Evaluating the Feasibility of a Nurse-Driven Telephone Triage Intervention for Patients With Cancer in the Ambulatory Setting
Objectives: To explore the feasibility of a nurse-driven telephone triage intervention to improve the symptom experience of patients with cancer receiving treatment in the ambulatory setting.
Sample & Setting: 90 patients in three ambulatory centers (breast, head and neck, and sarcoma) receiving active treatment at a National Cancer Institute–designated comprehensive cancer center.
Methods & Variables: Patients received 4–18 triage calls from a nurse during a period of as many as six months dependent on their diagnosis and treatment. Feasibility was defined as the completion of 70% of triage calls. Symptom experience was measured using the MD Anderson Symptom Inventory.
Results: The overall call completion rate was 78%. Interference (p = 0.002) and severity (p < 0.001) scores were significantly different among patients in the three centers and gradually decreased over time.
Implications for Nursing: Outcomes suggest that a telephone triage intervention is feasible to support patients receiving treatment. Future research can evaluate whether proactive triage affects symptom intensity during the course of the treatment trajectory.
Jump to a section
Effective symptom management is a priority for patients with cancer because it contributes significantly to patients’ overall well-being and can be an indicator of successful patient– or caregiver–provider communication (D’Agostino et al., 2017; Tang et al., 2018). However, studies indicate that patients receive insufficient symptom support (Johnsen et al., 2013) and often feel left alone to manage their symptoms (Spichiger et al., 2012). With more patients being managed in the ambulatory setting, where they are expected to take on greater responsibility for monitoring and managing treatment- and disease-related symptoms, this gap may be further exacerbated. In a qualitative study of 28 patients with cancer, Coolbrandt et al. (2015) identified that the symptom experience in the home setting is very personal, and patients in this study reported that they felt best supported when healthcare providers were perceived to take an active interest in their symptom experience by offering advice and coaching. Identifying opportunities to maximize self-management through proactive symptom support may result in decreased symptom exacerbation and enhanced quality of life for patients, as well as fewer emergency department visits and hospital admissions, which can cause distress for the patient and family, strain hospital resources, and increase healthcare costs (McCorkle et al., 2011). According to the Institute of Medicine (2001), care should be based on continuous healing relationships using in-person and telehealth communication, and care should anticipate, rather than simply react to, patient needs.
Telephone triage interventions have been broadly described as a means for follow-up to monitor the status of patients in surgical, medical, and oncologic settings (Dickinson et al., 2014). Although some triage interventions are proactively used for follow-up, many are available as a way for patients to reach a healthcare provider with questions or when experiencing symptoms. As telehealth continues to evolve, new opportunities exist to proactively use telephone triage to connect with patients in the ambulatory setting, identify symptoms early, and enhance patient interactions with healthcare providers or systems (Anglea et al., 2018).
Symptom management in the outpatient setting is often addressed by responding to telephone triage calls from patients or caregivers (Flannery et al., 2013). In previous studies, one of the most common reasons for patient-initiated calls was to report symptoms, such as fatigue, pain, anorexia, dyspnea, neuropathy, and nausea (Flannery et al., 2013; Lucia et al., 2007). Other reasons included requests for medication refills, appointment clarification, procedural preparation, and self-care information (Basch et al., 2016; Flannery et al., 2013; Lucia et al., 2007). This reactive approach has been used extensively to support the large number of patients who experience side effects from chemotherapy and radiation therapy at home (Anastasia, 2002; Groves, 2005). However, research examining whether a proactive approach initiated by the healthcare team during the first course of chemotherapy could help improve symptom control is limited.
To date, studies have demonstrated inconclusive evidence about the superiority of nursing telephone triage interventions compared to standard of care for symptom assessment and management in patients with cancer (Coolbrandt et al., 2014; Traeger et al., 2015). However, using nurse-driven triage calls, as well as computer-generated calls, to administer valid and reliable symptom assessment instruments may contribute to early identification and management of symptoms in patients with cancer in the home setting (Sikorskii et al., 2007). Such measures encourage patients, informal caregivers, and clinicians to be collaborative partners in symptom management during cancer treatment.
Purpose
At the University of Texas MD Anderson Cancer Center (MDACC) in Houston, 137,000 patients accounted for about 1.5 million ambulatory visits from September 2017 to August 2018. Of these ambulatory visits, the breast center accounted for approximately 50,000 visits, the head and neck center accounted for approximately 30,000 visits, and the sarcoma center accounted for approximately 17,000 visits. Patients in these cancer centers, who represent diverse patient populations undergoing multimodal cancer therapy primarily in the ambulatory setting, are at increased risk for symptom burden, requiring consistent engagement with healthcare providers (Cleeland et al., 2000; Mason et al., 2016). Although each center had an existing triage process, in which patients could reach staff via telephone with treatment-related issues or concerns, an opportunity was identified to enhance this process by providing proactive calls to patients during active treatment.
Based on the lack of literature on proactive telephone triage calls in cancer care in the ambulatory setting, this study was designed to evaluate the feasibility of such calls across diverse patient populations. In addition, the study sought to descriptively explore trends in patients’ symptom experiences across these populations to integrate symptom assessment within nurse-driven proactive telephone triage calls, with the aim of evaluating the efficacy of this modality and its effect on symptom severity in patients with cancer receiving their first course of cancer treatment. Although studies have been conducted to evaluate proactive telephone triage calls, this literature has primarily been in the context of newly discharged or postoperative patients (Dewar et al., 2004; Zhang et al., 2012). This study, however, used proactive telephone triage calls for symptom assessment to help support patients through and mitigate the symptom burden of chemotherapy in the ambulatory setting.
The primary aim of this study was to evaluate the feasibility of a proactive nurse-driven telephone triage intervention for patients receiving first-line chemotherapy in the ambulatory setting. Feasibility was defined as completing 70% of the nurse-driven telephone triage calls. Completion was defined as the patient answering the call and completing the assessment. In addition, secondary aims included exploring the symptom experience, patient satisfaction, and frequency of emergency department visits and hospital admissions for symptom management in the study population.
Methods
Sample and Setting
This study was performed in the ambulatory breast, head and neck, and sarcoma centers at MDACC. These specific cancer centers were selected to reflect diverse patient populations with distinct treatment and symptom profiles. The study was first proposed by nurses in the breast center, and additional centers were recruited to broaden the scope of the study. Ultimately, the sarcoma and head and neck centers were added based on the interest of nurses in those centers. Thirty patients aged 18 years or older undergoing first-line chemotherapy at the study institution were recruited from each center. The total sample consisted of 90 patients. Patients were screened using electronic health records and then assessed for eligibility. Patients from the head and neck center were receiving radiation therapy in addition to first-line chemotherapy. Patients were excluded from the sample if they had previously received chemotherapy, had undergone definitive surgical treatment for their cancer, or were on a research protocol, pregnant, non-English speaking, or unable to communicate verbally. The study was reviewed by the institutional review board at the University of Texas MDACC, and all patients provided consent prior to participation.
Procedures
A quasiexperimental study with a repeated measures design was used to examine the feasibility of a nurse-driven telephone triage intervention. The Roy Adaptation Model (RAM) (Roy, 2009), which underscores the role of nurses in partnering with patients to support their adaptation to a healthy state, provided the theoretical framework for this study. RAM focuses on the concept of an individual’s adaptation to changes in self-concept, physiologic needs, role functions, and relationships during health and illness. According to RAM, the unique goal of nursing is to assist individuals in their adaptation efforts through environmental management, which results in attaining an optimal level of wellness (Andrews & Roy, 1986). Promoting adaptation during health and illness enhances the interaction between the environment and human systems (i.e., a whole with parts that function together as one unit for some purpose) and, ultimately, improves health (Roy & Andrews, 1999; Ursavas et al., 2014).
Eight nurses completed telephone triage calls (four clinical nurses in the breast center, three clinical nurses in the sarcoma center, and one advanced practice nurse in the head and neck center). All volunteers underwent training in accordance with regulations for the protection of human research participants and completed an education session with the researchers to ensure consistency. The education session included an overview of the intervention and a discussion of the study instruments. Education session materials included the study checklist and procedures, study tools (e.g., patient log, call log), telephone call instructions, and documentation on the electronic health record, MD Anderson Symptom Inventory (MDASI), and Research Electronic Data Capture (REDCap).
Measures
The core MDASI was used to measure the symptom experience of patients in the breast and sarcoma cancer centers. The core MDASI consists of 13 symptom items (pain, fatigue, nausea, disturbed sleep, feeling distressed, shortness of breath, problem remembering things, lack of appetite, feeling drowsy, dry mouth, feeling sad, vomiting, and numbness or tingling) and 6 symptom interference items (general activity, mood, work, relationships with others, walking, and enjoyment of life), which are rated based on the level of interference caused by the symptoms (Cleeland et al., 2000, 2004). Symptoms are measured on an 11-point scale ranging from 0 (symptom not present) to 10 (as bad as can be imagined), with scores of 7 or higher considered as severe. The reliability and validity of the MDASI have been well documented in a variety of patient populations (Cleeland et al., 2000, 2004; Mendoza et al., 2013). A high rate of reliability was demonstrated in the original validity study, with a Cronbach alpha of 0.85 and 0.82 for the symptom scale and 0.91 for the interference scale (Cleeland et al., 2000). Patients in the head and neck center completed the MDASI for head and neck cancer (MDASI-HN). The MDASI-HN consists of the core MDASI’s 13 items, with an additional 9 items designed and validated for patients in this population based on the premise that patients with head and neck cancer have additional symptoms that are distinct from those experienced by the general population of patients with cancer and require routine monitoring.
A subset of seven questions from the Press Ganey Outpatient Oncology survey was used with permission to measure patient satisfaction at the midpoint of the intervention and within one week postintervention. Patients were asked seven questions on the nurses’ and healthcare team’s helpfulness, friendliness and courtesy, concern for questions or worries, efforts to include the patient in decision making, information on medications, instructions about follow-up care, and sensitivity to patient needs. This survey was selected because it is the standard tool used to measure patient satisfaction at the study institution.
The number of times patients presented to the emergency department for care and frequency of admissions as an inpatient for symptom support were evaluated descriptively. In addition, patient demographic information and clinical variables, such as age, race, gender, ethnicity, diagnosis, cancer stage, comorbidities, and treatment regimen, were collected and examined descriptively to identify any potential correlation between these characteristics and the patients’ responses to the telephone triage intervention. Symptom data, frequency of emergency department visits, and information on hospital admissions were also collected during the telephone triage intervention and documented electronically via REDCap, a secure, web-based application (Harris et al., 2009). Baseline MDASI data were collected by the researchers prior to the patient starting chemotherapy. In addition, responses to the Press Ganey Outpatient Oncology survey were collected during the patients’ visits to their respective centers at the designated study time points (midpoint and within one week postintervention) or at the closest visit in proximity to these dates.
Intervention
Using a standardized template, a clinical or advanced practice nurse called patients following their first dose of chemotherapy. The frequency of the calls varied based on the disease treatment protocol, ranging from 4 to 18 calls (i.e., patients with breast cancer on four cycles of docetaxel anhydrous and cyclophosphamide received four telephone calls, and patients with sarcoma on a standard chemotherapy care regimen received as many as 18 telephone calls). During the telephone triage calls, patients were asked about their symptoms, and the nurse reviewed and administered the MDASI with the patient. Responses were evaluated during each call with the patient to identify symptom severity. Symptom management was addressed with the patient using a standardized triage algorithm, which was based on the guidelines outlined in Telephone Triage for Oncology Nurses (Hickey & Newton, 2012), and documented in the electronic health record. Patients who did not answer on the first attempt were called as many as three times at each determined frequency based on the patient’s chemotherapy schedule (every three weeks for patients in the breast center; weekly for patients in the head and neck and sarcoma centers). Patients who received a score of 5 or greater on the MDASI (defined as moderate severity) were escalated for symptom management intervention per standard practice at the study institution.
Data Analysis
The primary aim of this study was to evaluate the feasibility of completing nurse-driven telephone triage calls. In this study, completion was defined by the patient answering the telephone call and completing the MDASI and Press Ganey survey. The intervention was considered feasible in each center (breast, head and neck, and sarcoma) if the 90% confidence interval (CI) for the completion rate was above or equal to 70%. Call completion was evaluated separately by center and across all centers.
The secondary aim of this study was to examine the symptom experience of patients receiving a telephone triage intervention using the MDASI. Scores on the MDASI were assessed by center and time point, as well as by time point across all centers. A 90% CI was calculated for MDASI scores over multiple measurements using linear mixed models. Responses on the Press Ganey survey were summarized by time point (midpoint and postintervention) using frequencies and percentages. A McNemar’s test was used to assess whether satisfaction responses differed between the two time points (p < 0.5) based on the responses of very good versus all other responses (poor, fair, and good). All statistical analyses were performed using Stata/MP, version 15.0.
Results
A total of 30 patients were enrolled from each of the three cancer centers (breast, head and neck, and sarcoma). Patient ages ranged from 21 to 78, with a mean age of 52. The majority of patients were Caucasian (n = 68) and identified as Non-Hispanic/Latino (n = 70). At the time of enrollment, 80 patients had localized disease, and 10 patients had metastatic disease. Demographic information is summarized in Table 1 and grouped by center. 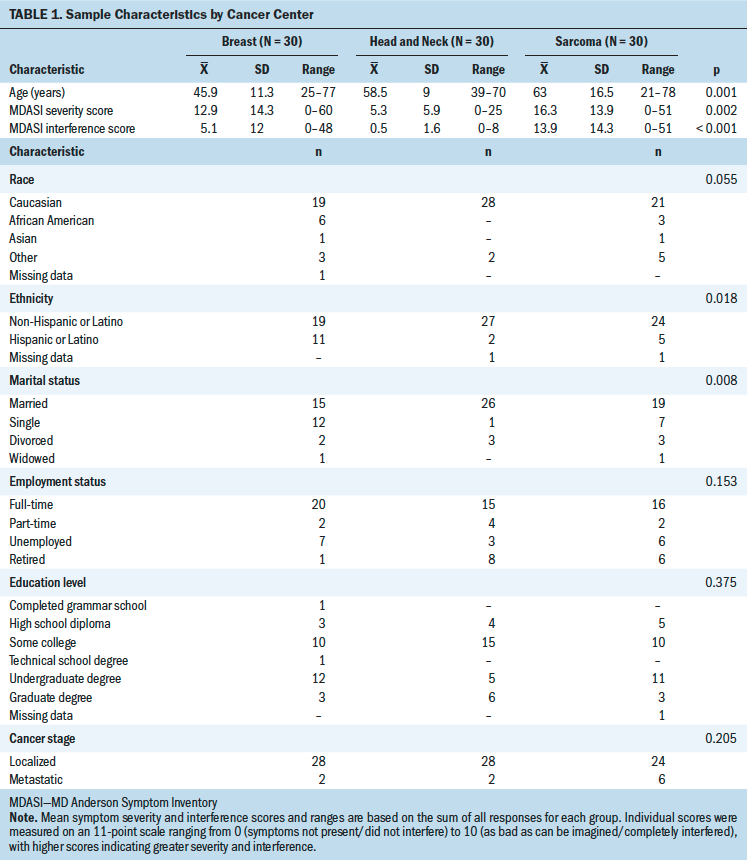
In this study, MDASI interference (p = 0.002) and symptom severity (p < 0.001) scores were significantly different among the three cancer centers. A significant association was also found between cancer center and ethnicity (p = 0.018) and cancer center and marital status (p = 0.008). A summary of the statistics for completed telephone triage calls for each of the centers is presented in Table 2. 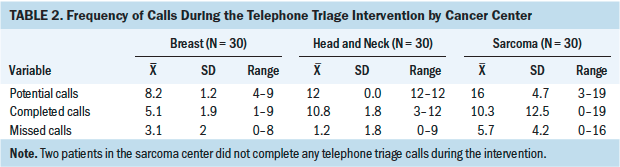
The overall telephone call completion rate was 78% (90% CI [72.8, 83.1]). The completion rate was 64% (90% CI [55.9, 71.3]) for patients in the breast center, 65% (90% CI [53.4, 74.6]) for patients in the sarcoma center, and 94% (90% CI [89.9, 96.8]) for patients in the head and neck center. Therefore, by the definition of feasibility for this study, the completion rate for nurse-driven telephone triage calls was deemed to be feasible across all cancer centers.
Linear mixed models were used to assess scores on the MDASI across multiple calls from the initial triage call assessment. The results suggest that interference and symptom severity scores decreased over time. In addition, symptom severity scores demonstrated a statistically significant change from baseline to the completion of the study for patients overall (p < 0.001), which may have been influenced by a statistically significant decrease in the patient population of the sarcoma center during the same period (p < 0.001). The overall symptom severity score across the three cancer centers was 0.03 points lower on average for each day following the baseline score; therefore, it was expected that the average MDASI score would be 0.42 points lower two weeks into the telephone triage intervention (0.03 multiplied by 14 days). In addition, the researchers tracked the number of emergency department visits and hospital admissions of patients between telephone triage calls to help determine the efficacy of the intervention. Overall, the majority of patients did not visit the emergency department and were not admitted to the hospital following the most recent telephone triage call that they received (see Table 3). According to the responses received on the Press Ganey survey, the majority of patients were satisfied with the care provided by the healthcare team during the intervention. Press Ganey summary statistics are presented in Table 4. 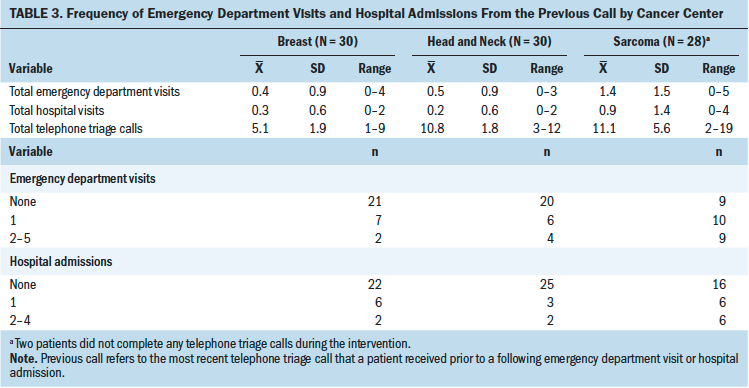
Discussion
The purpose of this study was to determine the feasibility of a nurse-driven telephone triage intervention for symptom assessment and management in the ambulatory setting. Although previous research has examined the use and efficacy of nurse-driven interventions (Cox & Wilson, 2003; De Leeuw & Larsson, 2013), this study aimed to determine whether proactive telephone triage calls to support patients with cancer receiving their first round of chemotherapy would be manageable in a large academic medical center. Although the intervention was found to be feasible overall, the patterns of telephone call completion varied by center. In particular, overall completion rates were significantly higher among patients in the head and neck center (94%) where an advanced practice nurse completed all of the telephone calls. The consistency of having a single nurse complete all calls with a timely response to patient concerns may have contributed to patients feeling more connected to a particular nurse, and, therefore, more likely to respond to and participate in the triage assessments. However, patients in the breast and sarcoma centers, where the completion rates were 64% and 65%, respectively, did not experience the same consistency. Instead, telephone triage calls were made in these centers by a team of trained clinical nurses who, although specifically trained for their role in this study, did so in addition to their regular work assignments. Each clinical nurse was assigned to call a specific group of patients; however, these schedules were subject to change based on staffing variables, and other clinical nurses could be asked to call a patient who was not in their group. Based on workload in the centers, there were also instances where the designated nurse was able to make an initial telephone call to patients but had difficulty completing follow-up calls within the required time frame (one week from each study time point on average). One factor that may have contributed to the differences in completion rates is the possibility that the patients were adapting to the changing demands of their illnesses, had less need for the calls, and, therefore, did not respond as the study progressed (Roy, 2009). In addition to considering time management for nurses who are volunteering to complete telephone calls, determining the appropriate number of triage calls will be essential to future research. [[{"fid":"55051","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
Although much is known about the nature of cancer treatment and the corresponding side effects that patients experience, there is lack of agreement about how to manage care in a way that optimizes patient outcomes, is resource efficient, and ensures patient engagement (De Leeuw & Larsson, 2013). According to the literature, study designs, patient retention, and outcomes of nurse-driven telephone interventions vary, and the differences seen in this study’s sample reflect what has been previously reported in other studies (Cox & Wilson, 2003; Traeger et al., 2015).
In addition, symptom severity and interference scores on the MDASI varied significantly across the three centers, with symptom severity decreasing slowly over time. In a large randomized controlled trial (RCT) comparing a nurse-driven symptom intervention to an automated telephone symptom management intervention that used a voice response version of the MDASI, Sikorsii et al. (2007) found that symptom severity decreased from baseline to the end point of the study. This may suggest that a patient’s need for support, and the concurrent use of nursing resources, could diminish as treatment progresses when either the symptoms abate or the patient’s ability to adapt improves.
Patient satisfaction, which was measured using an abbreviated version of the Press Ganey Outpatient Oncology survey, improved from the study’s midpoint to postintervention for the patient populations of the three centers as a whole. Similar to the reports of other nurse-driven interventions (Lewis et al., 2009; Malmström et al., 2015; Traeger et al., 2015), patients in this study reported overall satisfaction with the telephone triage intervention. This instrument was chosen because it is used to assess patient satisfaction for all ambulatory patient populations at this institution; however, selecting only specific items on the survey may have compromised validity. In future studies, researchers must consider using a validated instrument to determine whether enhanced patient satisfaction has an impact on patients’ resilience and quality of life (Malmström et al., 2015).
Despite the proactive telephone triage calls, patients in all three centers visited the emergency department and were admitted to the hospital during the study period. However, patients in the sarcoma center, who were called an average of 11 times during the treatment period, experienced a greater need for acute care support than patients who were called 5 (breast center) or 10 (head and neck center) times on average. The effectiveness of nurse-driven interventions in reducing the need for acute care services is not conclusively supported in the literature. In a small quality improvement project on assisting adults aged 65 years or older to manage the complications of chemotherapy, Lynch et al. (2010) suggested that routine telephone assessment may prevent emergency department visits, decrease hospital admissions, and minimize treatment delays by offering earlier interventions and preventive strategies. The study by Lynch et al. (2010) and other studies suggest that nurses play an essential role in supporting the needs of patients with cancer, managing disease-related complications, and coordinating care (Coolbrant et al., 2015; De Leeuw & Larsson, 2013). Evaluating these outcomes in the context of an RCT can better inform whether proactive telephone triage calls reduce emergency department visits and hospitalizations during active treatment with chemotherapy.
According to Roy (2009), the purpose of nursing is to ensure adaptation. Promoting adaptation during health and illness enhances the interaction between the environment and human systems to improve overall health (Ursavas et al., 2014). The role of nurses includes manipulating stimuli from the environment to enable patients to experience positive coping with their cancer diagnosis and its symptoms, which eventually can lead to adaptation. Consistent with RAM (Roy, 2009), this study implemented proactive telephone triage calls to monitor and support patients with managing the symptoms associated with cancer and its treatment. Although the results of this study suggest feasibility, a larger RCT is needed to assess whether proactive telephone triage calls improve patient outcomes by supporting adaptation to a cancer diagnosis and its treatment, as well as enhancing symptom management.
Limitations
The current study was limited in size and scope. Because only feasibility was tested, an understanding of how proactive telephone triage affects symptom burden and other treatment-related outcomes cannot be determined from the study findings. From the perspective of generalizability, only patients with solid tumors were included in this study, and, therefore, feasibility for patients with hematologic malignancies is not reflected. Using select items from the Press Ganey survey also limits reliability and the ability to measure patient satisfaction, which is further limited by being unable to discern whether participant responses were reflective of their experience with the telephone triage intervention or with the entire healthcare system. The variability in completion rates between the advanced practice nurse and trained clinical nurses suggests the need to further explore how to best manage the nurse-related factors, such as time, availability, and frequency of calls, to promote optimal efficiency and sustainability.
Implications for Nursing
The findings of this study support engaging nurses in the ambulatory setting to thoroughly assess and provide ample care to patients who are navigating their first course of chemotherapy. Being aware of the potential for symptom burden and effectively managing physical and psychological symptoms has the potential to reduce the need for additional patient resources, which can reduce costs, improve the ability of patients to manage their experience, and enhance quality-of-life outcomes. The goal of a larger RCT would be to evaluate the effect of a nurse-driven telephone triage intervention on symptom burden and other patient-reported and clinical outcomes, as well as to evaluate varying feasibility data based on current staffing and practice patterns at the study institution. One strategy to improve feasibility could include the implementation of a full-time triage nurse, which would ensure that ample time is provided to conduct telephone triage calls with patients consistently. In addition, a combination approach using technology and nurse-driven interventions may have practical implications for managing larger patient populations where the ability to replicate individual proactive telephone calls at the frequency defined in this study in everyday clinical care is limited. Additional discussions are needed on how to most effectively leverage these variables and shape the course of cancer care moving forward. 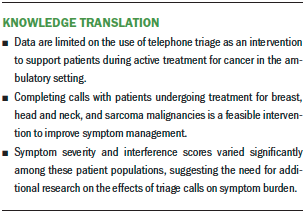
Conclusion
Implementing a proactive nurse-driven telephone triage intervention can potentially transform cancer care and patient outcomes during active treatment in the ambulatory setting, similar to how it has improved the management of postoperative patients with varying diagnoses and disease stages. From an operational perspective, additional research is needed on how to optimize the timing of telephone calls based on cancer type and individual patient characteristics to ensure that the calls are effective for patients and that resources are being used by nurses and other healthcare providers. Developing an algorithm to determine call schedules can also help to personalize patient support for symptom management. Proactive triage is a promising area for practicing nurses to help patients with cancer adapt to active treatment and its potential outcomes in the ambulatory setting.
About the Author(s)
Colleen Jernigan, PhD, RN, AOCN®, NEA-BC, is the director of ambulatory nursing, Theresa Johnson, MSN, RN, is the clinical administrative director of the sarcoma center, Susan Varghese, PhD, RN, ANP-BC, is an advanced practice provider in thoracic-head and neck medical oncology, and Bryan Fellman, MS, is a senior statistical analyst, all at the University of Texas MD Anderson Cancer Center in Houston. This research was supported by a grant (#P30CA016672) from the National Institutes of Health National Cancer Center through the use of the biostatistics resource group. Jernigan, Johnson, and Varghese completed the data collection. Varghese and Fellman provided statistical support. All authors contributed to the conceptualization and design, provided the analysis, and contributed to the manuscript preparation. Jernigan can be reached at cjerniga@mdanderson.org, with copy to ONFEditor@ons.org. (Submitted April 2019. Accepted October 3, 2019.)
References
Anastasia, P.J. (2002). Telephone triage and chemotherapy symptom management in the ambulatory care setting. Oncology Supportive Care Quarterly, 1, 40–55.
Andrews, H.A., & Roy, C. (1986). Essentials of Roy Adaptation Model. Appleton-Century-Crofts.
Anglea, T., Murray, C., Mastal, M., & Clelland, S. (Eds.). (2018). Scope and standards of practice for professional telehealth nursing (6th ed.). American Academy of Ambulatory Care Nursing.
Basch, E., Deal, A.M., Kris, M.G., Scher, H.I., Hudis, C.A., Sabbatini, P., . . . Schrag, D. (2016). Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. Journal of Clinical Oncology, 34(6), 557–565. https://doi.org/10.1200/jco.2015.63.0830
Cleeland, C., Crawford, J., Lubeck, D., & Tomita, D. (2004). Using the MD Anderson Symptom Inventory (MDASI) to assess symptom burden and interference: Interim results of an open-label study of darbepoetin Alfa 200 mcg every 2 weeks (Q2W) for the treatment of chemotherapy induced anemia (CIA). Journal of Clinical Oncology, 22(14S), 8065. https://doi.org/10.1200/jco.2004.22.90140.8065
Cleeland, C.S., Mendoza, T.R., Wang, X.S., Chou, C., Harle, M.T., Morrissey, M., & Engstrom, M.C. (2000). Assessing symptom distress in cancer patients: The MD Anderson Symptom Inventory. Cancer, 89(7), 1634–1646. https://doi.org/10.1002/1097-0142(20001001)89:7%3C1634::AID-C-CR29%3E3…
Coolbrandt, A., Dierckx de Casterlé, B., Wildiers, H., Aertgeerts, B., Van der Elst, E., van Achterberg, T., & Milisen, K. (2015). Dealing with chemotherapy-related symptoms at home: A qualitative study in adult patients with cancer. European Journal of Cancer Care, 25(1), 79–92. https://doi.org/10.1111/ecc.12303
Coolbrandt, A., Wildiers, H., Aertgeerts, B., Van der Elst, E., Laenen, A., Dierckx de Casterlé, B., . . . Milisen, K. (2014). Characteristics and effectiveness of complex nursing interventions aimed at reducing symptom burden in adult patients treated with chemotherapy: A systematic review of randomized controlled trials. International Journal of Nursing Studies, 51(3), 495–510. https://doi.org/10.1016/j.ijnurstu.2013.08.008
Cox, K., & Wilson, E. (2003). Follow-up for people with cancer: Nurse-led services and telephone interventions. Journal of Advanced Nursing, 43(1), 51–61. https://doi.org/10.1046/j.1365-2648.2003.02672.x
D’Agostino, T.A., Atkinson, T.M., Latella, L.E., Rogers, M., Morrissey, D., DeRosa, A.P., & Parker, P.A. (2017). Promoting patient participation in healthcare interactions through communication skills training: A systematic review. Patient Education and Counseling, 100(7), 1247–1257. https://doi.org/10.1016/j.pec.2017.02.016
De Leeuw, J., & Larsson, M. (2013). Nurse-led follow-up care for cancer patients: What is known and what is needed. Supportive Care in Cancer, 21(9), 2643–2649. https://doi.org/10.1007/s00520-013-1892-6
Dewar, A., Scott, J., & Muir, J. (2004). Telephone follow-up for day surgery patients: Patient perceptions and nurses’ experience. Journal of PeriAnesthesia Nursing, 19(4), 234–241. https://doi.org/10.1016/j.jopan.2004.04.004
Dickinson, R., Hall, S., Sinclair, J.E., Bond, C., & Murchie, P. (2014). Using technology to deliver cancer follow-up: A systematic review. Biomed Central Cancer, 14(1), 311. https://doi.org/10.1186/1471-2407-14-311
Flannery, M., McAndrews, L., & Stein, K.F. (2013). Telephone calls by individuals with cancer. Oncology Nursing Forum, 40(5), 464–471. https://doi.org/10.1188/13.ONF.464-471
Groves, E.L. (2005). Auditing a chemotherapy triage telephone service. Cancer Nursing Practice, 4(6), 25–29. https://doi.org/10.7748/cnp2005.07.4.6.25.c169
Harris, P.A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J.G. (2009). Research Electronic Data Capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Hickey, M., & Newton, S. (Eds.). (2012). Telephone triage for oncology nurses (2nd ed.). Oncology Nursing Society.
Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press.
Johnsen, A.T., Petersen, M.A., Pedersen, L., Houmann, L.J., & Groenvold, M. (2013). Do advanced cancer patients in Denmark receive the help they need? A nationally representative survey of the need related to 12 frequent symptoms/problems. Psycho-Oncology, 22(8), 1724–1730. https://doi.org/10.1002/pon.3204
Lewis, R., Neal, R.D., Williams, N.H., France, B., Wilkinson, C., Hendry, M., . . . Weller, D. (2009). Nurse-led vs. conventional physician-led follow-up for patients with cancer: Systematic review. Journal of Advanced Nursing, 65(4), 706–723. https://doi.org/10.1111/j.1365-2648.2008.04927.x
Lucia, V.C., Decker, V.B., Israel, C.E., & Decker, D.A. (2007). Telephone contacts between triage nurses and cancer patients: An integral part of a community oncology practice. Community Oncology, 4(5), 350–354. https://doi.org/10.1016/s1548-5315(11)70130-9
Lynch, M.P., Marcone, D., & King, J. (2010). Chemotherapy follow-up in older adults: Results of a quality-improvement project. Clinical Journal of Oncology Nursing, 14(5), 619–625. https://doi.org/10.1188/10.CJON.619-625
Malmström, M., Klefsgard, R., Ivarsson, B., Roman, M., & Johansson, J. (2015). Quality of life measurements as an indicator for timing of support after esophagectomy for cancer: a prospective study. BMS Health Services Research, 15(1), 96. https://doi.org/10.1186/s12913-015-0747-x
Mason, H., De Rubeis, M.B., Burke, N., Shannon, M., Karseis, D., Wolf, G., . . . Worden, F. (2016). Symptom management during and after treatment with concurrent chemoradiotherapy for oropharyngeal cancer: A review of literature and areas for future research. World Journal of Clinical Oncology, 7(2), 220–226. https://doi.org/10.5306/wjco.v7.i2.220
McCorkle, R., Ercolano, E., Lazenby, M., Schulman-Green, D., Schilling, L.S., Lorig, K., & Wagner, E.H. (2011). Self-management: Enabling and empowering patients living with cancer as a chronic illness. A Cancer Journal for Clinicians, 61(1), 50–62. https://doi.org/10.3322/caac.20093
Mendoza, T.R., Zhao, F., Cleeland, C.S., Wagner, L.I., Patrick-Miller, L.J., & Fisch, M.J. (2013). The validity and utility of the MD Anderson Symptom Inventory in patients with breast cancer: Evidence from the symptom outcomes and practice patterns data from the Eastern Cooperative Oncology Group. Clinical Breast Cancer, 13(5), 325–334. https://doi.org/10.1016/j.clbc.2013.02.014
Roy, C. (2009). The Roy Adaptation Model (3rd ed.). Pearson Education.
Roy, C., & Andrews, H.A. (1999). The Roy Adaption Model (2nd ed.). Appleton and Lange.
Sikorskii, A., Given, C.W., Given, B., Joen, S., Decker, V., Decker, D., . . . McCorkle, R. (2007). Symptom management for cancer patients: A trial comparing two multimodal interventions. Journal of Pain and Symptom Management, 34(3), 253–264. https://doi.org/10.1016/j.jpainsymman.2006.11.018
Spichiger, E., Müller-Fröhlich, C., Denhaerynck, K., Stoll, H., Hantikainen, V., & Dodd, M. (2012). Prevalence and contributors to fatigue in individuals hospitalized with advanced cancer: A prospective, observational study. International Journal of Nursing Studies, 49(9), 1146–1154. https://doi.org/10.1016/j.ijnurstu.2012.03.003
Tang, C.C., Draucker, C., Tejani, M.A., & Von Ah, D. (2018). Patterns of interactions among patients with advanced pancreatic cancer, their caregivers, and healthcare providers during symptom discussions. Supportive Care in Cancer, 26(10), 3497–3506. https://doi.org/10.1007/s00520-018-4202-5
Traeger, L., McDonnell, T.M., McCarty, C.E., Greer, J.A., El-Jawahri, A., & Temel, J.S. (2015). Nursing intervention to enhance outpatient chemotherapy symptom management: Patient-reported outcomes of a randomized controlled trial. Cancer, 121(21), 3905–3913. https://doi.org/10.1002/cncr.29585
Ursavas, F.E., Karayurt, Ö., & Iseri, Ö. (2014). Nursing approach based on Roy adaptation model in a patient undergoing breast conserving surgery for breast cancer. Journal of Breast Health, 10(3), 134–140. https://doi.org/10.5152/tjbh.2014.1910
Zhang, J.E., Wong, F.K.Y., You, L.M., & Zheng, M.C. (2012). A qualitative study exploring the nurse telephone follow-up of patients returning home with a colostomy. Journal of Clinical Nursing, 21(9–10), 1407–1415. https://doi.org/10.1111/j.1365-2702.2011.03824.x




