The Effectiveness of Yoga on Cancer-Related Fatigue: A Systematic Review and Meta-Analysis
Problem Identification: The aim of this article is to evaluate the effectiveness of yoga on cancer-related fatigue (CRF) in patients undergoing chemotherapy and/or radiation therapy.
Literature Search: Relevant English and Chinese articles were retrieved from medical databases and included in this analysis. Standardized critical appraisal instruments from the Joanna Briggs Institute were adopted for the quality assessment.
Data Evaluation: 16 randomized controlled trials met the inclusion criteria.
Synthesis: Yoga interventions had a positive effect in reducing CRF among patients undergoing chemotherapy and/or radiation therapy, but the adherence to yoga was low. Mixed types of yoga, in addition to supervised and self-practicing strategies, were associated with increased patient adherence and improved CRF.
Implications for Practice: Yoga appears to be a safe and effective exercise for the management of CRF during chemotherapy and/or radiation therapy; however, additional high-quality studies are needed to define an optimal yoga intervention strategy.
Jump to a section
Cancer is the second leading cause of death in the world, with an estimated 9.6 million deaths occurring in 2018 (World Health Organization, 2018). According to a cancer progress report released by the American Association for Cancer Research (2018), the number of new cancer cases worldwide could increase to 24 million annually by 2035. With advancements in cancer prevention, diagnosis, and treatment, survival rates are continually increasing; however, the physical and psychological disorders associated with the occurrence, progression, and treatment of cancer, including nausea, poor appetite, fatigue, decreased immunity, anxiety, and depression, significantly affect the quality of life of cancer survivors.
Cancer-related fatigue (CRF) is one of the most common symptoms associated with cancer and is defined as “a distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to recent activity and interferes with the usual function” (National Comprehensive Cancer Network, 2018, p. MS-3). Research has shown that 60% to 99% of patients undergoing chemotherapy and/or radiation therapy have reported CRF (Wu et al., 2017). Exercise has been examined as one way to reduce CRF. The American College of Sports Medicine has recommended that an overall volume of weekly activity consisting of moderate-intensity exercise for 150 minutes, vigorous-intensity exercise for 75 minutes, or an equivalent combination is appropriate for cancer survivors (Schmitz et al., 2010). However, for patients undergoing chemotherapy and/or radiation therapy, several reviews have reported that shorter exercise sessions or lower targeted exercise volume were associated with greater improvements in CRF (Carayol et al., 2015; Kessels et al., 2018; Tian et al., 2016).
Yoga has been identified as one such low-intensity exercise. Yoga has its roots in ancient Indian philosophy and, differing from general aerobic exercise, yoga requires that the practitioner focuses on the integration, unity, and harmony of inner awareness, breathing, and body (Carayol et al., 2013; Cramer et al., 2017). There are various styles of yoga related to different yoga schools. Therapeutic yoga for patients with cancer commonly involves one or more physical postures, breathing techniques, and meditation. Research has demonstrated that yoga can modulate hypothalamic-pituitary-adrenal dysregulation and improve mental and physical health (Streeter et al., 2012). However, to date, insufficient evidence exists to substantiate the effectiveness of yoga on CRF in patients undergoing chemotherapy and/or radiation therapy.
A Cochrane review by Cramer et al. (2017) of 24 randomized controlled trials (RCTs), with a total of 2,166 women undergoing active treatment for breast cancer, found that yoga reduced CRF when compared to no therapy or psychoeducation only. However, the review only included patients with breast cancer and subgroup analysis could not be performed. In contrast, a meta-analysis by Pan et al. (2015) of nine RCTs revealed no significant relief of fatigue from yoga; however, data concerning CRF during treatment were not extracted independently.
The effectiveness of a yoga intervention as well as the amount of yoga to be performed by patients with CRF remains in question. Several reviews have attempted to examine this topic, but most have not been able to perform a meta-analysis, mostly related to small sample sizes and limited database searching (Danhauer, Addington, et al., 2015; Danhauer et al., 2019; Felbel et al., 2014; Harder et al., 2012; Pan et al., 2015; Sadja & Mills, 2013; Smith & Pukall, 2009; Tolia et al., 2018; Zuo et al., 2016); several have focused only on one cancer, particularly breast cancer (Felbel et al., 2014; Harder et al., 2012; Pan et al., 2015; Zuo et al., 2016); and some have not extracted and analyzed information about CRF in patients during chemotherapy and/or radiation therapy (Buffart et al., 2012; Carayol et al., 2015; Pan et al., 2015; Tomlinson et al., 2014). Therefore, additional large-scale data examinations are needed to determine the effectiveness of yoga on CRF in patients undergoing chemotherapy and/or radiation therapy.
Several clinical trials have been conducted to investigate the effectiveness of yoga on CRF among cohorts of patients treated for different cancers (Ben-Josef et al., 2017; Cramer et al., 2016; LÖtzke et al., 2016). The aim of the current review was to assess the effectiveness and appropriate amount of yoga as an intervention for adults experiencing CRF while undergoing chemotherapy and/or radiation therapy, compared with no therapy or psychoeducation. In addition, the optimal yoga intervention strategy and style for reducing CRF, as well as patient adherence and factors affecting patient adherence, were investigated. The safety and adverse events of a yoga intervention during chemotherapy and/or radiation therapy were also examined.
Methods
The systematic review was performed according to an established protocol (PROSPERO No. CRD42020156435) and presented using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (Moher et al., 2015).
Inclusion and Exclusion Criteria
The following criteria were required for study inclusion:
• Participants had to be older than age 18 years and undergoing chemotherapy and/or radiation therapy (regardless of type of drug or dose) for cancer (regardless of cancer type or stage).
• Study interventions must include yoga, regardless of the style, intensity, and duration, and be focused on yoga, including one or more sessions of posture yoga, meditation, and pranayama.
• The study must contain a routine care comparison group (e.g., standard nursing and/or psychoeducation).
• The primary outcome was CRF, measured through a standardized, validated, and reliable psychometric instrument, and the endpoint was during or just after the conclusion of the yoga intervention. Secondary outcomes included adherence and adverse events.
• Experimental and quasiexperimental study designs, including RCTs and non-RCTs, were included.
Studies were excluded if less than 50% of the total participant population were those who received chemotherapy and/or radiation therapy and the data for which were not extracted independently; the yoga intervention was combined with other therapy, such as massage, acupuncture, drug, and nutrition; and the study had a single-arm design with no comparison group.
Search Strategy
Eight English and Chinese databases, including PubMed®, Cochrane Library, OVID, EBSCOhost, ProQuest, CNKI, SINOMED, and Wanfang, were searched for relevant studies from inception to July 2019. An initial limited search on PubMed and Cochrane Library was undertaken to identify articles on the topic. Medical Subject Heading (MeSH) words and text phrases were used to develop a full search strategy for the PubMed database. The search strategy, including MeSH words, text phrases, title, abstract, keywords, and index terms, were adapted for each included information source. The languages were limited to English and Chinese. The reference lists of all studies selected for critical appraisal were screened for additional relevant studies.
Study Selection
Following the search, all identified citations were collected and uploaded into EndNote®, version 19.2, and duplicates were removed. Titles, abstracts, and the full text were assessed by two independent reviewers against the inclusion criteria. Any disagreements that arose between the reviewers at each stage of the study selection process were resolved through discussion or with a third reviewer.
Assessment of Methodologic Quality
Eligible studies were critically appraised for methodologic quality by two independent reviewers at the study level using the standardized critical appraisal instruments from the Joanna Briggs Institute for experimental and quasiexperimental studies. The risks of bias were assessed on the following domains: random sequence generation, allocation concealment, blinding of participants, intervention and outcomes assessors, intention-to-treat (ITT) analysis, selective reporting, and attrition bias. Any disagreements were resolved through discussion or with a third reviewer.
Data Extraction
Data were extracted by two independent reviewers using a standardized data extraction tool. The data extracted included specific details about the study characteristics (author, year, and country where the study was conducted), participant characteristics (age, gender, and type of cancer), study methods, treatment, intervention characteristics (the style of yoga and intensity [minutes per session, sessions per day, days per week, and total weeks]), and outcome characteristics (sample size, mean scores and effect size of CRF, the assessment tool, numbers of adherence, and adverse events). Authors of respective articles were contacted to request missing or additional data or for clarification where required.
Statistical Analyses
Data from studies were pooled for statistical meta-analysis using RevMan, version 5.3. The main outcome index was CRF, which was a continuous variable. However, there were various measuring instruments. Effect sizes of CRF were expressed as weighted mean difference for the same measuring instruments, while standardized mean difference (SMD) was used to express effect sizes for different measuring instruments. The 95% confidence interval (CI) was calculated for analysis and modified as appropriate. Relevant adverse events (sprain, fall, dizziness) and adherence (defined as patient participation in 70% or more of intervention) were binary outcomes, which were summarized using odds ratio (OR).
Heterogeneity was assessed statistically using the standard chi-square and I2 tests. Subgroup analyses were performed regardless of the presence or absence of statistically significant heterogeneity for the following: (a) types of cancer; (b) types of yoga, categorized into no postures (pure meditation and/or breathing without physical exercises), postures (physical exercises without meditation or breathing), and mixed types (physical exercises with one or more of meditation and breathing); (c) intervention duration, categorized into less than eight weeks and eight weeks or greater; (d) frequency and intensity of intervention, including less than 150 minutes per week or 150 minutes or greater per week; (e) cancer type, including breast, colorectal, and lung; and (f) intervention strategies, categorized into supervised intervention, self-practicing, or mixed. Statistical analyses were performed using the random-effects model due to factors that could affect the outcomes (e.g., different assessment instruments, yoga styles, and intervention strategies in studies) (Tufanaru et al., 2015). Sensitivity analyses were conducted to exclude studies with high heterogeneity of research methodology in subgroups, such as yoga style and variability in the ratio of random distribution. Publication bias was visually inspected using funnel plots and formally assessed using statistical tests. For all statistical analyses, p < 0.05 indicated statistical significance.
Results
Study Selection
Seven hundred records were identified from searches of nine databases, and nine additional studies were identified from other review articles. After duplicates were removed, the titles and abstracts of 588 articles were screened against eligibility criteria and 526 were excluded, leaving 62 full-text articles. Of the 62 articles, 46 were excluded for the following reasons: post-treatment or less than 50% of the total participants received chemotherapy and/or radiation therapy (n = 13); no CRF assessment (n = 9); full text not available (n = 7); single-arm design (n = 6); articles not in English or Chinese (n = 5); related to the same process and outcome (n = 3); and no routine care comparison (n = 3). Sixteen RCTs comprised of 20 intervention groups were included in the final study (see Figure 1). No quasiexperimental studies met the inclusion criteria. 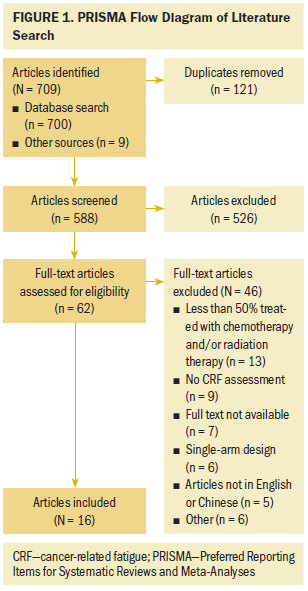
Characteristics of Included Studies
The included 16 studies comprised a total of 1,453 patients, of whom 105 were men and 1,348 were women. The sample size of each study ranged from 15 to 164 patients. Nine studies were conducted in the United States, three in mainland China, two in India, one in the Netherlands, and one in Taiwan. The types of cancer in the studies were breast cancer (n = 13), prostate cancer (n = 1), lymphoma (n = 1), and colorectal cancer (n = 1). Patients were receiving chemotherapy only (n = 9), radiation therapy only (n = 5), and chemotherapy and/or radiation therapy (n = 2). Interventions were conducted and compared with routine care in three studies, and one study measured CRF at two endpoints (during and after the intervention). Standard nursing was the comparator in 14 studies; in two other studies, psychoeducation was the comparator (see Table 1). 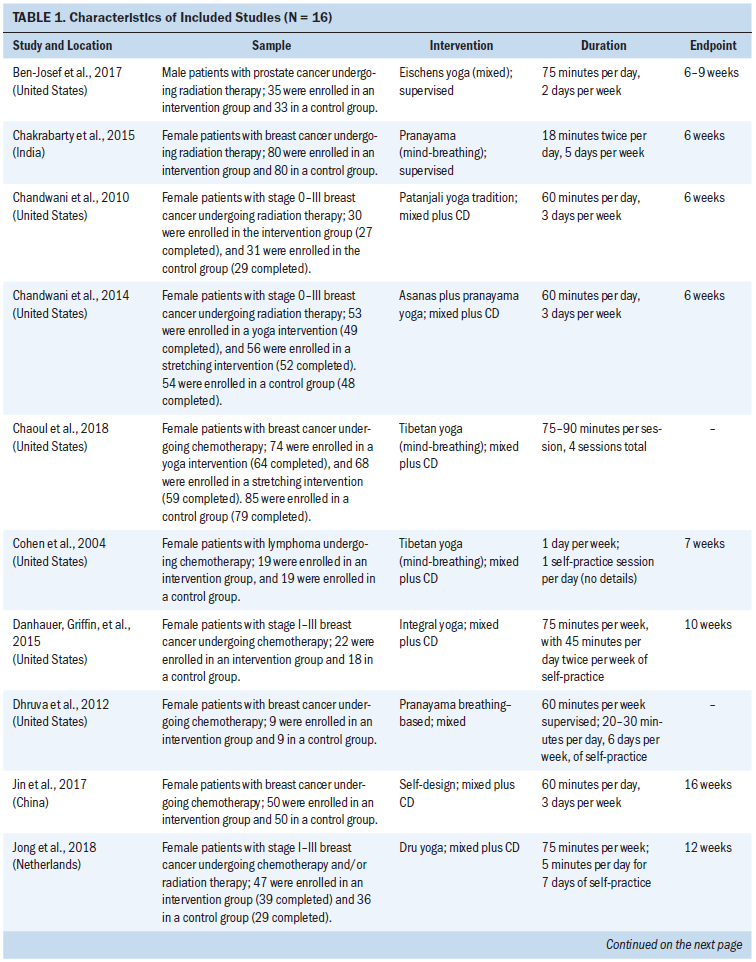
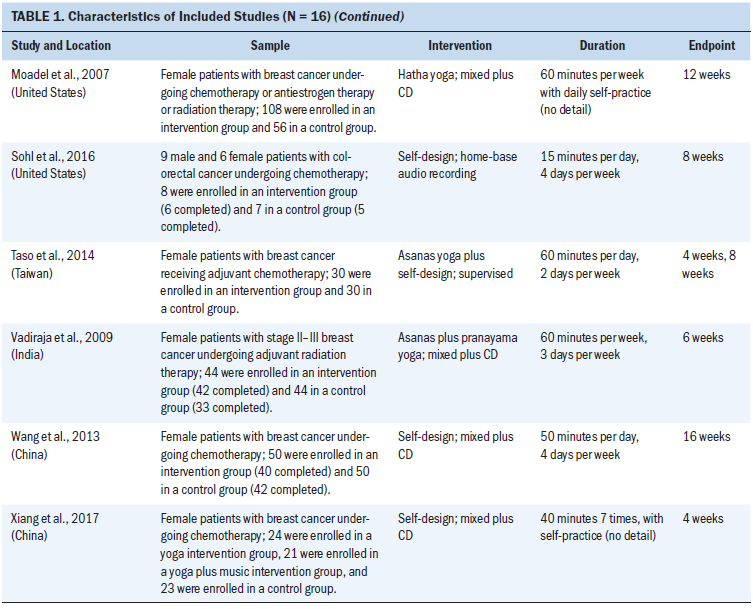
Regarding types of yoga as an intervention in the studies, 13 were mixed yoga, 2 were no posture (mind-breathing), and 2 were only posture (stretching practice). The styles of yoga were variable as well. The duration of the yoga interventions ranged from 4 to 16 weeks, the frequency of yoga interventions ranged from one to seven days per week, and the total duration of sessions ranged from 60 to 200 minutes per week. In most studies (n = 12), yoga was instituted as a combined supervised and self-practicing intervention; three studies conducted yoga intervention by supervision, and one study adopted a home-based strategy. The assessment tools for CRF included the Brief Fatigue Inventory (BFI) (n = 6), the Cancer Fatigue Scale (CFS) (n = 4), the Functional Assessment of Cancer Therapy–Fatigue subscale (n = 2), the Functional Assessment of Chronic Illness Therapy–Fatigue subscale (n = 1), the revised Piper Fatigue Scale (n = 1), the Multidimensional Fatigue Inventory (n = 1), and the European Organisation for the Research and Treatment of Cancer Quality-of-Life Questionnaire–Core 30 (n = 1).
Quality Assessment and Risk of Bias
Randomization was used for the assignment of participants to different groups in all studies, but detailed information regarding random sequence generation was not described in three studies. Only one study performed cluster randomization, using one cluster for yoga and one for comparison. Apart from one study that performed a random assignment in a 2:1 ratio, all others were performed in a 1:1 ratio. Concealed allocation was reported in seven studies, of which two did not provide detailed information. All studies compared baseline data between the yoga and control groups. Of all included studies, only one reported no blinding to outcomes assessors. Two studies did not report reasons for patient attrition, and four did not describe details about the patients’ adherence to the intervention. In two studies, patient attrition and reasons for attrition were significantly different between the groups. ITT analysis was performed in nine studies. None of the studies provided the registered protocol, so the risk of selective reporting was unclear. Only one study described the training of outcome assessors, whereas no studies provided the number of raters and intra-rater reliability. Pseudorandomization was performed in one study, whereas another study had assessed CRF using a measurement scale of unclear validity. These factors might have affected the quality of trial design and resulted in biases. 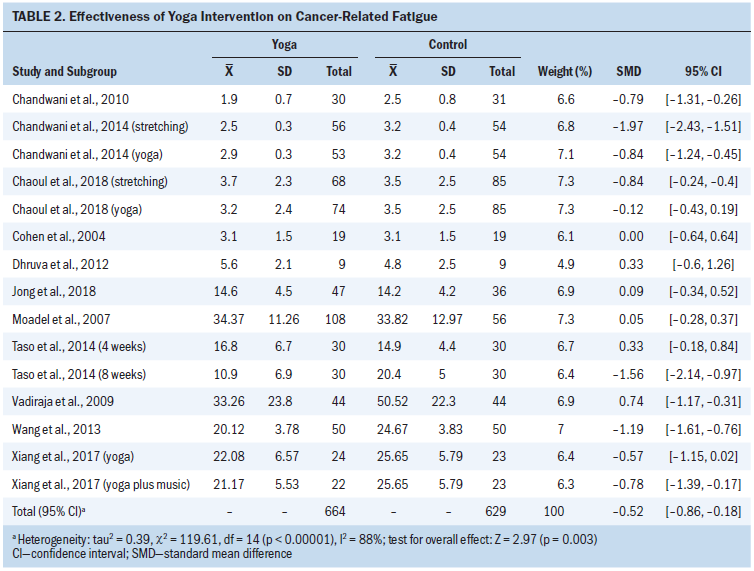
Pooled Effectiveness of a Yoga Intervention on CRF
All 16 studies reported outcomes on CRF. However, two studies presented the data by median and quartile, one study used only graphical representation, one study did not calculate the total scores of CRF, and one study compared the difference in the value of CRF between the two groups before and after the intervention. Therefore, 11 studies involving 15 results were pooled into the meta-analysis. When comparing the total effect on CRF of yoga intervention with routine care, the pooled SMD was –0.52 (95% CI [–0.86, –0.18]), indicating that yoga was favorable and statistically significant in reducing CRF during chemotherapy/radiation thearpy with a large heterogeneity (I2 = 88%, p < 0.00001). The funnel plot appeared symmetrical, suggesting a low risk of publication bias (see Table 2). 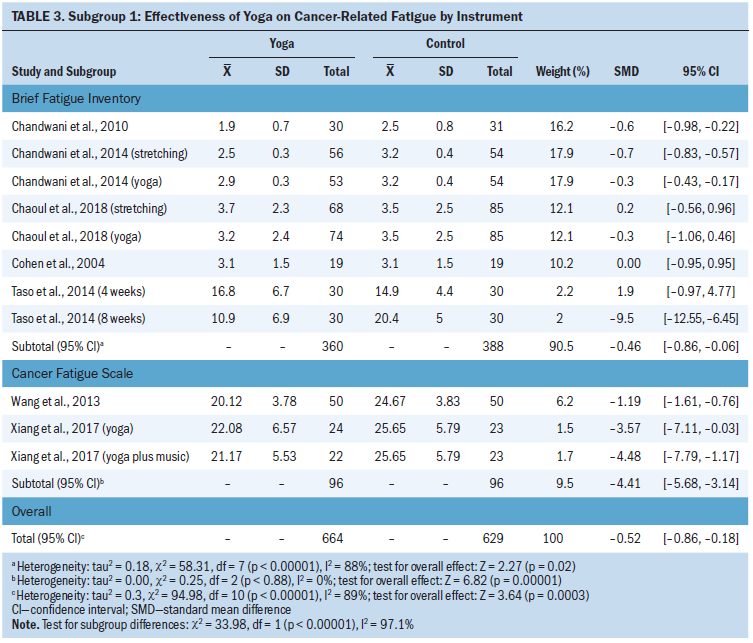
Subgroup 1: Effectiveness on CRF with different assessment instruments: Of the 11 studies included for meta-analysis, 6 (n = 748 patients) assessed CRF using the BFI, which showed the pooled effect of –0.46 (95% CI [–0.86, –0.06]) and high heterogeneity (I2 = 88%, p < 0.00001). Two studies (n = 192 patients) measured CRF using the CFS, which demonstrated the pooled effect of –4.41 (95% CI [–5.68, 3.14]) and low heterogeneity (I2 = 0%, p = 0.88) (see Table 3). The other four studies measured CRF using a different instrument; therefore, the measured data from these studies were not merged in the analysis. The difference between subgroups was statistically significant (I2 = 97.1%, p < 0.00001), indicating that the assessment instrument was an important factor contributing to heterogeneity. A sensitivity analysis was performed for the BFI subgroup, which showed that the heterogeneity was reduced (I2 = 19%, p = 0.29) following the omission of three interventions, and the outcome appeared stable (SMD = –0.34, 95% CI [–0.56, –0.13]) (see Table 4). 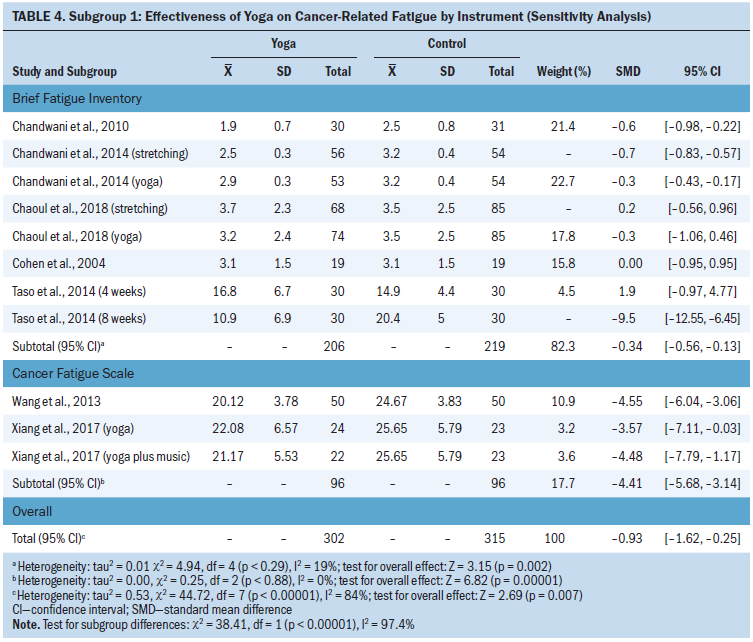
Subgroup 2: Effectiveness on CRF by yoga type: Of the included studies, 11 interventions (n = 853 patients) used mixed yoga types; the pooled effect on CRF was –0.54 (95% CI [–0.89, –0.19]) with substantial heterogeneity (I2 = 83%, p < 0.00001). Two interventions implemented posture-based or no posture (mind-breathing) yoga, and the pooled effects were –0.94 (95% CI [–2.95, 1.08], I2 = 98%, p < 0.00001) and –0.08 (95% CI [–0.37, 0.22], I2 = 0%, p = 0.37), respectively (see Table 5). 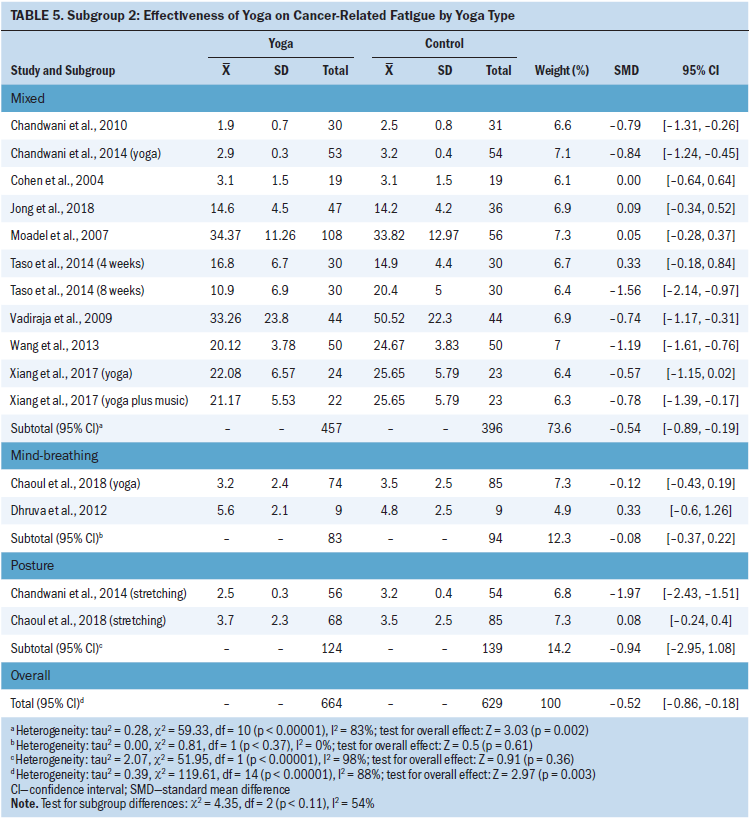
Subgroup 3: Effectiveness on CRF by intervention strategies: Ten studies (n = 1,173 patients) had implemented yoga with combined supervision and self-practicing strategy. The pooled effect on CRF was –0.51 (95% CI [–0.86, –0.16]) with substantial heterogeneity (I2 = 88%, p < 0.00001) (see Table 6). Only one study instituted yoga intervention by supervised strategy. 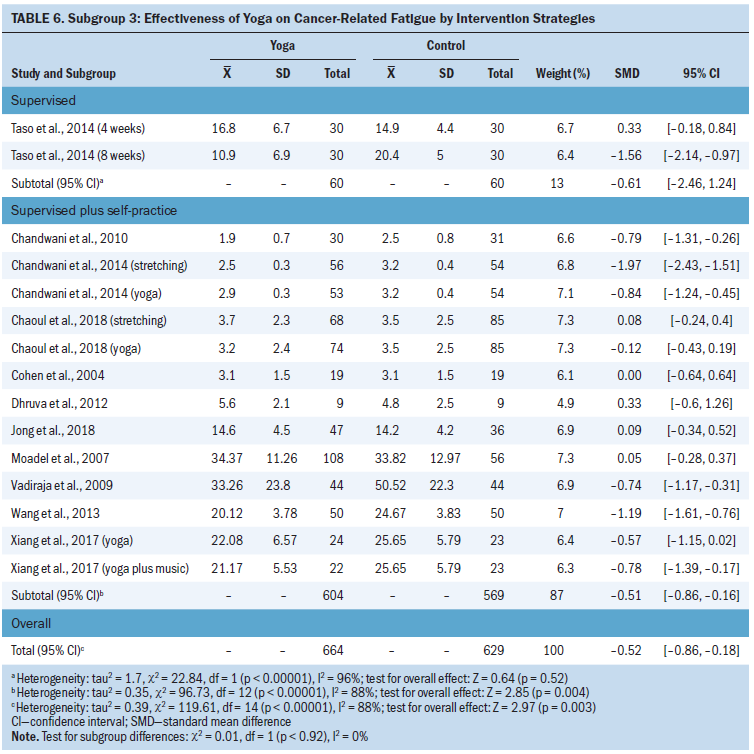
Subgroup 4: Effectiveness on CRF with a variable weekly duration of yoga intervention: The weekly total durations of yoga interventions were less than 150 minutes per week in six studies (n = 802 patients) and 150 minutes or greater per week in four studies (n = 423 patients). The pooled effect showed that yoga intervention of 150 minutes or greater per week significantly reduced CRF (–0.96, 95% CI [–1.52, –0.4], I2 = 85%, p < 0.0001) compared to routine care. When the yoga intervention was less than 150 minutes per week, CRF was only reduced slightly and not significantly different compared to routine care (–0.32, 95% CI [–0.65, 0.01], I2 = 81%, p < 0.00001) (see Table 7). 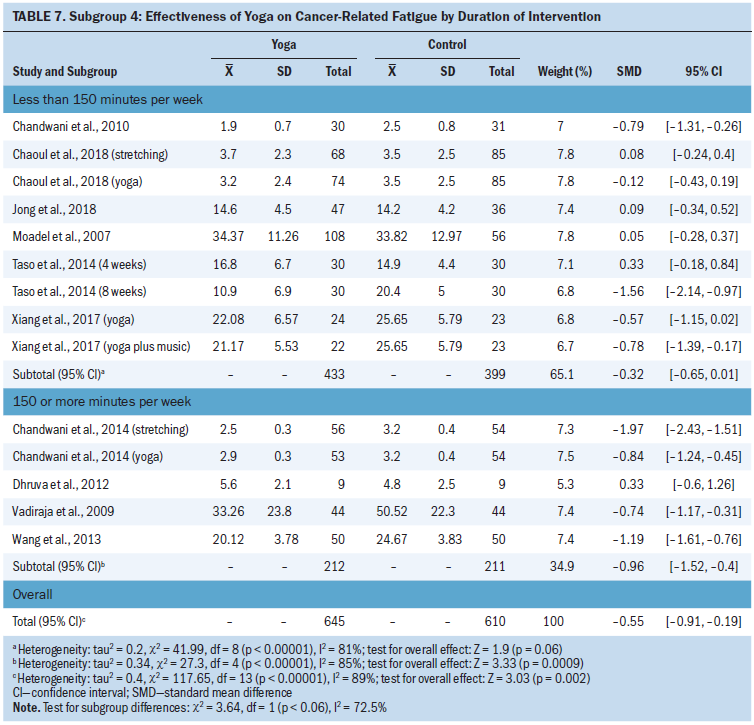
Subgroup 5: Effectiveness on CRF with different intervention durations: The duration of intervention in seven studies (n = 868 patients) was less than eight weeks, and five studies (n = 425 patients) had an intervention of eight weeks or greater. The pooled effect showed that yoga intervention of less than eight weeks reduced the CRF during chemotherapy, and the difference between the groups was statistically significant (–0.54, 95% CI [–0.95, –0.12], I2 = 88%, p < 0.00001). However, when comparing yoga intervention and routine care in relieving CRF for the duration of eight weeks or greater, there was no statistically significant difference in the pooled effect (–0.47, 95% CI [–1.18, 0.23], I2 = 91%, p < 0.00001) (see Table 8). 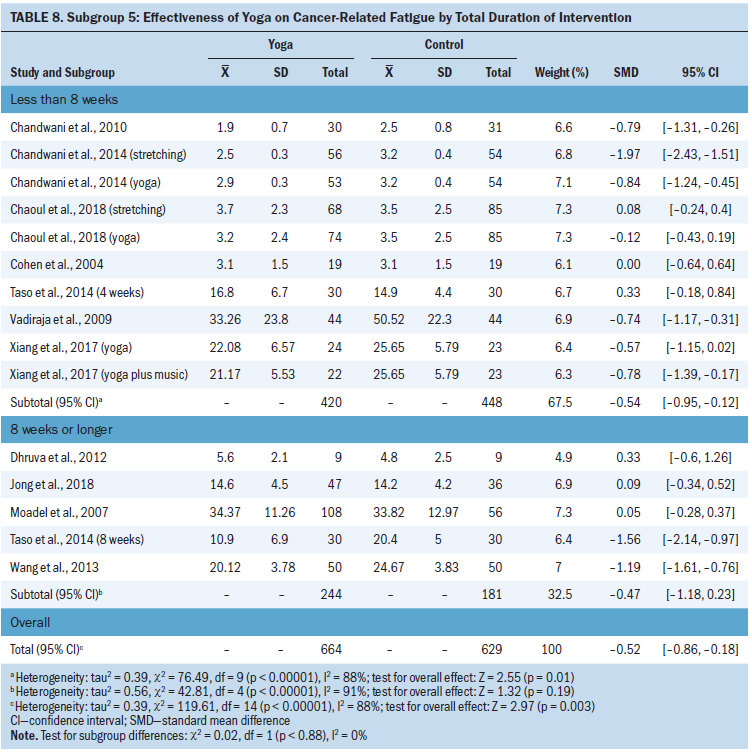
Subgroup 6: Effectiveness on CRF by cancer type: Ten studies examined the effectiveness of yoga on CRF in patients with breast cancer, which showed the pooled effect of –0.46 (95% CI [–0.58, –0.35]) with high heterogeneity (I2 = 89%, p < 0.00001) (see Table 9). 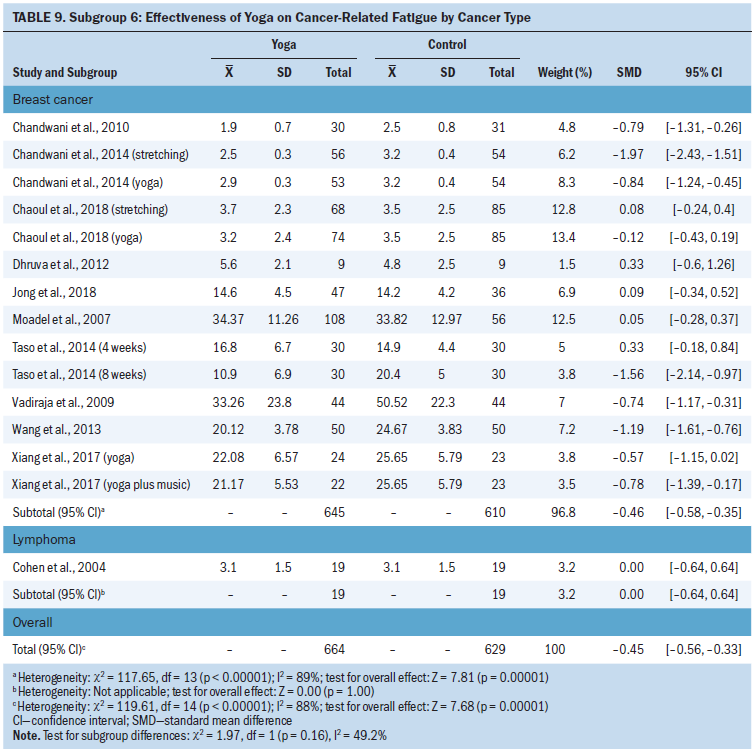
Pooled Effects of Adherence to Yoga Intervention
Fourteen studies reported the adherence rate to intervention, which ranged from 7% to 100%. One study reported 100% adherence; however, this was not estimated in the pooled result. The adherence rates of 13 studies were pooled into the meta-analysis (see Table 10), which showed a pooled OR of 0.55 (95% CI [0.4, 0.74]) with medium heterogeneity (I2 = 66%, p = 0.0002). The funnel plot appeared asymmetrical, indicating a potential risk of publication bias. Sensitivity analysis showed that there was significant heterogeneity in two studies; when removed, the pooled OR of adherence between the groups was 0.65 (95% CI [0.46, 0.94]) with low heterogeneity (I2 = 8%, p = 0.37) (see Table 11). Additional subgroup analyses were performed. 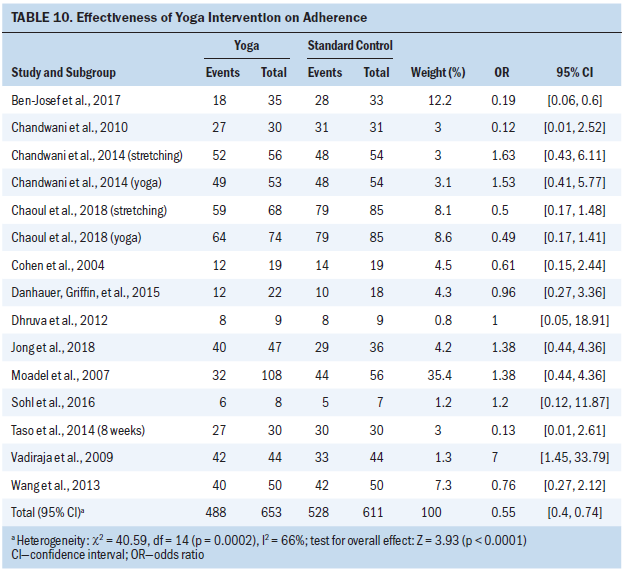
Subgroup 1: Impact on adherence with a different intervention strategy: Two studies involving 128 patients who had performed a yoga intervention via supervised-based strategy were examined. The pooled OR of adherence was 0.18 (95% CI [0.06, 0.52]) with low heterogeneity (I2 = 0%, p = 0.81), indicating that yoga interventions with supervision contributed to a statistically significant difference in the odds of adherence between the groups of patients undergoing chemotherapy and/or radiation therapy. Ten interventions involving 884 patients who had performed yoga by supervised-based strategy in addition to self-practicing strategy were examined. The pooled OR of adherence was 0.8 (95% CI [0.54, 1.19]) with low heterogeneity (I2 = 0%, p = 0.79) (see Table 12). 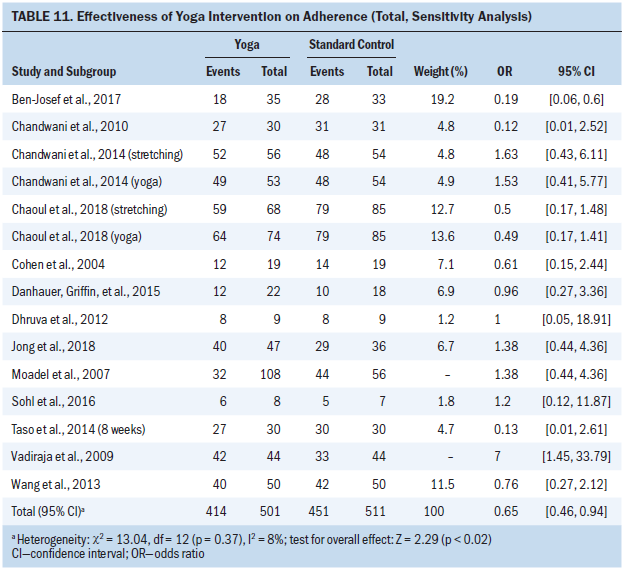
Subgroup 2: Impact on adherence with different weekly duration of yoga intervention: Five interventions involving 375 patients who had performed yoga interventions 150 minutes or greater per week were examined, as were seven interventions involving 599 patients who had performed less than 150 minutes per week. One study did not report a detailed weekly duration of intervention. The pooled OR of adherence on intervention of 150 minutes or greater per week and less than 150 minutes per week was 1.09 (95% CI [0.6, 1.96] with low heterogeneity (I2 = 0%, p = 0.89) and 0.46 (95% CI [0.28, 0.76] with low heterogeneity (I2 = 24%, p = 0.25), respectively (see Table 13). 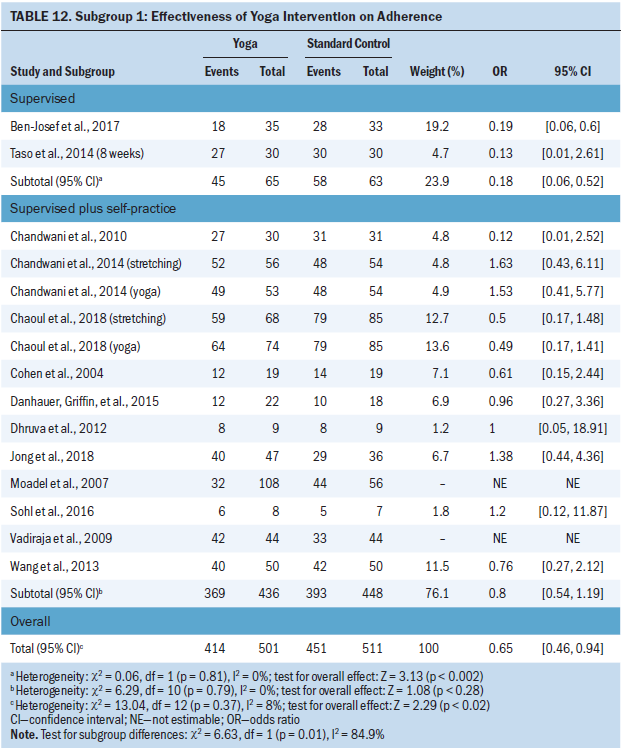
Subgroup 3: Impact on adherence with different cancer types: Ten interventions involving 891 patients with breast cancer had a pooled OR of 0.77 (95% CI [0.51, 1.16]) with high heterogeneity (I2 = 0%, p = 0.59). Three studies involving 121 patients with prostate cancer, lymphoma, and colorectal cancer had a pooled OR of 0.36 (95% CI [0.16, 0.81]), with medium heterogeneity (I2 = 29%, p = 0.25) (see Table 14). The validity of this result was low because of the small sample size. 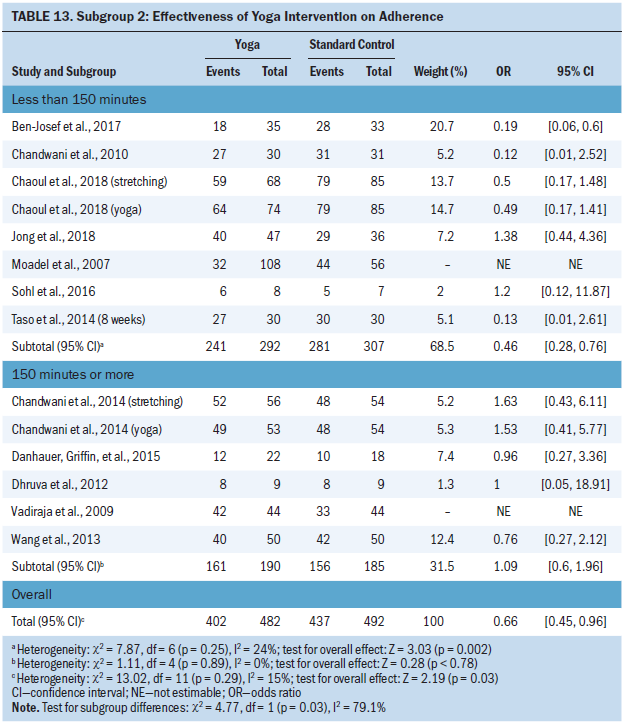
The results of other subgroup analyses showed no significant difference among different yoga styles and intervention durations on patient adherence. Only four of the included studies reported no adverse events associated with yoga. 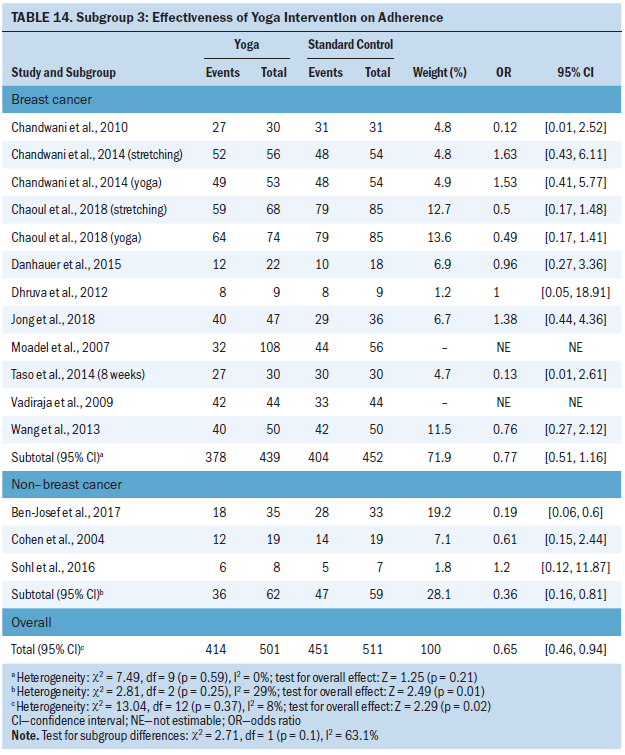
Discussion
This systematic review and meta-analysis included a reasonably adequate number of studies and total numbers of patients (n = 16, 1,453 patients), which provided evidence on the effectiveness of yoga on CRF in patients undergoing chemotherapy and/or radiation therapy. Compared with routine care, the current analysis has demonstrated that yoga could reduce CRF, which is consistent with findings from Cramer et al. (2017), but contrary to that of Hilfiker et al. (2018) and Pan et al. (2015). Small sample sizes and high heterogeneity between included studies may have contributed to inaccuracy, inconsistency, and variability among several systematic reviews. Also, in previous reviews, additional subgroup analyses were not performed.
Subgroup analysis in the current study demonstrated that yoga type, intervention strategy, weekly and total duration, and assessment instrument were significant factors that affected the reported effectiveness of yoga on CRF. Most of the studies included in the current review instituted mixed yoga, and the current meta-analysis has confirmed the effectiveness of mixed yoga compared to posture-only (stretching) or mind-breathing yoga. Patients with cancer experience significant fatigue, of which the root cause is often multidimensional, including physical, emotional, and/or cognitive factors. Mixed yoga could improve the physical function and mental state of patients undergoing cancer treatment.
Contrary to other reviews (Lipsett et al., 2017; Meneses-Echávez et al., 2015; Velthuis et al., 2010), the current meta-analysis revealed that supervision in addition to self-practicing strategy was more effective than supervision alone. Such inconsistency of findings may be related to the fact that the majority of the patients in the included studies were outpatients or part-time inpatients, who not only have been experiencing treatment-induced fatigue but also other life events, which may make them prefer to have flexible arrangements of yoga schedule and location of intervention. However, supervision of treatment at regular intervals would appear to be more conducive to providing physical and mental health support, which would improve patient adherence with treatment. Again, a small sample size in the subgroup of supervised strategy may contribute to the inconsistency of the results between meta-analyses.
Several previous reviews have concluded that a high volume of exercise does not relieve CRF in patients undergoing treatment for cancer (Carayol et al., 2015; Kessels et al., 2018; Schwartz et al., 2001; Velthuis et al., 2010), although the definition of high-volume exercise has been inconsistent among the studies. In the current analysis, yoga with a weekly duration of 150 minutes or greater per week and a total intervention duration of less than eight weeks appeared to be the most effective in reducing CRF.
In the reviewed studies, the adopted assessment instrument consisted of six scales, in which the reliability and validity have been verified in patients with cancer (Gebremariam et al., 2018; Paramita et al., 2016). The current authors did not merge the data from four of the six scales in one study. The BFI was the most commonly used assessment tool for CRF in the included studies. The current meta-analysis has shown that the effectiveness of yoga intervention in the subgroup analyzed with the BFI appeared lower but more precise than interventions analyzed using the CFS.
The heterogeneity was substantial in the current meta-analysis, which could not be reduced by subgroup analysis. However, in the BFI subgroup, three dubious interventions have been identified in the sensitivity analyses; when these were omitted, the heterogeneity was reduced and the outcome became steady. Causes of heterogeneity in the current analysis would likely be multifactorial, including different assessment instruments, yoga type (only stretching intervention in two studies) (Chandwani et al., 2014; Chaoul et al., 2018), and the outcome assessment on CRF following yoga intervention being too early (four weeks) (Taso et al., 2014), which were the major sources of heterogeneity.
Patient Adherence With Yoga Intervention
Patient adherence is one of the most important factors when determining the effectiveness of an intervention. To the authors’ knowledge, few reviews have performed a narrative-only analysis of patient adherence to an exercise intervention (Buffart et al., 2012; Meneses-Echávez et al., 2015; Velthuis et al., 2010). The current study represents the first meta-analysis examining patient adherence to yoga interventions while undergoing cancer treatment. Factors for patient attrition included schedule conflicts, movement restrictions, transportation issues, lack of time, difficulty in attending regularly, changing treatment regimens, and other health-related problems. In the current study, several factors may have affected patient adherence. Of note, the adherence of patients involved in a supervised-based yoga intervention less than 150 minutes per week was significantly lower, in parallel with the effectiveness on CRF. This suggests that a supervised-based format in addition to self-practicing strategy might offer more flexibility and improve adherence to outpatient visits. An optimal intervention duration might correspond to improved CRF, leading to increased persistence and confidence in the practice of yoga.
When patient adherence was analyzed in the current study, significant heterogeneity was noted among three studies; one study performed random assignment in a 2:1 ratio and the others performed in a 1:1 random assignment. Patient adherence might be increased when the yoga intervention is instituted in an inpatient setting, as was the case in the study by Vadiraja et al. (2009).
Quality of Evidence
The overall risk of bias of the included studies was medium to low. Of the 16 studies, 12 provided detailed information regarding random sequence generation, of which allocation concealment and detailed information were reported in five studies (Chakrabarty et al., 2015; Cohen et al., 2004; Moadel et al., 2007; Taso et al., 2014; Vadiraja et al., 2009). This resulted in a moderate risk of selection bias. Blinding is an important principle in the RCT setting but is difficult to implement when the investigators need to know the intervention and when CRF is a patient-reported outcome. Therefore, none of the studies implemented blinding. Although downgrading of the evidence did not occur as a result of this, the risk of performance and detection bias remained notable. Nine studies were classified as low risk of attrition bias because ITT analysis was performed and adequate information regarding reasons for patient attrition were provided (Ben-Josef et al., 2017; Chakrabarty et al., 2015; Chandwani et al., 2010, 2014; Chaoul et al., 2018; Danhauer, Griffin, et al., 2015; Sohl et al., 2016; Taso et al., 2014). None of the studies provided the registered protocol; therefore, the risk of selective reporting remains unclear.
Limitations
The current study had several limitations. First, there were very small sample sizes (less than 30 participants) in four of the included studies, which could increase the risk of bias. Second, there was high heterogeneity in the analyses of pooled effects of yoga on CRF, which could not be eliminated or reduced by performing subgroup analysis. Third, various instruments were used in the studies for the assessment of CRF. Therefore, performing a pooled analysis of data became difficult. Fourth, detailed information about participants who completed the yoga intervention was reported in only nine studies (Chandwani et al., 2010, 2014; Chaoul et al., 2018; Cohen et al., 2004; Danhauer, Griffin, et al., 2015; Jong et al., 2018; Moadel et al., 2007; Taso et al., 2014; Vadiraja et al., 2009), and data on attrition had to be extracted to replace the actual participation of other studies, which could influence the ultimate results.
Implications for Practice and Research
Despite the methodologic limitations, the practice of yoga, particularly mixed yoga that combines with posture and either mind and/or breathing control exercise, can be recommended as an additional strategy in the management of CRF in patients undergoing chemotherapy and/or radiation therapy. Supervised yoga practice in addition to self-practicing strategy using yoga manuals or DVDs might be beneficial in increasing patient adherence and improving the effectiveness of yoga intervention. As a low-intensity exercise, yoga practice of 150 minutes or greater per week is safe and effective. Additional research consisting of adequate sample sizes, variety of cancer types other than breast cancer, a clear objective of assessment and outcome, inclusivity of blinding (at least the outcome assessors), and assessment of patient adherence to yoga intervention is required. Future studies should focus on strengthening the supervision of yoga exercise as management for CRF in the outpatient setting. 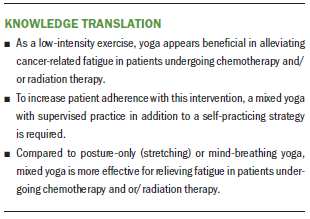
Conclusion
This study provides valuable evidence on the effect of yoga interventions on CRF in patients undergoing chemotherapy and/or radiation therapy. Yoga is a safe and effective tool in this regard. Mixed yoga and supervised in addition to self-practicing strategy might be more beneficial in increasing patient adherence and relieving CRF. Additional rigorous studies are required to explore an optimal strategy for yoga intervention.
About the Author(s)
Jihong Song, MA, is a PhD student in the School of Nursing at Xi’an Jiaotong University Health Science Center in Xi’an, Shaanxi, and a teacher in the School of Nursing at Fujian Medical University in FuZhou, Fujian; Tao Wang, MA, is a PhD student in the School of Nursing at Xi’an Jiaotong University Health Science Center and a teacher at Hainan Medical University in Haikou, Hainan; Yujie Wang, MA, is a PhD student in the School of Nursing at Peking University in Beijing; Rong Li, MA, is a nurse in Qilu Hospital of Shandong University in JiNan, Shandong; Sitian Niu, BSN, and Litao Zhuo, BSN, are students in the School of Nursing at Fujian Medical University; and Qian Guo, MA, is a research assistant, and Xiaomei Li, PhD, is a professor, both in the School of Nursing at Xi’an Jiaotong University Health Science Center, all in China. This study was supported by the Natural Science Foundation of Fujian Province, China (grant no. 2017J01815). X. Li contributed to the conceptualization and design. T. Wang, Y. Wang, R. Li, Niu, Zhuo, and Guo completed the data collection. Song, T. Wang, Y. Wang, and X. Li provided analysis. Song, Guo, and X. Li contributed to the manuscript preparation. X. Li can be reached at roselee8825@163.com, with copy to ONFEditor@ons.org. (Submitted July 2020. Accepted October 10, 2020.)




