situation (n = 7). Medication-related strategies were taking a given medication to help relieve a symptom (n = 4) and specific strategies for taking the medication (n = 2).
Depiction of Symptoms and Symptom Self-Management Strategies
Children’s drawings illustrated the complexity of the symptom experience and the experience of multiple physical and psychosocial symptoms. Their drawings also illustrated the common, yet very personal, experiences of children receiving treatment for cancer. A seven-year-old girl with leukemia illustrated the experience of stomachache, fevers, and procedural pain associated with asparaginase injections. Her profound sadness at separation from her younger sister and the grief in response to a friend’s death from leukemia also affected the flowers in her environment (see Figure 1).
Children frequently depicted their symptoms and the strategies they used to manage their symptoms in the context of how symptoms affected their day-to-day lives. Even if children did not name a specific self-management strategy, the drawings of days when they were feeling sick frequently depicted themselves as lying down or reclining, feeling sad, and not being able to engage in their usual activities. A seven-year-old boy with leukemia related “feeling sad because I’m not at home, feeling sick, have to take pills, lots of pills” and being “stuck in my room for days” about his symptom experience associated with getting methotrexate in the inpatient setting. On days when he feels sick, an eight-year-old boy with leukemia related feeling “sad and droopy” and “[I] don’t like it.” He related having “no energy,” feeling “tired,” and that his “head hurts,” which cause him to “stay in bed” or “lie down on the couch with a blanket.” Other children depicted the need to position themselves near a bathroom or to keep an emesis bag within reach. 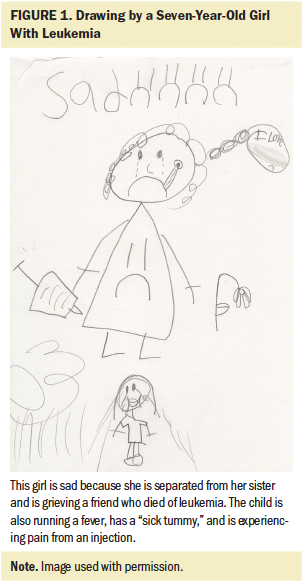
Some children depicted how their self-management strategies helped them engage in normalizing activities or prevent symptoms. An eight-year-old girl with a liver tumor depicted how support from a hospital volunteer helped her manage the consequences of her cisplatin-induced hearing loss (see Figure 2). On days when Hospital Bingo was broadcast over the hospital’s closed-circuit television system, the volunteer would come to her room to repeat the words that had been spoken. He also would call in jokes (an activity that is part of Hospital Bingo) on her behalf so that she could fully participate like any other child in the hospital. 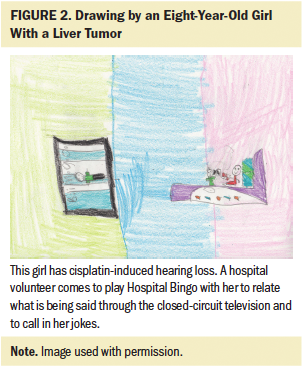
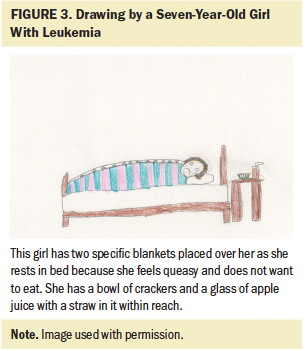
Many children were very deliberate and detailed in drawing and describing their symptom self-management strategies. A seven-year-old girl with leukemia drew a picture that included the two blankets she placed over herself when lying in bed, as well as the bowl of crackers on her nightstand and the glass of apple juice with a straw in it to help manage her nausea and not feeling like eating (see Figure 3).
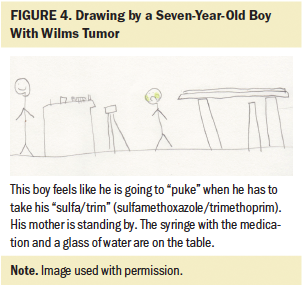
A seven-year-old boy with Wilms tumor was very detailed in depicting the multiple glasses of water he needed to take his syringe of “sulfa/trim” (sulfamethoxazole/trimethoprim) and the nausea he experienced when taking this medication (see Figure 4).
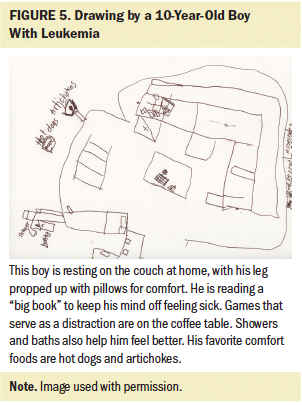
A 10-year-old boy with leukemia depicted himself in his family room, which was laid out much like a map, with different self-management strategies accessible to him. These included reading a “big book” that has a lot of things he can think about when he is sad, propping his hurting leg on pillows while reclining on the couch, playing his favorite games on the coffee table, and taking a shower to help him feel better. He added that he likes steamed artichokes and hot dogs but that “sometimes I don’t like to eat if my stomach feels sick” (see Figure 5).
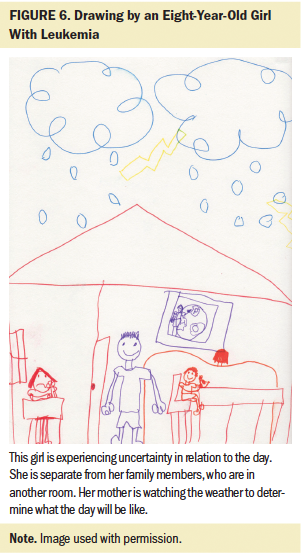
Some children’s depictions of their symptom experiences reflected the consequences on others, including family members. An eight-year-old girl with leukemia depicted her mother as the gatekeeper of information (see Figure 6). She depicted herself as separate from her family, waiting for her mother to obtain information to relay to her about what to expect for the day.
Children’s responses also related preferences for rating symptom severity and the meaning attached to their ratings. For example, an eight-year-old girl with a liver tumor related her frustration with numeric ratings and preferred that she be allowed to “just say ‘low,’ ‘medium,’ or ‘high.’” For her, “low” meant to allow her to be left alone, whereas “medium” or “high” meant that she needed an intervention. In contrast, a 10-year-old boy with osteosarcoma preferred a numeric rating scale with the capacity to personalize the scale to accommodate decimal points.
Discussion
Results of this study demonstrate the role of a developmentally sensitive arts-based approach—the draw-and-tell interview—to support children in relating rich personal data about their symptoms and symptom self-management strategies. When symptoms are approached solely as side effects, children often provide minimal description (Woodgate, 2008). Using drawings allowed children’s symptom experiences to be approached as multidimensional experiences. This child-centric approach allowed a greater understanding of children’s perspectives and the context in which they experienced and managed their symptoms.
Younger and older children of both genders were able to articulate symptoms. Children’s depictions of their symptoms included not only the symptoms themselves, but also the larger context in which children experienced them, including the strategies they used to manage their symptoms and the consequences of symptoms on their day-to-day lives. Anecdotally, several parents reported learning insights into their children’s experiences by listening to the draw-and-tell interviews.
Similar to previous studies with school-aged children, the most frequently reported symptoms were nausea, fatigue, pain, and sadness (Baggott et al., 2010; Linder et al., 2018; Miller et al., 2011; Walker et al., 2010; Williams et al., 2012). This study also highlighted the importance of the capacity to assess for other less frequently occurring symptoms that may be of greater importance to the child (e.g., hearing loss) that are not included on many multisymptom assessment scales (Collins et al., 2000, 2002; Williams et al., 2012). Study results also emphasize ongoing symptom assessment challenges, with some children using terms like “stomachache” and feeling “sick” or “yucky” to describe symptoms, which can limit clinicians’ ability to discern individual symptoms (Woodgate, 2008).
Participants’ pictures and accompanying explanations provided insight into different aspects of commonly reported symptoms. For example, sleep-related symptoms included sleeping more during the day, difficulty sleeping at night, and increased sleepiness/drowsiness. Appetite- and eating-related symptoms included a sense of not feeling like eating, changes in taste, and changes in appetite.
This study also emphasized the strategies that children initiate to manage their symptoms. Participants’ symptom self-management strategies emerged within their drawings and accompanying explanations without prompts to relate them. Although self-management strategies were most frequently depicted on days when the child was feeling sick, children also related strategies they used on days when they were feeling well to prevent symptoms and to cope with the consequences of chronic symptoms. Symptom self-management strategies promoted children’s comfort and supported them in being able to engage in desired activities, such as participating in Hospital Bingo.
Developmental similarities across age groups were also noted in children’s self-management strategies. Similar to adolescents and young adults (AYAs) receiving chemotherapy, children reported physical and psychosocial care strategies to manage their symptoms (Linder et al., 2017). Children most frequently related lying down and resting as a symptom management strategy, often with personal blankets or pillows arranged in a specific manner. Likewise, distractions were related by children and AYAs. Although medications were reported less frequently by children compared to AYAs, the importance of medications, as well as children’s individual strategies for taking medications, should be recognized.
Limitations
Limitations of this study include a small cross-sectional, heterogeneous sample with limited racial and ethnic diversity from a single institution. Because the emphasis of the study was children’s depiction of their symptoms, they were not prompted to relate their symptom self-management strategies. Other children may have provided information about their self-management strategies if prompted to do so. This study also did not seek to identify strategies in response to specific symptoms. In addition, this study did not assess children’s symptoms at a given point in time but rather asked them to recall their perspectives of days when they were feeling well and days when they were feeling sick.
Implications for Future Research
The scope of symptoms illustrated through children’s drawings highlights limitations of existing resources for young children (e.g., short lists of common symptoms) to fully capture children’s symptom experiences. Areas for future research include the development and validation of child-centric resources that will support a more complete report from the child’s perspective. Incorporating arts-based approaches to complement traditional self-report measures may further support a richer, child-centric understanding of the child’s experience.
Additional research is needed to explore the self-management strategies children reported in response to specific symptoms and their perceived effectiveness of these strategies. Research comparing similarities and differences among symptom self-management strategies used by patients with cancer across the lifespan is also needed. Results of this study provide initial guidance for intervention-based studies that incorporate children’s preferred symptom self-management strategies.
Implications for Nursing
Results of this study demonstrate the importance of using child-centric approaches to support children in relating rich personal data about their symptoms and symptom self-management strategies. Children as young as six years old were able to relate their symptoms and self-management strategies and to illustrate the effect of symptoms on day-to-day life. Incorporating arts-based approaches within the healthcare system may augment existing approaches to symptom assessment and may support a more comprehensive understanding of the child’s perspective, particularly with regard to less frequently reported symptoms. The addition of arts-based approaches to complement traditional measures may further serve to enhance nurse–patient communication, resulting in more personalized symptom management.
Study results also emphasize the ongoing significance of nausea and fatigue and the need for effective strategies to alleviate these symptoms. Although the evidence base for effective symptom management strategies for children is limited, nurses need to be aware of children’s capacity to implement personalized symptom self-management strategies, many of which can be easily incorporated in the clinical care setting. Integrating children’s preferred self-management strategies into the plan of care has the potential to result in more effective symptom management. Nurses can also support children’s symptom self-management by suggesting strategies that have been endorsed by other children. 
Conclusion
Children’s symptoms and the strategies they use to self-manage their symptoms reflect common, shared experiences and ones that are distinct and individual. Arts-based approaches can support nurses in gaining a more comprehensive understanding of children’s symptoms by supporting children’s ability to recall experiences and their associated meaning on day-to-day life. Children also are able to identify and implement meaningful symptom self-management strategies that can be incorporated into plans of care.
About the Author(s)
Lauri A. Linder, PhD, APRN, CPON®, is an associate professor, and Heather Bratton, MS, BSN, and Anna Nguyen are research assistants, all in the College of Nursing at the University of Utah; Kori Parker, RN, BSN, is an RN at the University of Utah Hospital; and Sarah E. Wawrzynski, BSN, RN, CCRN, is a pediatric critical care nurse at the Primary Children’s Hospital, all in Salt Lake City, UT. Linder and Parker contributed to the conceptualization and design. Linder, Bratton, and Parker completed the data collection. Linder, Nguyen, and Parker provided statistical support. All authors provided the analysis and contributed to the manuscript preparation. This research was funded by a grant (1K23NR014874-01) from the National Institute of Nursing Research. The research reported in this publication was supported, in part, by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR000105 (formerly UL1RR025764). Linder can be reached at lauri.linder@nurs.utah.edu, with copy to ONFEditor@ons.org. (Submitted July 2017. Accepted October 18, 2017.)
References
Aldridge, A.A., & Roesch, S.C. (2007). Coping and adjustment in children with cancer: A meta-analytic study. Journal of Behavioral Medicine, 30, 115–129. https://doi.org/10.1007/s10865-006-9087-y
Altay, N., Kilicarslan-Toruner, E., & Sari, C. (2017) The effect of drawing and writing technique on the anxiety level of children undergoing cancer treatment. European Journal of Oncology Nursing, 28, 1–6. https://doi.org/10.1016/j.ejon.2017.02.007
Audulv, A., Packer, T., Hutchinson, S., Roger, K.S., & Kephart, G. (2016). Coping, adapting, or self-managing—What is the difference? A concept review based on the neurological literature. Journal of Advanced Nursing, 72, 2629–2643.
Baggott, C., Dodd, M., Kennedy, C., Marina, N., Matthay, K.K., Cooper, B.A., & Miaskowski, C. (2010). Changes in children’s reports of symptom occurrence and severity during a course of myelosuppressive chemotherapy. Journal of Pediatric Oncology Nursing, 27, 307–315. https://doi.org/10.1177/1043454210377619
Butler, S., Gross, J., & Hayne, H. (1995). The effect of drawing on memory performance in young children. Developmental Psychology, 31, 597–608. http://doi.org/10.1037/0012-1649.31.4.597
Collins, J.J., Byrnes, M.E., Dunkel, I.J., Lapin, J., Nadel, T., Thaler, H.T., . . . Portenoy, R.K. (2000). The measurement of symptoms in children with cancer. Journal of Pain and Symptom Management, 19, 363–377.
Collins, J.J., Devine, T.D., Dick, G.S., Johnson, E.A., Kilham, H.A., Pinkerton, C.R., . . . Portenoy, R.K. (2002). The measurement of symptoms in young children with cancer: The validation of the Memorial Symptom Assessment Scale in children aged 7–12. Journal of Pain and Symptom Management, 23, 10–16.
Driessnack, M. (2006). Draw-and-tell conversations with children about fear. Qualitative Health Research, 16, 1414–1435. https://doi.org/10.1177/1049732306294127
Driessnack, M., & Furukawa, R. (2012). Arts-based data collection techniques used in child research. Journal for Specialists in Pediatric Nursing, 17, 3–9.
Druin, A. (1999). Cooperative inquiry: Developing new technologies for children with children. In, Proceedings of the SIGCHI conference on human factors in computing systems: The CHI is the limit (pp. 592–599). New York, NY: Association for Computing Machinery.
Dupuis, L.L., Taddio, A., Kerr, E.N., Kelly, A., & MacKeigan, L. (2006). Development and validation of the pediatric nausea assessment tool for use in children receiving antineoplastic agents. Pharmacotherapy, 26, 1221–1231. https://doi.org/10.1592/phco.26.9.1221
Elo, S., & Kyngäs, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62, 107–115.
Gabriels, R.L., Wamboldt, M.S., McCormick, D.R., Adams, T.L., & McTaggart, S.R. (2000). Children’s illness drawings and asthma symptom awareness. Journal of Asthma, 37, 565–574.
Gross, J., & Hayne, H. (1998). Drawing facilitates children’s verbal reports of emotionally laden events. Journal of Experimental Psychology, 4, 163–179.
Gross, J., Hayne, H., & Drury, T. (2008). Drawing facilitates children’s reports of factual and narrative information: Implications for educational contexts. Applied Cognitive Psychology, 23, 953–971.
Harris, P.A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J.G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42, 377–381.
Hinds, P.S., Yang, J., Gattuso, J.S., Hockenberry, M., Jones, H., Zupanec, S., . . . Srivastava, D.K. (2010). Psychometric and clinical assessment of the 10-item reduced version of the Fatigue Scale-Child instrument. Journal of Pain and Symptom Management, 39, 572–578.
Hockenberry, M.J., Hinds, P.S., Barrera, P., Bryant, R., Adams-McNeill, J., Hooke, C., . . . Manteuffel, B. (2003). Three instruments to assess fatigue in children with cancer: The child, parent and staff perspectives. Journal of Pain and Symptom Management, 25, 319–328.
Linder, L.A. (2008). Developmental diversity in symptom research involving children and adolescents with cancer. Journal of Pediatric Nursing, 23, 296–309.
Linder, L.A., Al-Qaaydeh, S., & Donaldson, G. (2018). Symptom characteristics among hospitalized children and adolescents with cancer. Cancer Nursing, 41, 23–32.
Linder, L.A., Erickson, J.M., Stegenga, K., Macpherson, C.F., Wawrzynski, S., Wilson, C., & Ameringer, S. (2017). Symptom self-management strategies reported by adolescents and young adults with cancer receiving chemotherapy. Journal of Supportive Care in Cancer, 25, 3793–3806.
Magnusson, D. (2000). The individual as the organizing principle in psychological inquiry: A holistic approach. In L.R. Bergman, L.G. Nillson, & L. Nystedt (Eds.), Developmental science and the holistic approach (pp. 33–47). Mahwah, NJ: Lawrence Erlbaum Associates.
Malchiodi, C.A. (1998). Understanding children’s drawings. New York, NY: Guilford Press.
Miles, M.S., & Holditch-Davis, D. (Eds.). (2003). Enhancing nursing research with children and families using a developmental perspective. In Annual review of nursing research (pp. 1–22). New York, NY: Springer.
Miller, E., Jacob, E., & Hockenberry, M.J. (2011). Nausea, pain, fatigue, and multiple symptoms in hospitalized children with cancer [Online exclusive]. Oncology Nursing Forum, 38, E382–E393.
Miller, W.R., Lasiter, S., Bartlett Ellis, R., & Buelow, J.M. (2015). Chronic disease self-management: A hybrid concept analysis. Nursing Outlook, 63, 154–161.
Rodgers, C.C. (2011). Health promotion of the school-age child and family. In M.J. Hockenberry & D. Wilson (Eds.), Wong’s nursing care of infants and children (9th ed., pp. 645–683). St. Louis, MO: Elsevier.
Rodgers, C., Norville, R., Taylor, O., Poon C., Hesselgrave, J., Gregurich, M.A., & Hockenberry, M.J. (2012). Children’s coping strategies for chemotherapy-induced nausea and vomiting. Oncology Nursing Forum, 39, 202–209.
Siegel, R.L., Miller, K.D., & Jemal, A. (2018). Cancer statistics, 2018. CA: A Cancer Journal for Clincians, 68, 7–30.
Stafstrom, C.E., Goldenholz, S.R., & Dulli, D.A. (2005). Serial headache drawings by children with migraine: Correlation with clinical headache status. Journal of Child Neurology, 20, 809–813.
Stefanatou, A., & Bowler, D. (1997). Depiction of pain in the self-drawings of children with sickle cell disease. Child: Care, Health, and Development, 23, 135–155.
von Baeyer, C.L. (2006). Children’s self-reports of pain intensity: Scale selection, limitations and interpretation. Pain Research and Management, 11, 157–162.
Walker, A.J., Gedaly-Duff, V., Miaskowski, C., & Nail, L. (2010). Differences in symptom occurrence, frequency, intensity, and distress in adolescents prior to and one week after the administration of chemotherapy. Journal of Pediatric Oncology Nursing, 27, 259–265.
Williams, P.D., Williams, A.R., Kelly, K.P., Dobos, C., Gieseking, A., Connor, R., . . . Del Favero, D. (2012). A symptom checklist for children with cancer: The Therapy-Related Symptom Checklist-Children. Cancer Nursing, 35, 89–98.
Woodgate, R.L. (2008). Feeling states: A new approach to understand how children and adolescents with cancer experience symptoms. Cancer Nursing, 31, 229–238.
Woodgate, R.L., & Degner, L F. (2003). Expectations and beliefs about children’s cancer symptoms: Perspectives of children with cancer and their families. Oncology Nursing Forum, 30, 479–491. https://doi.org/10.1188/03.ONF.479-491
Woodgate, R.L., Degner, L.F., & Yanofsky, R. (2003). A different perspective to approaching cancer symptoms in children. Journal of Pain and Symptom Management, 26, 800–817.
Woodgate, R.L., West, C.H., & Tailor, K. (2014). Existential anxiety and growth: An exploration of computerized drawings and perspectives of children and adolescents with cancer. Cancer Nursing, 37, 146–159.


