Effect of Foot Reflexology and Aromatherapy on Anxiety and Pain During Brachytherapy for Cervical Cancer
Objectives: To determine if the addition of aromatherapy and foot reflexology to the standard of care improves pain and anxiety in patients receiving brachytherapy for cervical cancer.
Sample & Setting: 41 women with locally advanced cervical cancer who received intracavitary brachytherapy as part of their treatment.
Methods & Variables: Participants were randomized to either the control group, which received the standard-of-care management during brachytherapy, or the intervention group, which received the addition of aromatherapy and foot reflexology to standard of care. Participants rated their pain on a numeric rating scale and anxiety on the State–Trait Anxiety Inventory (STAI) and a numeric rating scale at five different time points.
Results: All average pain and anxiety scores were equal or lower at each key time point for the intervention group. Statistically significant differences were found for the intervention group for anxiety on the numeric rating scale and on the STAI, but only post-reflexology.
Implications for Nursing: Nurses and other healthcare providers can be trained to provide reflexology during painful, anxiety-producing procedures to increase patient tolerance of these treatments and overall quality of life.
Jump to a section
Integrative therapies, such as relaxation, guided imagery, massage, aromatherapy, and reflexology, are becoming more commonly used by patients with cancer (Blackburn et al., 2017; Candy et al., 2020). However, there is a lack of clear scientific evidence to support their use. Integrative therapies are safe, comparatively inexpensive, and may offer an alternate or additive option when conventional techniques fail to rid the patient of symptoms. Some experts report that aromatherapy and foot reflexology have the potential to improve pain and anxiety (Blackburn, 2018; Candy et al., 2020; Schiff et al., 2019; Wyatt et al., 2012, 2017) and, therefore, may be beneficial to patients who experience these symptoms. This study aimed to determine if the addition of two common integrative therapies, aromatherapy and foot reflexology, would decrease patients’ pain and anxiety when receiving brachytherapy treatment for cervical cancer.
Background
Integrative Therapies
Interest in the use of integrative therapies has grown during the past two decades, particularly in the population of patients with cancer (Blackburn et al., 2017; Candy et al., 2020). These techniques are used to enhance physical and mental health and wellness, manage pain and other symptoms, and empower individuals to take responsibility for their own health (National Center for Complementary and Integrative Health, n.d.). The techniques, when used with allopathic or Western medicine, are called complementary therapies. In more recent terminology, integrative therapies refer to a combination of mainstream medicine and complementary therapies based on scientific evidence of safety and effectiveness (National Center for Complementary and Integrative Health, 2018).
Aromatherapy: Aromatherapy has been used in countries like Egypt and India as a tradition of herbal medicine for thousands of years (Lua & Zakaria, 2012). According to the National Association of Holistic Aromatherapy (2021), aromatherapy uses natural plant extracts (e.g., essential oils, hydrosols, carrier oils) to heal the body, mind, and spirit. Essential oils use the olfactory system to create a mind–body connection (Harris, 2011). Evaluation of the effects of aromatherapy is complicated by its emotional and physiologic effects (Hodge et al., 2014). Specific aromas may work differently for individual patients, either positively or negatively, based on their previous experience with that fragrance (Buckle, 2003). The aroma from the chosen essential oil binds with the receptors in the nasal epithelium, which results in a neurochemical reaction that is transmitted to the olfactory bulb in the brain, the limbic system, and the thalamus, causing a release of endorphins and serotonin (Lane et al., 2012; Stringer & Donald, 2011; Varney & Buckle, 2013).
Lack of rigorous research on aromatherapy and essential oils has been a barrier to their use in the hospital environment (Lane et al., 2012). Sarris and Byrne (2011) conducted a systematic review on the use of complementary medicine and found that many randomized controlled trials lacked methodologic rigor, had small sample sizes, or had an inadequate control condition. Among the studies that met the inclusion criteria, there was evidence to support acupressure, tai chi, and yoga, but studies meeting the inclusion criteria using aromatherapy or reflexology were not located or did not exist. A randomized controlled trial by Trambert et al. (2017) of 87 women undergoing breast biopsies who received aromatherapy showed a statistically significant decrease in anxiety. A systematic review and meta-analysis by Lakhan et al. (2016) reviewed 12 studies that showed a significant positive effect of aromatherapy on pain, including postoperative and obstetric/gynecologic pain.
Foot reflexology: Foot reflexology is a manual technique based on the zone theory. The zone theory explains that certain points on the feet correspond to parts of the body (Candy et al., 2020; Öztürk et al., 2018). These points are linked to internal organs, glands, and other body parts by energy channels, zones, and/or meridians. Techniques, such as thumb- and finger-walking, hook and backup, and rotating on a point, stimulate the complex neural pathways linking body systems and support the body’s efforts to function optimally (Ball, 2016; Karatas & Dalgic, 2020). Based on the neuromatrix theory of pain, reflexology is thought to relieve pain by transmitting afferent impulses to close neural gates in the dorsal horn of the spinal cord, blocking pain transmission.
Studies on reflexology have demonstrated its effectiveness as a distinct complementary practice within the holistic field, but more research is needed. In a study by Wyatt et al. (2017), reflexology was shown to be an evidence-based intervention to improve health-related quality of life for patients with advanced breast cancer during chemotherapy and hormone therapy. Another study demonstrated the technique to be safe and useful in relieving dyspnea and enhancing function in patients with advanced breast cancer (Bao et al., 2014). In systematic reviews, Lee et al. (2011) found reflexology to be a useful intervention to relieve pain and promote sleep, and Bao et al. (2014) found that it may be useful in relieving cancer pain. Reflexology has been shown to be an effective method to decrease the physiologic signs of anxiety and decrease sedation needs in mechanically ventilated patients (Akin Korhan et al., 2014). In a randomized controlled trial, Dikmen and Terzioglu (2019) found that reflexology and progressive muscle relaxation exercises provided to patients with gynecologic cancer during chemotherapy decreased pain and fatigue and increased quality of life. A randomized controlled trial by Öztürk et al. (2018) looked at the effects of reflexology on anxiety and pain post–abdominal hysterectomy and found that foot reflexology may be an effective nursing intervention to increase well-being and decrease pain in female patients.
Brachytherapy for Cervical Cancer
The standard-of-care treatment for patients with locally advanced cervical cancer is combination chemotherapy and radiation therapy, consisting of external beam radiation therapy with concurrent chemotherapy followed by brachytherapy (Kirchheiner et al., 2014; Proud, 2007). Brachytherapy allows the administration of high doses of radiation to the primary tumor while sparing doses to the normal organs at risk, resulting in improved local control and survival when compared to those who do not receive brachytherapy (Gill et al., 2014). Brachytherapy is performed by placing an applicator and radioactive source inside the uterus and/or vagina to deliver a high dose of radiation to the patient. Because of the rapid dose fall-off of the radioactive source, organs at risk, including the bladder and rectum, are spared most of the high dose of radiation from the treatment (Amsbaugh et al., 2016; Kirchheiner et al., 2014; Proud, 2007; Weibe et al., 2011).
Intracavitary brachytherapy for cervical cancer uses a ring and tandem applicator in the ambulatory setting, typically over five treatments (Proud, 2007). Patients receive about five weeks of external beam radiation therapy prior to being reevaluated for brachytherapy. The radiation oncologist confirms the patient is a candidate for intracavitary brachytherapy based on clinical examination findings and pelvic magnetic resonance imaging that occur during a preprocedural visit in the fourth week of pelvic radiation. Patients at the Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (the James) in Columbus, Ohio, typically undergo general anesthesia for cervical sleeve placement. The sleeve is sutured to the cervix and left intact throughout the five fractions. The first ring and tandem applicator placement is performed at this same time, with the patient under general anesthesia (Proud, 2007). During the remaining four fractions of treatment, conducted over the following two weeks, general anesthesia is not used routinely, and ring and tandem applicators are placed and removed at each treatment visit. The schedule for the five fractions of brachytherapy are represented in Table 1. 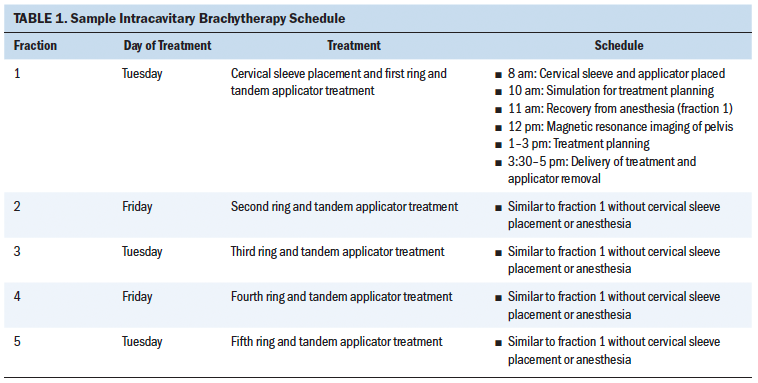
Tandem placement in the uterine corpus causes sympathetic stimulation of the hypogastric plexus, leading to cramping and visceral pain. In addition, the presence of the ring and cervical sleeve elicits parasympathetic stimulation of the pelvic splanchnic nerve, with resulting lumbar pain (Proud, 2007). Analgesia is essential to patient comfort and facilitates correct applicator placement, which improves dose delivery to the target area and decreases potential toxicity to adjacent organs (Proud, 2007). Analgesia during the procedures at the James consists of IV opioids, anti-inflammatory analgesics, and antianxiety medications as needed for the duration of the treatment planning and delivery of the radiation dose (Weibe et al., 2011). The ring and tandem applicator is removed after each treatment, and the patient is returned to the room for a short recovery and then discharged (Proud, 2007).
Key time points identified by patients for pain and anxiety during these procedures include during placement of the applicator, during treatment, and during applicator removal (Kirchheiner et al., 2014; Kwekkeboom et al., 2009; Néron et al., 2014; Weibe, et al., 2011). The transvaginal application itself is an invasive procedure in an intimate and vulnerable body area, which is often fraught with taboo. Manipulation in the genital area may represent an immediate impairment of physical integrity and an unwanted body intrusion (Kirchheiner et al., 2014; Perez et al., 2016). Symptom management, in general, in this patient population requires a considerable amount of support and expert medication management during repeated ambulatory visits. Optimal pain and anxiety management is sometimes elusive despite the best efforts of experienced practitioners.
Objective
Brachytherapy is invasive by nature, with potential long-lasting emotional effects on the patient. Alleviating pain and anxiety from the procedures would provide significant benefit to the well-being of women with locally advanced cervical cancer. The purpose of this randomized controlled trial was to determine if the addition of aromatherapy and foot reflexology to the standard of care could improve pain and anxiety in patients receiving brachytherapy for cervical cancer. The implications of a nonpharmacologic treatment for pain and anxiety relief during treatment could significantly affect the psychological well-being of these women.
Methods
Sample and Setting
Women with locally advanced cervical cancer were recruited for the study. Participants could be included in the study if they had locally advanced cervical cancer treated with combination chemotherapy and radiation therapy and were a candidate for intracavitary brachytherapy. Patients were excluded from the study if they required interstitial brachytherapy (treatment with radioactive seeds in the tissue rather than intracavitary applicators); were unable to give informed consent or use the numeric rating scale; had asthma, sleep apnea, reactive airway disease, or open areas or rash on their feet; had deep vein thrombosis or other limb circulatory problems including phlebitis, gallstones, or kidney stones; or were non–English speaking.
To achieve at least 80% power to detect a treatment effect from aromatherapy and foot reflexology, the minimum sample size was set at 40 patients. This sample size would detect a treatment effect of 0.6 or more points on the numeric rating scale for pain and 0.6 points or more on the State–Trait Anxiety Inventory (STAI). The power analysis was determined by performing a Monte Carlo simulation for each combination of the factor effects that were used in the power analysis, generating 1,000 datasets. The power analysis used a mixed-design analysis of variance to fit the model.
Instruments
Measurement of pain: A numeric rating scale was used to measure pain in this study. Patients chose a number that best represented their pain intensity on a scale of 0 (no pain) to 10 (worst pain imaginable). The numeric rating scale remains the most widely accepted pain scale in health care (Pasero & McCaffery, 2010). The reliability and validity of this pain scale is well established (Jensen & Karoly, 2001). Studies indicate that the numeric rating scale is valid as a measure of pain intensity among patients with cancer. A Spearman correlation coefficient demonstrates a strong positive correlation between the visual analog scale and the numeric rating scale (r = 0.847, p < 0.001). Other major strengths of this tool are that most patients and clinicians are familiar with it, and it is easily administered. The universal adoption of a 0–10 numeric rating scale for pain assessment has been promoted for some time (Paice & Cohen, 1997).
Measurement of anxiety: The long and short forms of the STAI for adults were used to measure anxiety. The STAI is one of the most frequently used measures of anxiety in health care and psychology research (Marteau & Bekker, 1992). The long-form STAI consists of 40 questions and is reliable and sensitive to measures of anxiety (Martean & Bekker, 1992). The short-form STAI consists of six questions and produces similar scores to that of the long-form STAI. It has acceptable reliability (reliability coefficients: long-form STAI = 0.91, short-form STAI = 0.82) and produces similar scores (paired t tests demonstrated p < 0.05) across subject groups manifesting normal and raised levels of anxiety (Marteau & Bekker, 1992). The long-form STAI was used for the initial/baseline survey regarding anxiety, and the short-form STAI was used during brachytherapy treatments for anxiety assessment at multiple time points. Patients in the study were also asked to rate their anxiety on a numeric rating scale from 0 (no anxiety) to 10 (worst anxiety imaginable) to allow for comparison of anxiety and pain.
Design
Patients were scheduled for brachytherapy by the radiation oncologist. Following study approval by the institutional review board and the cancer scientific research committee at the James, new patients were screened for inclusion and exclusion criteria when they were scheduled. If eligible for the study, the patient was approached for consent by the clinical nurse specialist during an ambulatory clinic visit. After consenting for the study, patients were randomized using GraphPad software to either the control group, which received the standard-of-care management during brachytherapy, or the intervention group, which received the addition of aromatherapy and foot reflexology. The standard-of-care management received by all participants during their treatments consisted of all of the usual pain and anxiety medications, warm blankets, limited position changes and propping with pillows for comfort, and staff support. Because of the importance of the patients’ scent preference and previous experience (either positive or negative) with aromas, the patients in the intervention group were given a choice of the three differently scented essential oils approved for use at the James: lavender, lemon, or peppermint. Patients were introduced to the scents by placing a drop of each essential oil on a cotton ball for them to smell.
All patients completed the long-form STAI and a pain assessment on the numeric rating scale to serve as a baseline of their pain and anxiety prior to starting treatment. Demographic and other data were then collected from the electronic health record, including diagnosis, stage, histology, age, marital status, and income. Details regarding treatment, including radiation dose of external beam and brachytherapy and chemotherapy regimen, were also collected. Historical medical details, including current use of opioids, other pain medication, or antianxiety medication; history of substance use disorder; and history of anxiety diagnosis, were collected and recorded.
During the entire brachytherapy treatment for patients in the intervention group, a hospital-approved travel diffuser with the chosen essential oil was placed at the head of the patients’ bed. Three drops of the chosen essential oil were added, and the scent was diffused until the patient was discharged. The patients in the intervention group also received a 30-minute foot reflexology treatment during the time set aside for treatment planning by the radiation oncologist. This time period occurs consistently after applicator placement and imaging and just prior to the actual treatment delivery. Patients routinely experience 90–120 minutes of rest time, during which they are cared for in a separate room in the radiation oncology department, given medication as needed, and made as comfortable as possible with standard-of-care interventions. The staff who performed foot reflexology were limited to two psychiatric mental health clinical nurse specialists who were trained in the technique through the same training program. These two practitioners developed and tested a framework for a standard, consistent 30-minute reflexology session (see Figure 1). 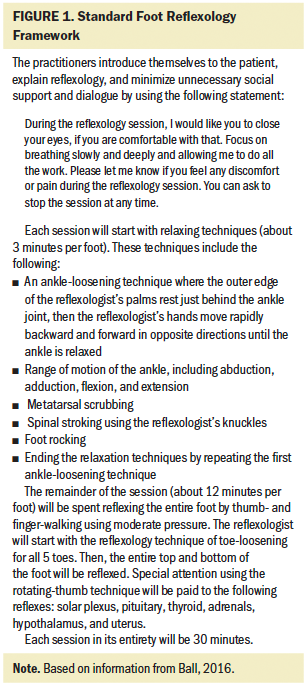
Participants in both groups rated their pain on the numeric rating scale and anxiety on the short-form STAI at five different times during their ambulatory visit: on arrival to the clinic, after placement of the ring and tandem applicator, just prior to reflexology, after foot reflexology (and associated times for the control group), and after removal of the ring and tandem applicator. In addition, patients in the intervention group were asked to evaluate their experience with aromatherapy and foot reflexology prior to being discharged from their fifth treatment. All pain and anxiety medication and dosages that were administered to patients during these treatments were tracked. Average morphine milligram equivalents (MMEs) for pain medications and average lorazepam milligrams for anxiety were compared for the two groups.
Results
Forty-one women with locally advanced cervical cancer who received a total of 193 intracavitary brachytherapy treatments as part of their treatment for cervical cancer were enrolled in this study. Full demographics for participants in the study are listed in Table 2. FIGO staging for cervical cancer can range from least invasive (stage 0 or carcinoma in situ) to most invasive (stage IV with cancerous spread beyond the true pelvis or into the mucosa of the bladder or rectum) (Matsuo et al., 2019). Staging and histology were similar in both groups of participants. Almost all participants received cisplatin as their chemotherapy regimen, with the exception of three participants in the control group who received carboplatin. There were more participants in the intervention group with an opioid prescribed at baseline prior to the study by 20%. More patients in the control group (16% more than intervention group) were on antianxiety agents prior to the study; however, more patients in the intervention group (9% more than control group) had a documented history of anxiety prior to the study. Both groups had an equal prevalence of opioid substance use disorder prior to study initiation. Overall, demographics and other important medical and health history data proved to be fairly equal between the two groups. 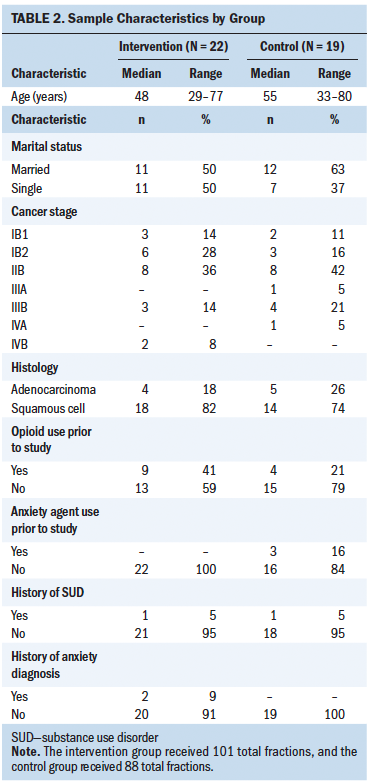
Six participants were unable to complete the data for the full five fractions of treatment. A CONSORT diagram for participant participation in this study is shown in Figure 2. Lavender was the essential oil scent chosen most frequently (n = 12), followed by lemon (n = 7), and then peppermint (n = 3). 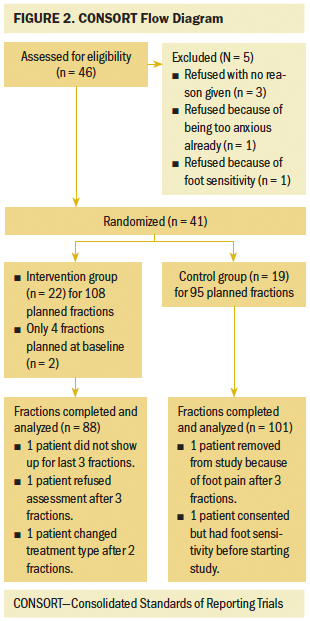
Participants who completed five planned fractions of treatment (n = 35) had as many as 25 pain ratings, five from each of the five treatment fractions. Pain scores were averaged over fractions to give each participant one overall average pain rating per fraction. Anxiety scores were treated similarly, and each participant ended up with one overall average anxiety score for each treatment fraction. The analyses were based on these average scores. Table 3 provides summary statistics for the average pain and anxiety scores for each group at each key time frame. 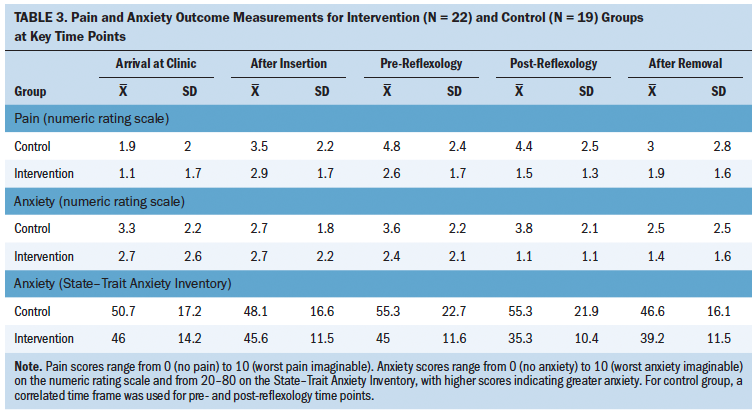
To account for the possible correlation of pain scores from the same subject, the within-subject repeated measures were modeled using an unstructured covariance matrix. All modeling was done in SAS, version 9.4, using the MIXED procedure. The goals of modeling were to assess whether there were treatment differences between the two groups and to assess whether the effect of the intervention after reflexology was different from that before reflexology. Anxiety scores were treated in a similar fashion.
Average pain scores were lower for the intervention group at each time of measurement, with the greatest differences demonstrated at the post-reflexology measure. The average pain score was 2.9 points lower in the intervention group than the control group for the post-reflexology measure. Anxiety was measured on two different scales. The STAI was used because it provided an evidence-based tool that has shown validity and reliability. The numeric rating scale was used to be able to better compare scores for pain and anxiety to determine which was affected to a greater extent. Average anxiety scores on the STAI and numeric rating scale were lower for the intervention group at each time of measurement with one exception—on the numeric rating scale, anxiety scores were the same in both groups after insertion of the applicator. The greatest difference in average anxiety scores was a difference of 2.7 points on the numeric rating scale and a difference of 20 points on the STAI, which both occurred at the post-reflexology time point.
Table 4 shows treatment differences between the two groups in pain and anxiety after baseline and the differences pre- to post-reflexology. All average pain and anxiety scores were equal or lower at each time point for the intervention group. However, statistically significant differences were found for the intervention group for pain (p ≤ 0.0001), anxiety on the numeric rating scale (p ≤ 0.0001), and anxiety on the STAI (p ≤ 0.0001) only post-reflexology. 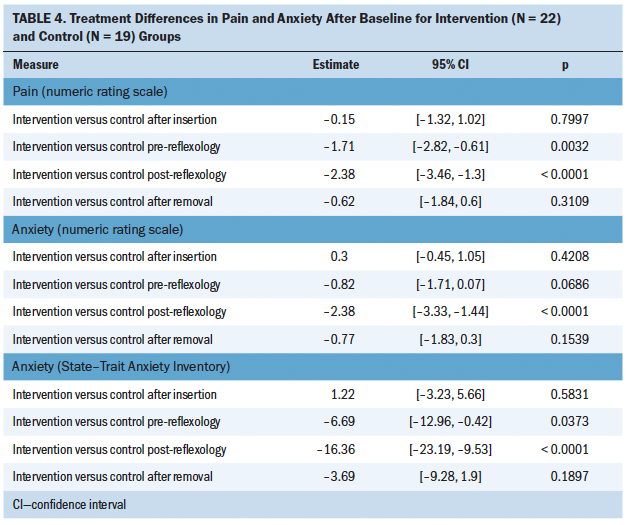
Not including medications given for anesthesia during the first fraction, IV medications that were given to patients to decrease reported pain included morphine, fentanyl, hydromorphone, toradol, and vistaril. Oral medications given for pain control included acetaminophen/hydrocodone, oxycodone, acetaminophen/oxycodone, and tramadol. All of those medications were converted to MMEs to compare doses between the two groups. The average MME was lower for the intervention group (mean = 47.7 mg, range = 18–89.5 mg, median = 45 mg) than for the control group (mean = 53.5 mg, range = 20–142.5 mg, median = 43 mg); however, there was no evidence of a treatment group effect on MMEs (p = 0.98).
Many participants received IV lorazepam to reduce anxiety, which was not included in the MME. The total lorazepam use was 51 mg (0.5 mg per fraction) for the intervention group and 66.5 mg (0.8 mg per fraction) for the control group. Less lorazepam overall was prescribed to the intervention group, but there was no evidence of a treatment effect on lorazepam (p = 0.12).
At the end of the five fractions of brachytherapy, the intervention group was asked to self-evaluate their experience with each intervention in terms of the experience itself and the degree to which it eased their pain and anxiety on a scale of 1 (terrible) to 10 (exceptional). Table 5 shows that both interventions were rated highly, with foot reflexology being the most helpful of the two and making the most difference in anxiety. 
Discussion
This study was designed to generate evidence for or against the use of integrative therapies (i.e., aromatherapy and foot reflexology) to decrease pain and anxiety in patients with cervical cancer during brachytherapy treatment. The current standard of care entails using pain and anxiety medications that do not work optimally for all patients and come with their own set of negative side effects. The medications are supplemented by support from staff and minimal position changes with propping. Position changes are difficult because of the internally placed ring and tandem applicator and because treatment planning has been done to determine dosage of radiation to surrounding tissues and structures. Additional integrative therapies, if found to be evidence-based, would provide another tool to optimize the patient experience.
The sample for this study was adequate for the projected power analysis, and demographic data were similar in both groups. Statistically significant differences between the two groups were evident for pain and anxiety measures post-reflexology. Because aromatherapy was administered throughout the patient’s ambulatory stay, it appears that aromatherapy did not contribute as much to the differences between groups as did foot reflexology. This is also reflected in the intervention group’s final evaluation, with reflexology being rated as most helpful and affecting anxiety to the greatest extent.
Pain and anxiety ratings on all scales were lower in patients who had aromatherapy and foot reflexology added to the standard of care at all time frames assessed during treatment, with the exception of one assessment of anxiety after insertion that was equal in both groups on the numeric rating scale for pain and for anxiety. All differences in pain and anxiety between the groups were the greatest at the post-reflexology time point. All differences in pain and anxiety between the two groups at the post-reflexology time point were found to be statistically significant. Because aromatherapy was being used throughout the treatment period, it can be inferred that it was reflexology that made the difference at that critical time point. Participants in the intervention group enjoyed the experience of both interventions but rated reflexology as helping to a great extent in managing their pain and anxiety. One patient commented that she could not have imagined the difference these interventions would make when she was in such distress, and another stated that the relaxation and decreased pain effects of the foot reflexology would sometimes last until the evening when she was home and settled. The intervention group used less medication for pain and anxiety than did the control group; however, this difference was not statistically significant.
The findings of significant pain and anxiety reduction post-reflexology are important and should continue to be investigated, particularly for treatments that are known to cause these symptoms. The current findings for reflexology support the previous findings of the studies listed in the literature review. Some patients with cancer require aggressive therapy, leading to much symptomology to adequately treat their disease and give them the best chance of long-term survival. These patients deserve to have evidence-based integrative therapies, such as foot reflexology, offered to them as a support during treatment. The barriers to offering such therapies, such as lack of time and resources, must be balanced with the need for better symptom management for these patients.
Strengths and Limitations
Major strengths of the study include the rigorous methods applied to assessment at five key time points commonly affecting these patients. Internal reliability was achieved by having only a limited number of staff intervening with the patients, including one clinical nurse specialist for consent and baseline evaluation, two similarly trained clinical nurse specialists providing reflexology, two physicians performing brachytherapy procedures, and three RNs assessing pain and anxiety in patients.
Limitations of the study include that the intervention group participants did not have anonymity during their treatment because of the aromatherapy diffuser on their hospital beds. Because of the changing nature of the daylong brachytherapy patient schedule, it was difficult to anticipate when the foot reflexology session would be needed. The reflexology practitioners demonstrated extreme flexibility to meet patient and study requirements. In addition, a potential confounder to the results is that patients could have premedicated themselves for either pain or anxiety prior to arriving at the clinic. Although the patients were randomized, the two groups had statistically significant differences in pain and anxiety at baseline.
Implications for Nursing
Oncology nurses are a critical point of contact for patients receiving repeated invasive treatment procedures, such as intracavitary brachytherapy. These nurses have the opportunity to develop a trusting relationship with the patient and family during treatment. During this time of opioid crisis, the use of integrative therapies along with standard medications to treat symptoms of pain and anxiety are of the utmost importance. Effective, evidence-based integrative therapies can decrease patient symptom burden without medication-associated cost and potential side effects. Part of the oncology nurse–patient therapeutic relationship must be the use of systematic, evidence-based integrative therapies.
Nurses can initiate aromatherapy safely and effectively with minimal training. They can teach patients to use aromatherapy, which can cause patients to have a greater sense of control over their treatment environments. Family and friends can also become involved in treatment by supporting the use of aromatherapy. Reflexology requires additional training, but once completed, could be added to a nurse’s arsenal of evidence-based interventions to allay pain and anxiety during treatments that are known to be stressful for patients. The technique of foot reflexology is simple, can be performed anywhere, requires no special equipment, is noninvasive, and does not interfere with other treatments the patient may be receiving.
Oncology nurses play an essential role in the assessment, management, and intervention of treatment-related symptoms that occur related to cancer treatment. Aromatherapy and reflexology have the potential to enhance existing medical and pharmacologic therapies within the oncology setting, particularly in terms of symptom management. For oncology nurses, an emphasis should be placed on continuing to research practical interventions that can improve the experience of patients with cancer throughout their treatment and afterward in various settings with diverse patient populations. 
Conclusion
Foot reflexology is a viable intervention for improving pain and anxiety for this specific subset of patients with cancer. This intervention is less costly and safer than the standard use of pharmacologic measures. More studies are needed to add to the growing evidence and to test applicability of aromatherapy and foot reflexology in other patient populations.
About the Author(s)
Lisa Blackburn, MS, APRN-CNS-BC, AOCNS®, is a clinical nurse specialist, Catherine Hill, MBA, RN, OCN®, is a patient care resource manager and RN, and Amy L. Lindsey, MS, APRN-CNS, PMHCNS-BC, is a mental health clinical nurse specialist, all at the Arthur G. James Cancer Hospital and Richard J. Solove Research Institute; Loraine T. Sinnott, PhD, is a senior statistician at the Data Coordinating and Analysis Center at the Ohio State University; Kathrynn Thompson, MS, APRN-CNS, PMHCNS-BC, is a retired mental health clinical nurse specialist at the Arthur G. James Cancer Hospital and Richard J. Solove Research Institute and a retired instructor of practice in the College of Nursing at the Ohio State University; and Allison Quick, MD, is a radiation oncologist at the Ohio State University Wexner Medical Center, all in Columbus. Blackburn, Thompson, and Quick contributed to the conceptualization and design. Blackburn, Hill, Lindsey, and Thompson completed the data collection. Blackburn and Sinnott provided statistical support. Blackburn, Sinnott, and Quick provided the analysis. Blackburn, Lindsey, Thompson, and Quick contributed to the manuscript preparation. Blackburn can be reached at lisa.blackburn@osumc.edu, with copy to ONFEditor@ons.org. (Submitted September 2020. Accepted November 24, 2020.)




