The Impact of Livestrong® at the YMCA for Cancer Survivors
Objectives: To determine the clinical significance of pre- and post-exercise rehabilitation physical and psychosocial outcomes of the Livestrong® at the YMCA program.
Sample & Setting: 158 participants at the YMCA of the Fox Cities in Appleton, Wisconsin, were analyzed for pre- and postparticipation physical outcomes, 68 participants were analyzed for pre- and postparticipation psychosocial outcomes, and 11 participants were interviewed about their experiences.
Methods & Variables: Participant interviews and statistical analysis of pre- and postparticipation measurements of physical and psychological determinants of health were used to evaluate the effectiveness of this exercise rehabilitation program.
Results: Quantitative data suggest physical measures of strength, balance, flexibility, and endurance, and psychosocial measures of anxiety, fatigue, sleep disturbance, satisfaction with social role, and pain interference were significantly improved post-exercise rehabilitation. Six themes that addressed experiences with Livestrong at the YMCA were qualitatively identified through participant interviews.
Implications for Nursing: It is crucial for the members of the interprofessional healthcare team to disseminate exercise rehabilitation information to survivors. Equally important is identifying when and how an exercise program will be discussed in the treatment plan. A referral system cue within the current electronic health record could help link local community exercise programs for survivors.
Jump to a section
Cancer is arguably one of the most devastating diagnoses for deteriorating overall health related to the condition itself and selected treatment modalities. With significant advances in medicine involving early screening and detection and subsequent diagnosis and treatment, cancer is no longer consistently associated with fatal outcomes. In fact, the overall mortality rate for cancer in the United States has steadily declined since the 1990s (National Cancer Institute [NCI], 2018). About 67% of individuals with a cancer diagnosis live at least five years beyond their date of diagnosis, with most dying from noncancerous causes (NCI, 2016). The growing presence of cancer survivors increases the demand to meet needs related to post-treatment concerns, particularly those that yield a loss of physical functioning or an inability to perform activities of daily living (ADLs), and the outcomes associated with alterations in social and emotional abilities (Kollas & Kollas, 2016). For these reasons, the various facets of survivorship care planning, which include conversations about exercise rehabilitation, are fundamental to the future health outcomes of cancer survivors.
Exercise rehabilitation is an effective way to mitigate assorted impairments and deconditioning that can develop in relation to treatment recovery to prevent progression to a potentially deleterious level. Exercise rehabilitation programs empower patients to improve functional capacity and achieve holistic health goals (YMCA of the Fox Cities, 2017). The YMCA, in partnership with the Livestrong Foundation, has a well-established exercise rehabilitation program, Livestrong® at the YMCA, that has served more than 55,500 cancer survivors in more than 650 communities nationwide (Livestrong Foundation, 2018). The 12-week program takes place twice weekly, with sessions lasting about 75 minutes. Trained professionals lead group-based activities with individualized exercise prescriptions that focus on cardiovascular conditioning, strength training, balance, and flexibility. Because of grants and ancillary funding, all individuals who participate in the program have no associated fees. Based on satisfaction and outcomes of Livestrong at the YMCA, survivors also can extend their YMCA membership for an additional nine months and participate in the Stay Strong program at no additional cost. This allows for continued guidance to ensure that post-treatment toxicities are kept at bay and the beneficial sequelae brought about by exercise is sustainable over time (YMCA of the Fox Cities, 2017).
The rationale for this program evaluation was to perform an impact assessment of Livestrong at the YMCA because a data analysis has never been formally conducted. The overarching objectives of this study were to determine the impact of Livestrong at the YMCA on physical and psychosocial measures of the participants during the past five years, and to gain additional perspectives about this local branch of the community-based Livestrong at the YMCA through interviews with current and previous participants.
Theoretical Framework
Exercise motivation is a difficult task to undertake for any population, but it is particularly challenging for individuals with chronic diseases. The most widely used theory to explain exercise motivation for cancer survivors is the theory of planned behavior (TPB) (Ajzen, 1991; Courneya, Karvinen, & Vallance, 2007). This theory focuses on individual intention as the primary determinant of behavior because it reflects a conscious decision on whether a behavior will be performed or executed (Ajzen, 1991). Several studies that have been conducted to determine the efficacy of this theoretical framework have deduced that the TPB adequately supports an understanding of the correlates of exercise motivation and behavior in cancer survivors (Courneya et al., 2007).
Methods
An explanatory, mixed-methods approach was used. The institutional review board at the University of Wisconsin–Oshkosh granted approval to conduct this study.
Sample and Setting
For the quantitative portion of this study, inclusion criteria were having a cancer diagnosis and participating in Livestrong at the YMCA in Appleton, Wisconsin. Physical and psychosocial measures were tracked from 2012–2017 by this YMCA through the use of a secure Microsoft® Excel spreadsheet. The psychosocial measures were not included in the data collection process until 2016, so the sample size of this dataset (n = 68) is significantly less than the physical measures (n = 158). Age, sex, ethnicity, cancer diagnosis, and rate of program attendance were not captured or disclosed per participant for the data that were analyzed.
For the qualitative portion of this study, inclusion criteria were the following: being aged 18 years or older; being able to read and speak English; having been diagnosed with cancer and undergone treatment with chemotherapy, radiation therapy, and/or surgical intervention; and having previously been or currently being participants in Livestrong at the YMCA.
Quantitative Purpose
For physical measures, balance, flexibility, strength, and cardiovascular endurance were assessed with multiple evidence-based tools. Balance was measured by two means. The balance stand test assessed the participant’s ability to balance on one foot for as long as 60 seconds, repeated bilaterally (Centers for Disease Control and Prevention, 2017). The functional reach test assessed how far a participant could reach forward without losing balance (Jones & Rikli, 2002). Shoulder flexibility was measured with the back scratch test, which was scored by the following criteria (Jones & Rikli, 2002):
• If the fingertips do not touch, the distance between the fingers represents a negative score.
• If the fingertips just touch, the score is 0.
• If the fingertips overlap, a positive score is achieved.
Upper and lower body strength were measured with the chest and leg press, respectively, by adding incremental weight (5–10 pounds at a time) and performing one repetition at each weight until muscular failure was achieved (Phillips, Batterman, Valenzuela, & Burkett, 2004). Cardiovascular endurance was measured with the six-minute walk test, which determines the distance that a patient can quickly walk on a flat, hard surface in six minutes (American Thoracic Society, 2002). Intake forms regarding the purpose, setting, equipment use, and techniques were available to the instructors for reference on the proper evidence-based execution of each test.
The validity and reliability of the previously mentioned physical tests are important to highlight in deeming these measures accurate, consistent, and trustworthy. For the balance stand test, test-retest reliability was 0.9–0.91 (Frachignoni, Tesio, Martino, & Ricupero, 1998). For the functional reach test, internal consistency was 0.71 and test-retest reliability was 0.89 (Weiner, Duncan, Chandler, & Studenski, 1992). The back scratch test is considered to be the best measure of shoulder flexibility, with test-retest reliability of 0.96 (Rikli & Jones, 1999). The chest and leg press both have high test-retest reliability at 0.98 and 0.99, respectively (Levinger et al., 2009). For the six-minute walk test, internal consistency was 0.52 when analyzed with standing balance, and test-retest reliability was 0.95 (Harada, Chiu, & Stewart, 1999).
The PROMIS ([Patient-Reported Outcomes Measurement Information System], 2018)–29 Profile is an evidence-based tool, with an internal consistency of 0.96–0.98 and test-retest reliability of 0.92–0.96 (Jensen et al., 2015), that aids in evaluation and monitoring of physical, mental, and social health. Within the context of Livestrong at the YMCA, it is used to assess functional and psychosocial health. The PROMIS-29 Profile is comprised of eight indices that measure physical function, anxiety, depression, fatigue, sleep disturbance, satisfaction with social role, pain interference, and pain intensity. Individuals were asked to rate each item from questions 1–28 on a five-point ordinal scale ranging from 1 (without any difficulty, never, or not at all) to 5 (unable to do, always, or very much) with respect to the questions being asked. Question 29 focused on pain intensity and used a numeric pain scale ranging from 0 (no pain) to 10 (worst pain imaginable). Total PROMIS-29 Profile scores have the potential to range from 0–150, with lower scores indicating less impact of the various indices on overall quality of life.
Data analysis of the physical and psychosocial measures was performed by a researcher through the Excel data analysis function, 2016 version. Variables were analyzed using paired t-test comparisons. A significance level of 0.05 and confidence level of 95% were set for all variables. Consultation with an expert statistician was used in planning for and after completion of data analysis to ensure accuracy.
Qualitative Purpose
Face-to-face interviews were conducted by a researcher in a quiet, private setting on the local YMCA campus. Before each interview, participants signed an informed consent form and completed a demographic survey. Participants had the option to disclose their cancer diagnosis or diagnoses if they felt comfortable doing so. All participants were assigned a case number to maintain confidentiality during and after the interview process. Each interview lasted about 30–45 minutes. A semistructured interview style was used by the researchers to determine a participant’s perceptions through the following prompt: “Tell me about your experience with the Livestrong program.” Questions were formulated throughout the duration of the interview process when necessary to gain additional insight.
After obtaining written permission from the participants, a professional transcriptionist transcribed verbatim audio-recorded interviews. Determination that an adequate amount of interviews were completed occurred when data saturation was met. Each interview was coded, and each line was numbered to enable statement origins. The two researchers examined the transcribed interviews independently to identify possible categories. In this initial phase, each researcher identified key phrases and words that captured the interviewee’s experiences with Livestrong at the YMCA. Researchers met multiple times to discuss the findings through thematic analysis and identify patterns within the dialogue. An overall theme was identified by the researchers for each grouping from the qualitative data interviews (Streubert & Carpenter, 2007). The analysis process and procedure were maintained in a master codebook to ensure confirmability and an audit trail. This study’s transferability is limited to other similar YMCA Livestrong programs.
Results
Quantitative Findings
Bivariate associations between pre- and postprogram physical and psychosocial measures were examined to determine the quantitative impact of Livestrong at the YMCA. Statistically significant positive changes were seen in the following physical measures: single leg balance on the right, single leg balance on the left, six-minute walk test, leg press, chest press, right shoulder flexibility, left shoulder flexibility, and functional reach test (see Table 1). Statistically significant positive changes also were seen in the following psychosocial measures: anxiety index, fatigue index, sleep index, social role index, and pain interference index (see Table 2). The physical function, depression, and pain intensity indices were not affected in a statistically significant way. 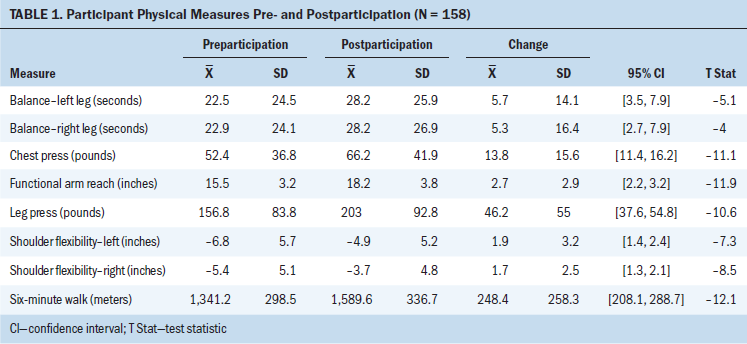
Although these results clearly demonstrate that participants in Livestrong at the YMCA showed notable improvements on a wide array of physical and psychosocial measures, which may speak to the benefit of the program, the lack of a control group limits the degree to which the authors can fully credit the improvements to the program. Specifically, one would expect cancer survivors to improve to some extent during the recovery phase following cancer treatment, regardless of participation, so it is intuitive to assume that some share of the measured improvement would have occurred without participation in the program. That being said, the size, breadth, and nature of the improvements present a strong case that the program played a noteworthy role in aiding in the physical and psychosocial improvement of these patients. 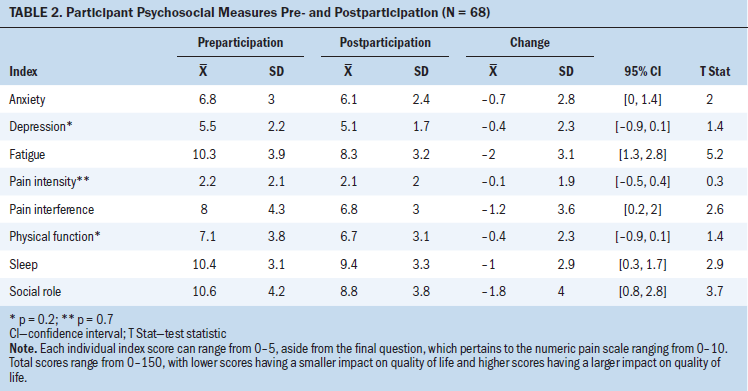
Qualitative Findings
Eleven participant interviews occurred during a three-week period. Of the participants, six were women and five were men, and their ages ranged from 35–74 years. All participants were Caucasian. Diagnoses included multiple myeloma, lymphoma, and breast, ovarian, thyroid, prostate, bile duct, endometrial, renal, colon, and skin cancer. About 91% (n = 10) of the participants were married or in a domestic partnership. Thirty-six percent (n = 4) were employed, 55% (n = 6) were retired, and 1% (n = 1) were unable to work because of disability.
The following six themes were identified from the interviews in response to personal experiences with Livestrong at the YMCA: positive physical changes, mental well-being, “we’re in this together,” “there’s something for everybody,” back on track, and “it was fun.” See Figure 1 for a summation of quotes from the interview participants related to each theme. Of the 11 interview participants, seven pursued the Stay Strong program. Of the four who did not, barriers included work conflicts and limited program availability prior to 2016. 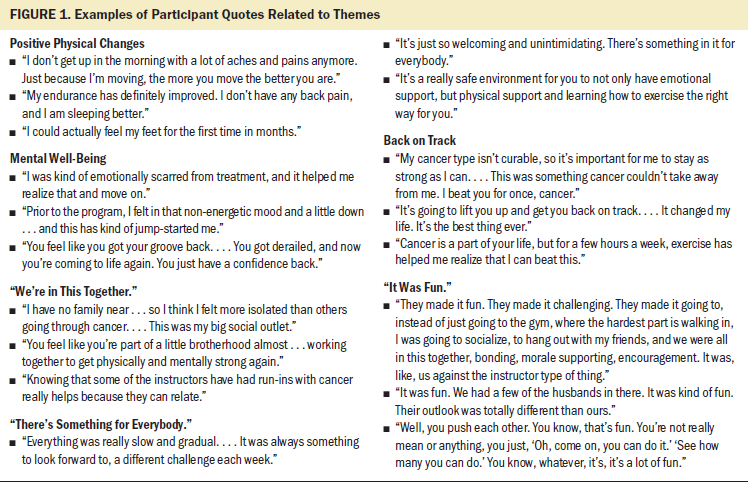
Discussion
Physical Benefits for Survivors
The intensity of aerobic activity is a significant predictor of quality of life and is strongly associated with increased endurance, particularly for interventions of longer duration (Knobf, Thompson, Fennie, & Erdos, 2014). Livingston et al. (2015) discussed similar findings that deduced that exercising for 45 minutes was most effective and increased the likelihood of meeting current guidelines. Research also has pointed to statistically significant improvements in upper and lower body strength from trials of resistance and aerobic-based physical activity (Hatchett & Bellar, 2012; Schmitz et al., 2010; Stene et al., 2013). Kollas and Kollas (2016) and Cheifetz et al. (2014) discussed an overall increase in aerobic function, flexibility, balance, and strength with an exercise rehabilitation program. Such interventions result in improved physical functioning and ADLs (Jones et al., 2013). Exercise rehabilitation also can contribute to reduced risk of recurrence in some cancers, specifically breast and colon (Musanti & Murley, 2016). However, for benefits to be sustainable, continued exercise is indicated after programs end (Cheville et al., 2010).
Psychosocial Benefits for Survivors
Participation in an exercise rehabilitation program promotes and improves emotional well-being, social functioning, and mental health (Knobf et al., 2014; Salakari, Surakka, Nurminen, & Pylkkänen, 2015; Wolin, Dart, & Colditz, 2013). Kollas and Kollas (2016) and Livingston et al. (2015) noted a specific impact on decreasing depression, which is a common comorbid condition that exists with cancer-related fatigue (CRF). CRF is most effectively managed and reduced in patients who have completed chemotherapy or radiation therapy (Oldervoll et al., 2011). Individuals who failed to complete exercise rehabilitation programs reported a higher than average rating of CRF in comparison to baseline measures (Tran et al., 2016). In addition, three to five days per week of aerobic exercise interventions result in significant improvements in energy levels (Silver, Baima, & Mayer, 2013). Hatchett and Bellar (2012) deduced that CRF decreased in conjunction with cardiovascular and strengthening exercises. This was echoed by Silver et al. (2013), who mentioned that, contrary to popular belief, rest is not an effective method to reduce symptoms of CRF when compared to exercise.
Program Comparison
To determine the impact of Livestrong at the YMCA, it is important to compare this form of exercise rehabilitation with other equivalent programs. FitSteps for Life® is a Texas-based program that operates in a variety of settings, including churches and community centers, and focuses on individualized exercise programs with ongoing supervision. Observation of two years of involvement in the program showed improvements in various aspects of quality of life (Haas, Kimmel, Hermanns, & Deal, 2012). FitSteps for Life is unlike other forms of community-based exercise rehabilitation in that no limit is placed on the duration of time an individual can participate in the program (Musanti & Murley, 2016). Comparable programs, such as Life Now Exercise and CanWell, exist in Canada and Australia, with similar program components and outcomes (Cormie et al., 2017). The overall conclusion remains consistent in the established efficacy of exercise in reducing treatment-related side effects and increasing quality of life in cancer survivors, regardless of the community-based program available.
Limitations
Quantitatively, there were three limitations. The first limitation centered on the single-site analysis of one YMCA. Results can only be generalized to individuals in the area where the study occurred. The second limitation was an inadequate level of control. If this study were to be replicated in the future, results would be strengthened by having a physical control group that did not participate in Livestrong at the YMCA or satisfied by means of creating a control group, using program attendance to determine if the amount of participation changed the significance of the outcomes. The third limitation was a lack of participant demographic information to determine if a specific age, sex, ethnicity, or cancer diagnosis bene-fited most from the exercise rehabilitation. Additional efforts should be made to better track these data as a goal for future analyses.
Qualitatively, there were an additional three limitations. The interviews were solely based on participants’ recollections of their experience with Livestrong at the YMCA. Therefore, the information that was provided can only be assumed to be an accurate representation of overall experience, which increases the chance of recall bias. Interview participants were recruited at the discretion of the researcher. This may have presented a potential for selecting participants with more positive experiences. Finally, the sample population used in this portion of the study did not include any variants in ethnicity or any participants within the 18–34 years or 75 years or older age groups. Opinions about the program likely would be consistent with the sample of individuals who were interviewed; however, this assumption cannot be made.
Implications for Practice
Determining the most appropriate timeframe to initiate the conversation about exercise rehabilitation is a component of cancer care that can pose a significant obstacle. Given that the diagnostic and initial treatment stages are often fraught with uncertainty and fear, presenting irrelevant information at that time may render the discussion wholly ineffective. However, during the survivorship phase of care, patients may not have concerns to this extent and, thereby, may be more receptive to exercise rehabilitation. Unfortunately, this falls into the tertiary level of prevention, so, in contrast, many patients may already have developed treatment-related complications, which could have been prevented or lessened if exercise were started sooner. Regardless of whether a true right time to have these discussions exists, information about exercise rehabilitation preferably should be a topic of conversation or talking point during each office visit.
Despite evidence that demonstrates the cumulative benefits of initiating and maintaining a healthy lifestyle after a cancer diagnosis, only 20% of oncologists help guide patients in ways to be successful in this realm of care (Wolin et al., 2013). An insufficient amount of time during office visits may be one of the largest contributing factors to the issue of educating and advocating for patients to begin exercise sooner (Rajotte et al., 2012). Interprofessional collaboration with advanced practice nurses, oncology nurse navigators, and nurses may be the missing link to ameliorate this problem. Implementing exercise rehabilitation programs on a broader scale will require training oncology healthcare providers about these benefits and how to identify and refer survivors to local, community-based programs (Alfano, Ganz, Rowland, & Hahn, 2012). Information obtained from this study could assist oncology nurses with the opportunity to have discussions about exercise rehabilitation programs with survivors and allow them to perform more targeted assessments based on knowledge of the program structure.
Incorporating an exercise-based intervention into oncology practice as a standard of care for survivorship would be easy to replicate, generalizable across the nation, and ultimately lead to lifelong behavior changes in patients (Haas & Kimmel, 2011). In accordance with this thought, an adequate referral system should be devised to avoid the underuse of exercise rehabilitation because accessing such services is dependent on provider referrals (Alfano et al., 2012). Literature is lacking in terms of ways that this can be done efficiently and effectively in congruence with overall survivorship planning. Therein lies the need for a sustainable method of referral to exercise rehabilitation programs available to survivors with varying incomes and cultural backgrounds. Future nursing research should focus on the incorporation of a referral cue within electronic health records to link local community exercise rehabilitation programs with survivors during care planning. 
Conclusion
The findings from the current study further support the importance of exercise rehabilitation for cancer survivors. The evidence-based program highlighted in this study can be used as one example that provides an opportunity for oncology healthcare providers to collaborate with local community partners. Partnerships, such as with the YMCA, may lend resources toward sustainability of these types of programs and allow a team to continue offering support and care, and the opportunity to improve the health of cancer survivors.
The authors gratefully acknowledge Chad Cotti, PhD, and the YMCA of the Fox Cities in Appleton, WI, for their assistance throughout the study, as well as all of the participants of the Livestrong program who shared their experiences.
About the Author(s)
Molly M. Schumacher, DNP, RN, OCN®, CCAP, FNP-BC, is an oncology/hematology nurse practitioner at ThedaCare Regional Cancer Center in Appleton, WI; and Paula McNiel, DNP, RN, APHN-BC, is an associate professor in the College of Nursing at the University of Wisconsin in Oshkosh. This research was funded through a student/faculty collaborative research grant from the University of Wisconsin-Oshkosh Office of Student Research and Creative Activity. Both authors contributed to the conceptualization and design, completed the data collection, provided statistical support and the analysis, and contributed to the manuscript preparation. Schumacher can be reached at mschumacher18@alumni.uwosh.edu, with copy to ONFEditor@ons.org. (Submitted April 2018. Accepted June 11, 2018.)
References
Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211. https://doi.org/10.1016/0749-5978(91)90020-T
Alfano, C.M., Ganz, P.A., Rowland, J.H., & Hahn, E.E. (2012). Cancer survivorship and cancer rehabilitation: Revitalizing the link. Journal of Clinical Oncology, 30, 904–906. https://doi.org/10.1200/JCO.2011.37.1674
American Thoracic Society. (2002). ATS statement: Guidelines for the six-minute walk test. American Journal of Respiratory and Critical Care Medicine, 166, 111–117. https://doi.org/10.1164/ajrccm.166.1.at1102
Centers for Disease Control and Prevention. (2017). STEADI materials for healthcare providers. Retrieved from https://www.cdc.gov/steadi/materials.html
Cheifetz, O., Park Dorsay, J., Hladysh, G., MacDermid, J., Serediuk, F., & Woodhouse, L.J. (2014). CanWell: Meeting the psychosocial and exercise needs of cancer survivors by translating evidence into practice. Psycho-Oncology, 23, 204–215. https://doi.org/10.1002/pon.3389
Cheville, A.L., Girardi, J., Clark, M.M., Rummans, T.A., Pittelkow, T., Brown, P., . . . Gamble, G. (2010). Therapeutic exercise during outpatient radiation therapy for advanced cancer: Feasibility and impact on physical well-being. American Journal of Physical Medicine and Rehabilitation, 89, 611–619. https://doi.org/10.1097/PHM.0b013e3181d3e782
Cormie, P., Lamb, S., Newton, R.U., Valentine, L., McKiernan, S., Spry, N., . . . Galvão, D.A. (2017). Implementing exercise in cancer care: Study protocol to evaluate a community-based exercise program for people with cancer. BMC Cancer, 17, 103. https://doi.org/10.1186/s12885-017-3092-0
Courneya, K.S., Karvinen, K.H., & Vallance, J.K.H. (2007). Exercise motivation and behavior change. In M. Feuerstein, Handbook of Cancer Survivorship (pp. 113–132). Boston, MA: Springer.
Frachignoni, F., Tesio, L., Martino, M.T., & Ricupero, C. (1998). Reliability of four simple, quantitative tests of balance and mobility in healthy elderly females. Aging, 10, 26–31.
Haas, B.K., & Kimmel, G. (2011). Model for a community-based exercise program for cancer survivors: Taking patient care to the next level. Journal of Oncology Practice, 7, 252–256. https://doi.org/10.1200/JOP.2010.000194
Haas, B.K., Kimmel, G., Hermanns, M., & Deal, B. (2012). Community-based FitSTEPS for life exercise program for persons with cancer: 5-year evaluation. Journal of Oncology Practice, 8, 320–324. https://doi.org/10.1200/JOP.2012.000555
Harada, N.D., Chiu, V., & Stewart, A.L. (1999). Mobility-related function in older adults: Assessment with a 6-minute walk test. Archives of Physical Medicine and Rehabilitation, 80, 837–841.
Hatchett, A., & Bellar, D. (2012). Physiologic and behavioral outcomes of a physical activity intervention designed specifically for survivors of cancer: A pilot study. Integrative Medicine: A Clinician’s Journal, 11(4), 19–25.
Jensen, R.E., Potosky, A.L., Reeve, B.B., Hahn, E., Cella, D., Fries, J., . . . Moinpour, C.M. (2015). Validation of the PROMIS physical function measures in a diverse U.S. population-based cohort of cancer patients. Quality of Life Research, 24, 2333–2344. https://doi.org/10.1007/s11136-015-0992-9
Jones, C.J., & Rikli, R.E. (2002). Measuring functional fitness of older adults. Journal on Active Aging, 2(2), 24–30.
Jones, L., FitzGerald, G., Leurent, B., Round, J., Eades, J., Davis, S., . . . Tookman, A. (2013). Rehabilitation in advanced, progressive, recurrent cancer: A randomized controlled trial. Journal of Pain and Symptom Management, 46, 315–325. https://doi.org/10.1016/j.jpainsymman.2012.08.017
Knobf, M.T., Thompson, A.S., Fennie, K., & Erdos, D. (2014). The effect of a community based exercise intervention on symptoms and quality of life. Cancer Nursing, 37(2), 43-50. https://doi.org/10.1097/NCC.0b013e318288d40e
Kollas, B., & Kollas, C. (2016). Exploring the emotional, psychosocial and physical effects of a community-based exercise program for cancer survivors (S788). Journal of Pain and Symptom Management, 51, 456–457. https://doi.org/10.1016/j.jpainsymman.2015.12.091
Levinger, I., Goodman, C., Hare, D.L., Jerums, G., Toia, D., & Selig, S. (2009). The reliability of the 1RM strength test for untrained middle-aged individuals. Journal of Science and Medicine in Sport, 12, 310–316. https://doi.org/10.1016/j.jsams.2007.10.007
Livestrong Foundation. (2018). Livestrong at the YMCA. Retrieved from https://www.livestrong.org/what-we-do/program/livestrong-at-the-ymca
Livingston, P.M., Craike, M.J., Salmon, J., Courneya, K.S., Gaskin, C.J., Fraser, S.F., . . . Kent, B. (2015). Effects of a clinician referral and exercise program for men who have completed active treatment for prostate cancer: A multicenter cluster randomized controlled trial (ENGAGE). Cancer, 121, 2646–2654. https://doi.org/10.1002/cncr.29385
Musanti, R., & Murley, B. (2016). Community-based exercise programs for cancer survivors. Clinical Journal of Oncology Nursing, 20(6 Suppl.), S25–S30. https://doi.org/10.1188/16.CJON.S2.25-30
National Cancer Institute. (2016). Statistics. Retrieved from https://cancercontrol.cancer.gov/ocs/statistics/statistics.html
National Cancer Institute. (2018). Cancer statistics. Retrieved from https://www.cancer.gov/about-cancer/understanding/statistics
Oldervoll, L.M., Loge, J.H., Lydersen, S., Paltiel, H., Asp, M.B., Nygaard, U.V., . . . Kaasa, S. (2011). Physical exercise for cancer patients with advanced disease: A randomized controlled trial. Oncologist, 16, 1649–1657. https://doi.org/10.1634/theoncologist.2011-0133
Patient-Reported Outcomes Measurement Information System. (2018). PROMIS-29 profile [v.2.1]. Retrieved from http://www.healthmeasures.net/index.php
Phillips, W.T., Batterman, A.M., Valenzuela, J.E., & Burkett, L.N. (2004). Reliability of maximal strength testing in older adults. Archives of Physical Medicine and Rehabilitation, 85, 329–334. https://doi.org/10.1016/j.apmr.2003.05.010
Rajotte, E.J., Yi, J.C., Baker, K.S., Gregersen, L., Leiserowitz, A., & Syrjala, K.L. (2012). Community-based exercise program effectiveness and safety for cancer survivors. Journal of Cancer Survivorship, 6, 219–228. https://doi.org/10.1007/s11764-011-0213-7
Rikli, R.E., & Jones, C.J. (1999). Development and validation of a functional fitness test for community-residing older adults. Journal of Aging and Physical Activity, 7, 129–161.
Salakari, M.R., Surakka, T., Nurminen, R., & Pylkkänen, L. (2015). Effects of rehabilitation among patients with advances cancer: A systematic review. Acta Oncologica, 54, 618–628. https://doi.org/10.3109/0284186X.2014.996661
Schmitz, K.H., Courneya, K.S., Matthews, C., Demark-Wahnefried, W., Galvão, D.A., Pinto, B.M., . . .Schwartz, A.L. (2010). American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Medicine and Science in Sports and Exercise, 42, 1409–1426. https://doi.org/10.1249/MSS.0b013e3181e0c112
Silver, J.K., Baima, J., & Mayer, R.S. (2013). Impairment-driven cancer rehabilitation: An essential component of quality care and survivorship. CA: A Cancer Journal for Clinicians, 63, 295–317. https://doi.org/10.3322/caac.21186
Stene, G.B., Helbostad, J.L., Balstad, T.R., Riphagen, I.I., Kaasa, S., & Odervoll, L.M. (2013). Effect of physical exercise on muscle mass and strength in cancer patients during treatment—A systematic review. Critical Reviews in Oncology/Hematology, 88, 573–593.
Streubert, H.J., & Carpenter, D.R. (2007). Qualitative research in nursing (4th ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Tran, H., Lin, C., Yu, F., Frederick, A., Mieras, M., & Baccaglini, L. (2016). A multicenter study on the relative effectiveness of a 12-week physical training program for adults with an oncologic diagnosis. Supportive Care in Cancer, 24, 3605–3713. https://doi.org/10.1007/s00520-016-3194-2
Weiner, D.K., Duncan, P.W., Chandler, J., & Studenski, S.A. (1992). Functional reach: A marker of physical frailty. Journal of the American Geriatrics Society, 40, 203–207.
Wolin, K.Y., Dart, H., & Colditz, G.A. (2013). Eight ways to stay healthy after cancer: An evidence-based message. Cancer Causes and Control, 24, 827–837. https://doi.org/10.1007/s10552-013-0179-z
YMCA of the Fox Cities. (2017). Programs for cancer survivors. Retrieved from http://www.ymcafoxcities.org/ymca/livestrong/liveSTRONG.asp




