Update to 2019–2022 ONS Research Agenda: Rapid Review to Promote Equity in Oncology Healthcare Access and Workforce Development
Purpose: The Oncology Nursing Society (ONS) tasked a rapid response research team (RRRT) to develop priorities to increase diversity, equity, and inclusivity in oncology clinical care and workforce development.
Methods: An RRRT of experts in health disparities conducted a rapid review of the literature, consulted with oncology nurse leaders and disparities researchers, and reviewed priorities from funding agencies.
Results: Significant gaps in the current oncology disparities literature were identified and used to inform priority areas for future research practice and workforce development in oncology nursing.
Synthesis: This is the second article in a two-part series that presents findings on structural racism and health inequities in oncology nursing. In the first article, three priority areas for oncology nursing research were presented. In this article, strategies to improve diversity, equity, and inclusivity in clinical practice and the oncology workforce are described.
Implications for Research: Recommendations are presented to inform research, clinical, administrative, and academic oncology nursing settings on increasing diversity, equity, and inclusivity and deconstructing structural racism.
Jump to a section
This is the second article in a two-part series that presents results from a rapid review about structural racism and health inequities in oncology nursing research. The first article presents recommendations for oncology nursing research (Jones et al., 2021). This article discusses structural racism and the inequities within nursing education, the nursing workforce, and the delivery of oncology nursing care.
Background
The influence of structural racism is evident in the development of nursing education and the nursing profession, which has a long history of racism and segregation. Black nurses faced two significant obstacles in the 1860s. Black nurses were working to claim their new place in society following the Emancipation Proclamation. In addition, the role of nurses was not yet respected, and they were instead seen as subservient handmaidens (Kalisch & Kalisch, 1995). The profession of nursing is rooted in structural racism because it developed during the time of racial segregation and the legal doctrine of separate but equal. Black nurses were primarily trained in Black colleges and took care of patients in Black hospitals or segregated sections of prominently White hospitals, all of which lacked equal resources. The first school for Black nurses was established by the Provident Hospital in Chicago, Illinois, in 1891. The National Association of Colored Graduate Nurses (NACGN) was founded in 1908 and was comprised of 1,200 members by the 1940s (Vaughan, 1997). In the 1940s, Black nurses were trained in 32 all-Black schools and 14 desegregated schools, and they fought for the opportunity to serve in the U.S. Army (Hine, 1982). In 1951, the NACGN and American Nurses Association (ANA) merged. However, Mabel Staupers, RN, the executive director of NACGN at the time, voiced concerns about the integration experience and cited it as tokenism (Vaughan, 1997). At the time of the integration, Black nurses were not allowed to hold office in ANA. Subsequently, the National Black Nurses Association was established in 1971 and continues today. The impact of early nursing education segregation and disparities is still evident; only 19.9% of RNs self-identify as members of underrepresented racial and ethnic groups despite about 39.3% of the U.S. population being comprised of individuals from these groups (Smiley et al., 2018; U.S. Census Bureau, 2019).
Methods
Methods are detailed in the first article in this two-part series (Jones et al., 2021). Briefly, a rapid response research team (RRRT) of experts in the areas of cancer disparities, equity, oncology research, and leadership was convened by the Oncology Nursing Society (ONS) in June 2020 to update the 2019–2022 ONS Research Agenda (Von Ah et al., 2019). Guided by critical race theory (CRT), the RRRT discussed the nature of racism in nursing, oncology, and ordinary life in the past and present, as well as their personal race consciousness. The RRRT also conducted a rapid literature review (Hamel et al., 2021) in which more than 200 publications were synthesized to identify research gaps in oncology nursing research related to racism and health inequities. Informed by these identified gaps, as well as input from funding agencies, a COVID-19 RRRT (Zanville et al., 2021), the ONS Board of Directors, and ONS membership and leadership, priorities were developed for future oncology nursing research, practice, education, and workforce development.
Results
Key Concepts
In the first article in this two-part series, a detailed justification is provided for the authors’ use of terms related to race and ethnicity, as well as a discussion of race, racism, and cancer disparities (Jones et al., 2021). The authors’ use of terms related to race and ethnicity is thoughtfully selected and intentional. Broad and consistent terms are not used for convenience; rather, every effort is made to use specific terminology to accurately describe people the authors are referencing. The authors respect that some readers will prefer different uses of terms, and the authors commit to continuous attention to the ever-changing meaning, power, and respectful usage of words.
Identified Gaps and Needs Related to Equity in Oncology Nursing Practice and Workforce Development
The literature reveals significant disparities between the racial and ethnic makeup of the United States as compared to the nursing workforce and the implications that this has on the health of individuals. For example, the 2017 National Nursing Workforce Survey reported that the racial and ethnic makeup of the RN workforce is 80.8% White, 7.5% Asian, 6.2% Black, 5.3% Hispanic, and 0.4% American Indian (Smiley et al., 2018), whereas the racial and ethnic makeup of the United States is 60.1% White, 18.5% Hispanic, 13.4% Black, 5.9% Asian, and 1.3% American Indian (U.S. Census Bureau, 2019). These data point to a particular need to increase the number of Black, Hispanic, and American Indian nurses in the United States. Similar disparities are also evident in academia at large by a significant funding gap between Black/African American and White scientists. According to a National Institutes of Health (NIH, 2021) scientific workforce report, about 2% of NIH R01 grants were awarded to Black scientists. In addition, less than 13% of nursing faculty are people of color (Hamilton & Haozous, 2017).
Although racial and ethnic diversity is needed in the nursing workforce, the literature identifies numerous barriers for individuals of color in undergraduate and graduate education. For example, racially and ethnically underrepresented faculty report a lack of purposeful mentorship regarding cultural capital (e.g., style of speech and dress that is valued and promotes mobility within academia), informal rules, professional socialization, expectations for promotion, and access to social networks (Zambrana, 2018), all of which are hindrances to academic success and career advancement (Boyd et al., 2010).
The American Association of Colleges of Nursing (AACN, 2021) reported that 11% of students who graduated from baccalaureate nursing programs in 2020 identified as Black/African American. The AACN also noted that, during the past 10 years, overall diversity in baccalaureate programs increased slightly; however, the percentage (9.2%) of Black/African American graduates in entry-level nursing baccalaureate programs was stagnant, and Black/African American students who graduated from RN-to-baccalaureate nursing programs decreased by about 2%. Considering the lack of nursing faculty of color in academic institutions, AACN (2017, 2021) has noted that this may affect the number of students of color who enroll in and graduate from schools of nursing. This would, in turn, not only affect the number of nurses of color entering the nursing workforce, with fewer nurses to choose oncology nursing, but also create fewer nurses of color entering academic roles.
Racial and ethnically underrepresented doctoral students report insufficient mentorship (Farmbry, 2007). However, when mentored, students of color demonstrate increases in GPA, completion of programs, self-efficacy, and clarity on academic goals (Tsui, 2007; Zambrana et al., 2015). Unfortunately, mentorship is often a symbolic form of change that can mask authentic social change at the institutional level (Zambrana, 2018). For example, racially and ethnically underrepresented faculty report negative experiences with well-intentioned faculty when institutional values, attitudes, and resources are not also addressed (Zambrana, 2018). There are few mentorship opportunities, such as the National Research Mentoring Network (NRMN, 2021) from NIH, that focus on the development of scientists who are from racial and ethnic groups that are underrepresented in science. Mentorship barriers for racially and ethnically underrepresented scientists in academia have been identified as lack of representation among faculty, excessive work demands, time constraints, and majority culture faculty having little interest in diversity (Diggs et al., 2009; Zambrana, 2018). However, mentorship that is built on trust, as well as training about overt and covert racism, unconscious bias, and diverse backgrounds and experiences, can lead to successful mentorship of racially and ethnically underrepresented scientists in academia (Diggs et al., 2009; Zambrana, 2018). In 2021, the American Academy of Nursing recognized the importance of nurses understanding the impact of structural racism by calling for inclusion of CRT in nursing education. CRT recognizes that racism is deeply embedded in society and that an understanding of the structures and systems that support racism is needed to deconstruct structural racism and improve the lives and health of those who are hurt by it (Delgado & Stefancic, 2017). It is critical that White nursing faculty and students be educated on harm caused by structural racism, as well as mitigation strategies that they can support for their students and colleagues of color (Diggs et al., 2009). For example, White nursing faculty and students should be able to identify and intervene to prevent microaggressions (i.e., subtle, frequently occurring, and often unintentional racial insults) (Williams et al., 2020).
Faculty of color also report feeling marginalized, tokenized, underappreciated, unsupported, and not mentored sufficiently (DeWitty & Murray, 2020). For example, only 37% of African American and 36% of Mexican American faculty report being mentored by someone of their same race/ethnicity (Zambrana, 2018). Underrepresentation of racially and ethnically diverse faculty often leads to faculty of color experiencing what has been called a time tax, which has negative effects on productivity and well-being (Gewin, 2020; Zambrana, 2018). Time tax refers to the extra service that faculty of color are asked to do as they are tokenized to increase diversity on multiple committees, looked to for leading and informing diversity and inclusion efforts, and asked to mentor too many faculty and students of color, all while managing their own feelings of aloneness and tokenism (Gewin, 2020; Zambrana, 2018). Coinciding with this, mentees report observing the burnout of racially and ethnically underrepresented faculty and that these faculty members are excluded from the institutional power-broker network (Zambrana, 2018).
The literature identifies that racism, discrimination, and exclusivity underpin disparities within all aspects of healthcare delivery (Gkiouleka et al., 2018; Krieger, 2012; Williams et al., 2019). Individuals of color are more likely to be hospitalized and die from a late diagnosis of cancer and have worse symptom burden, partly because of socioeconomic factors (e.g., income, geographic location, access to food and technology) and underlying health conditions (Alcaraz et al., 2020). Oncology nurses are called upon daily to address these complex health and social issues and the impact of racism that is often not fully understood and frequently goes unnoticed. Initiatives are needed to prepare the oncology nursing workforce to provide equitable care to patients who experience health disparities by understanding and intervening on the effects of systemic racism.
Based on these results, two priority areas of focus to improve equity in the oncology nursing workforce and delivery of equitable oncology nursing care are presented. Specific recommendations to support each area are also provided.
Priority Area 1: Identify Effective Strategies to Increase Racial and Ethnic Diversity and Inclusion in Academia and the Oncology Nursing Workforce
Recommendation 1: Initiate Advocacy Efforts and Programs to Increase Awareness of and Eliminate Structural Racism
An understanding of the multifaceted systems and operations of discrimination in education and healthcare practice and policy is needed (Williams et al., 2019). To this end, implementing and evaluating systems and the policies that facilitate discussion and understanding of microaggressions and overtly racist acts from patients and colleagues are critical. These understandings are necessary to create inclusive environments that will increase diversity in the profession, address the mental health of nurses of color, and improve the overall work environment. Deans and directors of schools of nursing must commit to actively recruiting, retaining, and supporting faculty, staff, and students of color; providing an environment of inclusivity; and establishing formal mentoring initiatives (Thompson, 2021). In addition, efforts are needed to evaluate how systemic barriers and a lack of mentors of color may affect advancement to graduate education and executive leadership positions. Examples of programs that nursing schools can implement and evaluate to increase understanding about racism include the Academics for Black Survival and Wellness (2020) initiative and various trainings offered by the Racial Equity Institute (n.d.).
Recommendation 2: Improve Mentorship for Racially and Ethnically Underrepresented Nurses
Effective mentorship is needed throughout the nursing education pipeline—from recruiting young individuals of color into undergraduate nursing programs through undergraduate and graduate education to focusing on mentorship for PhD-prepared nurse scientists (American Academy of Nursing, 2021). First, a foundational examination of how geography and access lead to fewer individuals of color pursuing and being accepted into nursing education at the undergraduate level is needed. Findings from this examination may inform the development of effective early mentorship models that begin before matriculation into nursing school. Equitable, diverse, and inclusive nurse scientist learning environments may be created by following recommendations of the annual report from the Josiah Macy Jr. Foundation (2020). Of note, outcomes of mentorship programs for underrepresented pre- and postdoctoral students, as well as research faculty, need to be evaluated. Examples of programs that can be implemented and evaluated include Project Uplift at the University of North Carolina, which provides early mentorship to diverse and underrepresented high school students (University of North Carolina Office for Diversity and Inclusion, 2020) and the Winston-Salem State University and Duke University Bridge to the Doctorate Program that provides a multitude of structured mentored research experiences focused on preparation for successful application to a nursing PhD program for students enrolled in a nursing program at a historically Black college or university (Brandon et al., 2014). In addition, schools can encourage and provide protected time for racially and ethnically underrepresented students and faculty to have mentoring outside of their respective institutions. Examples of this include the NRMH program offered by the NIH and the Diversity Institute for Emerging Leaders offered by the Society of Behavioral Medicine. Finally, nursing schools can partner with various organizations to improve mentorship for nurses of color, such as the Asian American/Pacific Islander Nurses Association, Black Nurses Rock, National Alaska Native American Indian Nurses Association, National Association of Hispanic Nurses, National Association of Indian Nurses of America, National Black Nurses Association, National Coalition of Ethnic Minority Nurse Associations, National Indian Nurse Practitioners Association of America, American Association for Men in Nursing, and Philippine Nurses Association of America.
Recommendation 3: Implementation and Evaluation of Leadership Development Programs for Racially and Ethnically Underrepresented Nurse Scientists
Efforts are needed to assess and consider structures and systems that support career development and leadership progression among nurses of color. Nursing schools and organizations should consider the effects of extra professional services (e.g., being asked to serve as a representative for people of color on numerous committees or workgroups, as a grant reviewer, as part of association leadership, and in mentoring or precepting of numerous students of color) on the mental health and professional progression of racially and ethnically underrepresented faculty (Gewin, 2020). Systems should be put in place to increase the pipeline of PhD-prepared nurses and nurse leaders of color that will also prevent overburden of current faculty and nurse leaders of color. Systems should be implemented to support professional progressions of racially and ethnically underrepresented faculty to deans and senior executive positions in healthcare and professional associations.
Priority Area 2: Promote Health Equity in Oncology Health Care
Recommendation 1: Implement Initiatives to Improve Access to Cancer Care
This recommendation relates to the research priority of increasing access through telehealth and technology in the 2019–2022 ONS Research Agenda (Von Ah et al., 2019). The multilevel barriers faced by individuals from underserved and historically marginalized groups in the healthcare system must be addressed in clinical practice. Specifically, the National Institute on Minority Health and Health Disparities Research Framework specifies that, within the healthcare system, patients face barriers at four levels: individual, interpersonal, community, and societal (Palmer et al., 2019) (see Figure 1). Evidence-based interventions that target these obstacles at each of these levels for prevention, early detection and treatment, survivorship, and rehabilitation should be implemented and evaluated. 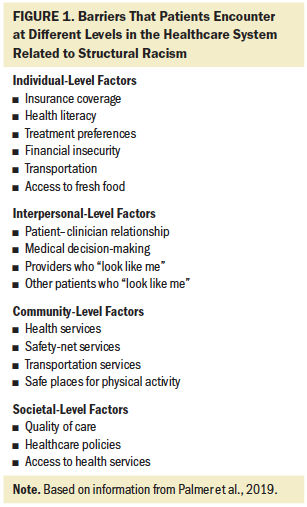
In some instances, technology may be leveraged to address cancer care inequities. Telehealth and other eHealth outreach initiatives must carefully consider health literacy, technology literacy, and internet access, because literacy is a significant contributor to screening, treatment, and communication in cancer care (National Cancer Institute, 2020). With the rise of telehealth, it is also important to develop understandings of patients’ computer, internet, and cellular access and use. Prior research has demonstrated that Americans with annual incomes of less than $30,000, who have an education level of a high school diploma or less, and/or are people of color use computers less frequently as compared to those with annual incomes of more than $50,000, who have at least some college education, and/or are White. The gaps decline between people of color and White Americans at higher income levels (Brodie et al., 2020). Although an understanding of the ability of patients to afford and access high-speed internet is critical to optimize and equalize access to quality cancer care, it is imperative that nurses never consider race or ethnicity as a proxy for socioeconomic status.
Culturally tailored and targeted communication is important to help increase trust and encourage engagement in health and cancer care services (e.g., cancer screenings, genetic counseling, vaccines) among patients from communities that have been historically underserved, as well as to promote participation in clinical trials (Chou et al., 2020; Kfir et al., 2020; Lucas et al., 2018). A contributing factor in healthcare disparities is the lack of cultural sensitivity engagement between patients and healthcare providers (Anderson et al., 2003; Brooks et al., 2019). When working with patients, nurses must remain cognizant of the heterogeneity in culture that often exists within one race and tailor communication at the individual level to build trust and facilitate effective communication with patients (Lucas et al., 2018).
Recommendation 2: Improve Equity in Cancer Symptom Management
Disparities in symptom burden and symptom management have been identified between different racial and ethnic groups. Disparities in the assessment and treatment of pain between African American patients and White patients are especially harmful and require intervention (Lucas, 2018; Rahavard et al., 2017; Walker Taylor et al., 2018). Barriers to pain treatment and reported pain severity have been shown to vary between different ethnic groups, in part because of factors such as ineffective communication and insufficient assessments (Kwok & Bhuvanakrishna, 2014). Initiatives are needed to improve symptom management among Black survivors of breast cancer (Samuel et al., 2018). Nurse should increase initiatives to implement evidence-based guidelines to promote effective cancer symptom management (e.g., for pain management, depression, or fatigue) for patients of color. 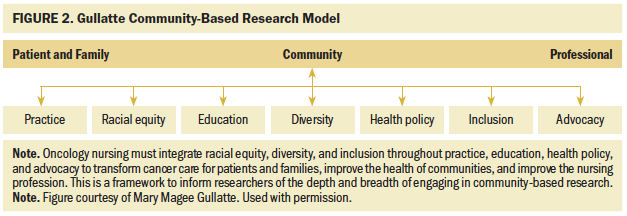
Recommendation 3: Develop an Understanding of the Effects of Racism on Cancer Outcomes
To provide high-quality and sensitive care to patients of color, it is imperative that nurses understand the historic and current effects that racism has on physical and mental health (American Academy of Nursing, 2021). For example, allostatic load theory has explained that constant stress resulting from living in systems of racism affects physiologic responses (e.g., increased cortisol, decreased telomere length) (Carlson & Chamberlain, 2005). It has been noted that the allostatic load related to structural racism severely affects the health of Black and Latinx patients (Langellier et al., 2021). Stress responses such as these have been linked to tumor progression (Moreno-Smith et al., 2010; Xing et al., 2020) and symptom severity (Andreotti et al., 2015). Nurses should work to better understand and consider how time and geographic location may affect cancer and experiences of patients (DeBord et al., 2016). In addition, while society works to reverse and end structural racism, people experiencing stress may benefit from effective strategies to mitigate the effects of racism. For example, nurses can support patients to identify and engage in self-care activities to mitigate the negative effects of stress. 
Conclusion
Outcomes related to the priorities presented in this article may lead to health equity in oncology nursing and patient care by improving representation of nurses of color in the field and providing equitable care to patients affected by racism. Nursing education can be strengthened by an infusion of PhD-prepared oncology nurses of color who are leaders and are supported by purposeful mentoring programs in higher education that are designed to develop and sustain a pipeline of future diverse nurses and nurse scientists. All oncology nurses can be informed and empowered to partner with diverse nursing organizations to advocate for sustained, concrete action plans.
Through implementation of the priorities within this article, combined with research priorities presented in the first article in this two-part series (Jones et al., 2021), oncology nurses can be advocates for equity in nursing practice, education, and health policy and advocate for patients with cancer and oncology professionals, as depicted in the Gullatte Community-Based Research Model (see Figure 2). This model highlights that diversity, equity, and inclusion support oncology nursing practice, education, healthcare policy, and advocacy to ultimately support the health of all patients, families, communities, and nurses. By synthesizing, implementing, and disseminating outcomes derived from the ONS proposed research priorities (Jones et al., 2021) and the priorities for nursing education and practice within this article, oncology nurses will be well positioned to inform policymakers and the general public about the nature and extent of racial and social inequities in health; partner with other nursing organizations to influence health policy and practice at local, state, national, and international levels; build community partnerships to advance health equity; and sustain healthier communities.
About the Author(s)
Randy A. Jones, PhD, RN, FAAN, is a professor in the School of Nursing at the University of Virginia (UVA) and the assistant director of community outreach and engagement at the UVA Emily Couric Cancer Center, both in Charlottesville; Rachel Hirschey, PhD, RN, is an assistant professor in the School of Nursing at the University of North Carolina at Chapel Hill and an associate member of the Lineberger Comprehensive Cancer Center in Durham, NC; Grace Campbell, PhD, MSW, RN, CNL, CRRN, FARN, is an assistant professor in the School of Nursing at Duquesne University and an adjunct assistant professor in the Department of Obstetrics, Gynecology, and Reproductive Sciences in the School of Medicine at the University of Pittsburgh, both in Pittsburgh, PA; Mary E. Cooley, PhD, RN, FAAN, is a lecturer in psychiatry at Harvard Medical School and a nurse scientist in Nursing and Patient Care at the Dana-Farber Cancer Institute, both in Boston, MA; Robin Lally, PhD, RN, AOCN®, FAAN, is the interim associate dean for research and the Bertha L. Pankratz Professor of Nursing in the College of Nursing at the University of Nebraska Medical Center and a member at the Fred and Pamela Buffett Cancer Center, both in Omaha, NE; Darryl Somayaji, PhD, MSN, CNS, CCRC, is an assistant professor in the School of Nursing at the University at Buffalo and an adjunct assistant professor of oncology at Roswell Park Comprehensive Cancer Center, both in Buffalo, NY; Erik K. Rueter, PMP, PMI-ACP, was, at the time of this writing, a project manager at the Oncology Nursing Society in Pittsburgh, PA; and Mary Magee Gullatte, PhD, RN, ANP-BC, AOCN®, LSSYB, FAAN, is the corporate director of nursing evidence-based practice and research at Emory Healthcare and an adjunct faculty member at the Nell Hodgson Woodruff School of Nursing at Emory University, both in Atlanta, GA. Jones and Hirschey are dual first authors. Rueter and Gullatte are dual senior authors. This review was funded, in part, by a grant from the National Institute on Minority Health and Health Disparities (1K23MD015719-01; principal investigator: Hirschey). Jones, Hirschey, Campbell, Cooley, Somayaji, Rueter, and Gullatte contributed to the conceptualization and design. Jones, Hirschey, Campbell, Cooley, Lally, and Somayaji completed the data collection. Hirschey, Campbell, Somayaji, and Rueter provided the analysis. All authors contributed to the manuscript preparation. Hirschey can be reached at hirschey@unc.edu, with copy to ONFEditor@ons.org. (Submitted February 2021. Accepted June 28, 2021.)

