Supportive Care Needs of Chinese Women With Newly Diagnosed Breast Cancer Prior to Adjuvant Chemotherapy
Purpose: To describe the supportive care needs of Chinese women newly diagnosed with breast cancer prior to adjuvant chemotherapy.
Participants & Setting: 13 women newly diagnosed with breast cancer were recruited from a public teaching hospital in northern China.
Methodologic Approach: Semistructured interviews were conducted, and data were analyzed following a qualitative descriptive approach and qualitative content analysis.
Findings: The following five themes emerged: (a) physical symptoms management; (b) complex psychological pressure related to chemotherapy, family, and the missing breast; (c) hope of acquiring chemotherapy-related information in advance; (d) daily life guidance; and (e) communication and surrounding support.
Implications for Nursing: Nurses should focus on patients’ prechemotherapy supportive care needs and comprehensively assess their specific needs and concerns related to post-surgery discomfort and chemotherapy, with considerations of the Chinese family concept, diet, and traditional culture. Targeted health information and psychological support are necessary to help patients transition to and adequately prepare for chemotherapy.
Jump to a section
Breast cancer is the most frequently diagnosed cancer among Chinese women (Sung et al., 2021). In 2020, about 416,371 Chinese women were newly diagnosed, with the crude incidence rate reaching 59 cases per 100,000 individuals as indicated by the GLOBOCAN 2020 online database (Ferlay et al., 2020), which is expected to further increase in China (Wen et al., 2018). Few newly diagnosed women have sufficient information about the disease or its treatment (Jiang et al., 2016), and they often experience anxiety about treatments and fear of recurrence (Stephens et al., 2008). Adjuvant chemotherapy after surgery can effectively reduce breast cancer recurrence rates, but patients who received adjuvant chemotherapy following surgery have previously reported a variety of unmet supportive care needs, including psychological, informational, physical, daily living, and sexual needs (Cai et al., 2017; Xiao et al., 2016). In addition, compared to those who received chemotherapy alone, patients had more supportive care needs before the initial chemotherapy treatment after surgery (Pérez-Fortis et al., 2018). Although the impacts of chemotherapy on patients’ quality of life are significant, their supportive care needs are often underestimated in routine care (Akechi et al., 2011; Nakaguchi et al., 2013).
Supportive care needs refer to the help required by patients with cancer and their families beyond medical, surgical, or radiation therapy interventions, such as their physical, social, emotional, informational, psychological, spiritual, and practical needs (Fitch, 2008). Numerous studies have found that supportive care is an essential service for helping individuals with cancer manage treatment-related symptoms and cope with psychological problems (Lai et al., 2019; Sussman et al., 2018). Many countries have extended this service to prechemotherapy, which was shown to effectively increase patients’ knowledge of the treatment schedule and potential adverse events, as well as decrease anxiety and psychological and procedural concerns (Apor et al., 2018; Piombo et al., 2020). However, supportive care is yet to be well established in mainland China, and there is a large gap between cancer supportive care services and the needs of Chinese patients with cancer (Li et al., 2019).
Previous quantitative studies have investigated the supportive care needs of Chinese women with breast cancer (Au et al., 2013; Wang et al., 2018). Wang et al. (2018) found that 60% of Chinese women had a moderate to high need following diagnosis. However, quantitative studies are unable to elicit a deeper description of the patients’ needs and concerns. A study by Klungrit et al. (2019) explored the supportive care needs of patients with breast cancer while receiving chemotherapy. During the transition period after surgery before receiving chemotherapy, patients’ needs related to recovery and impending chemotherapy were unclear. Understanding the supportive care needs of patients with breast cancer is the basis for providing high-quality, patient-centered care and implementing effective interventions (Lai et al., 2017). Having knowledge of these needs prior to adjuvant chemotherapy is necessary for nurses to provide targeted support and adequately prepare patients for chemotherapy. Therefore, this study aimed to describe the supportive care needs of newly diagnosed Chinese women with breast cancer in the prechemotherapy stage following surgery to increase nurses’ attention to patient supportive care needs prior to adjuvant chemotherapy.
Methods
Design, Participants, and Setting
A qualitative design using a descriptive approach was adopted to describe the supportive care needs of Chinese women with breast cancer prior to adjuvant chemotherapy. Participants were recruited from a large public teaching hospital in Dalian, China. Using purposive sampling, patients were eligible for the study if they were (a) newly diagnosed with stages I–III breast cancer and had completed surgery, (b) aged older than 18 years, (c) going to receive chemotherapy for the first time, and (d) aware of their cancer diagnosis. Patients were excluded if they had a history of other malignancies or if they were considered physically or mentally incapable of participating in the study by clinic staff.
Data Collection
Data were collected from October to December 2019. Eligible patients from the oncology unit were selected with considerations to their age, cancer stage, marital status, and education to obtain a diverse range of information. After learning about the purpose and procedures of the study, patients who provided written informed consent were enrolled. A face-to-face, semistructured interview was conducted with patients in Chinese one day before they started the first line of chemotherapy (about one month after surgery).
An interview guide, which focused on the supportive care needs of Chinese women with breast cancer, was developed based on a literature review (Cai et al., 2017; Zdenkowski et al., 2016) (see Figure 1). Interviews were audio recorded. Data saturation (i.e., when new data repeat the data that were already collated) was achieved after 13 participants were interviewed (Grove et al., 2012). The interviews lasted for 35 minutes on average. 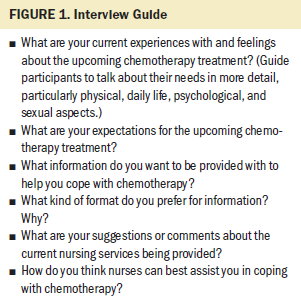
Data Analysis
A qualitative content analysis method was used to analyze the data (Schreier, 2012). The first author (Y.-J.C.) transcribed the interviews verbatim within 48 hours after each interview. Participants’ privacy and anonymity were assured.
First, material relevant to the research question was selected, then more abstract paraphrases for the material were progressively selected. Relevant material was marked, and a thematic criterion (i.e., where topic changes signal the end of one unit and the beginning of another) was used in segmenting the material, and the units of coding were marked. Two Chinese researchers (Y.-J.C. and X.Y.M) trial coded the same part of the material independently and made notes. The material, codes, and categories of the trial coding were translated into English by the first author (Y.-J.C), and the result of the trial coding was checked by the second author (H.M.), who is fluent in English. Differences were discussed, and then the coding frame was further modified. The first author (Y.-J.C.) coded all of the data under the coding frame, another Chinese researcher (X.-Y.M.) blindly coded part of the materials, and they discussed and re-evaluated the entire process. Finally, themes and subthemes were determined. At this point, all the relevant Chinese text, codes, and categories were translated into English. Three researchers (Y.-J.C., H.M., and X.-Y.M.) rechecked the results of the analysis together for consistency. Another researcher (T.-Y.S.) reviewed the translation from Chinese to English, and any inconsistencies were clarified after discussion (Schreier, 2012).
Trustworthiness
Several strategies were used to confirm the results’ trustworthiness (Morse, 2015). First, because the first author is a doctoral student with more than one year of experience in health education for Chinese women with breast cancer, a good understanding of patients’ concerns could be achieved. Second, a coding frame was developed to ensure reliability and validity. Third, the analysis process involved two Chinese researchers who conducted the trial coding and main coding. A researcher (H.M.) with extensive experience in qualitative research checked the coding frame and analysis process, and a consensus was achieved after discussion among all researchers.
Ethical Considerations
This study was approved by the ethics committees of Chiba University and the First Affiliated Hospital of Dalian Medical University. The purpose, possible risks of the study, anonymity, and confidentiality were explained to all participants, who were also aware of their right to withdraw at any time. All participants provided written informed consent.
Findings
Thirteen Chinese women with breast cancer were interviewed. The mean age of participants was 54 years. Demographic information and disease and treatment data are summarized in Table 1. 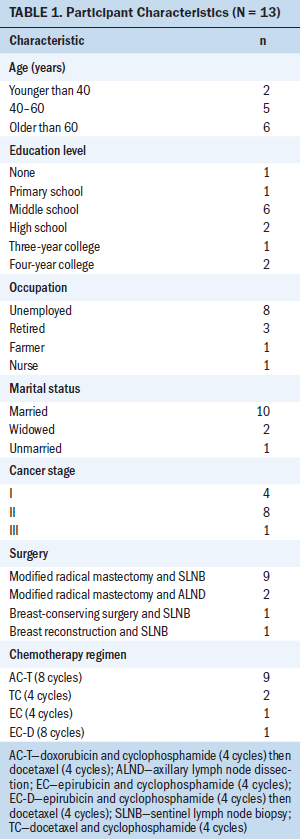
Participants reported a variety of prechemotherapy supportive care needs, which were divided into five themes and 14 subthemes (see Figure 2). Although each theme was related to a specific supportive care aspect, there was some overlap between themes. 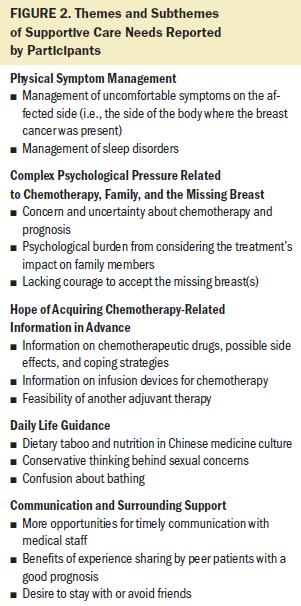
Physical Symptoms Management
Management of uncomfortable symptoms on the affected side: Twelve participants reported persistent discomfort on the surgery side. The most common symptoms were numbness, pain, and tingling around the surgical incisions and shoulder:
I feel a little numbness and pain on my arm. Why does it happen? Will the numbness last for a long time? Will it disappear later? I didn’t know how to deal with it after I was discharged from the surgery ward. (P1)
Participants wanted to know the causes and duration of symptoms, as well as how to relieve them. In addition, because of differences in education level, the surgical method used, and comprehension skills, some participants had an inaccurate understanding of self-rehabilitation exercises: “My education level is not high, and I cannot understand the instruction sheet given to me by the nurse” (P8). Participants also hoped to obtain individualized rehabilitation guidance from nurses: “For me, I had breast reconstruction surgery and have not recovered yet. I hope [the] nurses can give individualized guidance, such as when I shouldn’t do exercise and when to start” (P10).
Management of sleep disorders: A few participants had difficulty falling asleep and poor sleep quality, particularly when thinking about their upcoming hospitalization and chemotherapy treatment: “The main problem is that I cannot sleep well . . . especially when I am thinking about coming to the hospital soon. . . . Is there any way to make me sleep well?” (P2); “It is hard to fall asleep anyway. . . . I heard a lot of news about the [side effects of] chemotherapy. That scared me!” (P6).
Complex Psychological Pressure Related to Chemotherapy, Family, and the Missing Breast
Concern and uncertainty about chemotherapy and prognosis: Most participants expressed uncertainty and concern about the chemotherapy’s effectiveness, potential side effects, and the recurrence and metastasis of breast cancer: “I think chemotherapy is useless. Is chemotherapy equivalent to killing cancer cells? They [peer patients] said chemo would damage the body greatly. . . . Will I lose my hair when I start chemo?” (P2).
Participants were most concerned about the side effects of nausea, vomiting, and hair loss. Some were even afraid of being laughed at by others because of hair loss: “Oh, my God! I saw that they [peer patients] experienced heavy nausea and vomiting. If I start vomiting heavily, I couldn’t stand it” (P3).
Comparatively, a few participants mentioned uncertainty about future recurrence or metastasis: “I was diagnosed with invasive breast cancer. . . . I’m afraid of recurrence and metastasis” (P6).
Psychological burden from considering the treatment’s impact on family members: Participants of different ages expressed concerns about the cancer treatment’s impact on their families. For participants older than 60 years, when they were receiving treatment, their families put work aside to care for them, which made them feel stressed: “My daughter accompanied me to visit [the hospital] many times. . . . She still had a job. This messed her up; she also felt anxiety. . . . I increased her burden, I think” (P2). Middle-aged participants (aged 40–60 years) were highly concerned about the additional distress and burden on family members. This created a heavy psychological burden for them:
I am mainly considering my child. . . . I am afraid that cancer treatment may affect her studies. . . . Also, I didn’t tell my parents that I was sick. They are old; they cannot help me even if they know about it. I don’t want them to worry about me. . . . I need to comfort my husband because he is very introverted, and I worry he won’t get over my cancer. (P13)
Lacking courage to accept the missing breast(s): Some participants who underwent a mastectomy felt scared and found it difficult to face their lost breast(s): “I feel terrible. . . . It is hard for me . . . to see it. . . . I don’t even like seeing it myself. . . . It is uncomfortable, and it looks even worse than a man’s breast” (P9).
Hope of Acquiring Chemotherapy-Related Information in Advance
Information on chemotherapeutic drugs, possible side effects, and coping strategies: Twelve participants hoped to receive specific information in advance to help them fully understand chemotherapy and make informed choices: “Are the imported drugs better than the domestic [chemotherapy drugs]? Will the side effects [hair loss] be less? I don’t know which one to choose” (P6). They wanted to know more about the effects of different chemotherapeutic drugs and possible side effects, as well as how to deal with them, prior to receiving treatment: “I know nothing about chemotherapy—how to minimize side effects during chemotherapy or how to deal with side effects. If vomiting occurs, how can I minimize it? I hope to know in advance” (P5).
Information on infusion devices for chemotherapy: Eight participants had no idea how the infusion devices worked. They hoped to receive information about infusion devices, such as the placement position, cost, side effects, and limitations to daily life, before they chose a device: “I would like to know whether arm movement will be restricted after the infusion port is placed, and will it affect my daily life? Will it be infected if it is placed for a long time?” (P12); “I am still hesitant [about whether to use an infusion port]; I hope I can get more information early, so I will have enough time to decide” (P5).
Feasibility of another adjuvant therapy: In addition to chemotherapy, some participants wanted information on traditional Chinese medicine treatments: “I heard that chemotherapy drugs are toxic to the heart. I am confused as to whether I can use some traditional Chinese medicine to have the effect of Fuzheng Jiedu [strengthening body immunity and detoxification] during chemotherapy” (P13).
Daily Life Guidance
Dietary taboo and nutrition in Chinese medicine culture: Because of the ambiguity of the dietary guidelines provided by their doctor and uncertainty about the credibility of other sources, 11 participants wanted additional information about diet and nutrition:
What should I pay attention to when eating? [For example], what can be eaten, and what cannot be eaten? Can I eat seafood? Some patients say that fawu, such as mutton, cannot be eaten. Is that correct? There is nothing we can do about the treatment; the only thing we can regulate by ourselves is diet. I also hope to aid nutrition through diet. Diet cures more than doctors! (P7)
Fawu is closely related to a dietary taboo in Chinese medicine and greatly influences the diet of Chinese patients (Zhu & Xie, 2018). All participants in the current study resided in coastal areas, and most mentioned their need for accurate information about fawu, such as seafood: “I keep searching on Baidu [a Chinese website] . . . [to] try to find out how to improve nutrition . . . but I am still confused about food that belongs to the fawu [group], so I do not dare to eat them” (P13).
Conservative thinking behind sexual concerns: Because of conservative thinking, participants were embarrassed about asking their doctors about sexual matters. However, a few participants wanted this information:
Sex is private and embarrassing, but I also want to know whether it is possible to have sex during chemotherapy and whether it will affect my recovery. I think we Chinese people may be relatively traditional. Usually, I won’t ask. (P10)
Some worried that having less sex was a factor that caused breast cancer: “[My sex life] was less before diagnosis. I think [having] no sex life caused breast nodules. I am more concerned about this” (P13).
Confusion about bathing: A few participants were concerned about bathing while the surgical wound healed or while infusion devices were in place:
Can I take a bath during this period [of receiving chemotherapy]? How can I deal with this [infusion port] when taking a bath? After surgery, the wound [had] not healed well until now, and I have not dared to take a bath. I just wipe it with a towel. (P8)
Communication and Surrounding Support
More opportunities for timely communication with medical staff: Some participants tried to obtain information regarding cancer treatment from the Internet at home before the initial chemotherapy treatment, but difficulties with understanding medical terms and determining the accuracy of information confused them and made them feel scared. More than half of the participants reported their expectations for timely verbal communication with medical staff:
I hope the doctor or nurse will have time to talk to me face-to-face to address my doubts. . . . It will make me feel at ease. . . . I’ve never experienced this before. It is the first time in my life. I know they are busy, but I need them. . . . It would be better if I could communicate with them at any time. (P11)
Benefits of experience sharing by peer patients with a good prognosis: Some participants benefited from having peer patients with a good prognosis share their experience. It increased their confidence in the treatment: “Several patients I knew in the breast department told me that they were recovering well. Watching them recover well, I have more confidence in the treatment” (P8).
Desire to stay with or avoid friends: Some participants wanted to avoid friends because they were afraid that their friends might laugh when they noticed participants’ hair loss and learned about their cancer: “I am afraid of losing my hair. And it will be horrible if others know about it [that I have cancer]. . . . I fear being laughed at [about hair loss]! I will not contact my friends anymore” (P6).
Comparatively, a few participants who could not be sufficiently supported by family wanted to be accompanied by their friends:
I didn’t tell my parents or child about my cancer to not make them worry. . . . I don’t want anyone to know about my cancer and trouble them. But, in fact, I particularly hope that my best friend can accompany me, help me to share my feelings, [and] release my pressure. (P13)
Discussion
This study examined the supportive care needs of Chinese women with breast cancer prior to adjuvant chemotherapy. Almost all participants experienced uncomfortable symptoms on the affected side, such as numbness, pain, and tingling, and their daily activities were limited during the transitional stage of prechemotherapy. They wanted to know the causes and duration of symptoms, as well as strategies to relieve symptoms and manage discomfort. More than 88% of women with breast cancer chose to have a mastectomy in China because they were convinced it was safer than breast-conserving surgery (Wang et al., 2020; Zhang et al., 2015), and the majority of participants (n = 11) in the current study underwent a mastectomy. Accordingly, discomforting symptoms after a mastectomy are common in the Chinese patient population (Fu & Fu, 2019). The need for more support in managing uncomfortable symptoms may be because health education is conducted while patients are hospitalized in a surgical unit, whereas most of these symptoms appear following discharge. However, the focus of nursing in an oncology unit is caring for chemotherapy-related symptoms. Therefore, it is recommended that nurses be aware of the disparities in care involving providers in different locations during this transitional period. Nurses in the surgical unit should increase their follow-up and provide relevant information to help patients to manage discomfort and ensure continuity of care.
For some participants, psychological and emotional fluctuations related to their imminent hospitalization and chemotherapy treatment led to sleep disorders. Although some studies have confirmed that cognitive behavioral therapy and mindfulness-based stress reduction therapy (Qiu et al., 2018; Reich et al., 2017) can effectively alleviate sleep problems in individuals with breast cancer, these methods have not been widely used in women with breast cancer in China. Possible reasons may be related to the fact that some nurses may not have the professional knowledge and skills to implement psychological interventions. Therefore, it is necessary to explore more feasible nursing interventions to manage sleep disorders and improve patients’ quality of sleep.
Individuals with breast cancer may require support to overcome psychological distress. Owing to the lack of relevant information, participants in the current study experienced uncertainty and concerns about the possible side effects of short-term chemotherapy, as well as long-term recurrence and metastasis of breast cancer, which is consistent with the results of a previous study (Lai et al., 2017). Some participants reported a fear of being ridiculed because of hair loss after chemotherapy and planned to stay away from friends. These reactions may be related to the value of “saving face” in traditional Chinese culture (Wang et al., 2020). Participants also had a more significant psychological burden related to cancer’s impact on their families. Based on the influence of Chinese Confucianism, family culture has an extremely important social value. Participants cared about the impact of cancer on their families and not only on themselves (Wang et al., 2020). This was particularly true for the middle-aged women who were taking care of their parents and raising children. Considering the traditional cultural background of Chinese patients in supportive care interventions, providing cancer and chemotherapy-related information and implementing psychological counseling for patients in advance may help to alleviate feelings of psychological pressure on patients and lead to more effective transitions to chemotherapy treatment.
Participants in the current study reported that they needed more information in advance to adequately prepare for chemotherapy and make informed decisions. This finding is consistent with the results of a study by Au et al. (2013) in which patients worried about treatment because of the initial diagnosis of breast cancer and the lack of coping experience. Therefore, patients need more information about the effects of different chemotherapeutic drugs, the possible side effects of chemotherapy, coping strategies, infusion devises, and other adjuvant therapy to understand and best prepare for starting chemotherapy. In the current study, although participants researched chemotherapy and rehabilitation on the Internet and discussed their concerns with other patients, they still needed information support because they could not judge the accuracy of the information they found. Providing chemotherapy-related information during patients’ prechemotherapy procedures is necessary and essential in helping them feel prepared.
In addition, the findings of this study indicated that, under the influence of traditional Chinese culture, most participants coped conservatively when lacking knowledge. For instance, they did not perform self-rehabilitation exercises, intake any food they thought was fawu, or actively seek information about sexual activity, all of which was disadvantageous to their daily lives, as well as physical and mental recovery. This was especially true about diet, which is particularly important in Chinese culture. Fawu is a dietary term derived from traditional Chinese medicine that is widely spread among the population. It is believed that fawu may exacerbate surgical problems, such as sores and tumors, and cause allergic diseases or relapses. Many foods are considered fawu, including onions, leeks, chicken, mutton, fish, and shrimp (Zhu & Xie, 2018). There is no clear evidence, however, supporting fawu as a dietary taboo in breast cancer. Eating more vegetables may reduce breast cancer rates (Wu et al., 2015). Therefore, nurses should strengthen the educational information provided to patients about diet, sexual activity, and other aspects of daily life.
Based on their education level, comprehension ability, and different surgical methods, patients preferred to receive face-to-face, individualized guidance from nurses. Having more opportunities to communicate with doctors and nurses promptly, as well as hearing about other patients’ successful experiences, decreased their anxiety and made them feel more at ease. This finding is confirmed by Jefford et al. (2011), who found that nurse-led, individualized education information plays an essential role in meeting patients’ needs and improving their quality of life. A study by Kinnane (2012) also found that hospital-based information support provided by nurses and peers is effective in meeting the changing information and support needs of patients. In addition to providing patients with personalized education as much as possible considering limited medical resources, future studies on how to use the exemplary role of peers and meeting patients’ needs during the transition period prechemotherapy are needed.
Strengths and Limitations
This is the only known study focusing on the needs of newly diagnosed Chinese women with breast cancer prior to adjuvant chemotherapy. Understanding the needs of these patients during this period is essential for a smooth transition from surgery to chemotherapy. In addition, the study findings reflect patients’ specific needs within a Chinese cultural context and a limited medical resource background, which may help nurses to have a clear direction when providing care for patients with similar backgrounds.
This study has some limitations. First, all interviews were conducted in Chinese. There may be cultural differences despite best efforts to translate the findings into English. Second, the study was conducted at one public teaching hospital in the coastal area of China and may primarily reflect the characteristics of this location only. Therefore, patients in other geographic areas may have different and/or additional needs. Future studies should expand the diversity of the study sample.
Implications for Nursing
This study informs oncology nurses’ approach to patient care, particularly in the case of Chinese women with newly diagnosed breast cancer prior to adjuvant chemotherapy. Key areas in which nurses can make targeted and effective interventions are as follows: (a) following up with patients on any post-surgery discomfort; (b) addressing chemotherapy concerns, including important cultural concerns such as family, diet, and traditional culture (e.g., conservatism); (c) recognizing patients’ specific needs by combining subjective patient-reported outcomes with objective outcomes; (d) providing targeted health information and psychological support to help the patient smoothly transition from surgery to chemotherapy and adequately prepare for chemotherapy; and (e) informing patients on where to find support to address their health-related concerns. Ways to integrate cultural factors into supportive care interventions require future research and discussion. 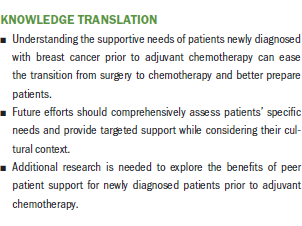
Conclusion
Patients newly diagnosed with breast cancer have specific supportive care needs prior to receiving adjuvant chemotherapy. In particular, they need support for physical symptom management, complex psychological adjustment, acquiring chemotherapy-related information, daily life guidance, and communication and surrounding support. These needs are both independent and interconnected, reflecting their complexity. Existing services do not adequately meet the prechemotherapy supportive care needs of these patients; therefore, this study may support nurses in providing supportive care interventions for newly diagnosed patients that can help to adequately prepare them for chemotherapy.
The authors gratefully acknowledge the patients and the medical care team at the First Affiliated Hospital of Dalian Medical University for their time and assistance with this study and Xiang-Yu Meng, MA, and Hui-Qing Yang, MA, who assisted in the data analysis process.
About the Author(s)
Ying-Jie Cai, MA, is a doctoral student in the Department of Gerontological Nursing at Chiba University in Japan and in the Department of Nursing at the First Affiliated Hospital of Dalian Medical University in China; Harue Masaki, PhD, RN, PHN, is a professor in the Graduate School of Nursing at Chiba University; and Tie-Ying Shi, MA, is chief of the Department of Nursing at the First Affiliated Hospital of Dalian Medical University. This study was funded by the Guangzhou Concord Medical Humanities Research and Education Foundation (201909). Cai and Shi contributed to the conceptualization and design. Cai completed the data collection. Cai and Masaki provided analysis. All authors contributed to the manuscript preparation. Shi can be reached at sty11177@163.com, with copy to ONFEditor@ons.org. (Submitted October 2020. Accepted January 6, 2021.)




