A Qualitative Cultural Sensitivity Assessment of the Breathe Easier Mobile Application for Lung Cancer Survivors and Their Families
Purpose: To evaluate the cultural sensitivity of the Breathe Easier mobile health application for African American lung cancer survivors and their families. Breathe Easier is an intervention designed to teach strategies to combat symptoms related to lung cancer.
Participants & Setting: 12 African American lung cancer survivors and their family members were recruited from an American College of Surgeons–approved cancer program in South Carolina.
Methodologic Approach: Participants completed in-depth interviews, which were guided by the Cultural Sensitivity Assessment Tool and the Cultural Sensitivity Checklist. Two researchers performed open and axial coding to conceptually organize the data.
Findings: Multiple culturally relevant themes emerged, including benefits, concerns, and suggestions related to content literacy and inclusiveness, as well as acceptability of and motivations for using the mobile application. However, lung cancer survivors and their family members reported being more concerned about accessing accurate survivorship information.
Implications for Nursing: Attention to health literacy, eHealth literacy, and cultural sensitivity may enhance patient outcomes, and nurses can advocate for patients regarding these communication issues.
Jump to a section
Cultural sensitivity is the extent to which health information materials accommodate cultural, historical, environmental, social, and psychological factors or values (Barrera et al., 2013). Culture is a key driver of cancer outcomes because of its influence on values, attitudes, beliefs, and behaviors related to prevention, diagnosis, treatment, and survivorship (Kagawa-Singer et al., 2010). Previous research has shown that the cultural beliefs of African Americans may affect how and to what extent they participate in their lung cancer care (Jonnalagadda et al., 2012; Lin et al., 2014). According to Jonnalagadda et al. (2012), ethnic minorities, including African Americans, may have more fatalistic views and misconceptions about cancer than Caucasians, which can affect whether they receive timely and adequate treatment. Developing community-driven interventions that address the cultural beliefs and heritage of African Americans can improve their response to cancer communication interventions (Huang & Shen, 2016) and enhance patient–provider communication (Li et al., 2017). Culturally sensitive interventions are warranted for African American lung cancer survivors and their family members in particular because of their higher rate of lung cancer mortality (Siegel et al., 2019) and poorer survivorship outcomes (Bryant & Cerfolio, 2008; Chang et al., 2016).
Background
Lung cancer is the second most common and deadliest cancer in the United States, accounting for more than one-fourth of all cancer-related deaths (Siegel et al., 2019). However, African Americans experience the highest mortality (64%) and have lower five-year survival rates (18%) than Caucasians (54% mortality and 20% five-year survival rates, respectively) (American Cancer Society [ACS], 2019a; Siegel et al., 2019). This disparity may be attributed partly to later diagnosis, a lower likelihood of undergoing surgery following diagnosis, and longer time periods between diagnosis and treatment (ACS, 2019a; Holmes & Chen, 2018). Despite the high mortality associated with lung cancer, five-year survival rates have shown a steady increase for all individuals. The five-year survival rates for individuals diagnosed with localized, regional, or distal lung cancer from 2008 to 2014 were 56%, 30%, and 5%, respectively. These rates are markedly improved compared to survival rates from 1975 to 1990, which were 47% for localized lung cancer, 16% for regional lung cancer, and 2% for distal lung cancer. From 2009 to 2015, the average five-year survival rate for individuals diagnosed with localized lung cancer was 57%, and the average five-year survival rate for individuals whose cancer spread regionally or distantly was 31% and 5%, respectively (Jemal et al., 2017). According to the National Cancer Institute Surveillance, Epidemiology, and End Results Program (n.d.), about 540,000 lung cancer survivors live in the United States. A cancer survivor refers to “any person with a history of cancer, from the time of diagnosis through the remainder of their life” (ACS, 2019b, p. 1).
Mindfulness-Based Stress Reduction
Following treatment, which may involve surgery, chemotherapy, and/or radiation therapy, lung cancer survivors often experience side effects, such as dyspnea, fatigue, and pain, which can be exacerbated by stress and compromise quality of life (Poghosyan et al., 2013; Vijayvergia et al., 2015). Lung cancer can also influence the stress levels of family members who are intimately involved in the survivor’s care (Tan et al., 2018). Unchecked, this stress can lead to negative consequences, like chronic illness, for family members (Oliveira et al., 2016).
To combat the symptoms of lung cancer, organizations such as the American College of Chest Physicians recommend the use of complementary therapy (Deng et al., 2013). These therapies include mindfulness-based stress reduction (MBSR), which was developed to manage pain and stress and has been shown to relieve symptoms related to lung cancer (Kabat-Zinn, 1982; Kabat-Zinn et al., 1985). The standard MBSR program consists of eight weeks of courses (2.5–3.5 hours in duration) and home activities (45 minutes per day) that include practices such as meditation, yoga, and breathing exercises (Santorelli, 2014). MBSR is a therapy that is commonly used for improving health and quality of life in individuals with a range of mental and physical conditions, including cancer (Cillessen et al., 2019; de Vibe et al., 2017; Li & Bressington, 2019; Rush & Sharma, 2017). For lung cancer in particular, MBSR or similar mindfulness-based interventions have been understudied, but three previous studies have employed these interventions in patients with lung cancer. In a randomized controlled trial of 107 participants in the Netherlands, Schellekens et al. (2017) assessed whether lung cancer survivors and family members who received MBSR in addition to standard of care had lower psychological distress; secondary outcomes explored quality of life, relationship satisfaction, caregiver burden, mindfulness skills, self-compassion, rumination, and post-traumatic stress syndrome. Although survivors in the MBSR group showed significant improvement across all but two outcomes (relationship satisfaction and caregiver burden), family members in the MBSR group did not show significant differences in outcomes when compared to family members in the standard of care group (Schellekens et al., 2017). Schellekens et al. (2017) were the only research group to study the effectiveness of MBSR among lung cancer survivors and family members (i.e., dyads). A pilot study by Lehto et al. (2015) of 40 lung cancer survivors in the United States who received a modified MBSR intervention aimed to determine whether participants receiving the intervention had less symptom severity and interference and greater improvements in other health-related quality-of-life parameters, such as physical and social function, compared to those who received standard of care. Although the sample size was small, Lehto et al. (2015) found that survivors in the intervention group (n = 20) had moderate to meaningful differences on all outcomes when compared to the control group using linear mixed-effects models. Another pilot study by McDonnell, Gallerani, et al. (2019) assessed whether an MBSR intervention for 32 dyads of Caucasian and African American lung cancer survivors and their family members led to changes in dyspnea, fatigue, sleep quality, and perceived stress over time. The results from McDonnell, Gallerani, et al.’s (2019) study showed that survivors had significantly less dyspnea and perceived stress over time, and survivors and family members had improved fatigue and sleep scores from pre- to postintervention.
Mobile Health Interventions
According to Smith (2014a), African Americans are less likely to have access to a computer or Internet at home compared to Caucasians, but they have almost equal access to smartphones (80% versus 82%, respectively); however, the adoption rate is only 55% among adults aged 65 years or older (Smith, 2014b). African Americans are more likely than Caucasians to use their smartphones for activities such as identifying health information (Anderson, 2015). Therefore, it has been posited that delivering interventions via mobile platforms could eliminate disparities in cancer survivorship and mediate barriers and access to care (e.g., transportation) and information (Gonzalez, 2018). Several mobile health (mHealth) interventions have been developed for improving disease education, chronic symptom management, and access to health care for a range of diseases, including cancer (Loh et al., 2018; Marcolino et al., 2018). mHealth interventions have been demonstrated to be acceptable and efficient for African Americans (James et al., 2016), but this population is not well represented across mHealth studies (James et al., 2017).
This study aimed to qualitatively assess the cultural sensitivity of a mobile application called Breathe Easier, which was designed to teach African American lung cancer survivors and their family members how to self-manage symptom burden and improve quality of life. The mobile application was developed to expand access to the Breathe Easier intervention so that it could be easily disseminated to lung cancer survivors and families across the country.
Methods
Participants and Setting
The Breathe Easier mobile application was adapted from an eight-week, dyadic (lung cancer survivor and family), in-person mindfulness-based intervention by the same name. Each week contains a combination of audio-directed breathing practices, meditations, and yoga exercises of varying levels, which are demonstrated using instructional text and images of African American and Caucasian adults aged 55 years or older performing various poses. Twelve African American lung cancer survivors and family members (six survivor–caregiver dyads) who had previously participated in the face-to-face intervention completed the current study. Interviews took place with each survivor and family member individually in a conference room at a local medical center in urban South Carolina. This study received institutional review board approval from the University of South Carolina in Columbia.
Methodologic Approach
Participants were invited to engage in audio-recorded interviews lasting 30–60 minutes about the cultural sensitivity of the Breathe Easier mobile application. Study details were provided to all participants immediately prior to their participation through a written informed consent document. Two of the authors answered participant questions and conducted the interviews. After any questions were addressed, participants signed the written consent document. The interview guide, which was based on the Cultural Sensitivity Checklist (Friedman & Hoffman-Goetz, 2006) and Cultural Sensitivity Assessment Tool (Guidry & Walker, 1999), focused specifically on assessing the Breathe Easier mobile application’s content (e.g., whether it is easy to understand and culturally relevant for African Americans), images (e.g., how representative it is of African American survivors and families), and audio recordings (e.g., appropriateness for guiding African Americans through the intervention). In addition to informing the authors’ conceptual orientation to cultural sensitivity, the Cultural Sensitivity Checklist and Cultural Sensitivity Assessment Tool have been used in previous research to assess the cultural sensitivity of printed, web-based, and mobile-based health media (Choi et al., 2018; Owens et al., 2018). To make the checklist and assessment specific to this study, the questions were adapted to fit the context of the Breathe Easier mobile application (see Figure 1). 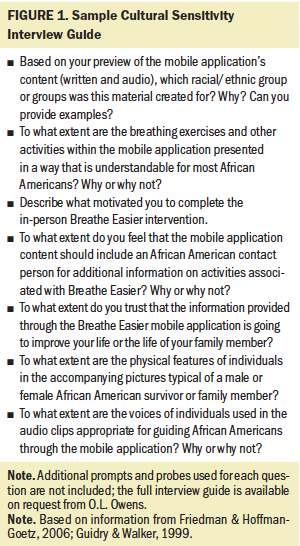
Data Analysis
Audio-recorded interviews were professionally transcribed and uploaded to the qualitative data analysis software MAXQDA™, version 12.0. The interviews were reviewed by one individual on the research team and compared to the professional transcripts for accuracy. A grounded theory methodology, which uses a constant comparative method to categorize data into relevant themes and compare identified themes to previous discoveries in the existing literature (Strauss & Corbin, 1997), was used as a framework for the data analysis. Saturation was based on the point at which no new salient themes emerged following the assessment of the interviewers’ expertise and written logs of some of the key points that were heard during the interviews (Saunders et al., 2018). Open coding was conducted by two raters from the research team to conceptually organize the data (Strauss & Corbin, 1997). During the open-coding process, semantic codes were assigned to sections of the interview transcripts and compared to ensure consistency. The research team then discussed these codes until consensus about the definition of each code was reached and a comprehensive list of codes was finalized (Strauss & Corbin, 1997). The two raters then independently used the codebook to analyze the two longest interview transcripts. The research team then discussed areas of disagreement, updated the codebook, and independently recoded the same two transcripts. Following the second round of coding, MAXQDA, version 12.0, was used to calculate reliability between the two independent raters (Hallgren, 2012). For this study, the percentage of agreement was 83%, which is considered acceptable (Hruschka et al., 2004). After resolving coding discrepancies, one rater coded the remaining 10 transcripts independently. During the axial coding process, the rater identified relationships among codes that were suggestive of themes and these themes were then compared among interviews (Strauss & Corbin, 1997). After completing the coding process, the two raters discussed and organized the final findings based on the themes that had emerged.
Findings
The study sample consisted of 12 African American lung cancer survivors (n = 6) and their family members (n = 6). Participant ages ranged from 29 to 73 years, with a mean age of 59 years (SD = 12.5). The following five major themes emerged from the data: (a) cultural sensitivity of content, (b) motivation for completing the intervention, (c) acceptability of mobile application, (d) quality of life, and (e) cancer versus culture. These themes are explicated in the following sections. Example quotes and suggestions for improvement from participants are presented in Figure 2. Although themes did not vary significantly between survivors and family members, quotes are denoted based on whether they were spoken by a survivor or a family member. 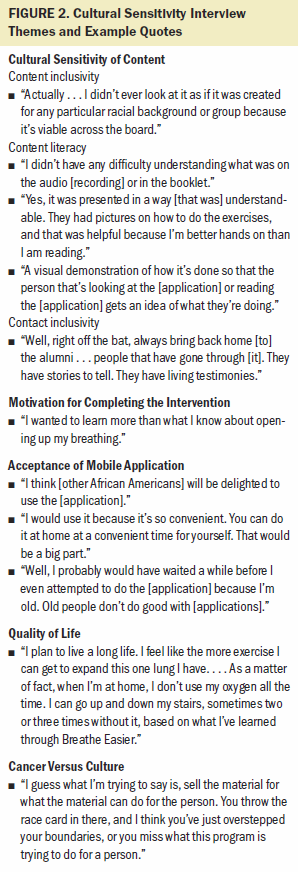
Cultural Sensitivity of Content
Overall, the most prominent theme was related to the cultural sensitivity of the Breathe Easier mobile application’s audio and visual content. The following three subthemes emerged related to cultural sensitivity: content inclusivity (the extent to which the content was appropriate for most African Americans), content literacy (the extent to which the information can be comprehended by most African Americans), and researcher contact inclusivity (the extent to which the contacts were relevant for African Americans).
Content inclusivity: The majority of participants believed that the content of Breathe Easier was appropriate for most African Americans. The audio recordings from African American and Caucasian individuals who guided participants through the weekly mindfulness exercises in the mobile application were perceived as appropriate for most participants. However, mindfulness-based practice was new to many participants as evidenced by one survivor who said, “There [are] Black people that, I’m sure, are into yoga and meditation, but the percentage is very small.” Audio instructions for each exercise were accompanied by relaxing slow music, which was deemed to be less favorable for most participants because it made them too relaxed and put some participants to sleep. Three participants suggested changing the music, with one survivor saying, “I think the audio version needs to be changed because to sit there and meditate . . . you’re going to sleep.” When asked how the music should be changed, a second survivor responded, “You should have had some . . . I don’t know, some upbeat music. Maybe a little . . . some type of jazzercise.” Images of African American and Caucasian individuals demonstrating seated yoga poses were also included in the mobile application and were perceived to be relatable to all participants.
Content literacy: The text within the mobile application was written in plain language so that participants of varying health literacy levels could understand. Participants perceived that the information could be understood by most African Americans, but they believed that some of the words that were included would not be as familiar. One family member told the interviewer “it all needs to be put in laymen terms,” whereas another survivor said, “I can read this, and it tells me what to do, but I’m better hands-on with a picture or something.” A second family member suggested that “more pictures would be a good idea.”
Contact inclusivity: The contacts included for Breathe Easier were all Caucasian individuals (principal investigator and two research coordinators). Most participants agreed that providing an African American contact person would enhance its cultural sensitivity, but many participants stated that this feature would be more important to other African Americans than to themselves. Many participants reported that they did not care about the race of the contact person as long as they were able to gather information that could improve their or their family members’ quality of life. For example, one family member said the following:
As the human race goes, possibly because someone of the same ethnic background might have . . . the African American may be more comfortable with another African American person. That’s not always the case, but, in a lot of cases, it is.
Similarly, a survivor said, “That’s not important . . . just as long as they have the knowledge.” One suggestion made by a family member was to include contact information and testimonials from participants who had previously used the mobile application.
Motivation for Completing the Intervention
All participants reported being motivated to complete the in-person Breathe Easier intervention to learn techniques for managing symptoms and enhancing quality of life. One survivor said, “I wanted to learn more than what I know about opening up my breathing.” Most quotes from family members demonstrated that they did not necessarily expect a personal benefit; instead, they felt that they would learn additional information about the disease that could help survivors or that their attendance could motivate survivors to sustain participation. One family member said, “So, I came to learn basically what to do . . . how to take care of her.” Another family member stated that “I wanted to see him get better.”
Quality of Life
All survivors and family members felt that participating in the Breathe Easier intervention and using the mobile application benefited the survivor physically. According to one survivor, “I can go up and down my stairs, sometimes two or three times without [oxygen], based on what I’ve learned through Breathe Easier.” All family members agreed that Breathe Easier helped them to gain knowledge about how to assist the survivor, and about half reported that they had experienced personal benefits from incorporating the techniques in their own lives. For example, one family member said, “It has given me ways of exercising that I did not have previously. I didn’t know I could do certain things, and now I know I can.” Similarly, a second family member told the interviewer, “It helped me, too. I’ve got a lot of medical problems—that’s another story—but it helped me, too.” Because of the success of the Breathe Easier in-person intervention, many participants saw value in offering the Breathe Easier mobile application to lung cancer survivors and their families.
Acceptability of Mobile Application
When asked about the acceptability of the Breathe Easier mobile application, 10 participants reported that they were receptive to using the application; the remaining 2 participants were not sure whether they would adopt it for regular use. Regarding their perceptions about whether other African Americans would use the mobile application, six participants believed that others would use it, four participants were not sure, and two participants had no opinion. One survivor who had a positive perception said, “I think [other African Americans] would. They know it. They need to know it. They would.” A family member said, “I think [other African Americans] will be delighted to use the [application].” A second family member suggested that the research team should consider providing slightly different information for survivors and family members:
You might have to have [application] 1 and 2. Because [application] 1, I’m gonna use the app, and I’m gonna be into it . . . and one of the family members might come along and say, “OK, what’s so interesting about that?”
The four participants who were unsure about whether other African Americans would use the mobile application expressed concern about users’ eHealth literacy (i.e., the ability for an individual to gain health information from an electronic source), particularly if the users are older. One uncertain family member said the following:
I think it would be based on how savvy they are. Because I can easily say, “OK, like, a 65-year-old person can’t do it, but maybe a 65-year-old person has an iPad and a computer, and maybe they play games. Maybe they do more than I do.” So, I think it’s just how savvy they are tech-wise.
Despite this concern, all participants thought using a mobile application would make Breathe Easier more accessible to a larger population of survivors and family members.
Cancer Versus Culture
Seven participants believed that the focus of the cultural sensitivity interview should be to ensure that lung cancer survivors are receiving information on survivorship in plain language. This concern was more important to participants than the cultural sensitivity of the mobile application’s content. Some participants reported that they did not understand why race was important to the discussion if the overall goal was to help improve the lives of survivors. When asked about the appropriateness of the mobile application for African Americans, one family member said the following:
When I look at the picture, I look at people who are trying to improve their health. . . . I don’t know whether it affects one group more than the other. When you have lung cancer, I just see that everybody is in the same boat.
A survivor also reiterated at several points during the interview that “[race is] not important . . . just as long as they have the knowledge.”
Discussion
To the authors’ knowledge, this is the first study to use a community-driven approach to develop a mindfulness-based mobile application to promote self-management of lung cancer symptoms. Overall, participants found Breathe Easier to be culturally sensitive; however, some improvements were suggested, such as adding upbeat music that was stylistically familiar. These findings were similar to those of Woods-Giscombé and Gaylord (2014), who discovered that connecting meditation to a target population’s religious practices (e.g., prayer) and accommodating for cultural familiarity (e.g., meditative drumming) may influence intervention uptake. In addition, Jiang et al. (2013, 2016) found that an individual’s preferred music genre mediated the effects of the music on stress reduction. In particular, preferred music that is higher in tempo can affect an individual’s stress level in the same way as music that is slower in tempo. A meta-analysis by de Witte et al. (2019) indicated that songs that are 60–80 beats per minute yield larger effects than music with another or unspecified tempo regardless of genre; this tempo range includes a number of songs across various genres (e.g., classical, jazz, pop). Based on the studies by Jiang et al. (2013, 2016) and de Witte et al. (2019), attention to music style preferences within a given tempo range among a targeted population may be warranted for reducing stress levels among survivors and family members.
Many participants were highly motivated to complete the in-person Breathe Easier intervention because of their desire to help themselves or their loved one. Although most family members did not expect to experience personal benefits from Breathe Easier beyond learning additional strategies to help their survivor, many family members reported experiencing positive benefits during the eight-week intervention, such as stress reduction. These benefits are consistent with findings from two dyadic studies by Schellekens et al. (2017) and van den Hurk et al. (2015) of survivors and family members, which demonstrated that caregiver burden is reduced significantly when MBSR is added to standard of care for survivors and their family members.
Based on their reviews of the mobile application and outcomes from their experiences with the in-person intervention, a majority of participants reported being willing to adopt the application but were uncertain about widespread adoption. The common concern was related to the eHealth literacy of participants and, more specifically, older African Americans. eHealth literacy refers to “the ability to seek out, find, evaluate and appraise, integrate, and apply what is gained in electronic environments toward solving a problem” (Norman & Skinner, 2006, p. 2). Lower eHealth literacy is associated with poorer health outcomes (Norman & Skinner, 2006). Therefore, in addition to providing training prior to downloading and using the mobile application, it may be advantageous to employ a family-centered approach to mobile application implementation so that younger, more technically experienced participants can facilitate use of the application until the older adult is more comfortable. This upstream approach to instruction is similar to that of a previous dyadic study by Warren-Findlow et al. (2010), in which younger family members shared health information through intergenerational channels with older family members. Similarly, older family members passed information downstream to younger family members to improve their health knowledge (Warren-Findlow et al., 2010). In the current study, this downstream transfer of information from lung cancer survivors to younger family members about their experiences following treatment improved family members’ understanding of the survivor’s condition and needs, which were further substantiated through Breathe Easier. However, this family-centered approach may not be possible for isolated older adults.
Health literacy (i.e., content literacy) was also a commonly reported suggestion from survivors and family members as a way to enhance adoption of Breathe Easier. Health literacy can be applied to all health information, not just information disseminated through an electronic source (Nielsen-Bohlman et al., 2004). In particular, survivors and family members stressed that the research team should ensure that all language used during the intervention and in the application be in layman’s terms. In previous studies, health literacy is presented as an important concern for African American lung cancer survivors and their family members (McDonnell, Owens, et al., 2019; Webb & McDonnell, 2018). Ideally, oncology nurses need to be aware of this concern and maintain a neutral stance in their interactions with survivors and family members, thereby giving them a chance to safely express their level of comprehension and comfort with health literacy without fear of judgment. By using this approach, oncology nurses can avoid assuming an individual’s level of health literacy.
An unexpected finding of this study was that more than half of the participants were confused by the research team’s efforts to assess the cultural sensitivity of Breathe Easier. Although the purpose of this study was to determine whether Breathe Easier met the cultural needs of African Americans, participants did not understand why race was important to the conversation when Breathe Easier was primarily focused on helping all lung cancer survivors and their family members. Race was perceived by some participants to be irrelevant to the assessment if the true desire of the research team was to improve symptom burden among everyone, particularly if race did not factor into the biologic benefits that participants would receive. Being a lung cancer survivor or a family member of a survivor was the most important cultural identifier despite some survivors and family members agreeing that certain inclusions (e.g., an African American contact person) would be important for other African Americans. Although this finding differs from previous research, which suggested that race/ethnicity is the strongest cultural identifier, it does validate the multifaceted nature of culture, suggesting that an individual’s priority of their main cultural identifier (race versus disease state) can be situation dependent (Kagawa-Singer et al., 2010). Kagawa-Singer (2012) suggested that limiting culture to discrete and narrow identifiers (e.g., race) instead of broad but well-defined systems limits researchers’ ability to identify facets of culture that are important to a given health disparity. To strengthen understanding of how culture affects cancer survivorship decisions, future research should rely on multiple integrated system theories that take into account the relationship among individuals, their culture, and their social and physical environment (Kagawa-Singer, 2012). In addition, future research can rely on individuals from the target population. Using community-based participatory processes, researchers can define what culture means to the target population and incorporate these priority areas when developing interventions and operationalized measures (Israel et al., 2010; Kagawa-Singer, 2012).
The relatively small sample in this study consisted of self-selected African American men and women from a southern U.S. state; therefore, findings cannot be generalized to individuals from other states and different racial/ethnic backgrounds. However, this study provides guidance on how nurses and other healthcare professionals can assess cultural sensitivity. The findings from the current study can also inform the development of culturally sensitive interventions.
Implications for Nursing
Greater attention is needed to implement culturally based integrated approaches that meet the survivorship needs of African American lung cancer survivors and their families. Oncology nurses and their interprofessional colleagues can more fully appreciate the impact of culture on the meaning and experience of cancer. Being aware of one’s own biases, attitudes, or behaviors that may elicit negative reactions when interacting with survivors who do not share the same cultural background is essential. Assessing structures in clinical settings that support or hinder culturally competent practice is a useful strategy. For example, oncology nurses could advocate for more comprehensive sociocultural histories to inform more open communication about the survivor’s perspective, cultural beliefs, and preferences. Cultural assessment models (e.g., ecologic model using seven levels of cultural assessment) exist to support restructuring elicited information (Kagawa-Singer et al., 2010). In research settings, involving African American lung cancer survivors and their families in the development and evaluation of interventions can help to determine which inclusions are relevant for enhancing clinical trial participation and desired outcomes. 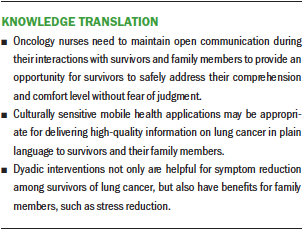
Conclusion
mHealth interventions are considered a viable option to enhance some aspects of cancer care management. However, healthcare providers may have difficulty locating effective, evidence-based, plain-language, and culturally sensitive mobile applications, particularly for lung cancer survivors and their family members (Owens et al., 2018). Because limited evaluation tools are available to assist healthcare providers in this process, mobile application developers should use existing tools to evaluate health literacy, eHealth literacy, and cultural sensitivity to inform mobile application designs. Many scales are available to assess these concepts, including the Short Assessment of Health Literacy–Spanish and English, Rapid Estimate of Adult Literacy in Medicine–Short Form, Test of Functional Health Literacy Scale, Newest Vital Sign, eHealth Literacy Scale, Cultural Sensitivity Checklist, and Cultural Sensitivity Assessment Tool (Arozullah et al., 2007; Friedman & Hoffman-Goetz, 2006; Guidry & Walker, 1999; Lee et al., 2010; Norman & Skinner, 2006; Osborn et al., 2007; Parker et al., 1995). Survivors and family members should also be involved throughout the design process to determine which features are most important to them and to what extent application developers should consider cultural sensitivity. Based on the findings of the current study, focusing too intently on cultural sensitivity factors can become distracting for some participants. Future research should make every effort to develop and test culturally sensitive interventions that target hard-to-reach and vulnerable populations of lung cancer survivors and their family members.
About the Author(s)
Otis L. Owens, MPH, PhD, is an assistant professor in the College of Social Work and core faculty in the Statewide Cancer Prevention and Control Program in the Arnold School of Public Health at the University of South Carolina in Columbia; Kasey N. Smith, MPH, is a research assistant and Jenay M. Beer, PhD, is an assistant professor, both in the Institute of Gerontology at the University of Georgia in Athens; and David G. Gallerani, MPH, is a research associate and Karen Kane McDonnell, PhD, RN, is an associate professor, both in the College of Nursing at the University of South Carolina in Columbia. During the writing of this article, Gallerani and McDonnell were supported by a grant from the Bristol Myers Squibb Foundation. Owens, Beer, Gallerani, and McDonnell contributed to the conceptualization and design. Owens, Gallerani, and McDonnell completed the data collection. Smith provided statistical support. Owens, Smith, and Beer provided the analysis. Owens, Smith, Beer, and McDonnell contributed to the manuscript preparation. Owens can be reached at owenso@mailbox.sc.edu, with copy to ONFEditor@ons.org. (Submitted May 2019. Accepted December 19, 2019.)
References
American Cancer Society. (2019a). Cancer facts and figures, 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
American Cancer Society. (2019b). Cancer treatment and survivorship facts and figures, 2019–2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
Anderson, M. (2015, April 30). Racial and ethnic differences in how people use mobile technology. Pew Research Center. https://www.pewresearch.org/fact-tank/2015/04/30/racial-and-ethnic-diff…
Arozullah, A.M., Yarnold, P.R., Bennett, C.L., Soltysik, R.C., Wolf, M.S., Ferreira, R.M., . . . Davis, T. (2007). Development and validation of a short-form, rapid estimate of adult literacy in medicine. Medical Care, 45(11), 1026–1033. https://doi.org/10.1097/mlr.0b013e3180616c1b
Barrera, M., Jr., Castro, F.G., Strycker, L.A., & Toobert, D.J. (2013). Cultural adaptations of behavioral health interventions: A progress report. Journal of Consulting and Clinical Psychology, 81(2), 196–205. https://doi.org/10.1037/a0027085
Bryant, A.S., & Cerfolio, R.J. (2008). Impact of race on outcomes of patients with non-small cell lung cancer. Journal of Thoracic Oncology, 3(7), 711–715. https://doi.org/10.1097/jto.0b013e31817c60c7
Chang, C.F., Feigenbaum, G.S., & Gould, M.K. (2016). Disparities in lung cancer outcomes. In L.B. Gerald & C.E. Berry (Eds.), Health disparities in respiratory medicine (pp. 237–264). Humana Press.
Choi, S.K., Seel, J.S., Yelton, B., Steck, S.E., McCormick, D.P., Payne, J., . . . Friedman, D.B. (2018). Prostate cancer information available in health-care provider offices: An analysis of content, readability, and cultural sensitivity. American Journal of Men’s Health, 12(4), 1160–1167. https://doi.org/10.1177/1557988318768599
Cillessen, L., Johannsen, M., Speckens, A.E.M., & Zachariae, R. (2019). Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: A systematic review and meta-analysis of randomized controlled trials. Psycho-Oncology, 28(12), 2257–2269. https://doi.org/10.1002/pon.5214
de Vibe, M., Bjørndal, A., Fattah, S., Dyrdal, G.M., Halland, E., & Tanner-Smith, E.E. (2017). Mindfulness-based stress reduction (MBSR) for improving health, quality of life and social functioning in adults: A systematic review and meta-analysis. Campbell Systematic Reviews, 13(1), 1–264. https://doi.org/10.4073/csr.2017.11
de Witte, M., Spruit, A., van Hooren, S., Moonen, X., & Stams, G.J. (2019). Effects of music interventions on stress-related outcomes: A systematic review and two meta-analyses. Health Psychology Review. Advance online publication. https://doi.org/10.1080/17437199.2019.1627897
Deng, G.E., Rausch, S.M., Jones, L.W., Gulati, A., Kumar, N.B., Greenlee, H., . . . Cassileth, B.R. (2013). Complementary therapies and integrative medicine in lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest, 143(5, Suppl.), e420S–e436S. https://doi.org/10.1378/chest.12-2364
Friedman, D.B., & Hoffman-Goetz, L. (2006). Assessment of cultural sensitivity of cancer information in ethnic print media. Journal of Health Communication, 11(4), 425–447. https://doi.org/10.1080/10810730600671920
Gonzalez, B.D. (2018). Promise of mobile health technology to reduce disparities in patients with cancer and survivors. JCO Clinical Cancer Informatics, 2, 1–9. https://doi.org/10.1200/CCI.17.00141
Guidry, J.J., & Walker, V.D. (1999). Assessing cultural sensitivity in printed cancer materials. Cancer Practice, 7(6), 291–296. https://doi.org/10.1046/j.1523-5394.1999.76005.x
Hallgren, K.A. (2012). Computing inter-rater reliability for observational data: An overview and tutorial. Tutorials in Quantitative Methods for Psychology, 8(1), 23–24. https://doi.org/10.20982/tqmp.08.1.p023
Holmes, J.A., & Chen, R.C. (2018). Racial disparities in time from diagnosis to treatment for stage I non–small cell lung cancer. JNCI Cancer Spectrum, 2(1), pky007. https://doi.org/10.1093/jncics/pky007
Hruschka, D.J., Schwartz, D., St. John, D.C., Picone-Decaro, E., Jenkins, R.A., & Carey, J.W. (2004). Reliability in coding open-ended data: Lessons learned from HIV behavioral research. Field Methods, 16(3), 307–331. https://doi.org/10.1177/1525822X04266540
Huang, Y., & Shen, F. (2016). Effects of cultural tailoring on persuasion in cancer communication: A meta-analysis. Journal of Communication, 66(4), 694–715. https://doi.org/10.1111/jcom.12243
Israel, B.A., Coombe, C.M., Cheezum, R.R., Schulz, A.J., McGranaghan, R.J., Lichtenstein, R., . . . Burris, A. (2010). Community-based participatory research: A capacity-building approach for policy advocacy aimed at eliminating health disparities. American Journal of Public Health, 100(11), 2094–2102. https://doi.org/10.2105/AJPH.2009.170506
James, D.C., Harville, C., Sears, C., Efunbumi, O., & Bondoc, I. (2017). Participation of African Americans in e-Health and m-Health studies: A systematic review. Telemedicine and e-Health, 23(5), 351–364. https://doi.org/10.1089/tmj.2016.0067
James, D.C.S., Harville, C., Whitehead, N., Stellefson, M., Dodani, S., & Sears, C. (2016). Willingness of African American women to participate in e-Health/m-Health research. Telemedicine and e-Health, 22(3), 191–197. https://doi.org/10.1089/tmj.2015.0071
Jemal, A., Ward, E.M., Johnson, C.J., Cronin, K.A., Ma, J., Ryerson, B., . . . Weir, H.K. (2017). Annual report to the nation on the status ofcancer, 1975–2014, featuring survival. Journal of the National Cancer Institute, 109(9), djx030. https://doi.org/10.1093/jnci/djx030
Jiang, J., Rickson, D., & Jiang, C. (2016). The mechanism of music for reducing psychological stress: Music preference as a mediator. Arts in Psychotherapy, 48, 62–68. https://doi.org/10.1016/j.aip.2016.02.002
Jiang, J., Zhou, L., Rickson, D., & Jiang, C. (2013). The effects of sedative and stimulative music on stress reduction depend on music preference. Arts in Psychotherapy, 40(2), 201–205. https://doi.org/10.1016/j.aip.2013.02.002
Jonnalagadda, S., Lin, J.J., Nelson, J.E., Powell, C.A., Salazar-Schicchi, J., Berman, A.R., . . . Wisnicesky, J.P. (2012). Racial and ethnic differences in beliefs about lung cancer care. Chest, 142(5), 1251–1258. https://doi.org/10.1378/chest.12-0330
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4(1), 33–47. https://doi.org/10.1016/0163-8343(82)90026-3
Kabat-Zinn, J., Lipworth, L., & Burney, R. (1985). The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine, 8(2), 163–190. https://doi.org/10.1007/bf00845519
Kagawa-Singer, M. (2012). Applying the concept of culture to reduce health disparities through health behavior research. Preventive Medicine, 55(5), 356–361. https://doi.org/10.1016/j.ypmed.2012.02.011
Kagawa-Singer, M., Valdez Dadia, A., Yu, M.C., & Surbone, A. (2010). Cancer, culture, and health disparities: Time to chart a new course? CA: A Cancer Journal for Clinicians, 60(1), 12–39. https://doi.org/10.3322/caac.20051
Lee, S.Y.D., Stucky, B.D., Lee, J.Y., Rozier, R.G., & Bender, D.E. (2010). Short Assessment of Health Literacy—Spanish and English: A comparable test of health literacy for Spanish and English speakers. Health Services Research, 45(4), 1105–1120. https://doi.org/10.1111/j.1475-6773.2010.01119.x
Lehto, R.H., Wyatt, G., Sikorskii, A., Tesnjak, I., & Kaufman, V.H. (2015). Home-based mindfulness therapy for lung cancer symptom management: A randomized feasibility trial. Psycho-Oncology, 24(9), 1208–1212. https://doi.org/10.1002/pon.3755
Li, C.C., Matthews, A.K., Dossaji, M., & Fullam, F. (2017). The relationship of patient–provider communication on quality of life among African-American and white cancer survivors. Journal of Health Communication, 22(7), 584–592. https://doi.org/10.1080/10810730.2017.1324540
Li, S.Y.H., & Bressington, D. (2019). The effects of mindfulness-based stress reduction on depression, anxiety, and stress in older adults: A systematic review and meta-analysis. International Journal of Mental Health Nursing, 28(3), 635–656. https://doi.org/10.1111/inm.12568
Lin, J.J., Mhango, G., Wall, M.M., Lurslurchachai, L., Bond, K.T., Nelson, J.E., . . . Wisnivesky, J.P. (2014). Cultural factors associated with racial disparities in lung cancer care. Annals of the American Thoracic Society, 11(4), 489–495. https://doi.org/10.1513/AnnalsATS.201402-055OC
Loh, K.P., Ramsdale, E., Culakova, E., Mendler, J.H., Liesveld, J.L., O’Dwyer, K.M., . . . Mohile, S.G. (2018). Novel mHealth app to deliver geriatric assessment-driven interventions for older adults with cancer: Pilot feasibility and usability study. JMIR Cancer, 4(2), e10296. https://doi.org/10.2196/10296
Marcolino, M.S., Oliveira, J.A.Q., D’Agostino, M., Ribeiro, A.L., Alkmim, M.B.M., & Novillo-Ortiz, D. (2018). The impact of mHealth interventions: Systematic review of systematic reviews. JMIR mHealth and uHealth, 6(1), e23. https://doi.org/10.2196/mhealth.8873
McDonnell, K.K., Gallerani, D.G., Owens, O.L., Beer, J.M., Khan, S., Hardin, J.W., . . . Bennett, A.M. (2019) A dyad-based mindfulness recovery program to reduce lung cancer symptoms: Mixed methods. Manuscript submitted for publication.
McDonnell, K.K., Owens, O.L., Messias, D.K.H., Heiney, S.P., Friedman, D.B., Campbell, C., & Webb, L.A. (2019). Health behavior changes in African American family members facing lung cancer: Tensions and compromises. European Journal of Oncology Nursing, 38, 57–64. https://doi.org/10.1016/j.ejon.2018.12.002
National Cancer Institute Surveillance, Epidemiology, and End Results Program. (n.d.) Cancer stat facts: Lung and bronchus cancer. https://seer.cancer.gov/statfacts/html/lungb.html
Nielsen-Bohlman, L., Panzer, A.M., & Kindig, D.A. (Eds.) (2004). Health literacy: A prescription to end confusion. National Academies Press.
Norman, C.D., & Skinner, H.A. (2006). eHEALS: The eHealth Literacy Scale. Journal of Medical Internet Research, 8(4), e27. https://doi.org/10.2196/jmir.8.4.e27
Oliveira, B.S., Zunzunegui, M.V., Quinlan, J., Fahmi, H., Tu, M.T., & Guerra, R.O. (2016). Systematic review of the association between chronic social stress and telomere length: A life course perspective. Ageing Research Reviews, 26, 37–52. https://doi.org/10.1016/j.arr.2015.12.006
Osborn, C.Y., Weiss, B.D., Davis, T.C., Skripkauskas, S., Rodrigue, C., Bass, P.F., & Wolf, M.S. (2007). Measuring adult literacy in health care: Performance of the Newest Vital Sign. American Journal of Health Behavior, 31(1), S36–S46. https://doi.org/10.5993/ajhb.31.s1.6
Owens, O.L., Beer, J.M., Reyes, L.I., Gallerani, D.G., Myhren-Bennett, A.R., & McDonnell, K.K. (2018). Mindfulness-based symptom and stress management apps for adults with chronic lung disease: Systematic search in app stores. JMIR mHealth and uHealth, 6(5), e124. https://doi.org/10.2196/mhealth.9831
Parker, R.M., Baker, D.W., Williams, M.V., & Nurss, J.R. (1995). The test of functional health literacy in adults. Journal of General Internal Medicine, 10(10), 537–541. https://doi.org/10.1007/bf02640361
Poghosyan, H., Sheldon, L.K., Leveille, S.G., & Cooley, M.E. (2013). Health-related quality of life after surgical treatment in patients with non-small cell lung cancer: A systematic review. Lung Cancer, 81(1), 11–26. https://doi.org/10.1016/j.lungcan.2013.03.013
Rush, S.E., & Sharma, M. (2017). Mindfulness-based stress reduction as a stress management intervention for cancer care: A systematic review. Journal of Evidence-Based Complementary and Alternative Medicine, 22(2), 348–360. https://doi.org/10.1177/2156587216661467
Santorelli, S.F. (Ed.). (2014). Mindfulness-based stress reduction (MBSR): Standards of practice. Center for Mindfulness in Medicine, Health Care, and Society, University of Massachusetts Medical School.
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., . . . Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality and Quantity, 52(4), 1893–1907. https://doi.org/10.1007/s11135-017-0574-8
Schellekens, M.P.J., van den Hurk, D.G.M., Prins, J.B., Donders, A.R.T., Molema, J., Dekhuijzen, R., . . . Speckens, A.E.M. (2017). Mindfulness-based stress reduction added to care as usual for lung cancer patients and/or their partners: A multicentre randomized controlled trial. Psycho-Oncology, 26(12), 2118–2126. https://doi.org/10.1002/pon.4430
Siegel, R.L., Miller, K.D., & Jemal, A. (2019). Cancer statistics, 2019. CA: A Cancer Journal for Clinicians, 69(1), 7–34. https://doi.org/10.3322/caac.21551
Smith, A. (2014a, January 6). African Americans and technology use: A demographic portrait. Pew Research Center. https://www.pewinternet.org/2014/01/06/african-americans-and-technology…
Smith, A. (2014b, April 3). Older adults and technology use. Pew Research Center. https://www.pewinternet.org/2014/04/03/older-adults-and-technology-use
Strauss, A.L., & Corbin, J.M. (Eds.). (1997). Grounded theory in practice. Sage.
Tan, J.Y., Molassiotis, A., Lloyd-Williams, M., & Yorke, J. (2018). Burden, emotional distress and quality of life among informal caregivers of lung cancer patients: An exploratory study. European Journal of Cancer Care, 27(1), e12691. https://doi.org/10.1111/ecc.12691
van den Hurk, D.G.M., Schellekens, M.P.J., Molema, J., Speckens, A.E.M., & van der Drift, M.A. (2015). Mindfulness-based stress reduction for lung cancer patients and their partners: Results of a mixed methods pilot study. Palliative Medicine, 29(7), 652–660. https://doi.org/10.1177/0269216315572720
Vijayvergia, N., Shah, P.C., & Denlinger, C.S. (2015). Survivorship in non–small cell lung cancer: Challenges faced and steps forward. Journal of the National Comprehensive Cancer Network, 13(9), 1151–1161. https://doi.org/10.6004/jnccn.2015.0140
Warren-Findlow, J., Seymour, R.B., & Shenk, D. (2010). Intergenerational transmission of chronic illness self-care: Results from the caring for hypertension in African American families study. Gerontologist, 51(1), 64–75. https://doi.org/10.1093/geront/gnq077
Webb, L.A., & McDonnell, K.K. (2018). Not a death sentence: Perspectives of African American women living with lung cancer. Oncology Nursing Forum, 45(1), 46–54. https://doi.org/10.1188/18.ONF.46-54
Woods-Giscombé, C.L., & Gaylord, S.A. (2014). The cultural relevance of mindfulness meditation as a health intervention for African Americans: Implications for reducing stress-related health disparities. Journal of Holistic Nursing, 32(3), 147–160. https://doi.org/10.1177/0898010113519010




