Patients With Breast Cancer Receiving Chemotherapy: Effects of Multisensory Stimulation Training on Cognitive Impairment
Background: Patients with breast cancer receiving chemotherapy can experience chemotherapy-related cognitive impairment (CRCI).
Objectives: This study observed the interventional effects of multisensory stimulation training on CRCI in patients with breast cancer receiving chemotherapy.
Methods: Eighty patients with breast cancer receiving chemotherapy at a grade A tertiary hospital in Tangshan City, Hebei Province, China, were divided into two intervention groups (audiovisual and multisensory) by random sampling (40 patients per group).
Findings: After four intervention cycles, participants’ cognitive and executive function scores were higher in the multisensory group than in the audiovisual group. Multisensory stimulation training had stronger effects than audiovisual training and effectively attenuated CRCI and executive dysfunction caused by breast cancer chemotherapy. Given the convenience and ease of use, multisensory stimulation has good potential for application in clinical practice.
Jump to a section
Breast cancer is caused by abnormal proliferation of breast epithelial tissue cells that cause malignant transformation, and its incidence has risen steadily (Zeng et al., 2017). Chemotherapy is commonly used pre- and postsurgery for patients with breast cancer, and the chemotherapy regimens are mainly based on anthracyclines (Li et al., 2018). Patients often experience reduced quality of life (QOL) from adverse side effects. Therefore, postoperative nursing care for this population has gained increased attention.
Chemotherapy-related cognitive impairment (CRCI), sometimes known as “chemobrain,” is a common side effect and an issue in patients with breast cancer (Kovalchuk et al., 2017). CRCI clinically manifests as verbal memory decline, information processing speed decrease, confusion of thinking, and the decline of executive function and visuospatial ability (Bompaire et al., 2017). Kaiser et al. (2014) found that 14%–85% of patients experienced deficits in attention, memory, executive control, and handling speed of life events following chemotherapy. Chemotherapy also led to a progressive decline in cognitive functioning in patients with breast cancer, with peak decline occurring during cycles 3–5 (Lange et al., 2019). CRCI substantially affects patients’ short- and long-term recovery and QOL. Memory dysfunction is an initial symptom of CRCI (Nott & Glass, 2018) and can trigger mental disorders, including depression and anxiety, which affects patients’ recovery and QOL. Kesler et al. (2013) tested a computerized cognitive training program for breast cancer survivors receiving chemotherapy, finding significant improvements in memory and attention. Other studies demonstrated therapeutic effects of audiovisual training on cognitive functioning recovery among patients who had a stroke (Chen & Mao, 2016; Zhang, Chen, et al., 2016). The authors of the current study developed a multisensory stimulation training program that consists of visual, auditory, tactile, and olfactory training techniques to attenuate CRCI and executive dysfunction in patients with breast cancer receiving chemotherapy. The results provide a scientific basis for the clinical application of such training to enhance patients’ QOL.
Methods
Sample and Setting
Eighty patients with breast cancer receiving chemotherapy at Tangshan People’s Hospital, a grade A tertiary hospital in Tangshan, Hebei, China, between March 2018 and April 2019 were recruited for participation. Inclusion criteria were (a) having received two chemotherapy cycles, with the total number of prescribed cycles being 6 or more of the ACT (epirubicin, cyclophosphamide, and docetaxel) chemotherapy regimen; (b) being aged 18–60 years; (c) having a Montreal Cognitive Assessment score of less than 26; and (d) providing informed consent to participate. Patients with severe vision or hearing loss, a history of mental disease, or severe physical or mental illness were excluded. Participants were randomized into audiovisual (n = 40) and multisensory (n = 40) intervention groups. Demographic information, including the participants’ ages and occupations, did not differ significantly between groups (see Table 1). The study was approved by the hospital’s ethics committee (No. RMYY-YWLL-2018-17). 

Procedures
Nurse training: Through intensive training, nurses are expected to know how to use assessment tools and master the standard intervention methods. A WeChat group was created to facilitate communication between the researchers and patients, allowing the researchers to be informed of the everyday training of patients at home.
Participant training: The experimental (multisensory) and control (audiovisual) groups of patients with breast cancer received routine nursing and audiovisual training; however, the experimental group also received multisensory stimulation training consisting of olfactory and tactile stimulation.
Based on the 66nao Brain Training system developed by Wispirit Tech, the audiovisual training was comprised of three modules: photo–name matching, listen and link, and sequence memory (Kesler et al., 2013). The photo–name matching module was designed to train patients’ ability to recognize faces, match photos and names, and improve delayed recall memory. The listen and link module trained patients’ semantic processing ability and working memory. Finally, the sequence memory module focused on training patients’ memory and execution capability. Researchers could log into the system and check patients’ daily training and the duration of time patients were hospitalized. After patient discharge, the researchers could communicate with the patients and their families, supervise the exercises, and ensure the effectiveness of the training using WeChat or telephone. One treatment cycle lasted for 26 days, consisting of 5 days of hospitalization for routine treatment and 21 days of rest at home. The stimulation training lasted for 20 minutes each day. The cycles of treatment were repeated four times.
The multisensory group received the audiovisual intervention and an intervention component that consisted of scalp tactile stimulation and tactile training with objects. The scalp tactile stimulation involved three steps. First, participants were instructed to keep their fingers adducted together and massage the temples in the clockwise and anticlockwise direction. Second, they used their ring finger to press the forehead area from the glabella to the Baihui acupoint at the top of the head, then along the midline and continuing downward to the Fengchi acupoint at the nape of the neck. Third, they used their fingertips on both hands to gently comb the head, starting at the forehead and moving toward the back of the head (see Table 2 and Figure 1). The tactile training with objects involved two different objects being placed in a cardboard box for the patients to feel the size, temperature, and texture using both hands (Dacleu Ndengue et al., 2017). 
The multisensory group also participated in an intervention method that comprised olfactory memory stimulation training and olfactory stimulation training during bedtime. The olfactory memory stimulation training involved the nurses preparing two test strips infused with different essential oils. One test strip was placed under the nose for 20 seconds, so the patient could memorize the scent. After two minutes, the participant smelled the other test strip. After five minutes, the patient was asked to name the two essential oils in order. During bedtime, the olfactory stimulation training comprised of nurses lighting a lavender-scented candle and placing it beside the participant’s bed while relaxing music was played. Patients engaged in diaphragmatic breathing for 10 minutes (Hassanzadeh et al., 2018). 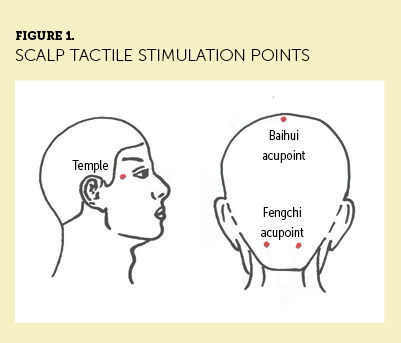
The tactile and olfactory stimulation trainings were performed once a day for five consecutive days, lasting for 10 minutes each time. These cycles were repeated four times.
Assessment
The CRCI and executive functioning of the participants in both groups were assessed before the stimulation training and after four cycles of stimulation training, using the second edition of the Rivermead Behavioural Memory Test (RBMT-II) (Gao et al., 2018) and the Behavioural Assessment of the Dysexecutive Syndrome (BADS) (Wilson et al., 1997). The RBMT-II consists of 12 subtests, including remembering names, remembering hidden belongings, and picture recognition. Total scores range from 0 to 24, with lower scores indicating worse executive function (Rosenblatt, 2011). BADS consists of six subtests, including rule-shift cards, action program, and temporal judgment (each ranging from 0 to 4 points). Total scores range from 0 to 24, with lower scores indicating more flawed executive function.
Data Analysis
Analyses were performed using IBM SPSS Statistics, version 23.0. Characteristics between groups were compared using a chi-square test, and test scores were expressed as means and standard deviations. Inter- and intragroup comparisons were performed using independent and paired-samples t tests, respectively. Differences were considered statistically significant at p < 0.05.
Results
RMBT-II
Table 3 shows participants’ pre- and postintervention RBMT-II scores. Preintervention, the standardized RBMT-II subtest and total scores did not differ significantly between groups. After four intervention cycles, the multisensory intervention group had significantly higher scores on 11 subtests and a significantly higher total score than the audiovisual group (all p < 0.05). In the audiovisual group, scores for eight subtests and the total RBMT-II score significantly increased postintervention. In the multisensory intervention group, all RBMT-II scores were significantly higher postintervention. 
BADS
On BADS, preintervention, the subtest and total scores did not differ significantly between groups (p > 0.05). After four intervention cycles, the multisensory intervention group had significantly higher scores in four tests and a higher total BADS score than the audiovisual group (p < 0.001). In both groups, the postintervention scores for four subtests and the total score were significantly higher than preintervention scores (p < 0.01 for the audiovisual group; p < 0.001 for the multisensory intervention group).
Discussion
The results showed that multisensory stimulation training was more effective than audiovisual training in memory restoration and executive function enhancement. Potential mechanisms of action are discussed in this section.
The photo–name matching module is training for delayed memory. The first recognition picture information is transmitted to the hippocampus through neurons to form short-term memory. This process calls forth the remaining information in the hippocampus. Repeated introduction, turnover, and output can strengthen the excitability of synapses in the hippocampus. The more the same stimulus is received, the closer the neural pathways are connected, and the final form is permanent (Bobkova et al., 2018).
The audiogram connection module uses the connection between things to memorize through association. When the systematic recording along the auditory nerve afferents to the posterior cortical area of the brain, it will respond to the listened words; that is, it is associated with memory traces or experiences, so the words correspond to specific items. When the game allows the patient to select the same category as the recorded words, it requires the patient to think of another thing related to the current perceived thing. Because of the strong integration function of the audiovisual center, it stimulates the continuous discharge between the dorsolateral and right anterior frontal cortex, so the body’s cognitive memory of external information is complete and comprehensive (Kato & Caplan, 2017).
Calming a patient’s emotions is also a potential mechanism. The emotional trauma of a cancer diagnosis and the physical discomfort caused by chemotherapy side effects can lead to feelings of extreme sadness and depression, aggravating CRCI (Dong et al., 2016). In the current study, the audiovisual training modules created a lively atmosphere that alleviated participants’ feelings of stress and dullness. The physical and mental comfort experienced by patients promoted the secretion of large amounts of endorphins by the pituitary gland, contributing to emotional reactions, alleviating anxiety and depression, regulating cardiovascular and respiratory functions, increasing cerebral blood flow, and promoting hippocampal glucose metabolism. All of this could have attenuated chemical damage to the cognitive function (Zhang, Zong, et al., 2016).
Self-worth manifestation may be involved as a mechanism. The games provided morale-boosting effects through sound effects such as “great job!” and “congratulations, you got it right again!” after successful task completion. Appropriate recognition of performance led to continuous enhancement of participants’ self-esteem and self-confidence, lessening adverse effects on cognitive and psychological state, aiding CRCI and executive function recovery to a certain extent.
Odors are potent stimulants that can arouse emotions and provide support for learning and memory. The neural basis for such strong odor–emotional memory connections is determined by the unique anatomical characteristics of the olfactory pathway (Aydın Yıldırım & Kitiş, 2020). In the olfactory memory stimulation training task, nurses provided olfactory stimulation to participants using two different essential oils, activating the neural network between axon terminals and dendrites. Consequently, neurons with identical receptors became engaged in neuronal population activity, leading to direct transmission of odor information to the limbic system, increasing the excitation level in the limbic system and enhancing memory effects (Liu et al., 2016). Scented candles made with natural essential oils can provide nerve-calming and sleep-promoting effects (Song et al., 2018). The olfactory stimulation training during bedtime was a relaxation therapy method. When participants were supine and engaged in diaphragmatic breathing, information regarding the aromatic compounds was transmitted by olfactory receptor cells in the nose to the brain, triggering the secretion of enzymes and hormones by the pituitary gland. Simultaneously, activity levels in the parasympathetic nervous system and related functions increased. In a state of deep relaxation, participants’ energy consumption decreased, which increased the myoglobin level and oxygen-carrying capacity of the blood, leading to a high blood oxygen level in the brain, which was conducive to brain tissue reconstruction (Bar et al., 2020; Laventure et al., 2016).
Tactile sensations are mainly responsible for transmitting varying sensory information to the central nervous system, which transmits the information to the relevant brain areas (Berkheimer et al., 2017). During tactile training, different objects’ temperatures and textures acted as stimuli to tactile receptors on participants’ skin. When the neurons detected stress level changes, minute electrical signals were transmitted via nerve fibers to the brain to regulate the vestibular nuclei reaction to the tactile stimulation, leading to effective connections between tactile nerves and brain areas involved in information processing, enhancing cognitive ability (Szameitat et al., 2016). The temples, Baihui acupoint, and Fengchi acupoint with tactile stimulation of the scalp are all related to cognitive function (Chen et al., 2019). The local scalp acupressure implemented in this study can stimulate brain nerve cells, accept impulses, release transmitters, and affect target organs to achieve the purpose of improving brain function, refreshing the brain, and improving the cognitive function of patients (Feng & Wang, 2015).
Limitations
This study has several limitations that merit discussion. In the current study, the sample included only 80 patients with breast cancer aged 18–60 years who were hospitalized for chemotherapy, and those receiving chemotherapy in outpatient clinics were not included. Therefore, generalizability is limited. Because older adults in China have limited use of smartphones, restrictions were placed on the age of the target population. As the effectiveness of this intervention reveals, future research by the study team will also include outpatients receiving chemotherapy, and the age range will be extended to increase the sample size and verify the current findings regarding multisensory stimulation training.
Implications for Nursing
Multisensory stimulation training has a specific effect on CRCI and execution function of patients with breast cancer receiving chemotherapy. A relaxed and pleasant atmosphere can ease the patient’s tension and anxiety. In addition, the intervention is not only enjoyable, but also simple to understand. It does not require patients to be of a certain age or have a certain education level, and no training is needed. It can make full use of common items, reduce the consumption of human and material resources, and reduce the use rate of medical resources. Combined with the network platform system, it is scientific and accurate. It provides a new intervention method for hospitals at all levels, particularly for grassroots community health centers, to accelerate rehabilitation treatment, enhance the confidence and safety of patients, reduce the psychological and mental burden of patients, and improve satisfaction with QOL and social communication ability. This intervention can broaden the breadth and depth of the nursing profession, make nursing work more professional, reflect the value of nursing, and accelerate the development of tumor rehabilitation. 
Conclusion
The research group innovatively applied comprehensive multisensory training to the population of patients with breast cancer receiving chemotherapy, and it significantly improved cognitive and executive function. The current study shows that multisensory stimulation training was more robust and provided better results than audiovisual training alone. It provides a new rehabilitation theory base and clinical application methods for patients with breast cancer experiencing CRCI. 
About the Author(s)
Zeyuan Li, BS, is a student in the Department of Preventive Medicine at the North China University of Science and Technology in Tangshan, Heibei, China; Xijun Hao, MS, is a PhD student in the Department of Geriatrics at Tianjin Medical University General Hospital in Tianjin, Heping, China, and an attending physician in the College of Nursing and Rehabilitation at the North China University of Science and Technology; Ping Lei, PhD, MD, is a professor and dean in the Department of Geriatrics at Tianjin Medical University General Hospital; Lizhi Zhou, MS, is the chief nurse in Breast Surgery at Tangshan People’s Hospital in Tangshan; Changxiang Chen, MS, is a professor and Tingting Tan, MS, is an assistant, both in the Department of Rehabilitation Medicine at the North China University of Science and Technology; and Liming Yue, BS, RN, is a nurse-in-charge in the Department of Breast Surgery at Tangshan People’s Hospital. Li and Hao are dual first authors. The authors take full responsibility for this content. This research was supported, in part, by grants from the Medical Scientific Research Project of Hebei Province (Grant no. 20200164) and the Tangshan City Talent Support Program (Grant no. A201901006). The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Zhou can be reached at zhoulizhi72@126.com and Lei can be reached at leiping1974@163.com, with copy to CJONEditor@ons.org. (Submitted December 2020. Accepted September 30, 2021.)
References
Aydın Yıldırım, T., & Kitiş, Y. (2020). The effect of aromatherapy application on cognitive functions and daytime sleepiness in older adults living in a nursing home. Holistic Nursing Practice, 34(2), 83–90. https://doi.org/10.1097/HNP.0000000000000371
Bar, E., Marmelshtein, A., Arzi, A., Perl, O., Livne, E., Hizmi, E., . . . Nir, Y. (2020). Local targeted memory reactivation in human sleep. Current Biology, 30(8), 1435–1446. https://doi.org/10.1016/j.cub.2020.01.091
Berkheimer, S.D., Qian, C., & Malmstrom, T.K. (2017). Snoezelen therapy as an intervention to reduce agitation in nursing home patients with dementia: A pilot study. Journal of the American Medical Directors Association, 18(12), 1089–1091. https://doi.org/10.1016/j.jamda.2017.09.009
Bobkova, N.V., Novikov, V.V., Medvinskaya, N.I., Aleksandrova, I.Y., Nesterova, I.V., & Fesenko, E.E. (2018). Effect of weak combined static and extremely low-frequency alternating magnetic fields on spatial memory and brain amyloid-b in two animal models of Alzheimer’s disease. Electromagnetic Biology and Medicine, 37(3), 127–137. https://doi.org/10.1080/15368378.2018.1471700
Bompaire, F., Durand, T., Léger-Hardy, I., Psimaras, D., & Ricard, D. (2017). Troubles cognitifs chimio-induits ou «chemobrain»: concept et état de l’art [Chemotherapy-related cognitive impairment or “chemobrain”: Concept and state of art]. Geriatrics and Psychology Neuropsychiatry of Aging/Geriatrie Et Psychologie Neuropsychiatrie Vieillissement, 15(1), 89–98. https://doi.org/10.1684/pnv.2017.0659
Chen, C.X., & Mao, R.H. (2016). BrainHQ shijue xunlian dui nao cuzhonghuanzhe zhixing gongneng de yingxiang fenxi [Effects analysis of BrainHQ visual training on executive function of patients with stroke]. Chinese Journal of Rehabilitation Medicine, 31(4), 439–442. https://doi.org/10.3969/j.issn.1001-1242.2016.04.013
Chen, J., Li, S.X., & Chen, C.X. (2019). Zonghe xuewei anmo dui gaishan COPD bingren renzhi gongneng he shenghuo zhiliang de xiaoguo yanjiu [Effect of comprehensive acupressure on cognitive function and quality of life in patients with COPD] .Chinese Nursing Research, 33(4), 660–662. https://doi.org/10.12102/j.issn.1009-6493.2019.04.026
Dacleu Ndengue J., Cesini, I., Faucheu, J., Chatelet, E., Zahouani, H., Delafosse, D., & Massi, F. (2017). Tactile perception and friction-induced vibrations: Discrimination of similarly patterned wood-like surfaces. IEEE Transactions on Haptics, 10(3), 409–417. https://doi.org/10.1109/TOH.2016.2643662
Dong, X.X., Shi, Y.R., & Hu, H. (2016). Qingdu renzhi sunhai bingren renzhi ganyu yanjiu jinzhan [Research progress on cognitive intervention for patients with mild cognitive impairment]. Chinese Nursing Research, 30(2), 144–146. https://doi.org/10.3969/j.issn.1009-6493.2016.02.006
Feng, X.M., & Wang, S.H. (2015). Xuewei anmo dui laonian qingdu renzhi gongneng zhangai huanzhe renzhi gongneng de yingxiang [Effect of acupressure on cognitive function in elderly patients with mild cognitive impairment]. Chinese Journal of Gerontology, 35(18), 5257–5259. https://doi.org/10.3969/j.issn.1005-9202.2015.18.106
Gao, J., Yang, F., & Chen, C.X. (2018). Gaodi yinpin zhuanhuan xunlian dui ruxian ai hualiao huanzhe renzhi ji jiyi gongneng de yingxiang [Effects of audio training on cognition and memory function of patients with breast cancer after chemotherapy]. Chinese Journal of Rehabilitation Medicine, 33(7), 789–793. https://doi.org/10.3969/j.issn.1001-1242.2018.07.007
Hassanzadeh, M., Kiani F., Bouya, S., & Zarei, M. (2018). Comparing the effects of relaxation technique and inhalation aromatherapy on fatigue in patients undergoing hemodialysis.Complementary Therapies in Clinical Practice, 31, 210–214. https://doi.org/10.1016/j.ctcp.2018.02.019
Kaiser, J., Bledowski, C., & Dietrich, J. (2014). Neural correlates of chemotherapy-related cognitive impairment. Cortex, 54, 33–50. https://doi.org/10.1016/j.cortex.2014.01.010
Kato, K., & Caplan, J.B. (2017). The brain’s representations may be compatible with convolution-based memory models. Canadian Journal of Experimental Psychology, 71(4), 299–312. https://doi.apa.org/doi/10.1037/cep0000115
Kesler, S., Hosseini, S.M.H., Heckler, C., Janelsins, M., Palesh, O., Mustian, K., & Morrow, G. (2013). Cognitive training for improving executive function in chemotherapy-treated breast cancer survivors. Clinical Breast Cancer, 13(4), 299–306. https://doi.org/10.1016/j.clbc.2013.02.004
Kovalchuk, A., Ilnytskyy, Y., Rodriguez-Juarez, R., Shpyleva, S., Melnyk, S., Pogribny, I., . . . Kolb, B. (2017). Chemo brain or tumor brain—that is the question: The presence of extracranial tumors profoundly affects molecular processes in the prefrontal cortex of TumorGraft mice. Aging, 9(7), 1660–1675. https://doi.org/10.18632/aging.101243
Lange, M., Joly, F., Vardy, J., Ahles, T., Dubois, M., Tron, L., . . . Castel, H. (2019). Cancer-related cognitive impairment: An update on state of the art, detection, and management strategies in cancer survivors. Annals of Oncology, 30(12), 1925–1940. https://doi.org/10.1093/annonc/mdz410
Laventure, S., Fogel, S., Lungu, O., Albouy, G., Sévigny-Dupont, P., Vien, C., . . . Doyon, J. (2016). NREM2 and sleep spindles are instrumental to the consolidation of motor sequence memories. PLOS Biology, 14(3), e1002429. https://doi.org/10.1371/journal.pbio.1002429
Li, Q., Hu, F., Li, X., Liu, T., & Guo, G. (2018). Progress in chemotherapy for breast cancer. Health Vision, 19, 291.
Liu, Y.L., Zhu, H.C., Jiao, S.J., & Li, C. (2016). Fei chidai pajinsen bing huanzhe xiujue gongneng zhangai he renzhi zhangai bianhua ji qi guanxi [Changes in olfactory dysfunction and cognitive impairment and their relationships in patients with Parkinson’s disease without dementia]. Shandong Yiyao, 56(39), 62–64. https://doi.org/10.3969/j.issn.1002-266X.2016.39.020
Nott, A., & Glass, C.K. (2018). Immune memory in the brain. Nature, 556(7701), 312–313. https://doi.org/10.1038/d41586-018-03800-6
Rozenblatt, S. (2011). Behavioral assessment of the dysexecutive syndrome. In J.S. Kreutzer, J. DeLuca, & B. Caplan (Eds.), Encyclopedia of clinical neuropsychology (pp. 377–379). Springer. https://doi.org/10.1007/978-0-387-79948-3_166
Song, W.D., Shen, J., Jiang, M., Liu, C., & Chen, W. (2018). Xunyicao jingyou de chunhua ji anmian gongxiao de yanjiu [Study on purification and hypnotic effect of lavender essential oil]. Zhongguo Yiyuan Yaoxue Zazhi, 38(18), 1911–1917.
Szameitat, A.J., Saylik, R., & Parton, A. (2016). Neuroticism related differences in the functional neuroanatomical correlates of multitasking. An fMRI study. Neuroscience Letters, 635, 51–55. https://doi.org/10.1016/j.neulet.2016.10.029
Wilson, B.A., Evans, J.J., Alderman, N., Burgess, P.W., & Emslie, H.E. (1997). BADS: Behavioural Assessment of the Dysexecutive Syndrome manual. In P. Rabbitt (Ed.), Methodology of frontal and executive function (pp. 549–559), Routledge. https://doi.org/10.4324/9780203344187
Zeng, Y., Zeng, Y., Tan, C., Liu, Q., & Zhao, S. (2017). [The correlation of chemotherapy-related cognitive impairment and self-efficacy in patients with breast cancer]. Journal of Nursing Science, 32(2), 9–12. https://doi.org/10.3870/j.issn.1001-4152.2017.02.009
Zhang, J.J., Chen, C.X., Li, S.X., Zhang, M., & Dou, N. (2016). [Effects of auditory training on cognitive function in patients with stroke]. Chinese Journal of Behavioral Medicine and Brain Science, 25(10), 905–908. https://doi.org/10.3760/cma.j.issn.1674-6554.2016.10.009
Zhang, W.-P., Zong, Q.-F., Gao Q., Yu, Y., Gu, X.-Y., Wang, Y., . . . Ge, M. (2016). Effects of endomorphin-1 postconditioning on myocardial ischemia/reperfusion injury and myocardial cell apoptosis in a rat model. Molecular Medicine Reports, 14(4), 3992– 3998. https://doi.org/10.3892/mmr.2016.5695

