Assessment of a Structured Self-Management Support Intervention by Nurses for Patients With Incurable Cancer
Objectives: To gain an understanding of the perceptions of patients with incurable cancer regarding a new nurse-led self-management support intervention with an integrated eHealth application (Oncokompas) and its potential effectiveness.
Sample & Setting: 36 patients receiving support in the home setting.
Methods & Variables: A pre- and post-test mixed-methods design was used with a period of 12 weeks between the tests and qualitative interviews. Outcome measures were the perceived application of the intervention, patient satisfaction, patient activation, and quality of life.
Results: 85% of patients were satisfied with the assessment of their needs and the advice received. They valued nurses’ expertise and the assistance provided in their homes. Twenty-five percent of the patients used Oncokompas. However, no statistically significant changes in patient activation and quality of life were found.
Implications for Nursing: This intervention can be used for encouraging self-management by patients with incurable cancer. Additional refinement and tailoring is desirable. Offering the intervention as early in the palliative phase as possible is recommended.
Jump to a section
Medical advances are allowing patients with incurable cancer to live independently for a longer period of time. Living with the knowledge of a limited life expectancy, the uncertainty that comes with that knowledge, and the deterioration of health may negatively affect daily living and may result in a loss of self-management capacities (Bailey et al., 2011; Moens et al., 2014). In this regard, self-management support can be helpful. The aim of this study is to gain an understanding of how patients with incurable cancer perceive a nurse-led self-management support intervention with an optional integrated eHealth application and its potential efficacy for enhancing patient activation and quality of life (QOL).
Self-management is a dynamic, interactive daily process that individuals use for managing their illness (Lorig & Holman, 2003). Self-management refers to a person’s ability to manage physical and psychosocial symptoms and to make decisions concerning treatment and/or care to best integrate the disease into daily life and to maintain satisfactory QOL despite the disease (Barlow et al., 2002; Bodenheimer et al., 2002). Prerequisites for self-management include knowledge about the disease and being able to acquire, select, and use appropriate information and help, both professional and other types (Barlow et al., 2002; Bodenheimer et al., 2002; Schulman-Green et al., 2012).
Self-management, however, is not easy for everyone, and some people need help managing the effect of their disease on daily life. Self-management is challenging for patients with incurable cancer who have to deal with physical deterioration and a limited life expectancy (Bailey et al., 2011; Moens et al., 2014). These patients may need self-management support. Self-management support is a collaborative approach in which providers and patients work together to define problems, set priorities, establish goals, create treatment plans, and solve problems along the way (Group Health Research Institute, n.d.; Von Korff et al., 1997). In the Netherlands, assisting patient self-management is part of the scope of nursing practice (Committee on Nursing Roles, 2015). Nurses may, therefore, be the appropriate professionals to provide that self-management support.
Existing self-management interventions mainly focus on patients with chronic diseases, such as diabetes, chronic obstructive pulmonary disease, and rheumatoid arthritis, whereas patients with cancer, and particularly incurable cancer, have received less attention (Budhwani et al., 2019; Charalambous et al., 2018; Schulman-Green et al., 2018; Zuidema et al., 2019). In addition, most of the interventions are not aimed at nurses to provide self-management support.
A structured nurse-led self-management support intervention for patients with incurable cancer was developed by Slev et al. (2016) and involves face-to-face contact with a nurse and an optional eHealth component. eHealth is the provision of information about illness or health care and/or support for patients and/or informal caregivers using computers or related technologies (Eysenbach, 2001). The face-to-face contacts were integrated into continuity home visits by a specialist oncology and/or palliative care nurse for patients who were not yet receiving regular home care (Docter et al., 2010; van Harteveld et al., 1997). The nurse’s self-management support during the visits was structured according to the steps of the 5 A’s model (Dutch Institute for Healthcare Improvement, 2014; Glasgow et al., 2003). In the Netherlands, the 5 A’s model is increasingly being adopted and integrated into care standards, nursing education, and interventions in self-management support (Beck et al., 2019; Huis In Het Veld et al., 2017). The feasibility among nurses, described in Slev et al. (2020), showed a high adoption rate (intention to use) of 81%. Nurses’ subjective evaluation of the intervention was positive (general satisfaction score = 7.57 out of 10). The usage rate (actual usage) was, however, lower than expected (56%), which suggests that the intervention did not fit nurses’ self-management support practice sufficiently well.
In the current study, the authors tested the feasibility of the self-management intervention from the patient perspective. The central aim of the current study was to gain an understanding of how people with incurable cancer evaluate the self-management support intervention. A secondary aim was to examine the possible effects of the intervention on patient activation and QOL. Patient activation can be described as the individual’s knowledge, skills, and confidence for managing their health and health care (Hibbard et al., 2005). Activated patients are patients who believe they have important roles to play in self-managing their care, collaborating with providers, and maintaining their health. Studies have demonstrated that patient activation positively affects various health-related self-management behaviors and is associated with improved health outcomes (Greene et al., 2015; Greene & Hibbard, 2012; Hibbard et al., 2007; Hibbard & Mahoney, 2010; Rask et al., 2009; Salgado et al., 2017). The optional eHealth component was Oncokompas, a web-based self-management instrument for monitoring various QOL aspects by means of Patient-Reported Outcome Measures (PROMs), followed by automatically generated tailored feedback and personalized advice about supportive care services (Duman-Lubberding et al., 2015, 2016; van der Hout et al., 2017).
The following research questions are addressed in this article:
• Do patients recognize that the nurses applied elements of the 5 A’s model (i.e., assessed their knowledge, beliefs, and behaviors related to their health; gave advice; agreed on goals; helped achieve these goals; and arranged a care plan and follow-up)?
• Are patients satisfied with how the nurse applied elements of the 5 A’s model, and how do patients generally evaluate the self-management support intervention?
• How is Oncokompas used and evaluated by patients?
• Are there indications that the self-management support intervention positively influences patient activation and the QOL of patients with incurable cancer?
Methods
Sample and Procedures
The sample size is calculated based on an expected Cohen’s d effect size of 0.4 for patients, an alpha of 0.05, a power of 0.8, and a two-tailed t test. The power analysis, based on the short version of the Patient Activation Measure (PAM), resulted in a sample of 52 patients. Taking into account a nonparticipant rate of 30% (Hui et al., 2013), 68 patients were required.
A convenience sample was used. From November 2016 to May 2018, eligible patients were invited to participate in this study by nurses from four homecare organizations in the Netherlands. Patients were eligible for study participation if they met the following inclusion criteria: (a) were aged 18 years or older, (b) had an incurable form of cancer, (c) were mentally and physically able to fill out a questionnaire at the time of recruitment, (d) had sufficient verbal and written mastery of Dutch, and (e) were a new referral for a continuity home visit.
A pre- and post-test design was used with a questionnaire at baseline (T0) and 12 weeks (T1). Eligible patients were asked by their nurses to participate in the study during the first continuity home visit and received an informed consent form and the baseline questionnaire. Patient participation was confirmed as soon as the signed informed consent form and the baseline questionnaire were received. Subsequently, a registration hyperlink for Oncokompas was sent by email to patients who provided an email address. Prior to the second continuity home visit, these patients were asked to complete Oncokompas.
Under Dutch legislation, the study did not need review by a medical ethical committee because the participants were not subject to procedures or required to follow rules of behavior (Central Committee on Research Involving Human Subjects, n.d.). All patients gave written informed consent to participate.
Measures
A study-specific questionnaire of sociodemographic and clinical factors (T0), items about the application of the self-management support intervention in general and satisfaction with it, and about Oncokompas specifically (follow-up [T1]), and scales for the patient’s activation and QOL (T0 and T1) were developed. Recognition of the 5 A’s model being applied by the nurse was measured at T1 with statements about the 5 A’s. Each A of the model was operationalized into a single behavior. Patients were asked to indicate whether they were satisfied with the extent to which the nurse applied the following behaviors:
• “I am satisfied with the extent to which the nurse spoke to me about my experiences (problems, wishes, and needs)” (Assess).
• “I am satisfied with the extent to which the nurse provided information (information, advice, and tips)” (Advice).
• “I am satisfied with the extent to which the nurse set goals together with me for handling my problems or being able to cope with them better” (Agree).
• “I am satisfied with the extent to which the nurse offered assistance solving the daily problems due to my illness” (Assist).
• “I am satisfied with the extent to which the nurse made an individual care plan with me containing agreements for the continuation of care” (Arrange).
The response options ranged from strongly disagree to strongly agree, with a “not applied” category also available. Perceived application of the 5 A’s was operationalized as the percentage of patients indicating that every A of the 5 A’s model was applied by the nurse.
Satisfaction with the 5 A’s was assessed using the scale mentioned previously. In addition, patients rated their satisfaction with the overall intervention and the nurse’s support on an 11-point Likert-type scale ranging from 0 (very poor) to 10 (very good).
Use of Oncokompas was defined as the percentage of patients who actually used Oncokompas as intended, based on logging data from the application. In the patient questionnaire, users of Oncokompas rated their satisfaction on an 11-point Likert-type scale from 0 (very poor) to 10 (very good). Non-users were asked why they had not used Oncokompas (open question).
Patient activation was measured with PAM as a 13-item PROM on knowledge, skills, and confidence about self-management of the patient’s own health or chronic condition. Patients were asked to say how much they agreed with various statements on a scale ranging from strongly disagree to strongly agree, with an additional option to indicate that the item was not applicable. The total score was transformed to a standardized activation score ranging from 0 to 100, with higher scores indicating higher patient activation (Hibbard et al., 2004). The Dutch translation of the PAM has good internal consistency (Cronbach alpha = 0.88) and a moderate test-retest reliability (r = 0.47) (Rademakers et al., 2012).
QOL was measured using the 15-item European Organisation for the Research and Treatment of Cancer Quality-of-Life Questionnaire–Core 15–Palliative (EORTC QLQ-C15-PAL) (Groenvold et al., 2006). It was developed as an abbreviated tool for assessing QOL in patients receiving palliative care (Fayers & Bottomley, 2002). The EORTC QLQ-C15-PAL includes two functional scales (physical and emotional), two symptom scales (pain and fatigue), five single items (dyspnea, insomnia, loss of appetite, nausea/vomiting, and constipation), and an overall QOL item. Symptoms and functioning are assessed using 14 items (Q1–Q14) on a four-point Likert-type scale ranging from 1 (not at all) to 4 (very much). Overall QOL is rated from 1 (very poor) to 7 (excellent). Each scale/item is converted to a score ranging from 0 to 100, with higher scores indicating higher QOL. Although the EORTC QLQ-C15-PAL has been developed partly with Dutch patients and professionals, information about the psychometric properties of the Dutch translation has not been published. In several other countries, the EORTC QLQ-C15-PAL proved to be reliable and valid (Alawneh et al., 2016; Bjorner et al., 2004; GolČiĆ et al., 2018; Suárez-del-Real et al., 2011; Zhang et al., 2016).
To describe experiences with the self-management support intervention, semistructured interviews were held among a subsample of patients (n = 11). Patients who had completed the T1 questionnaire were contacted and asked to participate. An interview guide was used to structure the interviews (see Figure 1). The interviews were conducted by telephone, took about 45 minutes, were audio-recorded with the interviewee’s permission, and were transcribed verbatim.

Data Analysis
Analyses were performed using IBM SPSS Statistics, version 23.0. The authors used descriptive statistics for reporting on perceived application of the 5 A’s model, Oncokompas usage rate, and general satisfaction. To assess the effects of the self-management support intervention on patient activation and QOL, paired t tests were conducted. Statistical significance was assumed when p < 0.05 (two-tailed). All interview transcripts were read and re-read for familiarization with the data. Information about the self-management support intervention in general and Oncokompas specifically was selected and summarized in a list of main themes by two authors (A.dV. and V.N.S.). All text fragments were arranged by theme and placed in Microsoft® Excel, after which A.dV. and V.N.S. discussed the conclusions for each theme. Disagreements in coding and conclusions were solved through consensus.
Results
Sample Characteristics
Of 131 patients who showed interest in participating in the study, 69 (53%) were included after providing informed consent and returning the T0 questionnaire (see Figure 2). Reasons for not participating included that the authors lost contact with the patient after several reminders (n = 13), that patients found themselves (physically and/or mentally) incapable of participating (n = 9), and that patients were too late returning the T0 questionnaire and informed consent, namely prior to the second continuity home visit (n = 7). In total, 33 of 69 patients (48%) dropped out during the study, leaving a study cohort of 36 patients. The main reason for dropping out was the death of the patient (n = 23).

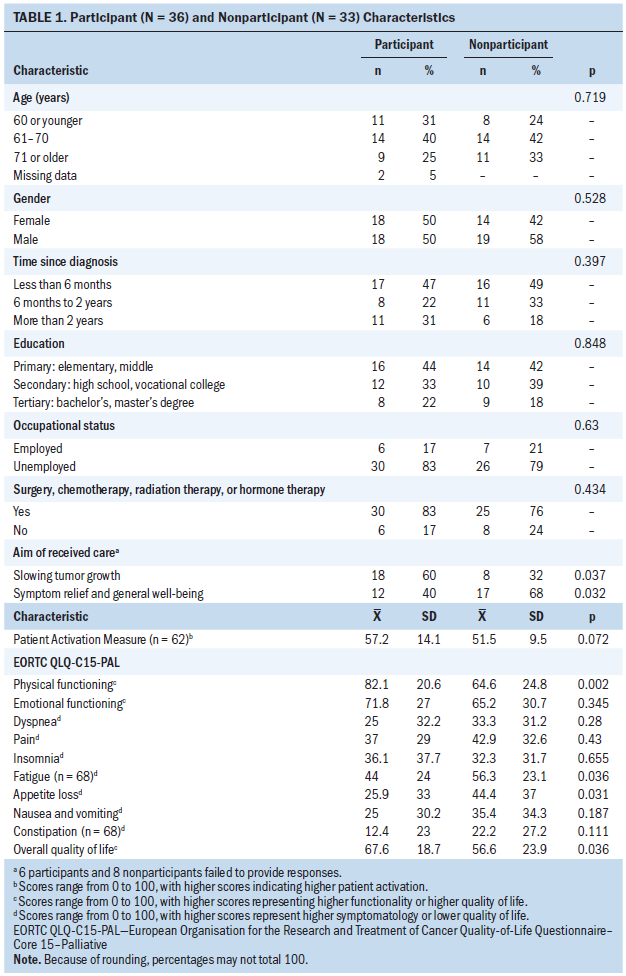
No significant differences were found between the participants and those who dropped out in terms of age, sex, marital status, education, occupational status, time since diagnosis, treatment modality, or PAM score (see Table 1). Significant differences were found for the aim of the received care as perceived by the patients. Participants more often indicated that slowing down tumor growth was the aim, whereas symptom relief and well-being were more common among those who dropped out. Significant differences were also found for physical functioning, fatigue, appetite loss, and overall QOL (better among participants). This reflects a poorer state of health among those who dropped out of the group and is in line with the large number of deaths in the nonparticipant group.
Application of the Intervention
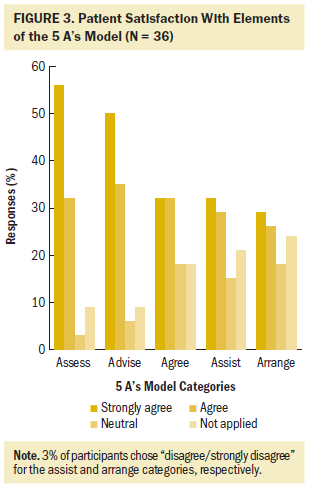
The following results are for the 36 patients who participated at T1. According to 74% of the patients (n = 25 of 34, 2 missing), the nurse applied the intervention in full, meaning that every A of the 5 A’s model was applied. Three patients (9%) indicated that none of the A’s were applied during the continuity home visits. Figure 3 shows that agree, assist, and arrange were the A’s that were least recognized.
 0
0
Satisfaction With the Intervention
Some of the most appreciated aspects were the nurse’s assessment of a broad range of actual and potential problems of the patient as well as their family members and the recommendations of the nurse.
. . . Someone who comes around to your home and takes a good look at your issues, so that you can have a right good talk about them. That’s valuable to me. (respondent 31)
You’re not only ill, as my oncologist said to me, but you’ve both got to cope with the disease, because it has a big impact. (respondent 79)
Some patients did not appreciate all the topics the nurse put forward; those concerning the terminal phase, in particular, were confrontational.
The facts are always being driven home . . . that small glimmer of hope that you’ve still got, the one thing you’re clinging onto in life . . . the hard truth is rammed home and that can be pretty tricky to cope with. . . . I think that people do benefit from not having whatever hope is left taken away from them. (respondent 11)
Patients mentioned many subjects that the nurse gave advice about, such as practical advice on how to arrange for a taxi, medical and other aids, or domestic help, information about possible places for dying or how to deal with symptoms, and advice on how to involve family and friends in the care.
It’s nice that you don’t have to search the whole Internet to find exactly where you need to be at; she knows the answers and will show you the way. Some people simply feel too ill to go Googling. (respondent 11)
Patients were generally also satisfied with the other A’s of the intervention, if applied (agree, assist, and arrange). In the interviews, patients stated that they perceived these A’s as less necessary. When asked if goals had been set, one patient (respondent 11) answered that there were no goals and “I don’t know what the future will bring.” Arrangements consisted mostly of appointments for further contact or that the patient agreed to contact the nurse when their state of health worsened. As one respondent (respondent 70) remarked, “When it gets that far . . . that you’ll have a fixed contact then, someone you’ve gotten to know.”
Patients gave the structured nurse-led self-management support intervention an average general satisfaction score of 7.2 on a scale from 0 (very bad) to 10 (very good) (range = 0–10, SD = 2). The average score for support by the nurse was 7.9 (range = 1–10, SD = 1.7) These broad ranges indicate large differences in how much the intervention was appreciated.
Patients greatly appreciated specialist oncology and/or palliative care nurses visiting them. The patients interviewed generally perceived this as pleasant because of the nurses’ expertise, empathy, and time for the patient. They also valued the fact that the visits were at the patient’s home, as this led to a more relaxed and open conversation.
At the hospital, you’re immediately just another patient. And the smell, and all the sick people you see around you—that always makes me so sad. (respondent 31)
At home, well, it’s cozier, more homey, more relaxing. Maybe the relaxing part comes first. You make a coffee or a tea and then we can have a cozy chat about it. (respondent 126)
Use and Evaluation of Oncokompas
In total, 59 of 69 patients (86%) provided an email address and were sent a registration link for Oncokompas. According to logging data, 35 patients registered, and 17 patients used Oncokompas. Whereas patients in the nonparticipant group and patients in the study cohort provided an email address equally often, fewer nonparticipant patients registered (n = 12, 36%) than patients in the study cohort (n = 23, 64%). Twelve percent of the patients in the nonparticipant group (4 of 33) used Oncokompas, compared to 36% of the patients in the study cohort (13 of 36). Six patients stated at T1 that they had discussed their scores with the nurse. At T1, 18 patients from the study cohort gave reasons for not using Oncokompas; these were that their physical condition was too poor or they were too tired (n = 4), had no interest in using Oncokompas (n = 4), had recurrent hospital admissions or visits (n = 2), experienced technical problems (n = 2), had not received access to Oncokompas (n = 2), did not remember that Oncokompas was available (n = 1), did not have Internet access (n = 1), did not understand Oncokompas (n = 1), or did not know Oncokompas (n = 1).
The average score for Oncokompas was 6.5, with large differences in scores noted (range = 1–9, SD = 1.9). In the interviews, patients noted that the value of Oncokompas is related to personal preferences (e.g., patients remarked that the topics in Oncokompas did not really fit their situation) and to the disease burden.
So, you’ve got to be up to it, be in good enough shape physically and mentally just to sit there with your PC or tablet and look everything up. (respondent 72)
Generally, they preferred a nurse and believed Oncokompas could sometimes have an added value.
For me, personal contact is what matters, and Oncokompas can then be a nice extra on top of that. (respondent 26)
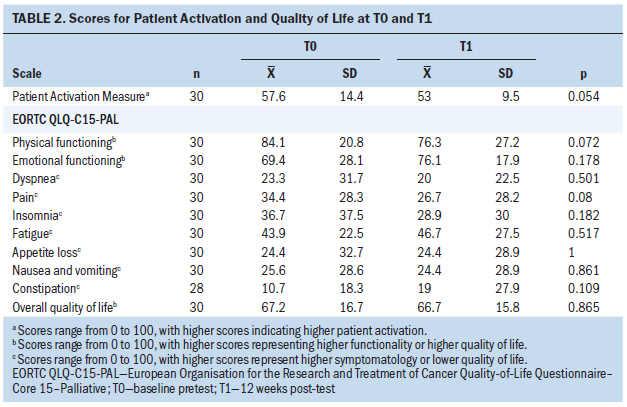
There was no statistically significant change in patient activation or QOL after the intervention (see Table 2).
Discussion
The current study provides an understanding of patients’ evaluation of a structured nurse-led self-management support intervention with optional use of Oncokompas and the preliminary effects on patient activation and QOL. The results showed a mean satisfaction score of 7.2 for the intervention as a whole, with patients being particularly satisfied with the assistance from the nurse (7.9). Patients greatly valued the expertise and attitude of the nurse, the time available for a quiet conversation, and the visits in their own home. This is in line with previous studies on specialist home palliative and cancer care professionals (Coolbrandt et al., 2018; Sarmento et al., 2017) reporting that competent specialist care was perceived as reassuring by patients and increased the self-perceived ability to deal with symptoms (Coolbrandt et al., 2018). In addition, earlier research revealed that visits by healthcare professionals to the patients’ own homes were often greatly appreciated by people facing a life-limiting disease because such visits provide a sense of security (Kleijn et al., 2019; Sarmento et al., 2017).
Oncokompas was less highly valued (mean score = 6.5). Other studies of Oncokompas showed mean scores of 6.9 and 7.3 from breast cancer survivors (Melissant et al., 2018) and head and neck cancer survivors (Duman-Lubberding et al., 2016), respectively. Some patients interviewed in the current study considered Oncokompas to add little value because the topics discussed did not really fit their situations, whereas others appreciated Oncokompas greatly. In addition, other studies found differences between people in the use and intended use of eHealth. People with lower education levels and with complex, unstable health conditions were found to be less open to eHealth than people with higher education levels and less complex health conditions (de Veer et al., 2015; Greenhalgh et al., 2018). Perceptions, such as the belief that eHealth will help, the perceived ease of use of an eHealth tool, the extent to which the results of an eHealth tool are easily observed, and self-efficacy were found to be strongly related to the use of eHealth (de Veer et al., 2015; Duman-Lubberding et al., 2016; Peeters et al., 2012). In addition, the current results suggest that patients lose interest in eHealth as they become weaker. Future research into the relationship between the added value of Oncokompas and advanced disease is desirable.
The nurse-led intervention to enhance self-management was structured using five steps: assess, advise, agree, assist, and arrange. Seventy-four percent of the patients (n = 25 of 34) recognized these steps as being applied by their nurse. Nurses particularly assessed problems, wishes, and needs, and gave information and advice. Setting goals, nurses’ assistance in achieving these goals, and arranging future care were less often applied, according to patients. This corresponds to what nurses themselves in this study indicated they had applied during the study period (Slev et al., 2020). A study among nurses showed that nurses felt confident in assessing and advising, but less confident in agreeing on goals, assisting patients in achieving these goals, and arranging follow-up care (Jongerden et al., 2019). The general skill level of the nurses may play a role in nurses feeling confident in applying the five steps.
This study also evaluated the potential effectiveness of the intervention on patient activation and QOL. Patient activation is a prerequisite of self-management behavior. High patient activation was found to be associated with higher engagement in advance care planning (David et al., 2018), which is an important aspect of qualitatively good palliative care and self-management in terms of patients contributing to their care. The mean activation scores in the group were 58 (T0) and 53 (T1), corresponding to mean activation scores of people who rated their own health as poor or fair (Hibbard et al., 2005). The post-test activation scores of the group were lower than the mean score found for breast cancer survivors (61 at T1) (Melissant et al., 2018). An explanation might be that feeling empowered and self-efficacy are less important for patients with a life-limiting illness as they are for other patient groups (Wakefield et al., 2018). However, there are indications that there might be room for improvement in patient activation.
The intervention did not improve QOL; no statistically significant changes were found across the study period of 12 weeks. It could be argued that even maintaining or slowing down the decline of patient activation and QOL might be a positive effect of the intervention. However, because of the absence of a control group, it is unknown what these patient outcomes would have been without the intervention. Additional information from professionals at T0 and T1 about the functional status of the patient (measured with the Palliative Performance Scale) could also have helped interpret the results.
Strengths and Limitations
A major strength is that the structured, nurse-led self-management support intervention studied is one of the few interventions that offers self-management support for people with incurable cancer (Budhwani et al., 2019; Schulman-Green et al., 2018; Wakefield et al., 2018). In addition, considering the review by Wakefield et al. (2018), this appears to be the first study with a pre- and post-test design among patients facing a life-limiting illness that included a relatively large group of patients.
In addition, the current study also illustrates the difficulty of carrying out intervention studies of patients with incurable cancer. The low activation scores and the high percentage of deceased patients in the nonparticipant group shows the extreme vulnerability of the study group and sets limits on the feasibility of such studies. In addition, patient recruitment turned out to be challenging, given that it took 17 months to include 69 patients. This is partly related to newly referred patients for continuity visits being either too ill to participate or being treated with curative intent, timing of recruitment, and because of nurses’ gatekeeping behavior (Slev et al., 2020). The recruitment and dropout data of 50% can help future studies estimate the number of people with incurable cancer required.
Another strength of this study is the mixed-method design, providing an in-depth picture of the patients’ experiences with distinct features of the intervention, such as the home setting, specialist nurses supporting self-management, and Oncokompas.
Limitations are the small sample size and the lack of a control group, which may have made it difficult to test differences between T0 and T1. Subsequently, no firm conclusions can be made about the efficacy of the intervention. Additional research should be carried out with a control group and larger numbers of patients.
Implications for Nursing Practice and Research
The intervention was appreciated by both nurses (Slev et al., 2020) and patients with incurable cancer for structuring self-management support and enhancing self-management of disease-related problems and needs. Using a model that distinguishes various domains of self-management, such as the Dutch General Model of Self-Management (Dutch Institute for Healthcare Improvement, 2014; Timmermans & Havers, 2013), could further improve the potential effectiveness of the intervention. This model distinguishes four self-management domains: experience-based knowledge, living with the condition, contributing to care, and organization of care and support. Nurses could use these domains to systematically assess problems and needs within each domain and further tailor their self-management support.
Additional testing of Oncokompas is needed prior to translation into the clinical arena. The prototype of Oncokompas for patients in the palliative phase of the disease that was used in this study has been developed further and is currently being tested in a randomized controlled trial (Schuit et al., 2019). Nurses stated that discussing the outcomes of Oncokompas allowed quicker assessment of patients’ problems and needs and helped them to tailor their self-management support better (Slev et al., 2020). As patients’ intentions to use eHealth depend strongly on their perceptions and expectations of eHealth (de Veer et al., 2015; Duman-Lubberding et al., 2016; Peeters et al., 2012), it is important that nurses help their patients with using Oncokompas by, for instance, explaining the use and showing the possibilities, as well as showing the possible gains of using Oncokompas.
It is advisable to offer the intervention as early in the palliative phase as possible. Patients’ perspectives of their deteriorating physical and mental health may make them lose faith in how they themselves could still take control of matters. If it is offered earlier in the palliative phase, patients will have more time to learn how to self-manage and how they can stay in control over their life and their care, and subsequently maintain their QOL. Using the Palliative Performance Scale score (or something similar) might assist in establishing a continuum of when such an intervention is helpful and when it is not. Additional research is needed. 
Conclusion
People with incurable cancer gave a positive assessment of the nurse-led self-management support intervention, although the usage of Oncokompas was rather low. The intervention did not positively influence patient activation and QOL. Offering patients the intervention in an earlier phase might enhance the efficacy of the intervention.
The authors gratefully acknowledge all the patients and nurses for their participation, and research assistants Malika Dahmaza and Sacha Onwuteaka for their logistical assistance and data gathering and data entry during the study.
About the Author(s)
Anke J.E. de Veer, PhD, is a senior researcher at the Netherlands Institute of Health Services Research (Nivel) in Utrecht; Vina N. Slev, PhD, is a researcher and H. Roeline Pasman, PhD, is an associate professor, both at Amsterdam University Medical Center (UMC), Vrije Universiteit Amsterdam, Department of Public and Occupational Health, Amsterdam Public Health Research Institute, and at the Expertise Center for Palliative Care; Irma M. Verdonck-de Leeuw, PhD, is a professor at Vrije Universiteit Amsterdam Public Health, Faculty of Behavioral and Movement Sciences Department of Clinical, Neuro and Developmental Psychology, a professor at Cancer Center Amsterdam, and a professor at Amsterdam UMC, Vrije Universiteit Amsterdam, Department of Otolaryngology–Head and Neck Surgery; Anneke L. Francke, PhD, is a professor at Netherlands Institute of Health Services Research (Nivel), a professor at Amsterdam UMC, Vrije Universiteit Amsterdam, Department of Public and Occupational Health, Amsterdam Public Health Research Institute, and a professor at the Expertise Center for Palliative Care; and Cornelia F. van Uden-Kraan, PhD, is a senior researcher at Vrije Universiteit Amsterdam Public Health, Faculty of Behavioral and Movement Sciences Department of Clinical, Neuro and Developmental Psychology, and a senior researcher at Cancer Center Amsterdam, all in the Netherlands. This study has been funded by ZonMw, the Netherlands Organisation for Health Research and Development, as part of the Tussen Weten en Doen program (grant No. 520002001). ZonMw had no involvement in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. Slev, Pasman, Verdonck-de Leeuw, Francke, and van Uden-Kraan contributed to the conceptualization and design. Slev and van Uden-Kraan completed the data collection. De Veer and Slev provided statistical support. De Veer, Slev, and Francke provided the analysis. All authors contributed to the manuscript preparation. De Veer can be reached at a.deveer@nivel.nl, with copy to ONFEditor@ons.org. (Submitted July 2019. Accepted December 6, 2019.)
References
Alawneh, A., Yasin, H., Khirfan, G., Qayas, B.A., Ammar, K., Rimawi, D., & Klepstad, P. (2016). Psychometric properties of the Arabic version of EORTC QLQ-C15-PAL among cancer patients in Jordan. Supportive Care in Cancer, 24(6), 2455–2462. https://doi.org/10.1007/s00520-015-3018-9
Bailey, D.E., Jr., Steinhauser, K., Hendrix, C., & Tulsky, J.A. (2011). Pairing self-management with palliative care: Intervening in life-limiting illness. Journal of Nursing and Healthcare of Chronic Illness, 3(1), 1–3. https://doi.org/10.1111/j.1752-9824.2011.01083.x
Barlow, J., Wright, C., Sheasby, J., Turner, A., & Hainsworth, J. (2002). Self-management approaches for people with chronic conditions: A review. Patient Education and Counseling, 48(2), 177–187. https://doi.org/10.1016/S0738-3991(02)00032-0
Beck, D., Been-Dahmen, J., Peeters, M., Grijpma, J.W., van der Stege, H., Tielen, M., . . . van Staa, A. (2019). A nurse-led self-management support intervention (ZENN) for kidney transplant recipients using intervention mapping: Protocol for a mixed-methods feasibility study. JMIR Research Protocols, 8(3), e11856. https://doi.org/10.2196/11856
Bjorner, J.B., Petersen, M.A., Groenvold, M., Aaronson, N., Ahlner-Elmqvist, M., Arraras, J.I., . . . Young, T. (2004). Use of item response theory to develop a shortened version of the EORTC QLQ-C30 emotional functioning scale. Quality of Life Research, 13(10), 1683–1697. https://doi.org/10.1007/s11136-004-7866-x
Bodenheimer, T., Lorig, K., Holman, H., & Grumbach, K. (2002). Patient self-management of chronic disease in primary care. JAMA, 288(19), 2469–2475.
Budhwani, S., Wodchis, W.P., Zimmermann, C., Moineddin, R., & Howell, D. (2019). Self-management, self-management support needs and interventions in advanced cancer: A scoping review. BMJ Supportive and Palliative Care, 9(1), 12–25. https://doi.org/10.1136/bmjspcare-2018-001529
Central Committee on Research Involving Human Subjects. (n.d.). Your research: Is it subject to the WMO or not? Retrieved January, 2016 from https://english.ccmo.nl/investigators/legal-framework-for-medical-scien…
Charalambous, A., Wells, M., Campbell, P., Torrens, C., Östlund, U., Oldenmenger, W., . . . Kelly, D. (2018). A scoping review of trials of interventions led or delivered by cancer nurses. International Journal of Nursing Studies, 86, 36–43. https://doi.org/10.1016/j.ijnurstu.2018.05.014
Committee on Nursing Roles. (2015). Future-proofed professions in nursing. Report of the Committee on Nursing Roles. https://www.nfu.nl/img/pdf/Rapport_toekomstbestendige-beroepen-in-de-ve…
Coolbrandt, A., Milisen, K., Wildiers, H., Aertgeerts, B., van Achterberg, T., Van der Elst, E., & Dierckx de Casterlé, B. (2018). A nursing intervention aimed at reducing symptom burden during chemotherapy (CHEMO-SUPPORT): A mixed-methods study of the patient experience. European Journal of Oncology Nursing, 34, 35–41. https://doi.org/10.1016/j.ejon.2018.03.002
David, D., Barnes, D.E., McMahan, R.D., Shi, Y., Katen, M.T., & Sudore, R.L. (2018). Patient activation: A key component of successful advance care planning. Journal of Palliative Medicine, 21(12). https://doi.org/10.1089/jpm.2018.0096
de Veer, A.J.E., Peeters, J.M., Brabers, A.E., Schellevis, F.G., Rademakers, J.J.D.J.M., & Francke, A.L. (2015). Determinants of the intention to use e-health by community dwelling older people. BMC Health Services Research, 15, 103. https://doi.org/10.1186/s12913-015-0765-8
Docter, A.F., Dingemans, I.H., & Willemse, K. (2010). Nazorg thuis voor kankerpatiënten noodzakelijk. [At home aftercare necessary for cancer patients]. Nederlands Tijdschrift voor Oncologie, 7(8), 324–329.
Duman-Lubberding, S., van Uden-Kraan, C.F., Jansen, F., Witte, B.I., van der Velden, L.A., Lacko, M., . . . Verdonck-de Leeuw, I.M. (2016). Feasibility of an eHealth application “OncoKompas” to improve personalized survivorship cancer care. Supportive Care in Cancer, 24(5), 2163–2171. https://doi.org/10.1007/s00520-015-3004-2
Duman-Lubberding, S., van Uden-Kraan, C.F., Peek, N., Cuijpers, P., Leemans, C.R., & Verdonck-de Leeuw, I.M. (2015). An eHealth application in head and neck cancer survivorship care: Health care professionals’ perspectives. Journal of Medical Internet Research, 17(10), e235. https://doi.org/10.2196/jmir.4870
Dutch Institute for Healthcare Improvement. (2014). Zorgmodule zelfmanagement 1.0. Het ondersteunen van eigen regie bij mensen met één of meerdere chronische ziekten [Dutch national care standard on self-management 1.0]. http://www.partnerschapovergewicht.nl/images/Organisatie/2014_03_Zorgmo…
Eysenbach, G. (2001). What is e-health? Journal of Medical Internet Research, 3(2), E20. https://doi.org/10.2196/jmir.3.2.e20
Fayers, P., & Bottomley, A. (2002). Quality of life research within the EORTC—The EORTC QLQ-C30. European Journal of Cancer, 38(Suppl. 4), 125–133. https://doi.org/10.1016/S0959-8049(01)00448-8
Glasgow, R.E., Davis, C.L., Funnell, M.M., & Beck, A. (2003). Implementing practical interventions to support chronic illness self-management. Joint Commission Journal on Quality and Safety, 29(11), 563–574. https://doi.org/10.1016/S1549-3741(03)29067-5
Golčić, M., Dobrila-Dintinjana, R., Golčić, G., Pavlović-Ružić, I., Stevanović, A., & Gović- Golčić, L. (2018). Quality of life in a hospice: A validation of the Croatian version of the EORTC QLQ-C15-PAL. American Journal of Hospice and Palliative Medicine, 35(8), 1085–1090. https://doi.org/10.1177/1049909118760781
Greene, J., & Hibbard, J.H. (2012). Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. Journal of General Internal Medicine, 27(5), 520–526.
Greene, J., Hibbard, J.H., Sacks, R., Overton, V., & Parrotta, C.D. (2015). When patient activation levels change, health outcomes and costs change, too. Health Affairs, 34(3), 431–437. https://doi.org/10.1377/hlthaff.2014.0452
Greenhalgh, T., Wherton, J., Papoutsi, C., Lynch, J., Hughes, G., A’Court, C., . . . Shaw, S. (2018). Analysing the role of complexity in explaining the fortunes of technology programmes: Empirical application of the NASSS framework. BMC Medicine, 16(1), 66. https://doi.org/10.1186/s12916-018-1050-6
Groenvold, M., Petersen, M.A., Aaronson, N.K., Arraras, J.I., Blazeby, J.M., Bottomley, A., . . . Bjorner, J.B. (2006). The development of the EORTC QLQ-C15-PAL: A shortened questionnaire for cancer patients in palliative care. European Journal of Cancer, 42(1), 55–64. https://doi.org/10.1016/j.ejca.2005.06.022
Group Health Research Institute. (n.d.). Self-management support. Retrieved April 20, 2015, from http://www.improvingchroniccare.org/index.php?p=Self-Management_Support…
Hibbard, J.H., & Mahoney, E. (2010). Toward a theory of patient and consumer activation. Patient Education and Counseling, 78(3), 377–381. https://doi.org/10.1016/j.pec.2009.12.015
Hibbard, J.H., Mahoney, E.R., Stock, R., & Tusler, M. (2007). Do increases in patient activation result in improved self-management behaviors? Health Services Research, 42(4), 1443–1463. https://doi.org/10.1111/j.1475-6773.2006.00669.x
Hibbard, J.H., Mahoney, E.R., Stockard, J., & Tusler, M. (2005). Development and testing of a short form of the patient activation measure. Health Services Research, 40(6p1), 1918–1930. https://doi.org/10.1111/j.1475-6773.2005.00438.x
Hibbard, J.H., Stockard, J., Mahoney, E.R., & Tusler, M. (2004). Development of the patient activation measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research, 39(4p1), 1005–1026. https://doi.org/10.1111/j.1475-6773.2004.00269.x
Hui, D., Glitza, I., Chisholm, G., Yennu, S., & Bruera, E. (2013). Attrition rates, reasons, and predictive factors in supportive care and palliative oncology clinical trials. Cancer, 119(5), 1098–1105. https://doi.org/10.1002/cncr.27854
Huis in het Veld, J.G., Willemse, B.M., van Asch, I.F.M., Groot Zwaaftink, R.B., Verkade, P.J., Veldhuijzen, N.J., . . . Francke, A.L. (2017). Online self-management support for family caregivers to help them manage behavior changes in their relative with dementia: Study protocol for a randomized controlled trial and a process evaluation. JMIR Research Protocols, 6(11), e239. https://doi.org/10.2196/resprot.8365
Jongerden, I.P., Slev, V.N., van Hooft, S.M., Pasman, H.R., Verdonck-de Leeuw, I.M., de Veer, A.J.E., . . . Francke, A.L. (2019). Self-management support in patients with incurable cancer: How confident are nurses? Oncology Nursing Forum, 46(1), 104–112. https://doi.org/10.1188/19.onf.104-112
Kleijn, G., van Uden-Kraan, C.F., Bohlmeijer, E.T., Becker-Commissaris, A., Pronk, M., Willemsen, V., . . . Verdonck-de Leeuw, I.M. (2019). Patients’ experiences of life review therapy combined with memory specificity training (LRT-MST) targeting cancer patients in palliative care. Supportive Care in Cancer, 27(9), 3311–3319. https://doi.org/10.1007/s00520-018-4613-3
Lorig, K.R., & Holman, H.R. (2003). Self-management education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine, 26(1), 1–7. https://doi.org/10.1207/s15324796abm2601_01
Melissant, H.C., Verdonck-de Leeuw, I.M., Lissenberg-Witte, B.I., Konings, I.R., Cuijpers, P., & Van Uden-Kraan, C.F. (2018). ‘Oncokompas’, a web-based self-management application to support patient activation and optimal supportive care: A feasibility study among breast cancer survivors. Acta Oncologica, 57(7), 924–934. https://doi.org/10.1080/0284186x.2018.1438654
Moens, K., Higginson, I.J., & Harding, R. (2014). Are there differences in the prevalence of palliative care-related problems in people living with advanced cancer and eight non-cancer conditions? A systematic review. Journal of Pain and Symptom Management, 48(4), 660–677. https://doi.org/10.1016/j.jpainsymman.2013.11.009
Peeters, J.M., de Veer, A.J.E., van der Hoek, L., & Francke, A.L. (2012). Factors influencing the adoption of home telecare by elderly or chronically ill people: A national survey. Journal of Clinical Nursing, 21(21–22), 3183–3193. https://doi.org/10.1111/j.1365-2702.2012.04173.x
Rademakers, J., Nijman, J., van der Hoek, L., Heijmans, M., & Rijken, M. (2012). Measuring patient activation in the Netherlands: Translation and validation of the American short form patient activation measure (PAM13). BMC Public Health, 12, 577. https://doi.org/10.1186/1471-2458-12-577
Rask, K.J., Ziemer, D.C., Kohler, S.A., Hawley, J.N., Arinde, F.J., & Barnes, C.S. (2009). Patient activation is associated with healthy behaviors and ease in managing diabetes in an indigent population. Diabetes Educator, 35(4), 622–630. https://doi.org/10.1177/0145721709335004
Salgado, T.M., Mackler, E., Severson, J.A., Lindsay, J., Batra, P., Petersen, L., & Farris, K.B. (2017). The relationship between patient activation, confidence to self-manage side effects, and adherence to oral oncolytics: A pilot study with Michigan oncology practices. Supportive Care in Cancer, 25(6), 1797–1807. https://doi.org/10.1007/s00520-017-3584-0
Sarmento, V.P., Gysels, M., Higginson, I.J., & Gomes, B. (2017). Home palliative care works: But how? A meta-ethnography of the experiences of patients and family caregivers. BMJ Supportive and Palliative Care, 7(4), 390–403.
Schuit, A.S., Holtmaat, K., Hooghiemstra, N., Jansen, F., Lissenberg-Witte, B.I., Coupé, V.M.H., . . . Verdonck-de Leeuw, I.M. (2019). Efficacy and cost-utility of the eHealth application ‘Oncokompas,’ supporting patients with incurable cancer in finding optimal palliative care, tailored to their quality of life and personal preferences: A study protocol of a randomized controlled trial. BMC Palliative Care, 18, 85. https://doi.org/10.1186/s12904-019-0468-8
Schulman-Green, D., Brody, A., Gilbertson-White, S., Whittemore, R., & McCorkle, R. (2018). Supporting self-management in palliative care throughout the cancer care trajectory. Current Opinion in Supportive and Palliative Care, 12(3), 299–307. 10.1097/spc.0000000000000373
Schulman-Green, D., Jaser, S., Martin, F., Alonzo, A., Grey, M., McCorkle, R., . . . Whittemore, R. (2012). Processes of self-management in chronic illness. Journal of Nursing Scholarship, 44(2), 136–144. https://doi.org/10.1111/j.1547-5069.2012.01444.x
Slev, V., Molenkamp, C., van Uden-Kraan, N., Francke, A., Verdonck-de Leeuw, I., Pasman, R., & Eeltink, C. (2016). Intervention protocol for ‘self-management support in incurable cancer.’ https://nivel.nl/sites/default/files/pdf/interventieprotocol-sms-EN.pdf
Slev, V.N., Molenkamp, C.M., Eeltink, C.M., Pasman, H.R.W., Verdonck-de Leeuw, I.M., Francke, A.L., & van Uden-Kraan, C.F. (2020). A nurse-led self-management support intervention for patients and informal caregivers facing incurable cancer: A feasibility study from the perspective of nurses. European Journal of Oncology Nursing, 45(101716), 10. https://doi.org/10.1016/j.ejon.2019.101716
Suárez-del-Real, Y., Allende-Pérez, S., Alférez-Mancera, A., Rodríguez, R.B., Jiménez-Toxtle, S., Mohar, A., & Oñate-Ocaña, L.F. (2011). Validation of the Mexican-Spanish version of the EORTC QLQ-C15-PAl questionnaire for the evaluation of health-related quality of life in patients on palliative care. Psycho-Oncology, 20(8), 889–896. https://doi.org/10.1002/pon.1801
Timmermans, H., & Havers, J. (2013). [The general model of self-management]. In R. van den Brink, H. Timmermans, J. Havers, & H. van Veenendaal (Eds.), [Room for control: Pioneers about self-management in care]. Kluwer.
van der Hout, A., van Uden-Kraan, C.F., Witte, B.I., Coupé, V.M.H., Jansen, F., Leemans, C.R., . . . Verdonck-de Leeuw, I.M. (2017). Efficacy, cost-utility and reach of an eHealth self-management application ‘Oncokompas’ that helps cancer survivors to obtain optimal supportive care: Study protocol for a randomised controlled trial. Trials, 18, 228.
van Harteveld, J.T.M., Mistiaen, P.J.M.L., & Dukkers van Emden, D.M. (1997). Home visits by community nurses for cancer patients after discharge from hospital: An evaluation study of the continuity visit. Cancer Nursing, 20(2), 105–114. https://doi.org/10.1097/00002820-199704000-00005
Von Korff, M., Gruman, J., Schaefer, J., Curry, S.J., & Wagner, E.H. (1997). Collaborative management of chronic illness. Annals of Internal Medicine, 127(12), 1097–1102. https://doi.org/10.7326/0003-4819-127-12-199712150-00008
Wakefield, D., Bayly, J., Selman, L.E., Firth, A.M., Higginson, I.J., & Murtagh, F.E.M. (2018). Patient empowerment, what does it mean for adults in the advanced stages of a life-limiting illness: A systematic review using critical interpretive synthesis. Palliative Medicine, 32(8), 1288–1304. https://doi.org/10.1177/0269216318783919
Zhang, L., Wang, N., Zhang, J., Liu, J., Luo, Z., Sun, W., . . . Wang, C. (2016). Cross-cultural verification of the EORTC QLQ-C15-PAL questionnaire in mainland China. Palliative Medicine, 30(4), 401–408. https://doi.org/10.1177/0269216315593671
Zuidema, R., van Dulmen, S., Nijhuis-van der Sanden, M., Meek, I., van den Ende, C., Fransen, J., & van Gaal, B. (2019). Efficacy of a web-based self-management enhancing program for patients with rheumatoid arthritis: Explorative randomized controlled trial. Journal of Medical Internet Research, 21(4), e12463. https://doi.org/10.2196/12463




