Socio-Ecological Environmental Characteristics of Young Chinese Breast Cancer Survivors
Purpose: To explore the environmental characteristics of young breast cancer survivors (YBCSs) in China.
Participants & Setting: 17 participants aged 18–45 years were recruited from hospitals and through participant referral in Shanghai, China.
Methodologic Approach: Semistructured interviews were conducted to explore the environmental characteristics of YBCSs. Content analysis was performed to analyze the data.
Findings: The following four domains emerged from the analysis: individual environment, interpersonal environment, community environment, and social environment. The YBCSs’ personal changes, relationship with family and friends, support from health workers especially peer survivors, social stigma, and other elements were relative to various environmental levels.
Implications for Nursing: The study provides insights into the specific issues of YBCSs at different environmental levels. Nurses should collaborate with the healthcare team, family members, and other stakeholders in addressing these issues to support YBCSs. Culturally tailored support should be developed to release the burden of socially desired roles and other cultural issues for Chinese YBCSs.
Jump to a section
Breast cancer is the most common cancer affecting women and the fifth-leading cause of cancer mortality among women in China (Chen et al., 2018). Approximately 416,371 women were diagnosed with breast cancer in 2020 (International Agency for Research on Cancer, 2020). The incidence rates of breast cancer continue to increase in young Chinese women aged 20 years and older, reaching a peak between ages 45 and 55 years (Chen et al., 2018), and younger than that in Western countries (Miller et al., 2019; Siegel et al., 2020).
Young breast cancer survivors (YBCSs) show dramatic changes in their ecological environments at the biologic, behavioral, and psychosocial levels. They often report more biologic symptoms, such as fatigue, cognitive problems, poor sexual function, depression, sleep disturbance, and vasomotor symptoms, than older breast cancer survivors (Accortt et al., 2015; Champion et al., 2014). The adverse effects of treatment are also different for YBCSs than for their older counterparts. Younger women (aged 20–44 years) with larger and/or more aggressive tumors are more likely to be treated with mastectomy and contralateral prophylactic mastectomy (Miller et al., 2019). In addition, various psychosocial issues may cause negative effects. Depression levels are approximately twice as high as those of older women because of mastectomy, a higher rate of secondary malignancy, poor body image, decreased sexual interest, and decreased perceived sexual attractiveness (Herbenick et al., 2008). YBCSs, particularly those who have received chemotherapy treatment, showed a significantly increased prevalence of preterm birth, low birth weight, and caesarean delivery (Anderson et al., 2017). Fertility is a major issue for child-bearing survivors. In addition to YBCSs, their partners also showed a worse quality of life than the partners of older survivors (Cohee et al., 2018; Li et al., 2016). Cohee et al. (2018) reported that younger partners had lower marital satisfaction and more hyperarousal. In addition, survivors, particularly those who were younger, faced financial hardship (Dean et al., 2018). The reappraisal of career development and role achievements is another common socioeconomic change for YBCSs (Dean et al., 2018).
An ecological approach was proposed to explore the internal and external environments of YBCSs (Greener et al., 2018; Schlüter et al., 2014). The ecological environment could be discussed not only in the individual domain but also in the interpersonal, community, and even broad social domains to obtain comprehensive, dynamic, and multi-view information on YBCSs (Dahlberg & Krug, 2002; Schlüter et al., 2014). Therefore, the understanding of ecological characteristics could support the development of a targeted and amenable intervention to reduce physical fatigue, facilitate transition readiness, and enhance the quality of life of survivors (Hiensch et al., 2020; Patel et al., 2020).
Existing research suggests that, in contrast to other breast cancer survivors, Chinese breast cancer survivors more frequently focus on cultural norms, encounter high levels of social and self-stigma, and face financial difficulties. These factors are associated with a typical survival environment and lead to a lower quality of survivorship (Chen et al., 2020; Wong et al., 2019; Xia et al., 2018). However, few studies have focused on the ecological environments of breast cancer survivors, particularly those of YBCSs in China.
According to life course theory, age is important from the perspectives of societies and individuals (Settersten, 2003). The timing of traumatic cancer may have different meanings for YBCSs than for older breast cancer survivors. For YBCSs, the provision of support and interventions according to their ecological environments can greatly reduce their level of disability and increase the rate of returning to society (World Health Organization, 2000). The quality of survivorship could be greatly improved through appropriate environmental changes.
This qualitative study aimed to explore the perceptions of YBCSs regarding the characteristics of ecological environmental factors that improve or inhibit the survivorship experience. The overall research question guiding this study was as follows: What are the characteristics of the changing environments of YBCSs that facilitate or inhibit the quality of survivorship in China?
Methods
Design
A qualitative study design was adopted for this study. The study aimed to explore the typical characteristics of the environments of YBCSs in China. The authors felt that in-depth semistructured interviews, which were used to collect and understand the lived experiences of YBCSs, would be the ideal method. The study design and findings are reported according to the Consolidated Criteria for Reporting Qualitative Research checklist (Tong et al., 2007).
Participants
A purposeful and theoretical sampling method was used to recruit women who (a) were aged 18–45 years, (b) had received a stage I–III breast cancer diagnosis, (c) had a survivorship of 6 months to 5 years, and (d) lived in Shanghai, China. The semistructured interviews were conducted, audio recorded, and transcribed. Recruitment was performed in person through telephone and WeChat. WeChat is a popular social app in China with a core function of messaging and voice chatting. Seventeen participants were recruited in this study because the themes of the prior two interviews were identified repeatedly, and no new information and themes were present in the data. Guest et al. (2006) noted that data saturation may be attained in as little as six interviews. Therefore, the authors considered that 17 YBCSs would be an adequate number of participants. All of the potential participants were informed about the study purpose and methods and then provided written consent. This study was approved by the institutional review board of the Shanghai Jiao Tong University School of Medicine.
Data Collection and Analysis
At the beginning of each interview, informed consent was obtained, and demographic information, such as age, marital status, and disease diagnosis, was collected. Next, the semistructured interview was conducted by an experienced qualitative researcher in a quiet hospital office or via WeChat. The interviews lasted from 40 to 120 minutes. Each participant was interviewed once to obtain topic-oriented information. The guidelines for the interview and the data analysis were developed according to the socio-ecological model. The model included individual, interpersonal, community, and societal levels, representing the ecological environments of an individual (Centers for Disease Control and Prevention, 2020). The individual level identifies biologic and personal history factors. Interpersonal represents the interaction between two or more people. Community indicates settings or institutions in which the social relationship occurs. Societal factors include social norms, cultural norms, health policies, economic policies, and educational policies.
The participants were asked the following semi-structured questions related to their breast cancer journey:
• Could you tell me your experience after you were diagnosed with cancer?
• What are the changes in your individual environment, interpersonal environment, community environment, and social environment?
• What changes facilitated your recovery, and what barriers did you encounter?
• Is there anything else you would like to tell me?
The interviewer encouraged participants to express their genuine feelings by actively listening without interruption or judgment. All the interviews were recorded and transcribed verbatim in Mandarin. Each respondent’s transcript was then emailed to her to ensure that the expressions and statements were accurate. The transcripts were supplemented and modified according to the feedback provided by each participant.
The method of content analysis proposed by Schuster and Weber (1986) was performed for the data analysis. First, the data were coded using a line-by-line coding process. Next, the codes were categorized, and themes reflecting the characteristics of the socio-ecological environments of the YBCSs were extracted through content analysis. Each stage was performed several times to maintain the quality and trustworthiness of the analysis. An analysis team comprised of an experienced qualitative researcher and a nurse, both with backgrounds in breast cancer and qualitative research, was formed to assist with the interpretation of the text. The two analysts performed their analyses separately. The themes were then compared and discussed until both analysts reached a consensus regarding the themes.
Findings
Interviews were conducted with 17 YBCSs. Thirteen interviews were conducted in hospital offices, and four were conducted by telephone. All of the participants were aged 25–45 years and had a mean survivorship of 1.35 years. Participant characteristics are presented in Table 1. 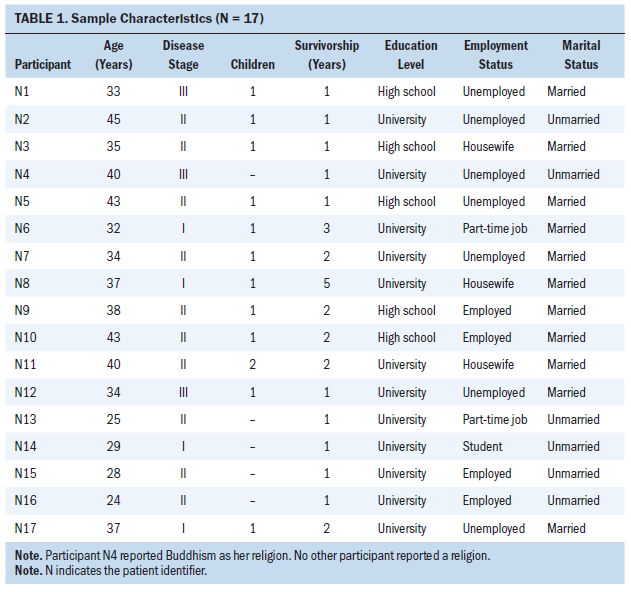
The authors developed a descriptive model of the ecological environments of YBCSs based on the current study findings. The characteristics of the environments of Chinese YBCSs were categorised into 16 themes for the individual, interpersonal, community, and societal domains through the analysis process (see Figure 1). The first domain is the individual environment, which includes biologic, behavioral, and other personal changes that may influence the quality of the survivorship of YBCSs. The second domain is the interpersonal environment, which reflects close relationships, including those with family members and other close friends, that may influence the behavior and experience of the survivors. The third domain is the community environment, which includes relationships with health workers, other breast cancer survivors, and other people in the survivors’ neighborhoods. The fourth domain is the broad societal environment, which may enhance or inhibit the quality of survivorship. The societal environment includes economic, cultural, and social factors that help to maintain, improve, or diminish the survivors’ quality of life. The major domains, themes, and supporting participant feedback are presented in Table 2. 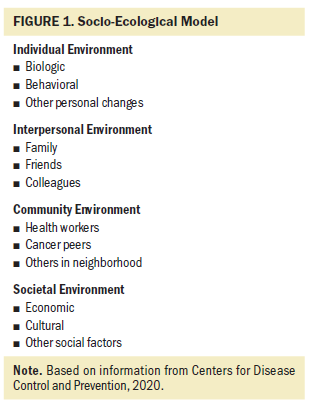
Individual Environment
Changes in attitudes from hopelessness and confusion to acceptance: Most YBCSs were in a poor emotional state and experienced difficult feelings when they were informed of their cancer diagnosis. Over time, and with increased knowledge of their cancer, the YBCSs gradually accepted the disease and could live with the vulnerability. Once they had accepted the disease, almost every survivor reconsidered life and death. Although still afraid because of their life-threatening diagnosis, they understood that negative emotions were detrimental to their health. Therefore, most of them focused on adopting a calm attitude in facing their cancer. 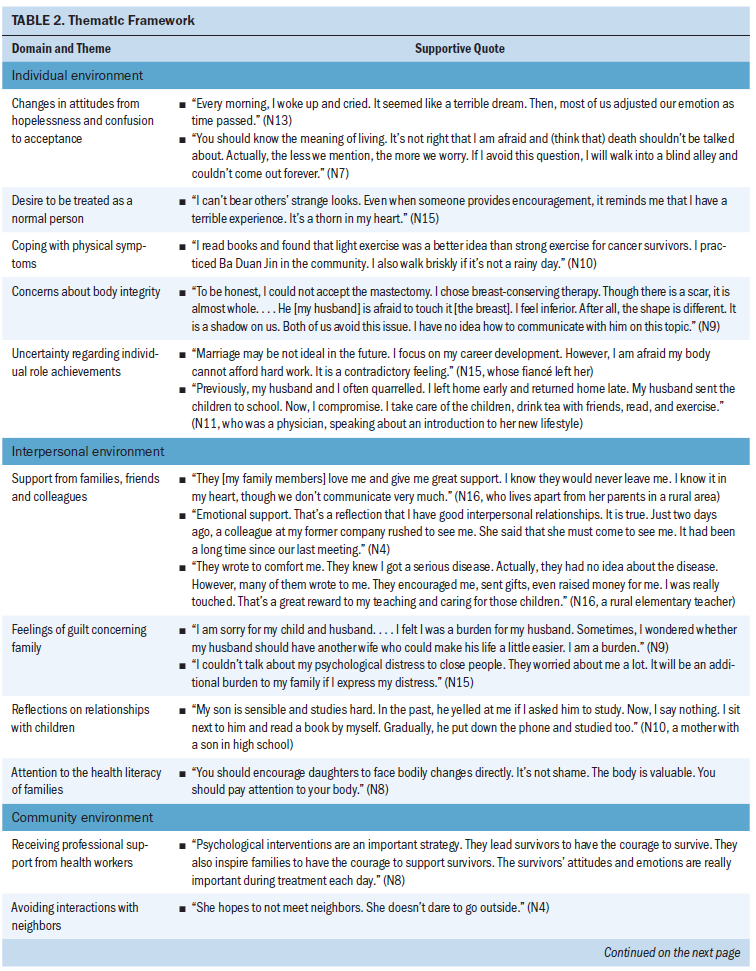
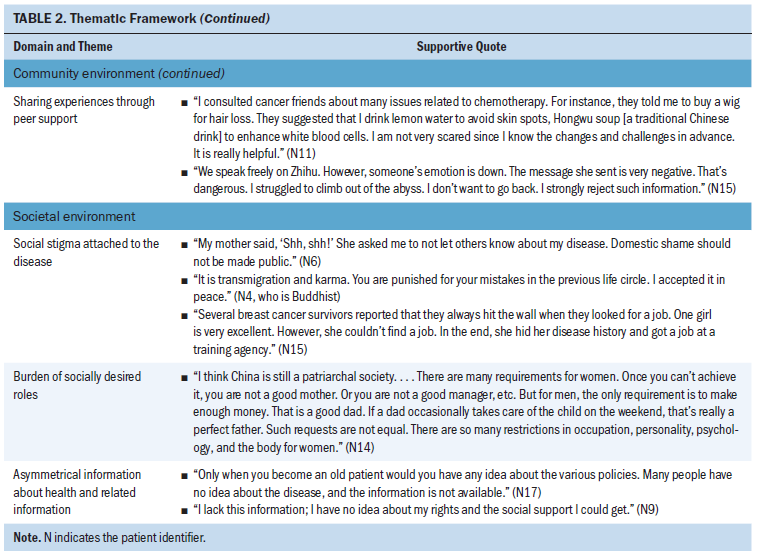
Desire to be treated as a normal person: Most survivors became very sensitive to people around them. In particular, they were sensitive to the words and looks of others and even to their offers of help and support. Although they admitted their vulnerabilities, they did not wish others to treat them as patients and disabled people and did not want to appear different from others. In some cases, the support made them embarrassed and annoyed with daily social interaction.
Coping with physical symptoms: YBCSs struggled with various side effects, including vomiting, sleep disturbance, pain, fatigue, lymphedema, and premenopausal symptoms. They exercised, meditated, and took medicine to relieve these symptoms. Traditional rehabilitation, including acupuncture, Taiji, and Chinese herbs, was a common strategy.
Concerns about body integrity: Treatment led to body changes, particularly the surgically removed breasts and hair loss from chemotherapy, leading the YBCSs to perceive that the integrity of their bodies had been disturbed. Some of the participants faced problems with sexual function and altered body image. Some experienced anxiety and depression, which they attributed to their strong concerns about their body shape.
Uncertainty regarding individual role achievements: Most of the young survivors were eager to achieve personal development. They were very concerned about their personal responsibilities as a daughter, wife, or mother. They still had hope for their marriages and careers. However, the uncertainty of their health status, particularly the recurring worry about this topic, led them to make compromises regarding various individual plans and instead focus on one area.
Interpersonal Environment
Support from families, friends, and colleagues: YBCSs received strong support from friends and colleagues, particularly family members, who showed warmth and recognition through their caring, encouragement, and listening.
Feelings of guilt concerning family: YBCSs were grateful for family support. However, they expressed feelings of guilt because of the considerable economic and psychological burden caused by the disease.
Reflections on relationships with children: Survivors significantly changed their interactions with their children, particularly how they managed their children’s education. Their children’s presence and encouragement provided substantial support. Both the survivors and their children matured considerably because of the cancer diagnosis.
Attention to the health literacy of families: The disease forced YBCSs to value health and health literacy, not only for themselves but also for their families. Some proposed that health literacy education should be provided in the early stages of children’s education.
Community Environment
Receiving professional support from health workers: Physicians and nurses were the most trusted members of the survivors’ communities. Health workers’ professional knowledge and comments encouraged survivors and increased their confidence in fighting the disease. The YBCSs followed the doctors’ recommendations and consulted the doctors first when they confronted issues. Many survivors expressed their great need for support from psychologists.
Avoiding interactions with neighbors: YBCSs were open to each other but were not willing to divulge their health information to those around them, particularly neighbors. They worried that the neighbors would discuss their disease and spread information in the community. Some YBCSs even isolated themselves so that they would not have contact with their neighbors.
Sharing experiences through peer support: Because the times of doctor consultation and nursing follow-up were limited, YBCSs considered peer support as an important way to obtain information about the disease and body changes, as well as to gain emotional support. YBCSs shared disease management experiences and even personal interests with each other through WeChat and Zhihu (a Chinese social media platform). Social media constituted an efficient, resourceful, and effective means of peer support. However, it was also associated with some side effects, particularly regarding the YBCSs’ emotions.
Societal Environment
Social stigma attached to the disease: Both survivors and family members were affected by the stigma of breast cancer. Soon after their diagnosis, survivors and family members were reluctant to talk about the disease. Karma was mentioned frequently during self-reflection. Religious beliefs became spiritual comfort for some survivors. Notably, the stigma against individuals with cancer made it difficult for YBCSs to find an ideal job and return to society. YBCSs complained of a lack of belonging and identity.
Burden of socially desired roles: YBCSs experienced the stressors of fulfilling multiple roles, including daughter, mother, wife, and employee. Young women struggled to constantly balance family and work or study. The cancer diagnosis made them feel powerless in managing their various roles.
Asymmetrical information about health and related information: Asymmetrical information was a common issue reported by YBCSs. They had low health literacy, particularly concerning prevention, self-examination, breast cancer awareness, and medical treatment procedures. Although information on these topics is published in many government and hospital media, they did not know how to access it. In addition, they had little knowledge of public health insurance, resulting in their inability to submit reimbursement applications.
Discussion
YBCSs encounter unique environmental issues in different ecological systems. Their special needs related to different environments should be recognised to enhance the quality of survivorship.
YBCSs struggle with various changes in their individual environment, including poor body image, pain, sleep disturbance, and other side effects of aggressive treatment (Hubbeling et al., 2018). Their decreased health leads to the loss of social identity, such as their identities as employees, girlfriends, and students, making them more likely to experience higher anxiety and depression than older adult breast cancer survivors (Nolan et al., 2018). Consistent with a previous study, most Chinese YBCSs in this study engaged in alternative treatments and traditional exercises to combat these symptoms (Hu et al., 2020). In addition, the uncertainty of the disease had a serious impact on their personal planning and future development (Henneghan et al., 2018). The participants all focused on their families, with some participants stopping activities such as education, marital activities, and career development during their treatment. However, they never abandoned their roles as mothers. Some even focused on taking care of children during their rehabilitation at home.
One prominent finding regarding the individual environment is that the survivors were eager to be treated as normal individuals. The authors attributed this finding to several factors. First, individuals with a collectivistic orientation, which is common in China, value in-group and interdependence with consistency and commonality (To et al., 2020). They dislike receiving encouragement from others because they perceive it as a signal of being alien and a member of an outgroup. Therefore, YBCSs are afraid and nervous to receive such encouragement. Second, in contrast to their older counterparts, YBCSs still maintain a hope of fulfilling various roles because of a longer natural life span. Gradually, they accept the uncertainty associated with the disease and learn to enjoy life, work, or study (Chen et al., 2017). However, encouragement seems to be a reminder that increases awareness of the disease’s presence and can create embarrassment for survivors (Chen et al., 2020). In addition, emotional suppression is encouraged in collectivistic culture (Yeung et al., 2020). YBCSs seldom express feelings of stress and share personal concerns, such as being a normal person, because they believe that expression is a sign of weakness and an impolite response that interrupts harmonious relationships. Future interventions should reduce the barriers of expression to enable them to share their concerns.
Regarding the interpersonal environment, YBCSs significantly value financial and emotional support from partners, parents, and extended family members (Wang et al., 2020). However, Chinese culture encourages emotional suppression to protect interpersonal harmony; therefore, it is common to suppress personal stress within the YBCS population (Lu et al., 2018). Many YBCSs are more likely to suppress their emotions rather than vocalize them, and some survivors even express feelings of guilt related to partners and other family members. Therefore, friends and close colleagues become helpful people with whom YBCSs can discuss their fear, anxiety, and symptoms during their cancer journeys.
A healthy parent–child relationship is beneficial for YBCSs. Most children of YBCSs are in the educational stage, and it is common for Chinese mothers to considerably value their children’s academic achievement. In collectivistic and high-power/distance cultures, the status differential of parents and children is emphasised. Therefore, Chinese parent and child closeness is lower, and conflicts occur more frequently than in families in the United States (Guan & Li, 2017). YBCSs are more prone to self-reflection and posttraumatic growth than older survivors (Manne et al., 2004). Therefore, their cognitive development may change family communication patterns, creating a positive effect on family ecology. In addition, the effect may intensify their cognitive development and facilitate harmonious relationships with their children, factors that improve mental status and quality of survivorship.
Regarding community environment, the positive roles of professional and peer support in YBCS survivorship are widely recognised (Hu et al., 2019). YBCSs tend to discuss their disease, treatment, and emotions via social media, such as on WeChat and Zhihu. They can easily state their concerns with other cancer survivors on social media. Most of them understand digital literature and can navigate online media (Lepore et al., 2019). They can discuss their disease in a more relaxed manner with strangers than familiar people. In addition, writing is a more comfortable medium through which to precisely express their feelings than face-to-face conversation. However, the negative stories and tendency to dwell about cancer in these settings are potential barriers to using online peer support (Legg et al., 2019).
Concerning the societal environment, YBCSs face role conflicts and treatment adoption difficulties because of the traditional image of the wife role. In addition, the inefficient access to health insurance and social support information creates difficulties. Furthermore, self-stigma is a common concern for YBCSs and is negatively associated with survivorship because it may lead to either increased negative thoughts or reduced positive thoughts (Wong et al., 2019). YBCSs learn disease knowledge and information more quickly than older adult survivors because of their greater social media competence and learning ability. However, traditional cultural values related to karma and fatalism still have subtle effects on some YBCSs. Some survivors believe that cancer is inevitable because it represents punishment for bad deeds in the last circle of life. Different cognitions intertwine and influence YBCSs, causing a constant struggle. Those negative cognitions may harm the quality of life among YBCSs and hinder their posttraumatic growth (Wong et al., 2019). In some cases, cultural beliefs may be a solution for their disease, helping survivors to acquire peace of mind. In addition, job hunting failure caused by the common societal stigma and the sense of shame surrounding expressions related to secondary sexual characteristics increase self-stigma among YBCSs.
Limitations
The generalization of these findings may be limited because of the participant characteristics. All participants were recruited in Shanghai, which is a well-developed, modern city in China with an advanced economy, as well as advanced education and medical services. Therefore, these environmental characteristics may not represent the diverse ecological system of YBCSs from different areas of China. Second, the participants may show age-related differences. The characteristics of participants in their 20s, 30s, and 40s should be explored in future studies. Third, there is survival bias inherent in interviewing only women without recurrence within five years of survivorship, and the current results do not describe the experiences of women who may experience recurrence and have long-term treatment needs after the five-year treatment period. Finally, interviews of health practitioners and family members are warranted to verify and enrich the findings with multiple perspectives. 
Implications for Nursing
The current findings support the need for nurses to understand YBCSs’ situation across the internal and external environments. The study indicates that nurses should maintain cultural sensitivity to the different issues and related needs of this specific population from a broad and feministic perspective. Nurses could collaborate with cancer survivors, other health professionals, family members, friends, and multiple stakeholders to develop a supportive environment for YBCSs. They could support YBCSs, particularly those with poor social well-being, in obtaining more social and personal resources to promote short-term and long-term quality of life for YBCSs and their families.
Conclusion
The authors’ research findings reveal the specific environmental issues of young Chinese breast cancer survivors at the individual, interpersonal, community, and societal environmental levels. In the future, nurses should focus on addressing the different needs of YBCSs and how to support them by reducing their level of disability and improving their broad ecological environments for this specific life course. YBCSs can then be inspired and confident to write new life stories after their cancer trauma.
The authors gratefully acknowledge the participants for taking part in the study.
About the Author(s)
Yun Hu, RN, PhD, is an associate professor in the School of Nursing, Jiehui Xu, MSN, is a nurse manager at Renji Hospital in the School of Medicine, Xiyi Wang, RN, PhD, is an assistant professor in the School of Nursing, and Yiwen Shi, RN, BS, is a nurse at Xin Hua Hospital in the School of Medicine, all at Shanghai Jiao Tong University in China; Menjie Chen, BS, is a master’s student in the School of Medicine at Jiangnan University in Wuxi, China; and Eun-Ok Im, PhD, MPH, RN, CNS, FAAN, is a professor in the Nell Hodgson Woodruff School of Nursing at Emory University in Atlanta, GA. This work was supported by the National Natural Science Foundation of China (No. 71804112) and the Construction of Plateau Discipline-Nursing (No. Hlgy1826kygg). Hu, Xu, and Im contributed to the conceptualization and design. Hu, Xu, Shi, and Chen completed the data collection. Hu, Xu, and Shi provided statistical support. Hu, Xu, Wang, and Chen provided the analysis. Hu, Xu, Wang, Chen, and Im contributed to the manuscript preparation. Hu can be reached at huyunsy@shsmu.edu.cn, with copy to ONFEditor@ons.org. (Submitted January 2021. Accepted March 20, 2021.)

