Improving the Pain Experience for Hospitalized Patients With Cancer
Purpose: To determine the effect of an evidence-based Pain Stoppers bundled intervention on pain management satisfaction scores and actual pain intensity scores of hospitalized patients with cancer, as well as nurses’ knowledge and attitudes on pain.
Participants & Setting: Participants and nurses took part in a preintervention group (n = 173 and 11, respectively) and a postintervention group (n = 157 and 9, respectively) at a National Cancer Institute–designated comprehensive cancer center.
Methodologic Approach: A pre- and postintervention design was used. Evidence-based strategies included staff education, improved staff communication, adoption of caring behaviors and timely responses, improved patient education, and efforts to maintain patients’ analgesic levels.
Findings: Patient satisfaction with staff improved from preintervention to postintervention. No statistically significant differences were noted in actual pain intensity scores between the groups; however, fewer patients in the postintervention group received chemotherapy within 30 days, and more were admitted for symptom management versus chemotherapy administration. In addition, no difference was noted between RN group scores, although there was statistically significant improvement on individual questions in the postintervention group.
Implications for Nursing: Implementation of a Pain Stoppers bundled intervention may be effective in improving the pain experience for hospitalized patients with solid tumor cancers.
Jump to a section
Pain is a significant and multidimensional problem for patients diagnosed with cancer. The National Comprehensive Cancer Network ([NCCN], 2018) adult pain guidelines advise providers to consider hospitalization of patients suffering from “acute, severe pain, or pain crisis” (p. MS-7). Cancer pain has several potential causes. Most often, pain is caused by tumor burden, but cancer treatments and unrelated comorbid conditions may also produce pain (American Cancer Society, 2018). Inadequate management of cancer pain denies comfort and acceptable quality of life, and may even reduce survival (NCCN, 2018). Cancer pain may produce emotional distress, with prolonged duration and higher pain intensity associated with depression (National Cancer Institute, 2018). Patients with cancer may fear addiction, developing tolerance, side effects, or the implications of needing opioid analgesics (National Institute for Health and Care Excellence, 2016). These many features of cancer pain affect the patient’s pain experience and the professional caregiver’s ability to influence this experience.
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey (Centers for Medicare and Medicaid Services, 2017; Giordano, Elliott, Goldstein, Lehrman, & Spencer, 2010) sought to measure patient satisfaction with pain management by asking discharged patients requiring pain medication during their admission to answer always, usually, sometimes, or never to two pain-related questions: “How often was your pain well controlled?” and “How often did the hospital staff do everything they could to help you with your pain?” Composite pain satisfaction HCAHPS scores on an adult medical oncology inpatient unit caring for patients with solid tumors was 58% from May to July 2017, indicating an opportunity to reduce suffering in this vulnerable population. Nurses, in the role of patient caregivers, advocates, and educators, are in a unique position to influence the pain experience of individuals with cancer; therefore, an evidence-based nursing intervention to improve pain management on this unit was sought.
Literature Review
A review of the literature yielded evidence that various staff educational offerings, staff behavior changes, and patient education techniques may reduce pain intensity scores, improve pain satisfaction scores, and/or increase RNs’ knowledge and attitudes on pain scores. The evidence supported staff interventions, which included staff education to improve pain knowledge, use of HCAHPS-based language scripting, hourly rounding, preparing to discuss pain management before entering patient rooms, and encouraging around-the-clock analgesic dosing, as well as other interventions (Alaloul, Williams, Myers, Jones, & Logsdon, 2015; de Rond, de Wit, van Dam, & Muller, 2000; Dulko, Hertz, Julien, Beck, & Mooney, 2010; Innis, Bikaunieks, Petryshen, Zellermeyer, & Ciccarelli, 2004; Jarrett, Church, Fancher-Gonzalez, Shackelford, & Lofton, 2013; Keen et al., 2017; Sterman, Gauker, & Krieger, 2003). There was also abundant evidence to support patient education and patient-centered approaches (Kim et al., 2012; Lim et al., 2015; Yildirim, Cicek, & Uyar, 2009; Zoëga, Gunnarsdottir, Wilson, & Gordon, 2016). Many studies promoted multi-pronged approaches to improve patient satisfaction with pain management (Comley & DeMeyer, 2001; Glowacki, 2015; Goldberg & Morrison, 2007; Muntlin, Carlsson, Säfwenberg, & Gunningberg, 2011; Sherwood, Adams-McNeill, Starck, Nieto, & Thompson, 2000; Trail-Mahan, Heisler, & Katica, 2016). The evidence also indicated that improving patient satisfaction with pain management is possible without necessarily improving actual pain intensity scores (Dulko et al., 2010; Innis et al., 2004; Lim et al., 2015) and that nurses affect the patient’s pain experience and influence satisfaction with pain management (Bozimowski, 2012; Brant, Mohr, Coombs, Finn, & Wilmarth, 2017; Craig, Otani, & Herrmann, 2015; de Rond et al., 2000; Innis et al., 2004; Jarrett et al., 2013; Sherwood et al., 2000; Sterman et al., 2003; Trail-Mahan et al., 2016). This is an important consideration because nurses are unable to directly influence medical orders for analgesics, but can influence the patients’ pain experience in other ways. The qualitative evidence from the literature was notable, demonstrating that patients want caring, quick responses to their pain needs and they want to participate, alongside their family members, in decision making with the healthcare team (Comley & DeMeyer, 2001; Sherwood et al., 2000).
A Pain Stoppers bundled intervention, informed by this evidence and the Ottawa Model of Research Use translation framework, was developed and implemented on the solid tumor inpatient unit at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins, a National Cancer Institute–designated comprehensive cancer center in Baltimore, Maryland (see Figure 1). 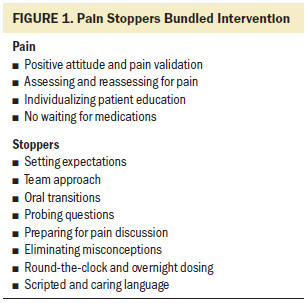
Methods
This quality improvement project used a pre- and postintervention design to determine the effect of an evidence-based Pain Stoppers bundled intervention on pain management satisfaction scores and actual pain intensity scores of hospitalized patients with cancer, as well as nurses’ knowledge and attitudes on pain. The objectives of this project were as follows:
• Explore the effect of an evidence-based Pain Stoppers bundled intervention on satisfaction with pain management in hospitalized patients with cancer.
• Determine the effect of an evidence-based Pain Stoppers bundled intervention on actual pain intensity scores in hospitalized patients with cancer.
• Measure oncology RNs’ knowledge and attitudes on pain scores pre- and postimplementation of the Pain Stoppers bundled intervention.
The dependent variables were (a) HCAHPS pain satisfaction scores, (b) patients’ actual pain intensity scores, and (c) nurses’ scores on the Knowledge and Attitudes on Pain Survey (KAP) (Ferrell & McCaffery, 2014). The preintervention time period was from May 1 to July 31, 2017, and the postintervention time period was from September 1 to November 30, 2017. The organization’s implementation of a new electronic health record (EHR) and patient call system prevented comparison to the previous year’s data.
Sample and Setting
Patients admitted to the solid tumor medical oncology unit who had a recorded pain intensity score of 1 or greater at any time during hospitalization were included in the study. Patients not discharged home following admission (deceased or transferred) were excluded. Permanent nursing staff providing direct patient care during the study period were also included.
Intervention
Following notification of exemption from the organization’s institutional review board to conduct this quality improvement project, an implementation team was convened. The team consisted of the project lead, nurse educator, patient educator, pain and palliative care nurse, a patient representative, three inpatient nurses, and the unit’s clinical nurse specialist. The evidence was reviewed and unit characteristics discussed, leading to the development of the intervention. Evidence-based strategies for improvement were categorized as (a) communication, caring behaviors, and timely responses; (b) patient education; and (c) maintenance of analgesic levels. Specific interventions are listed in Figure 2. 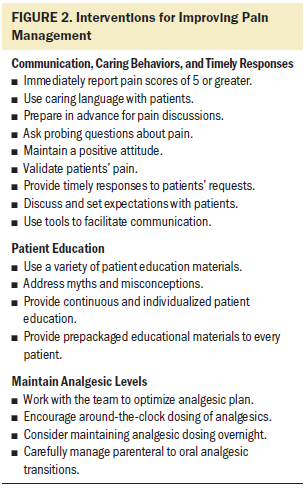
Procedures
Inservices providing background information on cancer pain, evidence for improving the pain experience of individuals with cancer, and describing the intervention were provided by the project lead to the unit’s RNs and clinical technicians (CTs) from July 24 to 31, 2017. Handouts were offered and left on the unit to reinforce the information shared during the educational sessions. Staff were highly engaged in discussion during the inservices. Six follow-up communications were emailed to RNs and CTs from August 1 to September 27, 2017. The emails reviewed the intervention and expectations, provided encouragement, presented pertinent information from NCCN pain guidelines, and specifically addressed five knowledge and attitude questions with low mean preintervention scores. Beginning in August, packaged patient education materials were placed bedside in patient rooms prior to admission. These materials addressed patient misconceptions, encouraged patients to notify staff immediately when experiencing pain (even if it is not time for pain medication), and asked patients to alert staff if they wished to see a pain and palliative care team member. The package included a small notebook and pen to attract the attention of the patient and/or family member and to allow he or she to record questions or notes. Staff were asked to record placement of these patient education materials on a centralized document located at the unit secretary’s desk. Placement of the patient education packet in patient rooms was sporadic in August, but greatly improved by September and for the remainder of the postintervention period. In addition, the institution’s two-page, patient education pain document was placed in frames in each patient room. CTs were instructed to call nurses immediately when patients reported a pain score of 5 or greater on routine screening. Prior to implementing the intervention, CTs would record high pain scores in the EHR but would not immediately inform the nurse. Pain Stoppers visual aids were placed in staff work areas and medication stations.
Instruments
HCAHPS surveys were mailed to a random sample of discharged patients through Press Ganey, a patient experience consulting company. Survey results were accessed from the Press Ganey website for each of the pre- and postintervention time periods. The unit’s RNs received email invitations to complete the KAP electronically, through Qualtrics, from July 7 to 24, 2017 (preintervention) and October 11 to November 30, 2017 (postintervention). The KAP survey has been used in many studies, and the authors report that “survey test-retest reliability was previously established (r > 0.8) by repeat testing in a continuing education class of staff nurses (N = 60)” and “internal consistency reliability was established (alpha r > 0.7) with items reflecting both knowledge and attitude domains” (Ferrell & McCaffery, 2014, p. 1). The survey consists of 22 true or false questions, 15 multiple choice questions, and two case studies each containing two questions. However, 4 of the 41 questions in the KAP survey were not used in this project. One question each from the case studies was intentionally excluded as they no longer reflected current practice, and two multiple choice questions were excluded because of an error in transcribing questions and possible answers into the electronic format. Demographic and pain intensity data were extracted from the EHR for eligible patients hospitalized during the data collection period. Patients receiving chemotherapy and/or biotherapy (not hormonal therapy) by any route of administration (including oral) within the past 30 days were coded as currently receiving chemotherapy. Pain intensity scores were measured on an 11-point Likert-type scale ranging from 0 (no pain) to 10 (worst pain imaginable). For each patient, the following was collected: first pain intensity score documented after admission, last score documented prior to discharge, and lowest score and highest score documented during the hospitalization. In addition, documentation of the provision of pain-specific patient education, and receipt of pain and palliative care team consultation, were recorded.
Data Analysis
All data were analyzed using IBM SPSS Statistics, version 25.0. Fisher’s exact test and descriptive statistics were employed to evaluate pre- and postintervention HCAHPS pain scores. An independent t test was used to determine any differences in pain intensity scores between the pre- and postintervention groups. Chi-square was used to compare pre- and postintervention nurse documentation of pain-related patient education and whether patients received a pain and palliative care team consultation during their hospitalization. Descriptive statistics, the Wilcoxon signed-rank test, and Fisher’s exact test were used to evaluate changes in nurses’ KAP scores. Demographic data were analyzed using chi-square, Fisher’s exact test, or independent t test, as appropriate. 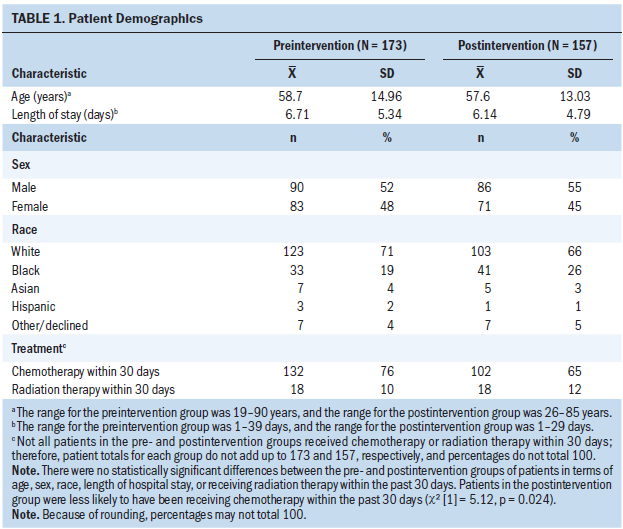
Results
Patient Demographic Data
One hundred and seventy-three hospitalized patients with cancer met criteria for inclusion in the preintervention group, and 157 met criteria for inclusion in the postintervention group. There were no statistically significant differences between the groups in terms of age, sex, race, length of hospital stay, or having received radiation therapy within the past 30 days (see Table 1). However, patients in the postintervention group were less likely to have received chemotherapy within the past 30 days (76% versus 65%, chi-square [1] = 5.12, p = 0.024). There were minor differences in cancer diagnoses between the groups, although this was not statistically significant. More patients in the postintervention group were admitted for fever/infection and respiratory problems, and fewer postintervention patients were admitted for chemotherapy administration (15% versus 8%, chi-square [1] = 3.6, p = 0.058). Detailed cancer and admission diagnosis data are demonstrated in Table 2. 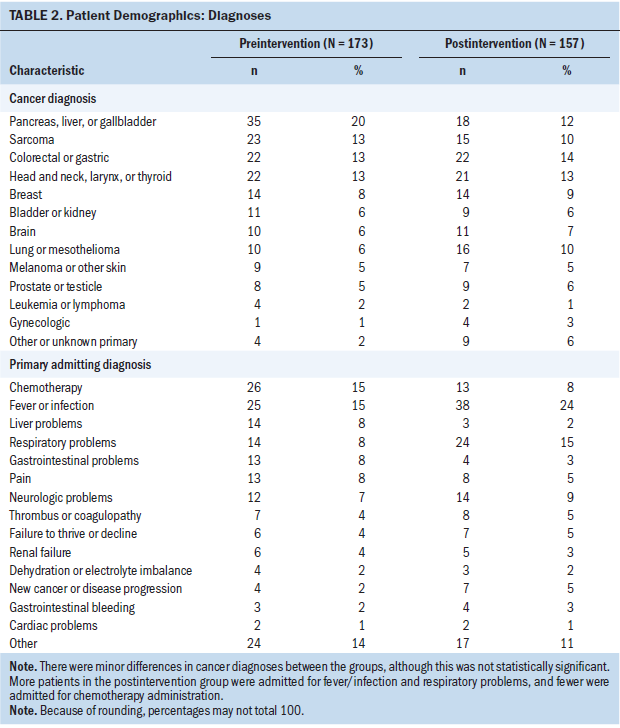
Pain Intensity, Patient Education, and Palliative Care Consultation
No statistically significant differences were noted between first, last, lowest, and highest mean pain scores between the groups (see Table 3), although highest mean pain score was 6.66 in the preintervention group and 6.98 in the postintervention group, and median pain scores were 7 and 8, respectively. This difference may be clinically meaningful. Provision of a pain and palliative care team consultation was documented for 25% of patients in the preintervention group and 29% in the postintervention group (not statistically significant). Pain-related patient education was documented as provided to patients or family members in 76% of the preintervention group and 70% of the postintervention group (not statistically significant). 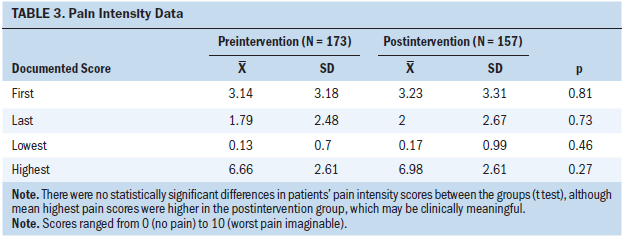
HCAHPS Pain Management Satisfaction Scores
Thirteen patients in the preintervention group and nine in the postintervention group answered the HCAHPS question “How often was your pain well controlled?” Of those, 7 of 13 (54%) and 5 of 9 (56%), respectively, answered “always.” In response to the question “How often did staff do everything to help with your pain?” 8 of 13 (62%) in the preintervention group and 9 of 10 (90%) in the postintervention group answered “always” (Fisher’s exact test, p = 0.179). One patient in the postintervention group did not answer the “pain well-controlled” question.
RN Demographic Data
Eleven (31%) RNs returned preintervention KAP surveys and nine (25%) returned postintervention surveys. Only five RNs completed both surveys; therefore, the pre- and postintervention groups’ demographic data are presented separately (see Table 4). All nurses reported BSN as their highest nursing degree. There were differences between the pre- and postintervention RNs in terms of attendance at end-of-life training (18% versus 0%, respectively) and mean years of experience as an RN at 16.7 (SD = 11.8) in the preintervention group and 9.4 (SD = 12.3) in the postintervention group. These differences were also demonstrated for years of oncology nursing and unit experience. Given the small sample size, these differences were not statistically significant. 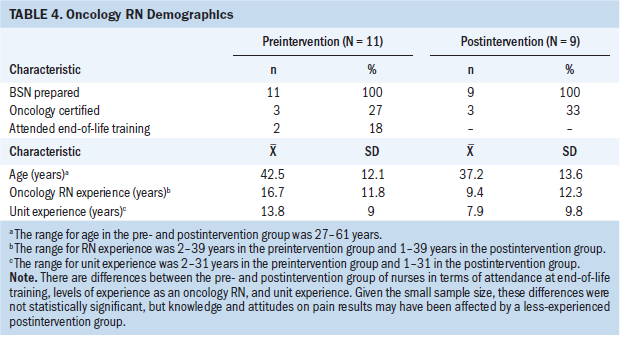
RN Knowledge and Attitudes on Pain Scores
The mean number of questions answered correctly on the KAP survey by the 11 RNs in the preintervention group was 30.6 (SD = 2.46), compared to 30.9 (SD = 2.42) for the 9 RNs representing the postintervention group. Comparison of scores for the five nurses that completed both surveys, using the Wilcoxon signed-rank test for paired data, demonstrated no difference between the median scores. Individual question data were also collected, and of the five questions that were specifically addressed in a follow-up email to staff highlighting pain information, two exhibited meaningful improvement. These were analyzed using Fisher’s exact test. Question 5 assessed RN knowledge on the effectiveness of nonsteroidal anti-inflammatory agents and aspirin on painful bone metastases. The preintervention group nurses scored 36% on the question, and the postintervention group scored 89% (p = 0.025). Question 16 tested knowledge of analgesic dose equivalencies. The preintervention group scored 46% and the postintervention group scored 89% (p = 0.058).
Discussion
The satisfaction with pain management of hospitalized patients with cancer may be improved through implementation of a bundled intervention that addresses staff education, staff behavior, consistent patient education, and a focus on analgesic level maintenance. Combining the various techniques supported by evidence from the literature resulted in improvement of the HCAHPS question addressing staff doing everything to help with pain. Reaching statistical significance with a small sample size was not possible; however, the results were clinically and operationally significant. Although December 2017 was not included in this project, the two patients responding to the “staff did everything” question that month also answered “always.” The project’s results were achieved with patients in the postintervention group demonstrating elevated highest mean pain scores (6.66 versus 6.98) and having a higher percentage of unscheduled, symptom-control admissions (85% preintervention versus 92% postintervention). The HCAHPS question asking how often pain was well-controlled showed minimal improvement, from 54% to 56% answering “always.” Accepting the “staff did everything” question as a proxy for satisfaction with pain management, these findings were consistent with earlier studies demonstrating that satisfaction with pain management can be improved without improving actual pain intensity scores. Of note, actual pain intensity scores were higher in the postintervention group. Fewer patients in the postintervention group were currently receiving chemotherapy (this was statistically significant), which may indicate that patients in the postintervention group had more advanced disease.
Although this difference was not statistically significant, patients in the postintervention group were more likely to have received consultation from the pain and palliative care team (25% in the preintervention group and 29% in the postintervention group). It is not possible, however, to determine whether this was a result of the intervention (patients received instructions to call immediately to request a consultation), having more patients with advanced disease in the postintervention group, or another unknown variable. Provision of a pain and palliative care team consultation was associated with higher pain scores in both groups. Mean highest pain score in the preintervention group was 7.98 (SD = 2.32) for patients receiving consultation and 6.21 (SD = 2.56) for patients who did not have a consultation (t[171] = –4.04, p = 0.000). Similar results were demonstrated in the postintervention group with worst mean pain score of 8.09 (SD = 1.79) for the consultation group and 6.54 (SD = 2.76) for the nonconsultation group (t[123] = –4.16, p = 0.000).
Although RN mean KAP scores were not improved postintervention, meaningful improvement was demonstrated on two important questions addressing the use of non-opioid pain medications to aid in cancer pain relief, and dose conversion of two types of pain medications. Only 5 of 37 questions were specifically addressed postintervention and prior to administration of the KAP postintervention survey. The initial staff education, provided via inservices and written materials, focused on the Pain Stoppers bundle, not specifically on improving nurse knowledge and attitudes on pain, which may explain the lack of improvement in KAP scores. Differences between the pre- and postintervention groups in terms of oncology nursing experience and end-of-life training may also have affected the results. Eighteen percent of RNs in the preintervention group reported fewer than five years of nursing experience compared to 56% in the postintervention group. Although the sample of five RNs taking the survey both pre- and postintervention was small, requiring use of a nonparametric test for statistical analysis, it may be worth noting that the mean score within this group of five RNs improved slightly from 31 (SD = 2.83) to 32.2 (SD = 1.79).
Limitations
This quality improvement project was limited by small sample size to identify a statistically significant improvement in satisfaction with pain management using the HCAHPS pain management questions. The HCAHPS is managed by an outside vendor, and neither the hospital nor the project lead were able to increase the number of surveys sent to patients. In addition, this project is limited by the inability of a pre- and postintervention design to control for confounding variables. Neither the patient nor the RN groups were perfectly similar in the pre- and postintervention samples, possibly affecting results. This quality improvement project focused on patients with solid tumor cancers on one inpatient unit and may not be generalizable to other patient populations. The sample of nurses was experienced and the mean score of the preintervention KAP was higher than expected based on the literature review, providing less opportunity for improvement, and again may not be generalizable to other populations. In addition, the KAP survey was altered from the original, possibly affecting validity and reliability. Lastly, the project implementation date was moved forward by two months when it was discovered, just after institutional review board exemption was obtained, that HCAHPS pain management satisfaction questions were to be changed on January 1, 2018. This led to reduced data collection periods and smaller sample sizes.
Implications for Nursing
This quality improvement project supports the findings of previous studies indicating that RNs are able to improve patients’ pain experience without affecting actual pain intensity scores, and that RNs can influence patients’ satisfaction with how their pain is managed. The Pain Stoppers bundled intervention relied on nursing and support staff approaches to improve patient satisfaction with pain management. Although RNs worked with pharmacy and medical colleagues to optimize the analgesic plan, the intervention did not directly adopt measures to change types of medications or doses of medications given or protocols for ordering and administering analgesics. RNs and support staff were able to improve the pain experience of patients with cancer through the use of evidence-based strategies focused on improving communication about pain and pain management, demonstrating caring behaviors, and providing timely responses; packaging and providing patients with meaningful patient education; and working with the healthcare team to maintain patients’ analgesic levels.
HCAHPS pain satisfaction composite scores, combining two questions asking patients how often their pain was well-controlled and how often staff did everything to control their pain, improved from 58% to 74% of respondents answering “always” following implementation of the Pain Stoppers bundled intervention. Although the HCAHPS sample size was small during the three months preintervention and three months postintervention, the main aim of the project was to improve these scores, and this was achieved. Future studies might be conducted on multiple inpatient units, providing a larger sample size and potential for greater generalizability. Sample size may also be increased by conducting the study during a longer time period. The 2018 HCAHPS satisfaction survey asks patients how often staff talk to them about the amount of pain they have and how often they discuss treatment of their pain. Although these questions cannot be compared to results prior to 2018, they can be used to measure satisfaction with pain management going forward. 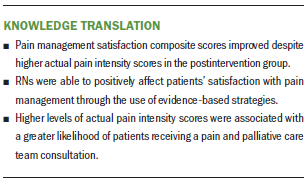
Conclusion
This quality improvement project demonstrated that it is possible to improve patient satisfaction with pain management without necessarily affecting actual pain intensity scores. Higher satisfaction scores were achieved through the efforts of RNs and support staff, without changing the analgesic regimen. Therefore, nurses, in their roles as caregivers, educators, and advocates, can improve the pain experience of hospitalized patients who are diagnosed with a solid tumor cancer.
About the Author(s)
Suzanne M. Cowperthwaite, DNP, RN, NEA-BC, is the director of nursing at the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center in Baltimore, and Sharon L. Kozachik, PhD, RN, FAAN, is an associate professor in the School of Nursing at Johns Hopkins University in Baltimore. During the writing of this article, Kozachik was supported through funding from the Center of Excellence in Pain Education, National Institutes of Health Pain Consortium, and Maryland Higher Education Commission. Cowperthwaite completed the data collection and provided the analysis. Both authors contributed to the conceptualization and design, provided statistical support, and contributed to the manuscript preparation. Cowperthwaite can be reached at suzannecowperthwaite@umm.edu, with copy to ONFEditor@ons.org. (Submitted September 2018. Accepted October 1, 2018.)
References
Alaloul, F., Williams, K., Myers, J., Jones, K.D., & Logsdon, M.C. (2015). Impact of a script-based communication intervention on patient satisfaction with pain management. Pain Management Nursing, 16, 321–327. https://doi.org/10.1016/j.pmn.2014.08.008
American Cancer Society. (2018). Facts about cancer pain. Retrieved from https://www.cancer.org/treatment/treatments-and-side-effects/physical-s…
Bozimowski, G. (2012). Patient perceptions of pain management therapy: A comparison of real-time assessment of patient education and satisfaction and registered nurse perceptions. Pain Management Nursing, 13, 186–193.
Brant, J.M., Mohr, C., Coombs, N.C., Finn, S., & Wilmarth, E. (2017). Nurses’ knowledge and attitudes about pain: Personal and professional characteristics and patient reported pain satisfaction. Pain Management Nursing, 18, 214–223. https://doi.org/10.1016/j.pmn.2017.04.003
Centers for Medicare and Medicaid Services. (2017). HCAHPS hospital survey. Retrieved from https://www.hcahpsonline.org/globalassets/hcahps/survey-instruments/mai…
Comley, A.L., & DeMeyer, E. (2001). Assessing patient satisfaction with pain management through a continuous quality improvement effort. Journal of Pain and Symptom Management, 21, 27–40.
Craig, A.R., Otani, K., & Herrmann, P.A. (2015). Evaluating the influence of perceived pain control on patient satisfaction in a hospital setting. Hospital Topics, 93, 1–8. https://doi.org/10.1080/00185868.2015.1012926
de Rond, M.E., de Wit, R., van Dam, F.S., & Muller, M.J. (2000). A pain monitoring program for nurses: Effects on communication, assessment and documentation of patients’ pain. Journal of Pain and Symptom Management, 20, 424–439.
Dulko, D., Hertz, E., Julien, J., Beck, S., & Mooney, K. (2010). Implementation of cancer pain guidelines by acute care nurse practitioners using an audit and feedback strategy. Journal of the American Academy of Nurse Practitioners, 22, 45–55. https://doi.org/10.1111/j.1745-7599.2009.00469.x
Ferrell, B.R., & McCaffery, M. (2014). Knowledge and attitudes survey regarding pain. Retrieved from http://prc.coh.org/Knowldege%20%20&%20Attitude%20Survey%207-14%20(1).pdf
Giordano, L.A., Elliott, M.N., Goldstein, E., Lehrman, W.G., & Spencer, P.A. (2010). Development, implementation, and public reporting of the HCAHPS survey. Medical Care Research and Review, 67, 27–37. https://doi.org/10.1177/1077558709341065
Glowacki, D. (2015). Effective pain management and improvements in patients’ outcomes and satisfaction. Critical Care Nurse, 35(3), 33–43. https://doi.org/10.4037/ccn2015440
Goldberg, G.R., & Morrison, R.S. (2007). Pain management in hospitalized cancer patients: A systematic review. Journal of Clinical Oncology, 25, 1792–1801. https://doi.org/10.1200/JCO.2006.07.9038
Innis, J., Bikaunieks, N., Petryshen, P., Zellermeyer, V., & Ciccarelli, L. (2004). Patient satisfaction and pain management: An educational approach. Journal of Nursing Care Quality, 19, 322–327.
Jarrett, A., Church, T., Fancher-Gonzalez, K., Shackelford, J., & Lofton, A. (2013). Nurses’ knowledge and attitudes about pain in hospitalized patients. Clinical Nurse Specialist, 27, 81–87.
Keen, A., McCrate, B., McLennon, S., Ellis, A., Wall, D., & Jones, S. (2017). Influencing nursing knowledge and attitudes to positively affect care of patients with persistent pain in the hospital setting. Pain Management Nursing, 18, 137–143. https://doi.org/10.1016/j.pmn.2017.04.002
Kim, E.B., Han, H.S., Chung, J.H., Park, B.R., Lim, S.N., Yim, K.H., . . . Kim, S.T. (2012). The effectiveness of a self-reporting bedside pain assessment tool for oncology inpatients. Journal of Palliative Medicine, 15, 1222–1233.
Lim, S.N., Han, H.S., Lee, K.H., Lee, S.C., Kim, J., Yun, J., . . . Choi, J. (2015). A satisfaction survey on cancer pain management using a self-reporting pain assessment tool. Journal of Palliative Medicine, 18, 225–231. https://doi.org/10.1089/jpm.2014.0021
Muntlin, A., Carlsson, M., Säfwenberg, U., & Gunningberg, L. (2011). Outcomes of a nurse-initiated intravenous analgesic protocol for abdominal pain in an emergency department: A quasi-experimental study. International Journal of Nursing Studies, 48, 13–23. https://doi.org/10.1016/j.ijnurstu.2010.06.003
National Cancer Institute. (2018). Cancer pain (PDQ®)—Health professional version. Retrieved from https://www.cancer.gov/about-cancer/treatment/side-effects/pain/pain-hp…
National Comprehensive Cancer Network. (2018). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Adult cancer pain [v.1.2018]. Retrieved from https://www.nccn.org/professionals/physician_gls/pdf/pain.pdf
National Institute for Health and Care Excellence. (2016). Palliative care for adults: Strong opioids for pain relief. Retrieved from https://www.nice.org.uk/guidance/cg140/chapter/1-recommendations
Sherwood, G., Adams-McNeill, J., Starck, P.L., Nieto, B., & Thompson, C.J. (2000). Qualitative assessment of hospitalized patients’ satisfaction with pain management. Research in Nursing and Health, 23, 486–495. https://doi.org/10.1002/1098-240X(200012)23:6<486::AID-NUR7>3.0.CO;2-5
Sterman, E., Gauker, S., & Krieger, J. (2003). Continuing education: A comprehensive approach to improving cancer pain management and patient satisfaction. Oncology Nursing Forum, 30, 857–864. https://doi.org/10.1188/03.ONF.857-864
Trail-Mahan, T., Heisler, S., & Katica, M. (2016). Quality improvement project to improve patient satisfaction with pain management: Using human-centered design. Journal of Nursing Care Quality, 31, 105–114.
Yildirim, Y.K., Cicek, F., & Uyar, M. (2009). Effects of pain education program on pain intensity, pain treatment satisfaction, and barriers in Turkish cancer patients. Pain Management Nursing, 10, 220–228. https://doi.org/10.1016/j.pmn.2007.09.004
Zoëga, S., Gunnarsdottir, S., Wilson, M.E., & Gordon, D.B. (2016). Quality pain management in adult hospitalized patients: A concept evaluation. Nursing Forum, 51, 3–12. https://doi.org/10.1111/nuf.12085




