Central Line–Associated Bloodstream Infection Prevention: Standardizing Practice Focused on Evidence-Based Guidelines
Central venous access devices (CVADs) are integral to the treatment and provision of supportive care for many patients with cancer. Central venous catheters are the most frequent cause of healthcare-associated bloodstream infections. Healthcare-associated bloodstream infections can be prevented when evidence-based practices are followed consistently over time. Establishing nursing best practice with CVADs in the ambulatory setting presents additional challenges because of multiple providers, caregivers, and policies. This article identifies evidence-based practice strategies implemented at a comprehensive ambulatory cancer center to standardize best nursing practice for central lines.
At a Glance
- Central line care must reflect knowledge of risk factors associated with central line–associated bloodstream infection.
- Central line care must be guided by credible evidence-based standards that focus on central line–associated bloodstream infection prevention.
- Standardizing port access and dressing practice by implementing evidence-based policies are associated with measurable improvement in patient outcomes.
Jump to a section
Central line–associated bloodstream infection (CLABSI) can cause significant avoidable morbidity and mortality (O’Grady et al., 2011). The Institute for Healthcare Improvement (IHI) introduced central line care bundles in 2001, which have demonstrated a 58% reduction in CLABSIs as a result (Centers for Disease Control and Prevention [CDC], 2011a; Umscheid et al., 2011). These improvements have occurred in the intensive care unit and acute care setting; research suggests that millions of patients outside the intensive care and acute care settings are at risk of developing CLABSIs (Chopra, Krein, Olmstead, Safdar, & Saint, 2013). This shift is relevant to the ambulatory setting because multiple patient care teams and caregivers and the absence of comprehensive surveillance methods are substantial obstacles to CLABSI prevention. Minimal research exists on measures to prevent CLABSIs in the ambulatory setting (Mollee et al., 2011; Tomlinson et al., 2011). Patients with cancer are at higher risk because of neutropenia, which has been identified by the IHI as a key risk factor for CLABSIs. Neutropenia is a common side effect of cancer treatment, with most treatments being provided in the outpatient setting (Chopra et al., 2013; Loveday et al., 2011; Schiffer et al., 2013). Central line care must reflect knowledge of risk factors and be guided by credible evidence-based standards that focus on the goal of preventing CLABSIs (Camp-Sorrell, 2011).
In 2011, the Dana-Farber Cancer Institute (DFCI), a National Cancer Institute–designated comprehensive cancer center, opened a cancer center with a centralized laboratory service unit for patient blood draws and venous access. The new unit was staffed by IV nurses and phlebotomists. An average of 300 patients per day were seen for blood draw and access by the IV team, and about 50% of those patients required port access. The opening of the laboratory service center integrated nursing staff with IV expertise from a variety of disease center units and institutions. Questions began to arise from staff about best practice as they observed and discussed individual practice. The practice variance was most evident in port access. Patients noticed this variance and were concerned that nurses did not follow the same routine. Patient interviews revealed dissatisfaction with the variance and expected consistency in the central line practices of the staff (Weingart, Hsieh, Lane, & Cleary, 2014).
Practices Associated With Prevention
The key advances from the science of CLABSI prevention focus on the following high-risk factors: heavy microbial colonization at the insertion site, heavy microbial colonization at the catheter hub, presence of neutropenia, and inadequate care of the central venous catheter after insertion (Chopra et al., 2013). The CDC (2011b) guideline bundle for postinsertion care of central lines emphasizes (a) compliance with hand hygiene requirements, (b) scrub of the access port or hub immediately prior to each use with an appropriate antiseptic, (c) accessing catheters only with sterile devices, (d) replacing wet or soiled dressings, and (e) performing dressing changes under aseptic technique using clean or sterile gloves (O’Grady et al., 2011). The literature and guidelines are in consensus that maintaining aseptic technique for care of port access devices is essential for preventing CLABSIs (Alexander, 2011; Camp-Sorrell, 2011; O’Grady et al., 2011) (see Table 1). 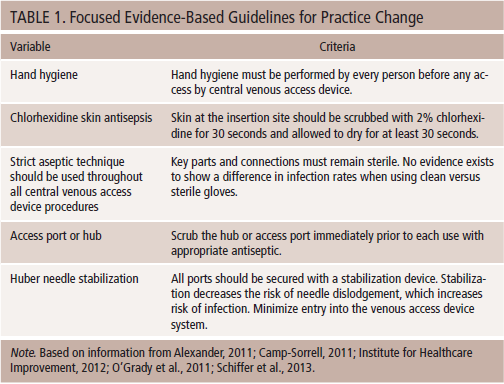
Assessment of Current State
The clinical specialist and nurse director conducted an assessment of the current state and found a wide variance in central line port access and dressing practices. Part of the controversy was that the current institutional policies provided for three types of port dressings: sterile, clean, and high risk. The clean technique was instituted at DFCI 10 years ago when the controversy of clean versus sterile was debated. The rationale was that short-term access did not require the sterile dressing. The inpatient oncology unit continued to require sterile technique. The third high-security dressing was applied to patients going home on continuous infusion of a highly irritant drug with a CADD® pump. The rationale that different types of port access were needed for outpatients versus inpatients was based on history and policy rather than on evidence. CLABSI rates are monitored by the infection control department and showed that, in the 10 years that DFCI used clean technique, no increase occurred in outpatient CLABSI rates.
Interviews with nurses revealed unique approaches and rationale for dressing practices. The desire to provide the best care for their patients was paramount, but no consensus existed on practice. Nurses expressed the need for a standard of practice based on evidence. The results of the assessment were presented to nursing practice committees. The CLABSI committee is a multidisciplinary, multi-institution membership, including infection control, that provided review and surveillance of CLABSI for outcome measures. Support to establish a standard of evidence-based practice for port access and dressing was attained. The committee reviewed and approved all practice change.
Methods
What is clear from the literature is that focus of central line procedures must be on aseptic technique and not the hierarchical paradigm that was used. Debate and variation surrounding aseptic technique in nursing has led to variability in technique in the absence of research (Aziz, 2009). The Aseptic Non Touch Technique (ANTT®) is a contemporary approach to aseptic practice rather than the conventional sterile, aseptic, and clean techniques (Rowley, Clare, Macqueen, & Molyneux, 2010). ANTT means that, when handling sterile equipment, the part of the equipment being used that comes into direct or indirect contact with a key site (port access site) is not touched or handled. Clarity on the definitions of dressing technique provided the foundation for practice change. The goal is to focus nurses’ attention on the principles and practices of aseptic technique that have been established to prevent CLABSI. In aseptic technique, one cause of infection exists: contamination of key parts or sites (Rowley et al., 2010).
Implementation
The team of clinical specialists from the Department of Clinical Education and Professional Development at DCFI developed and conducted mandatory 90-minute training sessions for all nursing staff. Flyers and posters depicted the correct technique and dressing procedure emphasizing zero CLABSIs as the outcome goal. A pre- and post-test assessed individual knowledge of the key concepts. Didactic sessions reviewed professional guidelines and the new port access and dressing policy. Skill stations provided a step-by-step demonstration and return demonstration of the correct aseptic technique, emphasizing key parts and key connections that were critical to preventing CLABSIs. They were identified as critical connections. A scrub-the-hub station included use of an ultraviolet light and marker that demonstrated whether the nurse had sufficiently cleaned the hub. Question-and-answer sessions were provided to encourage dialogue on practice evidence and culture. The sterile gloves and kits were the biggest stumbling block. Nurses had strong opinions on practice, and the interactive exchange provided a forum to introduce evidence-based standards and guidelines that are shown to prevent CLABSIs.
After the program began in June 2012, it was clear that misinterpretations of the key elements of the new technique occurred. Aseptic fields were omitted in some cases because nurses were opening sterile items and placing them onto nonsterile fields, such as a disposable pad. The 30-second scrub was not timed, and patients noted that some nurses cleaned the site longer than others (Weingart et al., 2014). When nurses were questioned, they would state that they only use clean technique. Other nurses continued to use sterile gloves because they did not believe clean gloves were as safe. The ANTT concept was not uniformly accepted, and, therefore, the goal of standardization was not achieved.
The IV team nurse director and charge nurse and the clinical specialist developed an audit tool to monitor practice and reinforce the evidence (see Figure 1). The emphasis of asepsis and critical connections while performing the access provided clarity on the importance of not contaminating key parts and sites. The auditor timed the nurse skin prep with chlorhexidine scrub and dry and reinforced the evidence that removing microorganisms at the insertion site is a key to CLABSI prevention. 
Audits were conducted monthly with peer-to-peer audits replacing clinical nurse specialist audits, which provided the necessary peer support for the practice. Peers can be very influential, and informal leaders may weigh in even stronger than formal leaders in practice change (Melnyk & Fineout-Overholt, 2011). The audits were instrumental in nurse compliance with the evidence-based interventions and the recommended standards. The CDC reported that well-organized programs that educate, monitor, and evaluate care are critical to success; declining infection rates follow standardization of aseptic care; and IV teams have shown unequivocal effectiveness in reducing incidence of CLABSIs (O’Grady et al., 2011).
Results
Consistent nursing practice for central line port access was achieved with audits demonstrating 100% compliance with the critical components known to prevent CLABSI by six months postintervention. This compliance has been sustained, and monitoring continues monthly. The most important outcome was a sustained decline in CLABSI rates. The CLABSI rate is measured per 1,000 line accesses in the outpatient setting. Rates prior to the intervention in quarter 3 of 2012 were 1.39 and measured at 0.88 in quarter 2 of 2013 (see Figure 2). These trends continued to be sustained through 2015. Expansion of education about critical components of best practice with port access led to development of online videos, teaching sheets, and skill demonstration in orientation. 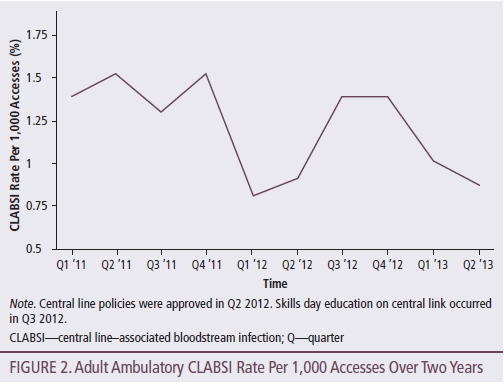
Conclusion
Standardizing port access and dressing practice by implementing evidence-based policies are associated with measurable improvement in patient outcomes. Patients want consistency in nursing practice (Weingart et al., 2014). A multifaceted approach is required to ensure that clinical guidelines are adopted into nursing practice at the point of care. Nursing culture and peer influence are aspects that must be considered in achieving practice change. Education that provides the rationale for change and opportunity for skill demonstration are critical elements to understanding and acceptance. Practice audits involving peer review to monitor change improve compliance and sustain the practice change. The goal for standardization and adherence to guidelines is to achieve zero CLABSIs.
References
Alexander, M. (Ed.). (2011). Infusion nursing standards of practice. Journal of Infusion Nursing. Retrieved from http://www.ins1.org/files/public/11_30_11_standards_of_practice_2011_co…
Aziz, A.M. (2009). Variations in aseptic technique and implications for infection control. British Journal of Nursing, 18, 26–31.
Camp-Sorrell, D. (2011). Access device guidelines: Recommendations for nursing practice and education (3rd ed.). Pittsburgh, PA: Oncology Nursing Society.
Centers for Disease Control and Prevention. (2011a). Guidelines for the prevention of intravascular catheter-related infections, 2011. Retrieved from http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
Centers for Disease Control and Prevention. (2011b). Vital signs: Central line–associated blood stream infections—United States, 2001, 2008, and 2009. Morbidity and Mortality Weekly Report. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6008a4.htm
Chopra, V., Krein, S.L., Olmstead, R.N., Safdar, N., & Saint, S. (2013). Prevention of central line-associated bloodstream infections: Brief update review. In V. Chopra, S.L. Krein, R.N. Olmsted, N. Safdar, & S. Saint, Making health care safer II: An updated critical analysis of the evidence for patient safety practices. Santa Monica, CA: RAND.
Institute for Healthcare Improvement. (2012). How-to guide: Prevent central line–associated bloodstream infection. Cambridge, MA: Author.
Loveday, H.P., Wilson, J.A., Pratt, R.J., Golsorkhi, A., Tingle, A., Bak, J.B., . . . Wilcox, M. (2014). Epic3: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. Journal of Hospital Infection, 86(Suppl.), S1–S70.
Melnyk, B.M., & Fineout-Overholt, E. (2011). Evidence-based practice in nursing and healthcare: A guide to best practice (2nd ed.). Philadephia, PA: Lippincott, Williams and Wilkins.
Mollee, P., Jones, M., Stackelroth, J., van Kuilenburg, R., Joubert, W., Faoagali, J., . . . Clements, A. (2011). Catheter-associated bloodstream infection incidence and risk factors in adults with cancer: A prospective cohort study. Journal of Hospital Infections, 78, 26–30.
O’Grady, N.P., Alexander, M., Burns, L.A., Dellinger, E.P., Garland, J., Heard, S.O., . . . Saint, S. (2011). Guidelines for the prevention of intravascular catheter-related infections. American Journal of Infection Control, 39(Suppl. 1), S1–S34. doi:10.1016/j.ajic.2011.01.003
Rowley, S., Clare, S., Macqueen, S., & Molyneux, R. (2010). ANTT v2: An updated practice framework for aseptic technique. British Journal of Nursing, 19(Suppl.), S5–S11.
Schiffer, C., Mangu, P., Wade, J., Camp-Sorrell, D., Cope, D., El-Rayes, B., . . . Levine, M. (2013). Central venous catheter care for the patient with cancer: American Society of Clinical Oncology clinical practice guideline. Journal of Clinical Oncology, 31, 1357–1370.
Tomlinson, D., Mermel, L.A., Ethier, M.C., Matlow, A., Gillmeister, B., & Sung, L. (2011). Defining bloodstream infections related to central venous catheters in patients with cancer: A systematic review. Clinical Infectious Diseases, 53, 697–710. doi:10.1093/cid/cir523
Umscheid, C.A., Mitchell, M.D., Doshi, J.A., Agarwal, R., Williams, K., & Brennan, P.J. (2011). Estimating the proportion of healthcare-associated infection that are reasonably preventable and the related mortality and costs. Infection Control and Hospital Epidemiology, 32, 101–114.
Weingart, S.N., Hsieh, C., Lane, S., & Cleary, A.M. (2014). Standardizing central venous catheter care by using observations from patients with cancer. Clinical Journal of Oncology Nursing, 18, 321–326. doi:10.1188/14.CJON.321-326
About the Author(s)
Susanne B. Conley, MSN, RN, AOCNS®, CPON®, is a clinical specialist at the Dana-Farber Cancer Institute in Boston, MA. The author takes full responsibility for the content of the article. The author did not receive honoraria for this work. No financial relationships relevant to the content of this article have been disclosed by the author or editorial staff. Conley can be reached at susanne_conley@dfci.harvard.edu, with copy to editor at CJONEditor@ons.org.




