Individualized Piano Instruction for Improving Cognition in Breast Cancer Survivors
Purpose: To evaluate the use of individualized piano instruction (IPI) for improving cognition among breast cancer survivors.
Participants & Setting: Six participants were included in an eight-week piano program with three data collection time points at baseline, midpoint, and postintervention. Participants were recruited from the breast cancer clinic of a university cancer center in South Florida.
Methodologic Approach: Neurocognitive, psychosocial, and self-report assessments were conducted to determine potential benefits and program feasibility, including the NIH Toolbox® Cognition Battery, the Functional Assessment of Cancer Therapy (FACT)–Cognitive Function, the FACT-Breast, the Patient Health Questionnaire-9, the Generalized Anxiety Disorder-7, and a participant questionnaire.
Findings: Results related to potential benefits suggest that IPI may significantly improve overall cognition in breast cancer survivors, with fluid cognition showing improvement. In addition, IPI may improve quality of life and self-reported measures of depression and anxiety, with large to moderate effect sizes, respectively.
Implications for Nursing: Nurses should explore different treatment options for chemotherapy-related cognitive impairment and consider including IPI in survivorship care plans.
Jump to a section
The term “chemotherapy-related cognitive impairment” (CRCI) is used to define a toxicity of chemotherapy treatment that affects cognitive abilities. CRCI affects attention, processing speed, executive function, and memory skills in individuals with cancer and survivors (Vannorsdall, 2017). Although it is not uncommon for patients undergoing treatment to have complaints about their cognition, CRCI is often reported to linger after treatment and have long-term effects. A review of CRCI literature suggests that as many as 75% of individuals with cancer had complaints of CRCI, and as many as 35% of them still had unresolved CRCI issues many years following treatment (Janelsins, Kesler, Ahles, & Morrow, 2014). Many cancer survivors complain that CRCI affects their ability to function typically in their work setting, and as many as 13% of cancer survivors cite a decline in their thinking skills as a reason for dropping out of the workforce (Short, Vasey, & Tunceli, 2005).
CRCI in individuals with breast cancer and survivors is well documented, with many studies showing differences in cognition compared to well-matched noncancer controls (Koppelmans et al., 2012; Wefel, Saleeba, Buzdar, & Meyers, 2010). Often, patients with CRCI report issues with executive function and memory (Hodgson, Hutchinson, Wilson, & Nettlebeck, 2013), as well as attention, processing speed (Vannorsdall, 2017), balance, and coordination (Meyers, 2012), among other cognitive skills.
Cognitive impairments following cancer treatment may result from many different factors, like the direct effects of the diagnosis or treatment on the central nervous system, hormonal changes due to postcancer therapies, or incidences of psychological factors, like low mood, and a comorbidity of depression (Biglia et al., 2012), elevated stress, fatigue, anxiety, or other affective symptoms (Vannorsdall, 2017). In addition, a meta-analysis by Hodgson et al. (2012) showed a significant negative relationship between the incidence and severity of CRCI and the length of treatment. CRCI is a multifaceted diagnosis; therefore, multimodal interventions are warranted.
No standard treatment for CRCI exists, but recommendations are often made for pharmacologic and behavioral approaches (Fardell, Vardy, Johnston, & Winocur, 2011). Physicians recommend psychoeducation, behavioral modification, brain training, physical exercise, biofeedback, brain stimulation, or cognitive rehabilitation therapies to ameliorate the impact of CRCI (Vannorsdall, 2017). Choosing an appropriate intervention is dependent on individuals’ preferences, as well as the impact on their daily routine, along with the perceived potential benefits. One option for exercising cognitive skills is music training, particularly playing an instrument like the piano.
The effects of music on cognitive skills in nonclinical populations have been widely explored, with many articles suggesting that musical ability is often associated with enhanced cognition and intellect (Faßhauer, Frese, & Evers, 2015). There have been promising results to support the use of individualized piano instruction (IPI) on improving cognitive skills among children (Jaschke, Honing, & Scherder, 2018) and typical older adults (Bugos, Perlstein, McCrae, Brophy, & Bedenbaugh, 2007; Seinfeld, Figureoa, Ortiz-Gill, & Sanchez-Vives, 2013), with current literature establishing a theoretical framework for cognitive impairment in medical populations such as Parkinson disease (Lesiuk, Bugos, & Murakami, 2018). One population-based co-twin control study by Balbag, Pederson, and Gatz (2014) found that playing a musical instrument, such as the piano, may even serve as a protective factor against dementia. After controlling for sex, education, and physical activity, playing a musical instrument was significantly associated with less likelihood of developing dementia or cognitive impairment (Balbag et al., 2014).
However, no research has been done regarding the use of IPI as a form of cognitive exercise for individuals affected by CRCI, or, therefore, the feasibility of such a program. Considering that support for IPI in improving CRCI is absent from the literature, an exploration of the feasibility of such an approach is warranted. To provide a foundation and effectively implement this intervention, research questions related to feasibility and potential benefits are described. Questions related to feasibility were the following:
• To what extent are breast cancer survivors willing to consent to participating in IPI as a treatment option for CRCI?
• To what extent are breast cancer survivors able to attend sessions for IPI?
• To what extent are breast cancer survivors able to adhere to the homework requirements of IPI?
Research questions related to potential benefits are as follows:
• Are there any changes in the study of neurologic measures?
• Are there any changes in the study of psychosocial measures?
• Are there any self-reported benefits found in the study participant questionnaire responses?
Methods
Participants and Setting
Eligible participants included patients who were diagnosed and treated for breast cancer, six months or more out of active treatment, experiencing cognitive issues (i.e., actively expressed concerns to their physician about struggles with cognitive skills such as memory, attention, executive function, and language), and not currently involved in other brain training or brain exercise programs. Exclusion criteria were as follows:
• Patients in active treatment for breast cancer
• Adults already proficient in piano playing or music theory, and those who play informally or professionally at least once per week
• Adults aged older than 65 years
• Patients diagnosed with a cognitive condition other than CRCI (e.g., Alzheimer disease, Parkinson disease, dementia, amyotrophic lateral sclerosis, autism)
• Adults who did not have functional movements in their hands (as assessed by tendon gliding and finger opposition exercises provided by a physical hand therapist)
Participants were recruited from the breast clinic at the University of Miami Sylvester Comprehensive Cancer Center in Florida. Based on the inclusion and exclusion criteria, along with potential participants’ interest level, the clinic staff forwarded the potential participants’ contact information to the co–principal investigator to schedule an initial meeting. This initial meeting was meant to consent the participant into the study and took place in a private office at the cancer center; it lasted about 30 minutes. The consent meeting usually occurred on the same day as a follow-up appointment at the breast clinic, but some participants made a special visit to the center for the meeting. The potential participant received study details, along with a thorough reading of the consent form, which was approved by the institutional review board for the University of Miami. Once the participants fully understood all requirements and procedures, they were scheduled to return the following week to begin the intervention.
Methodologic Approach
This feasibility study was designed as a first step in developing and testing the IPI intervention. Using the Herholzolz and Zatorre (2012) review as a model, the researchers theorized that IPI could improve cognitive measures in musically naive individuals because of the complex nature of learning a musical skill, understanding that musical training can integrate several sensory systems. The researchers theorized that this cognitive challenge may effectively exercise the participants’ affected cognitive skills, while also motivating them to continue the practice because of the social–emotional motivators found in playing music (Herholzolz & Zatorre, 2012). Participants were enrolled in an eight-week program comprised of weekly piano sessions, with three of those weeks also incorporating cognitive and psychosocial assessments at baseline, midpoint, and postintervention. At week 1, participants completed an electronic demographic survey and cognitive, quality-of-life, and mood assessments. In addition, they received their first piano lesson, a piano keyboard on loan, and piano lesson books to take home. At this point, they were scheduled to return weekly for an hour-long lesson. At week 4 (midpoint), participants completed the same assessments as in week 1 (baseline), as well as a program feasibility questionnaire; they also received their weekly piano session.
Participants continued with weekly sessions until week 8, when a final postintervention session was held. Participants again completed the same assessments and completed a final program feedback questionnaire. Assessment measures, collected at baseline, midpoint, and postintervention, were administered via an iPad with encrypted and password-protected software; each assessment session took about 50–60 minutes to complete, with breaks in between the cognitive and psychosocial measures.
Measures
To quantify the impact of IPI on CRCI, study measures included the NIH Toolbox® Cognitive Battery (NIHTB-CB); the Functional Assessment of Cancer Therapy (FACT)–Breast (FACT-B), version 4.0; the FACT–Cognitive Function (FACT-Cog), version 3.0; the Generalized Anxiety Disorder-7 (GAD-7); the Patient Health Questionnaire-9 (PHQ-9); and a researcher-designed demographics questionnaire.
NIHTB-CB: The NIHTB-CB was comprised of seven tests that measured fluid and crystallized neurocognitive abilities on five subdomains (executive function and attention, processing speed, episodic memory, working memory, and language). Fluid neurocognitive abilities are viewed as the capacity to learn and process new information in novel situations, peak in early adulthood, and decline with age (Gray, Chabris, & Braver, 2003). Crystallized abilities develop in childhood and progress with greater age and experience (Blair, 2006). Weintraub et al. (2014) and Heaton et al. (2014) provided in-depth descriptions of each NIHTB-CB subscale assessment. The battery yielded three cognitive composite scores, labeled fluid, crystallized, and total cognitive function. The fluid, crystallized, and total cognition scores have high test-retest reliability (r = 0.89) and sturdy convergent (r = 0.84) and discriminant (r = 0.29) validities in adults (Casaletto et al., 2015; Heaton et al., 2014; Weintraub et al., 2014).
FACT-B: The FACT-B is a 36-item questionnaire that assesses five domains of cancer treatment–related quality of life: physical well-being, social/family well-being, emotional well-being, functional well-being, and one disease-specific domain (additional concerns) (Brady et al., 1997). Higher scores indicate greater quality of life. Internal consistency for the FACT-B total score is high (r = 0.9), and the alpha coefficients for the subscales range from 0.63 to 0.86 (Pandey, Thomas, Ramdas, Eremenco, & Nair, 2002). In addition, high test-retest reliability was demonstrated for the FACT-B total score (r = 0.85). The FACT-B has been shown to discriminate patients with breast cancer from patients without breast cancer and is correlated with quality-of-life measures, as demonstrated by its convergent (r = 0.57) and divergent (r = 0.7) validity (Brady et al., 1997).
FACT-Cog: The FACT-Cog is a 33-item questionnaire that assesses four domains of cancer treatment–related perceived cognitive disturbances: perceived cognitive impairments, impact of perceived cognitive impairments on quality of life, deficits observed or commented on by others, and perceived cognitive abilities (Vardy et al., 2006). Higher scores indicate greater quality of life. The instrument has demonstrated that FACT-Cog total scores are validated strongly with measures of cognition in a sample with breast cancer (r = 0.73) (Cheung, Lim, Shwe, Tan, & Chan, 2013), with high internal consistency (r = 0.71–0.93) and satisfactory test-retest reliability (r = 0.76) (Wagner, Sweet, Butt, Lai, & Cella, 2009).
GAD-7: The GAD-7 is a seven-item self-report anxiety scale that measures severity of generalized anxiety disorder symptoms during a two-week period (Spitzer, Kroenke, Williams, & Löwe, 2006). Participants indicate on a four-point Likert-type scale the frequency in which the items applied to them within the past two weeks, with 0 indicating not at all, 1 indicating several days, 2 indicating more than half of the days, and 3 indicating nearly every day. Total scale scores are summed, in which scoring thresholds of 5, 10, and 15 indicate mild, moderate, and severe anxiety, respectively. The GAD-7 has demonstrated strong internal consistency (r = 0.92), high test-retest reliability (r = 0.83), and good validity in patients with cancer (Esser et al., 2018) and the general population (Löwe et al., 2008).
PHQ-9: The PHQ-9 is a nine-item self-report scale that measures symptoms of depression severity during a two-week period (Kroenke & Spitzer, 2002; Kroenke, Spitzer, & Williams, 2001). Total scale scores are summed, in which scoring thresholds of 5, 10, 15, and 20 indicate mild, moderate, moderately severe, and severe depression, respectively. The scale has high internal consistency (0.86–0.88) and high test-retest reliability (0.84–0.95) (Kroenke et al., 2001; Löwe et al., 2004); it also has good validity in patients with cancer and the general population (Hinz et al., 2016; Thekkumpurath et al., 2011).
Participant Questionnaire
The researchers developed a self-report questionnaire to assess participants’ perceptions about their cognition and the program’s feasibility and acceptability. This questionnaire acted as a general program evaluation and included participants’ demographic information and program applicability (the amount of time for piano practice per day and any barriers to piano practice). Participants also provided program evaluation by rating items, such as the effectiveness of the program, how enjoyable it was, and their mood while enrolled. Total scores were summed for each individual statement, in which higher scores indicated greater perceived cognitive ability, program feasibility, and acceptability. The questionnaire provided the basis to interpret and answer the questions related to feasibility to proceed to a main study (Bowen et al., 2009; Thabane et al., 2010).
Intervention
The IPI intervention was developed and implemented by a board-certified music therapist at the cancer center. The program was designed to adapt to the learning styles and baseline cognitive functioning of each participant. Although all participants followed the same eight-week lesson plan, the progress of each participant was dependent on attendance, ability to adhere to practice recommendations, and manifestation of cognitive health (e.g., stress level, ability to focus, ability to retain information and acquire new knowledge). The IPI intervention was modeled from past studies that have explored the impact of piano playing on cognition (Bugos et al., 2007; Seinfeld et al., 2013), as well as basics in music education and standards of practice in acquiring piano knowledge (Palmer, Manus, & Lethco, 2011). Each hour-long intervention session consisted of the following:
• Part 1: A warm-up period of playing seven major scales; playing the I, IV, and V chords of these scales; and playing five-finger exercises from A Dozen a Day (Burnam, 1950)
• Part 2: Working through Alfred’s Basic Adult All-in-One Course, which taught music theory concurrently with piano skills (Palmer et al., 2011)
• Part 3: A participant-chosen music piece in any musical style
Each section was meant to target a different area of cognition. Parts 1 and 2 allowed participants to exercise attention, different types of memory (working, short-term, and long-term), processing speed, and executive functioning skills, while integrating different sensory and motor systems. Part 3 was meant to integrate all previously stated skills while increasing motivation, elevating mood, and allowing for sharing of musical experiences with family and loved ones. This intervention was designed as a multimodal approach to exercising cognitive skills affected by cancer treatment.
During each session, participants were assigned homework and were instructed to practice at least 20 minutes per day. Each week, the participants were challenged to incrementally increase their knowledge and ability on the piano. In addition, the participants were taught strategies to acquire and retain knowledge on piano techniques, as well integrate piano playing into their daily routine. The sessions took place in a private room either in an office or a meeting room of the cancer center. The participants used the same piano keyboard for each lesson.
Data Analysis
Frequency counts were used to evaluate the distribution of demographic variables, such as country of origin, language, ethnicity, race, education, relationship status, and gender. Items that measured feasibility were also evaluated using frequency counts for data collected at the midpoint and at study completion. Baseline, midpoint, and postintervention neurocognitive assessments were analyzed using within-subjects analysis of variance to compare data across the three time points. In addition, paired sample t tests were used to compare pre- and postintervention data to include data from one additional participant who did not complete the midpoint assessment.
Although the sample was small, analyses on the longitudinal outcome data were conducted to estimate effect sizes, which may be used to power a future randomized trial. Effect size measures using Cohen’s d were calculated for all neurocognitive assessments and the self-report assessments comparing baseline and postintervention time points. Cohen’s d of 0.2 is considered a small effect, 0.5 is considered a moderate effect, and 0.8 is considered a large effect (Cohen, 1977).
Findings
Participant Characteristics
The majority of individuals interested in participating in the study qualified for inclusion (6 of 11). Participants were excluded for not meeting certain treatment criteria, not being able to adhere to the requirements of the piano lessons, or not being able to fit the lessons into their weekly schedule. However, among the participants who qualified for inclusion, there was a consent rate of 100% (i.e., all six participants who qualified consented). In addition, those who were excluded stated a willingness to pay for the program should it become available to the general population. Data were collected from all six participants. Table 1 summarizes the demographic characteristics of the sample. Most participants were born in the United States, spoke English, and were college educated. Although all participants were Caucasian women, two identified as Hispanic or Latino. 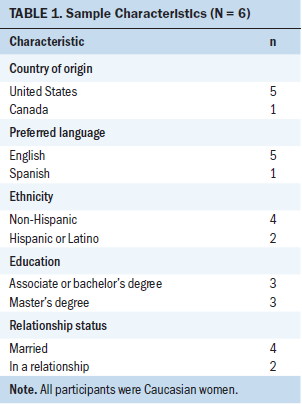
Acceptability
Most participants (four of six) successfully attended all eight required piano sessions. Participants who were unable to adhere to the attendance requirement cited scheduling conflicts as the main reason. Conversely, most participants (four of six) were able to complete all three data collection sessions. One participant missed one assessment session but continued with the remaining weeks until completion. Therefore, this participant completed the baseline and postintervention assessment only. Another participant cited a busy work schedule, was lost to follow-up after the baseline assessment, and was not able to complete any further sessions.
All participants rated the program as either good (n = 3) or outstanding (n = 2). They also found the program to be enjoyable, with one participant indicating that her level of enjoyment was good and four participants rating their level of enjoyment as outstanding. Regarding their mood as a result of participating in the program, two participants rated their mood as neutral, one rated her mood as positive, and two rated their mood as very positive. Participants were also asked to rate how confident they were in their ability to learn to play the piano. Two participants were neutral, two were very confident, and one was extremely confident. In addition, they all agreed that the program helped teach them the basics, with two participants saying “yes” and three saying “definitely yes.” They also all noted an improvement in their cognitive functioning, with four participants indicating that their cognitive function was better and one participant rating her cognitive improvement as noticeably better.
At study completion, participants were asked to rate how often they practiced piano and what factors impeded or facilitated their ability to practice piano. When asked about how many minutes they practiced piano per day, two participants said 5 to 10 minutes and three said they practiced 20 or more minutes per day. Factors that impeded the participants’ ability to practice included family/household responsibilities (n = 5) and physical symptoms (n = 1). Factors that facilitated practice included enjoying the music they played (n = 5), being motivated to learn (n = 3), feeling successful at playing (n = 3), and noticing improvement in cognitive function (n = 3). In addition, when asked how easily the program fit into their daily routine, four participants indicated that it fit somewhat easily. Although only one participant said it was not very easy to attend the weekly lessons, most participants indicated that it was somewhat (n = 3) or very (n = 1) easy to attend.
Potential Cognitive and Psychosocial Benefits
Table 2 shows the mean and standard deviation for the cognitive scores from the NIHTB-CB at baseline, midpoint, and postintervention. Total cognitive function showed significant improvement from baseline to postintervention, with a Cohen’s d of 1, and fluid cognitive function demonstrating a larger effect (d = 1.42) compared to crystallized cognitive function (d = 0.4). Higher scores are indicative of improved outcomes or better cognitive functioning in total, fluid, and crystallized cognition. 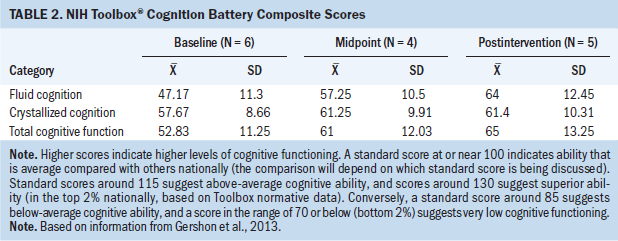
Psychosocial benefits and self-report measures are shown in Table 3. The FACT–Trial Outcome Index yielded a moderate effect when comparing baseline to postintervention (d = 0.69); FACT-B total demonstrated a moderate effect (d = 0.72); and the FACT-General total demonstrated a moderate effect (d = 0.56). Higher scores are indicative of better quality-of-life reports. FACT-Cog scores revealed a very large effect on perceived cognitive impairments (d = 2.18), a large effect on comments from others (d = 1.14), a moderate effect on perceived cognitive abilities (d = 0.56), and a very large effect on impact of perceived cognitive impairments on quality of life (d = 1.48). Higher scores indicate better quality-of-life reports. A moderate effect was found on anxiety from the GAD-7 (d = 0.69), and a large effect was found on depression from the PHQ-9 assessment (d = 1.24). Lower scores are indicative of lower anxiety and depression ratings from the participants. 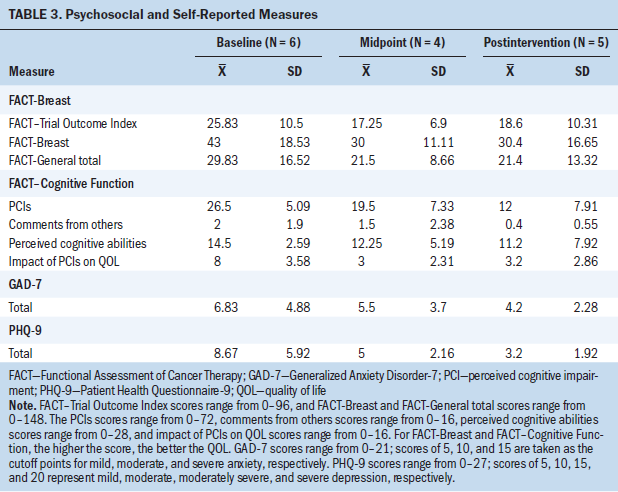
Discussion
Based on the evidence regarding the effect of music training on neuroplasticity (Herholz & Zatorre, 2012), acquiring piano skills was theorized to improve scores on standardized cognitive assessments, as well as improve other quality-of-life and mood measures for breast cancer survivors. Learning a musical instrument changes structural and functional properties of the brain, while also affecting new short-term learning and plasticity (Herholz & Zatorre, 2012). Therefore, learning the piano could potentially improve cognitive abilities affected by CRCI, like fluid cognition. Because changes in neuroplasticity are related to training effects, it was important to determine how often the participants were engaging in IPI outside of the weekly sessions to determine its feasibility. Program feasibility was explored through analysis of participant adherence and self-reporting of program acceptability. Results related to program feasibility and potential benefits for improving cognition and quality-of-life measures were generally favorable.
Program Feasibility
Feasibility was achieved through parameters such as a high consent rate, high number of completed sessions, positive adherence to homework requirements, and the generally favorable ratings in the program questionnaire. However, the IPI program within this population was not without its challenges. Enrolled participants found it difficult to adhere to attendance to the weekly sessions; often, scheduling was flexible for participants to complete the sessions. Although most participants were adherent to attendance to the sessions, the impact of complicated work and personal lives for breast cancer survivors cannot be disregarded. To apply this program effectively, a flexible delivery of IPI may be required. Virtual music lessons and therapy are becoming more popular among clinical populations because many patients are unable to attend in-person sessions (Lightstone, Bailey & Voros, 2018). Cancer survivors may explore a telemedicine approach to engaging in IPI weekly, or the program can be redesigned as a self-taught course with weekly follow-up telephone calls.
Potential Cognitive and Psychosocial Benefits
Results for the NIHTB-CB measures trended positively, with improvement in all composite scores, but showed a significant difference in the total cognition score and a large effect size for the fluid cognition subscale. It is promising to see that fluid cognition was improved by IPI. Fluid cognition is the capacity to learn and process new information in novel situations, independent of acquired knowledge. Fluid cognition is central to theories of human intelligence (Ferrer, O’Hare, & Bunge, 2009); therefore, it is an important set of skills to address when it comes to cognitive impairment. Although the impact of these improvements is minimal because of the extremely small sample size, the positive trend found across the time points is promising. Finally, these results align with past studies that have demonstrated improvements in cognition through piano playing for typical adults (Faßhauer et al., 2015; George & Coch, 2011) and older adults (Bugos et al., 2007; Seinfeld et al., 2013), and improving attention and mood among other breast cancer survivors (Lesiuk, 2015). These results also illustrate IPI’s ability to show improvements in cognition in a cancer treatment etiology.
The current study assessed known psychosocial factors that influence CRCI to determine if these were also affected by IPI. From the FACT-Cog results, large effect sizes found in perceived cognitive impairments, comments from others, and the impact of these impairments on their quality of life are noteworthy. Individuals’ self-perception of their cognitive abilities is sometimes as important as their scores on objective neurocognitive testing (Janelsins et al., 2014). For many survivors, perceived cognitive impairment was noticeably better after completing the intervention. In addition, these self-perceived improvements were corroborated by the results of the NIHTB-CB scores. The improvement in self-perception of cognitive abilities is a good indicator of IPI’s acceptability as an intervention for CRCI within this population.
The results of this study also support the theory that engaging in IPI may reduce feelings of depression and anxiety, with large and moderate effect sizes found, respectively. Individuals with breast cancer may perceive their cognitive decline as worse if they have a comorbidity of depression or anxiety (Biglia et al., 2012), and this negative perception may hinder their ability to effectively manage their impairment. Music therapy has been shown to positively affect depression (Aalbers et al., 2017) and anxiety in oncology care (Rossetti et al., 2017). This study supports this knowledge, while highlighting the need for further research into the role of IPI in addressing psychosocial measures that may affect CRCI. Understanding the relationship among depression, anxiety, mood, quality of life, and the severity of CRCI (Nelson, Nandy, & Roth, 2007), it is noteworthy to highlight IPI’s ability to address cognitive and psychosocial goals within one intervention.
Limitations
A homogeneous and small sample size, along with challenges with attendance to the IPI sessions, impedes the generalization of these results. A larger sample size is needed to confidently state the feasibility of the IPI intervention, along with the veracity of the potential cognitive and psychosocial benefits of the intervention. Staffing changes made it difficult to continue the study to achieve a larger sample size, and focusing on the breast cancer diagnosis also limited the diversity of the sample. In effect, the small sample can be attributed to institutional complications and is not related to the interest in the IPI program from the general population.
Although most enrolled participants were able to complete the required piano and assessment sessions, they all needed flexibility in scheduling to accommodate work and life events. To effectively apply any cognitive training intervention, the program must be designed to tackle the most common barriers to attendance, such as transportation, scheduling conflicts, and the traditional in-person intervention.
This program received high acceptability ratings partially because it was offered at no cost to participants. The free sessions and materials made it easier for participants to agree to participate and adhere to practice requirements. Survivors who do not have access to music therapy services in their survivorship programs may have to absorb these costs, which may become a barrier to regular cognitive exercise.
Implications for Nursing
As many as 35% of individuals with cancer report cognitive impairment following cancer treatment (Janelsins et al., 2014), and many women with breast cancer report issues with short-term memory, focus, word retrieval, reading, and driving (Meyers, 2012). In the 2005 Institute of Medicine report From Cancer Patient to Cancer Survivor: Lost in Transition (Hewitt, Greenfield, & Stovall, 2005), specific recommendations were directed to individuals with cancer, their advocates, and their healthcare providers. Included in the recommendations was for healthcare providers to ensure delivery of appropriate survivorship care and develop a clear survivorship care plan (SCP) (Nekhlyudov, Ganz, Arora, & Rowland, 2017). Nurses play a significant role in developing and implementing the SCP. Nurses at all levels of care who interact with individuals with breast cancer, survivors exhibiting symptoms of CRCI, or those self-reporting issues with cognition are encouraged to learn about treatment options available to address these issues and incorporate them into the patients’ SCP. Understanding the positive effects of piano playing on cognition (Balbag et al., 2014; Bugos et al., 2007; Pantev, Lappe, Herholz, & Trainor, 2009), nurses are encouraged to provide patients with the information that playing a musical instrument may serve as a good cognitive exercise during and following treatment.
This feasibility study incorporated advanced RN practitioners as the primary participant referral source, because they are the first line of outpatient care who could identify CRCI and make appropriate referrals. A best practice for nurses along the continuum of patient care is providing patient education based on the most current evidence-based practice information available. This study highlights the importance of further research into this area, while also allowing for patients to immediately engage in a cognitive exercise that is nonpharmaceutical, noninvasive, and cognitively challenging. Nurses are encouraged to include, within appropriate patient SCPs, education on IPI that may improve cognition and other psychosocial parameters. [[{"fid":"52701","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
Conclusion
IPI was determined to be a feasible intervention for addressing CRCI concerns among breast cancer survivors. The eight-week program’s feasibility was established through analysis of participant adherence to attendance and homework requirements, and self-reporting of program acceptability and applicability. Potential cognitive and psychosocial benefits were assessed through standardized neurocognitive testing; quality-of-life, depression, and anxiety instruments; and a researcher-designed questionnaire. Despite a small and homogeneous sample, the participant ratings suggest IPI is an acceptable and applicable intervention for CRCI among breast cancer survivors. Neurocognitive and psychosocial measures support IPI as a complex intervention that is able to address the cognitive deficits and psychosocial ramifications of CRCI. The favorable results related to program feasibility and potential benefits for improving cognition and psychosocial measures support further research into the use of IPI as an effective cognitive rehabilitation intervention for managing CRCI among breast cancer survivors. Future research must include a larger and more representative sample, while also addressing the common barriers to IPI, which include regular attendance or inability to travel for sessions and monetary costs associated with not having access to music therapy services as a part of survivorship care.
The authors gratefully acknowledge Vanessa Perez, ARNP, and Marc E. Lippman, MD, for identifying potential participants for this study. The authors also gratefully acknowledge Mary A. Kauffman, MT-BC, for implementing the piano intervention with some participants.
About the Author(s)
Marlen Rodriguez-Wolfe, MM, MT-BC, is a music therapist and independent scholar in Querétaro, México; Debbie Anglade, PhD, RN, MSN, LHRM, CPHQ, CCM, is an assistant professor of clinical and Jonas Nurse Leaders Scholar Alumnus and Karina A. Gattamorta, PhD, is a research associate professor, both at the School of Nursing and Health Studies, and William B. Hurwitz, MA, is a clinical research associate in the Sylvester Comprehensive Cancer Center, all at the University of Miami in Florida; and William F. Pirl, MD, MPH, is the Vice Chair for Psychosocial Oncology in Psychosocial Oncology and Palliative Care at the Dana-Farber Cancer Institute at Harvard Medical School in Boston, MA. No financial relationships to disclose. Rodriguez-Wolfe, Anglade, and Pirl contributed to the conceptualization and design. Anglade, Hurwitz, and Pirl completed the data collection. Anglade, Gattamorta, and Hurwitz provided statistical support. Anglade and Gattamorta provided the analysis. All authors contributed to the manuscript preparation. Rodriguez-Wolfe can be reached at marlen.rod@gmail.com, with copy to ONFEditor@ons.org. (Submitted October 2018. Accepted March 8, 2019.)
References
Aalbers, S., Fusar-Poli, L., Freeman, R.E., Spreen, M., Ket, J.C., Vink, A.C., . . . Gold, C. (2017). Music therapy for depression. Cochrane Database of Systematic Reviews, 11, CD004517. https://doi.org/10.1002/14651858.CD004517.pub3
Balbag, M.A., Pedersen, N.L., & Gatz, M. (2014). Playing a musical instrument as a protective factor against dementia and cognitive impairment: A population-based twin study. International Journal of Alzheimer’s Disease, 2014(Suppl. 4), 836748. https://doi.org/10.1155/2014/836748
Biglia, N., Bounous, V.E., Malabaila, A., Palmisano, D., Torta, D.M., D’Alonzo, M., . . . Torta, R. (2012). Objective and self-reported cognitive dysfunction in breast cancer women treated with chemotherapy: A prospective study. European Journal of Cancer Care, 21, 485–492. https://doi.org/10.1111/j.1365-2354.2011.01320.x
Blair, C. (2006). How similar are fluid cognition and general intelligence? A developmental neuroscience perspective on fluid cognition as an aspect of human cognitive ability. Behavioral and Brain Sciences, 29, 109–125. https://doi.org/10.1017/S0140525X06009034
Bowen, D.J., Kreuter, M., Spring, B., Cofta-Woerpel, L., Linnan, L., Weiner, D., . . . Fernandez, M. (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36, 452–457. https://doi.org/10.1016/j.amepre.2009.02.002
Brady, M.J., Cella, D.F., Mo, F., Bonomi, A.E., Tulsky, D.S., Lloyd, S.R., . . . Shiomoto, G. (1997). Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. Journal of Clinical Oncology, 15, 974–986. https://doi.org/10.1200/JCO.1997.15.3.974
Bugos, J.A., Perlstein, W.M., McCrae, C.S., Brophy, T.S., & Bedenbaugh, P.H. (2007) Individualized piano instruction enhances executive functioning and working memory in older adults. Aging and Mental Health, 11, 464–471. https://doi.org/10.1080/13607860601086504
Burnam, E.M. (1950). A dozen a day: Technical exercises for the piano to be done each day before practicing. Cincinnati, OH: Willis Music.
Casaletto, K.B., Umlauf, A., Beaumont, J., Gershon, R., Slotkin, J., Akshoomoff, N., & Heaton, R.K. (2015). Demographically corrected normative standards for the English version of the NIH Toolbox Cognition Battery. Journal of the International Neuropsychological Society, 21, 378–391. https://doi.org/10.1017/S1355617715000351
Cheung, Y.T., Lim, S.R., Shwe, M., Tan, Y.P., & Chan, A. (2013). Psychometric properties and measurement equivalence of the English and Chinese versions of the Functional Assessment of Cancer Therapy-Cognitive in Asian patients with breast cancer. Value in Health, 16, 1001–1013. https://doi.org/10.1016/j.jval.2013.06.017
Cohen, J. (1977). Statistical power analysis for the behavioral sciences (Rev. ed.). New York, NY: Academic Press.
Esser, P., Hartung, T.J., Friedrich, M., Johansen, C., Wittchen, H.U., Faller, H., . . . Mehnert, A. (2018). The Generalized Anxiety Disorder Screener (GAD-7) and the anxiety module of the Hospital and Depression Scale (HADS-A) as screening tools for generalized anxiety disorder among cancer patients. Psycho-Oncology, 27, 1509–1516. https://doi.org/10.1002/pon.4681
Faßhauer, C., Frese, A., & Evers, S. (2015). Musical ability is associated with enhanced auditory and visual cognitive processing. BMC Neuroscience, 16, 59. https://doi.org/10.1186/s12868-015-0200-4
Fardell, J.E., Vardy, J., Johnston, I.N., & Winocur, G. (2011).Chemotherapy and cognitive impairment: Treatment options. Clinical Pharmacology and Therapeutics, 90, 366–376. https://doi.org/10.1038/clpt.2011.112
Ferrer, E., O’Hare, E.D., & Bunge, S.A. (2009). Fluid reasoning and the developing brain. Frontiers in Neuroscience, 3(1), 46–51. https://doi.org/10.3389/neuro.01.003.2009
George, E.M., & Coch, D. (2011). Music training and working memory: An ERP study. Neuropsychologia, 49, 1083–1094. https://doi.org/10.1016/j.neuropsychologia.2011.02.001
Gershon, R.C., Wagster, M.V., Hendrie, H.C., Fox, N.A., Cook, K. F., & Nowinski, C.J. (2013). NIH Toolbox for assessment of neurological and behavioral function. Neurology, 80(11 Suppl. 3), S2–S6. https://doi.org/10.1212/WNL.0b013e3182872e5f
Gray, J.R., Chabris, C.F., & Braver, T.S. (2003). Neural mechanisms of general fluid intelligence. Nature Neuroscience, 6, 316–322. https://doi.org/10.1038/nn1014
Heaton, R.K., Akshoomoff, N., Tulsky, D., Mungas, D., Weintraub, S., Dikmen, S., . . . Gershon, R. (2014). Reliability and validity of composite scores from the NIH Toolbox Cognition Battery in adults. Journal of the International Neuropsychological Society, 20, 588–598. https://doi.org/10.1017/S1355617714000241
Herholzolz, S.C., & Zatorre, R.J. (2012). Musical training as a framework for brain plasticity: Behavior, function, and structure. Neuron, 76, 486–502. https://doi.org/10.1016/j.neuron.2012.10.011
Hewitt, M., Greenfield, S., & Stovall, E. (Eds.) (2005). From cancer patient to cancer survivor: Lost in transition. Washington, DC: National Academies Press.
Hinz, A., Mehnert, A., Kocalevent, R.D., Brähler, E., Forkmann, T., Singer, S., & Schulte, T. (2016). Assessment of depression severity with the PHQ-9 in cancer patients and in the general population. BMC Psychiatry, 16, 22. https://doi.org/10.1186/s12888-016-0728-6
Hodgson, K.D., Hutchinson, A.D., Wilson, C.J., & Nettlebeck, T. (2013). A meta-analysis of the effects of chemotherapy on cognition in patients with cancer. Cancer Treatment Reviews, 39, 297–304. https://doi.org/10.1016/j.ctrv.2012.11.001
Janelsins, M.C., Kesler, S.R., Ahles, T.A., & Morrow, G.R. (2014). Prevalence, mechanisms, and management of cancer-related cognitive impairment. International Review of Psychiatry, 26, 102–113. https://doi.org/10.3109/09540261.2013.864260
Jaschke, A.C., Honing, H., & Scherder, E.J.A. (2018). Longitudinal analysis of music education on executive functions in primary school children. Frontiers in Neuroscience, 12, 103. https://doi.org/10.3389/fnins.2018.00103
Koppelmans, V., Breteler, M.M., Boogerd, W., Seynaeve, C., Gundy, C., & Schagen, S.B. (2012). Neuropsychological performance in survivors of breast cancer more than 20 years after adjuvant chemotherapy. Journal of Clinical Oncology, 30, 1080–1086. https://doi.org/10.1200/JCO.2011.37.0189
Kroenke, K., & Spitzer, R.L. (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32, 509–515.
Kroenke, K., Spitzer, R.L., & Williams, J.B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613.
Lesiuk, T. (2015). The effect of mindfulness-based music therapy on attention and mood in women receiving adjuvant chemotherapy for breast cancer: A pilot study. Oncology Nursing Forum, 42, 276–282. https://doi.org/10.1188/15.ONF.276-282
Lesiuk, T., Bugos, J.A., & Murakami, B. (2018). A rationale for music training to enhance executive functions in Parkinson’s disease: An overview of the problem. Healthcare, 6, E35. https://doi.org/10.3390/healthcare6020035
Lightstone, A.J., Bailey, S.K., & Voros, P. (2015). Collaborative music therapy via remote video technology to reduce a veteran’s symptoms of severe, chronic PTSD. Arts and Health, 7(12), 123–136. https://doi.org/10.1080/17533015.2015.1019895
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Herzberg, P.Y. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 46, 266–274. https://doi.org/10.1097/MLR.0b013e318160d093
Löwe, B., Spitzer, R.L., Gräfe, K., Kroenke, K., Quenter, A., Zipfel, S., . . . Herzog, W. (2004). Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. Journal of Affective Disorders, 78, 131–140. https://doi.org/10.1016/S0165-0327(02)00237-9
Meyers, J.S. (2012). Chemotherapy-related cognitive impairment: The breast cancer experience [Online exclusive]. Oncology Nursing Forum, 39, E31–E40. https://doi.org/10.1188/12.ONF.E31-E40
Nekhlyudov, L., Ganz, P.A., Arora, N.K., & Rowland, J.H. (2017). Going beyond being lost in transition: A decade of progress in cancer survivorship. Journal of Clinical Oncology, 35, 1978–1981. https://doi.org/10.1200/JCO.2016.72.1373
Nelson, C.J., Nandy, N., & Roth, A.J. (2007). Chemotherapy and cognitive deficits: Mechanisms, findings, and potential interventions. Palliative and Supportive Care, 5, 273–280. https://doi.org/10.1017/S1478951507000442
Palmer, W.A., Manus, M., & Lethco, A.V. (2011). Alfred’s basic adult all-in-one course: Lesson, theory, technic. Van Nuys, CA: Alfred Publishing Company.
Pandey, M., Thomas, B.C., Ramdas, K., Eremenco, S., & Nair, M.K. (2002). Quality of life in breast cancer patients: Validation of a FACT-B Malayalam version. Quality of Life Research, 11(2), 87–90. https://doi.org/10.1023/A:1015083713014
Pantev, C., Lappe, C., Herholz, S.C., & Trainor, L. (2009). Auditory-somatosensory integration and cortical plasticity in musical training. Annals of the New York Academy of Sciences, 1169, 143–150. https://doi.org/10.1111/j.1749-6632.2009.04588.x
Rossetti, A., Chadha, M., Torres, B.N., Lee, J.K., Hylton, D., Loewy, J.V., & Harrison, L.B. (2017). The impact of music therapy on anxiety in cancer patients undergoing simulation for radiation therapy. International Journal of Radiation Oncology, Biology, Physics, 99, 103–110. https://doi.org/10.1016/j.ijrobp.2017.05.003
Seinfeld, S., Figueroa, H., Ortiz-Gill, J., & Sanchez-Vives, M.V. (2013). Effects of music learning and piano practice on cognitive function, mood, and quality of life in older adults. Frontiers in Psychology, 4, 810. https://doi.org/10.3389/fpsyg.2013.00810
Short, P.F., Vasey, J.J., & Tunceli, K. (2005). Employment pathways in a large cohort of adult cancer survivors. Cancer, 103, 1292–1301. https://doi.org/10.1002/cncr.20912
Spitzer, R.L., Kroenke, K., Williams, J.B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166, 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Thabane, L., Ma, J., Chu, R., Cheng, J., Ismaila, A., Rios, L.P., . . . Goldsmith, C.H. (2010). A tutorial on pilot studies: The what, why and how. BMC Medical Research Methodology, 10, 1. https://doi.org/10.1186/1471-2288-10-1
Thekkumpurath, P., Walker, J., Butcher, I., Hodges, L., Kleiboer, A., O’Connor, M., . . . Sharpe, M. (2011). Screening for major depression in cancer outpatients: The diagnostic accuracy of the 9-item patient health questionnaire. Cancer, 117, 218–227. https://doi.org/10.1002/cncr.25514
Vannorsdall, T.D. (2017). Cognitive changes related to cancer therapy. Medical Clinics of North America, 101, 1115–1134. https://doi.org/10.1016/j.mcna.2017.06.006
Vardy, J., Wong, K., Yi, Q.L., Park, A., Maruff, P., Wagner, L., & Tannock, I.F. (2006). Assessing cognitive function in cancer patients. Supportive Care in Cancer, 14, 1111–1118.
Wagner, L.I., Sweet, J.J., Butt, Z., Lai, J.S., & Cella, D. (2009). Measuring patient self-reported cognitive function: Development of the Functional Assessment of Cancer Therapy-Cognitive Function Instrument. Journal of Supportive Oncology, 7(6), W32–W39.
Wefel, J.S., Saleeba, A.K., Buzdar, A.U., & Meyers, C.A. (2010) Acute and late onset cognitive dysfunction associated with chemotherapy in women with breast cancer. Cancer, 116, 3348–3356. https://doi.org/10.1002/cncr.25098
Weintraub, S., Dikmen, S.S., Heaton, R.K., Tulsky, D.S., Zelazo, P.D., Slotkin, J., . . . Gershon, R. (2014). The cognition battery of the NIH toolbox for assessment of neurological and behavioral function: Validation in an adult sample. Journal of the International Neuropsychological Society, 20, 567–578.




