Reducing Compassion Fatigue in Inpatient Pediatric Oncology Nurses
Objectives: To develop an evidence-based compassion fatigue program and evaluate its impact on nurse-reported burnout, secondary traumatic stress, and compassion satisfaction, as well as correlated factors of resilience and coping behaviors.
Sample & Setting: The quality improvement pilot program was conducted with 59 nurses on a 20-bed subspecialty pediatric oncology unit at the St. Jude Children’s Research Hospital in Memphis, Tennessee.
Methods & Variables: Validated measures of compassion fatigue and satisfaction (Professional Quality of Life Scale V [ProQOLV]), coping (Brief COPE), and resilience (Connor-Davidson Resilience Scale-2) were evaluated preprogram and at two, four, and six months postprogram, with resilience and coping style measured at baseline and at six months postprogram.
Results: Secondary traumatic stress scores significantly improved from baseline to four months. Select coping characteristics were significantly correlated with ProQOLV subscale scores.
Implications for Nursing: Ongoing organizational support and intervention can reduce compassion fatigue and foster compassion satisfaction among pediatric oncology nurses.
Jump to a section
Pediatric oncology nurses are at an increased risk for developing compassion fatigue related to lengthy relationships with patients and families, ethical dilemmas in clinical care, and active participation in grief and bereavement (Zander, Hutton, & King, 2010). Compassion fatigue has been described as an acute loss of emotional and physical energy toward the self and work, with a hindered ability to provide compassionate care for patients experiencing suffering (Figley, 2002). Symptoms of compassion fatigue may include decreased job satisfaction, fatigue, negativism, outbursts, lessened compassion toward coworkers, inability to separate work and home, intrusive thoughts related to patient suffering, dependent nurse–patient relationships, and feelings of hopelessness and depression (Aycock & Boyle, 2009; Panos, 2007; Pfifferling & Giley, 2000). Compassion fatigue may lead to higher use of sick days and increased nursing turnover (Pfifferling & Gilley, 2000; Potter et al., 2010).
Individual factors, such as having fewer than five years in the nursing profession, blurred professional boundaries, ineffective coping styles, and traumatic personal life events, further exacerbate the nurse’s reaction to the stressors of the work environment (Yoder, 2010). Environmental factors (e.g., heavy workload, high patient acuity, end-of-life patient care, rapidly changing technology, lack of administrative support) also escalate the risk for compassion fatigue and burnout (Hinds et al., 1994; Hooper, Craig, Janvrin, Wetsel, & Reimels, 2010; Rourke, 2007).
Recommended interventions to prevent and treat compassion fatigue involve individual, professional, and organizational support (Rourke, 2007). Individual interventions for self-care may include healthy eating, sleep, exercise, relaxation techniques, mindfulness, prayer, work–life balance, and personal coping strategies. Professional interventions may include boundary setting, peer consultation, diversification of workloads, positivity, and team building (Rourke, 2007). Organizational interventions may include mentoring programs, support groups, team building, continuing education, and respite settings (Aycock & Boyle, 2009; Morrison, 2012; Rourke, 2007).
In the healthcare literature, the term compassion fatigue has been used synonymously with secondary traumatic stress, moral distress, vicarious traumatization, and burnout, causing confusion between conceptual definitions and operational definitions of survey instruments. To provide clarity and congruence, this article will refer to operational definitions of compassion fatigue, secondary traumatic stress, and burnout aligned with the Professional Quality of Life Scale V (ProQOLV), a validated scale widely used to assess workplace satisfaction, secondary traumatic stress, and burnout (Stamm, 2010). According to the ProQOLV instrument, compassion fatigue consists of two parts: secondary traumatic stress and burnout (Stamm, 2010). Secondary traumatic stress describes the stress response that caregivers experience from witnessing the suffering or trauma of others (Figley, 2002) and is characterized by intrusive thoughts of a traumatic event, insomnia, fear, and avoidance (Stamm, 2010). Burnout is defined as a chronic state of physical, mental, and emotional exhaustion and cynicism secondary to cumulative work-related demands and is associated with a lack of pride in self, aversion to work, and loss of interest. The onset of burnout is gradual and brought on by work-related stressors (Maslach, Schaufeli, & Leiter, 2001; Stamm, 2010), whereas secondary traumatic stress has a rapid onset and is associated with relational aspects of caring (Stamm, 2010). Together, secondary traumatic stress and burnout reflect the challenge of balancing role-related demands and fostering therapeutic relationships within complex healthcare environments.
In contrast to compassion fatigue is the phenomenon of compassion satisfaction. Compassion satisfaction is the fulfillment derived from helping others or from doing one’s job well (Stamm, 2010). An individual’s resilience, or his or her ability to cope effectively and grow amid stressful situations, is thought to promote compassion satisfaction and protect against secondary traumatic stress and burnout (Grafton, Gillespie, & Henderson, 2010; McSteen, 2010; Zander et al., 2010).
Presence of compassion fatigue was voiced as a concern in pediatric oncology nurses at the current authors’ institution. Therefore, a needs assessment was conducted to elicit the concerns and supportive needs of nurses; this identified the areas of grief and bereavement, teamwork, and stress/burnout management. The needs assessment was followed by administration of the ProQOLV to 132 inpatient and outpatient nurses and confirmed high levels of secondary traumatic stress, moderate burnout, and high compassion satisfaction. To improve compassion fatigue in nurses working at the authors’ institution, a compassion fatigue intervention pilot program was planned.
When seeking to develop a compassion fatigue intervention program, a standardized program for pediatric oncology nurses was not found in the literature; therefore, one was designed by the current authors based on recommendations in the literature for nonpediatric settings. Most described programs consisted of one-time seminars, educational offerings, or off-site retreats, with limited evidence of ongoing organizational resources. It was recommended that each organization create a program based on interventions tailored to individual, professional, and organizational needs (Roberts & Boyle, 2005; Zander et al., 2010).
Primary goals identified by the current authors were to design an ongoing evidence-based compassion fatigue program for nurses on an inpatient pediatric oncology unit and to evaluate its impact on nurse-reported compassion fatigue and compassion satisfaction. Secondarily, the authors also sought to determine whether there was a correlation among nurses’ reported compassion fatigue, compassion satisfaction, resilience, and coping methods.
Methods
Theoretical Framework
The Neuman Systems Model, which describes an individual as a whole client or client system who interacts with actual or perceived environmental stressors, was used as the guiding framework for this project; according to this model, clients use protective mechanisms to successfully cope with stressors and facilitate overall health (Gonzalo, 2011; Neuman, 1980). In this model, compassion fatigue could be likened to the depletion of one’s core energy because of ineffective coping and resilience against stressors. Conversely, compassion satisfaction reflects overall system wellness and resilience influenced by adaptive coping and role-related meaning. Consequently, this framework is focused on nurses’ wellness, resilience, and depletion of core energy.
Sample and Setting
The pilot program was conducted on a subspecialty pediatric oncology unit at the St. Jude Children’s Research Hospital, a National Cancer Institute–designated pediatric comprehensive cancer center in Memphis, Tennessee. RNs on an inpatient unit specializing in the complex care of children and adolescents with solid and central nervous system tumors were invited to voluntarily participate in the six-month pilot program. At the time of this study, the unit had 20 beds and an average daily census of 16.7 patients and 12.8 RN hours per patient day. Each nurse was invited to participate through a face-to-face encounter with the project nurse.
Variables
Prior to program initiation, all participants were given a unique identification number. Demographic variables and the nurses’ reported secondary traumatic stress, burnout, and satisfaction were collected at baseline (prior to program), with repeated measures at two, four, and six months (plus or minus 14 days at each time point). Resilience and coping style were assessed at baseline (prior to the program) and month six (plus or minus 14 days at each time point). All measures were completed in hard copy and placed in a secure location within the unit. At each repeated measure, the project nurse hand-delivered the assessment tools to each participant. The project nurse reviewed the surveys and followed up via email or face-to-face encounter with all nurses who did not return the survey. The quality improvement project received institutional review board exemption.
Measures
Professional Quality of Life Scale V: The ProQOLV is a 30-item self-report scale adapted from the Compassion Fatigue Self-Test developed by Figley (1995). It is the most widely used scale to assess the impact of helping in caring professionals (Stamm, 2010). Scores are reported as raw scores or t scores. Raw scores allow for better analysis of continuous data, whereas t scores provide standardized scoring, which facilitates comparison across various ProQOL versions (Stamm, 2010). Average scores were derived from a database of 1,289 cases from multiple studies (Stamm, 2010). Secondary traumatic stress subscale t scores average 50 (SD = 10, Cronbach alpha = 0.81), with t scores greater than 57 indicating higher levels of stress influenced by acute or traumatic events. Raw scores between 23 and 41 are equivalent to a mean t score of 50. Raw scores of 42 or greater indicate higher secondary traumatic stress levels (Stamm, 2010). Burnout subscale t scores average 50 (SD = 10, Cronbach alpha = 0.75), with t scores greater than 57 indicating negative feelings about one’s ability to effectively perform work functions. Raw scores between 23 and 41 are equivalent to a mean t score of 50. Raw scores of 42 or greater indicate higher burnout levels (Stamm, 2010). Compassion satisfaction subscale t scores average 50 (SD = 10, Cronbach alpha = 0.88), with higher t scores (greater than 57) representing greater satisfaction with one’s ability to effectively provide compassionate care (Stamm, 2010). Raw scores between 23 and 41 are equivalent to a mean t score of 50. Raw scores of 42 or greater indicate higher compassion satisfaction levels (Stamm, 2010). Raw scores range from 10 to 50 (Stamm, 2010).
Connor-Davidson Resilience Scale-2: The Connor-Davidson Resilience Scale-2 (CD-RISC2) is a two-item, four-point Likert-type assessment of personal resilience characteristics and symptom status (Vaishnavi, Connor, & Davidson, 2007) adapted from the original 25-item CD-RISC (Connor & Davidson, 2003). Items 1 (“able to adapt to change”) and 8 (“tend to bounce back after illness or hardship”) from the CD-RISC scale comprise the CD-RISC2 questionnaire. The CD-RISC2 has a strong correlation (r = 0.78, p < 0.001) with the remaining 23 items of the CD-RISC scale (Vaishnavi et al., 2007).
Brief COPE Scale: The Brief COPE Scale is a 28-item questionnaire to assess adult coping strategies that measures coping reactions through 14 two-item subscales (Carver, 1997). Coping reaction is ranked according to a four-point Likert-type scale ranging from 1 (not at all) to 4 (a lot), with higher scores indicating endorsement of the coping trait. Subscale internal Cronbach alphas range from 0.5 to 0.9. The Brief COPE was adapted from the 60-item COPE Inventory and shows general internal consistency (Grafton et al., 2010).
Unit-Based Self-Care Program Intervention
Self-care and healthy lifestyle resources were provided to the nurses as part of the intervention program (see Figure 1). Each component of the intervention was delegated to interprofessional team members, with oversight by the corresponding discipline. 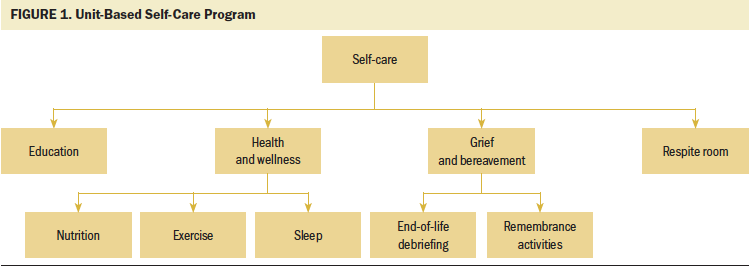
Education: Each nurse was provided with educational materials in a binder. The materials promoted awareness about compassion satisfaction and compassion fatigue and introduced self-care practices to enhance professional quality of life (i.e., health and wellness, grief and bereavement, and use of the respite room).
Health and wellness: Nutrition support was provided by a clinical registered dietitian who was available for individual consultation. The dietitian assisted with disseminating healthy snacks on the unit, including kale smoothies, blueberries, and granola bars. Healthy recipes for nurses to make at home were distributed monthly in a compassion satisfaction newsletter. Communication of on-site employee resources for physical activity, such as a free fitness center and health coaches, were included in the newsletter. In addition, nurses received educational materials describing exercises that could be performed at the nurses station. Yoga mats and handheld weights were made available in a respite room. Sleep hygiene education materials included details about maintenance of a healthy sleep schedule and shift-sensitive guidelines. As an incentive to monitor individual health and wellness goals, each nurse participant was given a Fitbit One™ calorie, activity, and sleep tracker.
Grief and bereavement: A monthly time of remembrance honoring patients who had recently died was established by the spiritual care service. Participants were encouraged to share memories and write messages honoring patients on a piece of paper; these were then folded into origami cranes and displayed in the respite room. This time of remembrance rotated monthly among the weekday, weeknight, and weekend shifts, occurring quarterly on each shift. Staff from spiritual care and quality-of-life services were available, as needed, for staff debriefings after a patient’s death. Group debriefing and remembrance sessions provided nurses the opportunity to express their emotions and concerns in a supportive environment. Individual supportive services were offered and included meeting with a member of the spiritual care and/or quality-of-life services or use of the employee assistance program, a professional counseling service offered free of charge to eligible employees and their family members. At each debriefing and remembrance session, a brief announcement was made to remind nurses of available individual supportive resources. To further assist with bereavement, sympathy cards were created and placed in the nurses’ educational binders. Nurses sent these cards to families after the death of their child, providing another method of coping and closure for the nurse.
Respite room: The respite room was constructed from a seldom-used consultation room on the inpatient unit and was furnished with comfortable furniture and soft lighting. A bookshelf housed self-care and relaxation references, such as therapeutic journaling. Additional resources for stress reduction and promotion of work–life balance, as well as music to facilitate relaxation and mindfulness, were available in the respite room. A mini refrigerator was equipped with healthy snacks and water.
Statistical Analysis
Participants’ demographic characteristics and self-reported quality-of-life scores were summarized by descriptive statistics. The Wilcoxon signed-rank test was used to compare the change in ProQOLV scores (burnout, secondary traumatic stress, and compassion satisfaction) from baseline to month two, from baseline to month four, and from baseline to month six. The change in quality-of-life scores from baseline at each time point was compared among demographic variables by using the Wilcoxon rank-sum test or the Kruskal–Wallis test. Demographic variables in the analysis included years as an RN, years as a pediatric oncology nurse, current shift, certifications, and participation in a nurse residency program. The Spearman rank correlation coefficient was used to assess the relationship between quality-of-life scores and resilience and coping style scores at baseline and at six months. A two-sided significance level of p < 0.05 was considered to be statistically significant. Statistical analyses were conducted using SAS, version 9.4.
Results
Table 1 displays demographic characteristics of the 59 RN participants. Most participants were women (n = 54). A majority of the participants were aged 20–29 years, had been an RN for fewer than five years, had fewer than five years’ experience as a pediatric oncology nurse, and had a bachelor’s degree or higher. Slightly more than half of the participants held professional certifications (n = 30). Although 59 nurses were initially enrolled, only 37 participants completed all outcome measures. The reasons for discontinuation in the project included maternity leave, transfer to another unit, and lost to follow-up. 
Changes in ProQOLV scores were compared between the following time points: preprogram (T0) to two months (T1), preprogram (T0) to four months (T2), and preprogram (T0) to six months (T3). Table 2 compares the participants’ reported ProQOLV subscale scores over time, with measures reported only for those with outcomes at the comparative time points. Eighty-one percent of nurses had comparative outcomes from T0 to T1, 83% had comparative outcomes from T0 to T2, and 69% had comparative outcomes from T0 to T3. A statistically significant (p = 0.029) reduction in secondary traumatic stress from preprogram (T0) to four months (T2) was found. 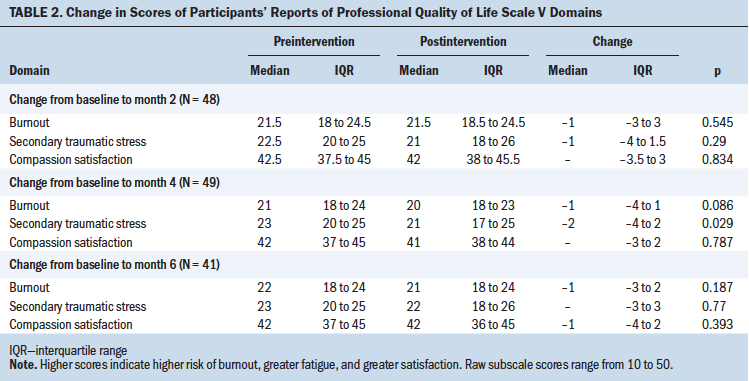
Demographic characteristics and changes in ProQOLV scores from baseline were evaluated at each time point for potential correlation. Years as an RN, shift worked, certification, and participation in the nurse residency program were not correlated with a change in ProQOLV scores from baseline over time. Also explored were the preprogram scores measuring burnout, secondary traumatic stress, and compassion satisfaction (ProQOLV subscales) and the scores’ correlation with the nurses’ reported resilience and coping style (see Table 3). Comparisons of coping styles and ProQOLV subscales of burnout, secondary traumatic stress, and compassion satisfaction demonstrated significant moderate to strong correlations (r = 0.3 to ≤ 0.5 and r > 0.5) at baseline (Cohen, 1988). The maladaptive coping mechanism of denial and self-blame positively correlated with burnout. Behavioral disengagement was positively correlated with secondary traumatic stress and burnout and negatively correlated with compassion satisfaction. 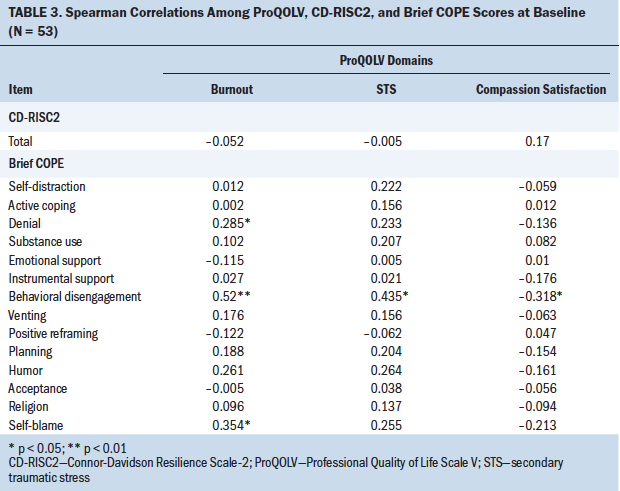
At program completion, being able to adapt and bouncing back were not significantly correlated with burnout and secondary traumatic stress. Overall scores of burnout and secondary traumatic stress minimally improved over time; however, the number of reported maladaptive coping mechanisms increased. The following maladaptive coping mechanisms were positively correlated with burnout and secondary traumatic stress: self-distraction (activities to take my mind off things), denial (believing something did not happen), substance use (glass of wine helps me escape), behavioral disengagement (giving up), venting (expressed negative emotions), humor, and self-blame. Behavioral disengagement and self-blame were negatively correlated with compassion satisfaction (see Table 4). 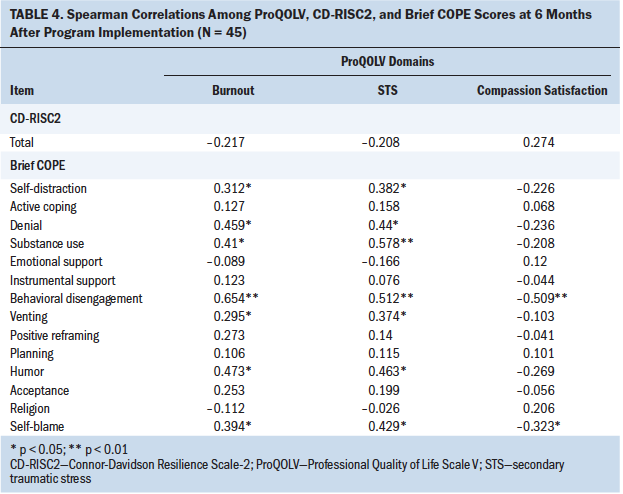
Discussion
Although not significant across all time points, the current study’s findings support those of Potter et al. (2013), who reported that a structured intervention program reduced overall levels of secondary traumatic stress in adult oncology nurses. An ongoing compassion fatigue program for pediatric oncology nurses was not found in the literature, so the current authors used a variety of evidence-based organizational and individual self-care practices for mitigating secondary traumatic stress and promoting resilience.
Although overall secondary traumatic stress and burnout scores decreased during the intervention, scores showed a slight increase at the last time point, with an increase in maladaptive coping mechanisms. This is consistent with the theoretical framework, in that maladaptive coping against stressors will increase stress (Neuman, 1980). This last time point occurred during the month of December, which coincides with important family and religious holidays. Within the pediatric oncology setting, healthcare providers often attempt to give patients and families a short respite from hospitalization over such holidays (Phillips, Barker, & Brewer, 2010). Patients who are hospitalized during the holidays likely require more time-sensitive or emergent services and close monitoring. At the same time, staffing levels may be lower because of vacations, seasonal illness, and seasonal affective disorder (Gooch, 2015). In addition, holiday staffing may consist of a larger proportion of less-experienced nurses, with limited exposure to emergency management. Following the holidays, scheduled treatment admissions tend to resume with an influx of patients.
The current authors hypothesize that the increase in secondary traumatic stress scores may have been influenced by holiday-related stress and a component of negative seasonal affective disorder. Nursing leadership should be aware of and consider the potential risk for increased stress among the nursing staff during the holiday season, providing a balanced skill mix of experienced and less-experienced nurses, as well as additional support and recognition to boost morale. Morale-boosting organizational interventions could include compensated meals, work release if census permits, bonus holiday pay, and fun holiday activities (Gooch, 2015). The current authors recommend that holiday staffing schedules and skill mix be aligned with patient treatment schedules and needs unique to this season.
Demographic characteristics were not found to be associated with secondary traumatic stress or burnout. These results are similar to those reported in a study by Potter et al. (2013) of adult oncology nurses. Potter et al. (2010) described higher stress and burnout in the more experienced nurse and suggested that higher education levels increase the risk of secondary traumatic stress and burnout. However, this was not a factor among participants in the current study, with 39 participants having fewer than five years of experience and 54 participants having a bachelor’s degree or higher. Lack of experience may be a lesser contributing factor, with most institutions offering nurses a didactic and clinical orientation program lasting several months, as well as a new-graduate nurse residency program. These programs provide an environment for mentoring of new nurses through education, collaboration, and professional development. In addition, resilience and compassion fatigue are often discussed, along with institutional resources and wellness activities.
Personal resilience is a trait thought to promote compassion satisfaction and protect against compassion fatigue. The characteristic of adaptability (ability to adapt when changes occur) was positively correlated with higher compassion satisfaction and negatively correlated with secondary traumatic stress and burnout. This suggests that adaptability may serve as a protective mechanism against secondary stress and burnout. At the last time point of assessment, secondary traumatic stress and burnout negatively correlated with resilience scores. In addition, over time, secondary traumatic stress and burnout positively correlated with maladaptive coping mechanisms; specifically, positive correlations were found with nurses’ endorsement of maladaptive coping with sarcasm and behavioral disengagement. These attitudes may serve as red flags, signaling the need for increased interventions. Self-assessments for the presence of maladaptive coping are practical ways that nurses can evaluate their risk for compassion fatigue while developing self-care strategies to foster adaptive coping and resilience.
Secondary outcomes of the current study include an increased awareness of stress and burnout, not only among nursing staff but among the entire oncology community. This nurse-led pilot program initiated awareness of the need for ongoing supportive resources for all employees involved in patient care. Several subsequent independent projects were conducted in various departments and units, with the ultimate outcome of hospital-wide resilience and coping initiatives, including the implementation of quarterly Schwartz Rounds™ and development of an interprofessional resilience center and committee. Ongoing Schwartz Center Rounds provide opportunities for interprofessional health professionals to gather and share their caregiving experiences, facilitating meaningful connections with patients and colleagues (Schwartz Center, n.d.). Respite rooms were incorporated into the construction plan for the institution’s new inpatient units, as was a dedicated nursing lounge on each unit. Promotion of staff self-care has been incorporated into orientation and ongoing education.
Limitations
Limitations of the current project include the young and less experienced sample of nurses; therefore, this sample may not represent more seasoned nurses’ compassion fatigue levels. In addition, the pilot program was conducted on only an inpatient unit; other inpatient and outpatient service areas may have responded differently to the interventions. Also, this project was limited by its six-month timeframe, with the last time point aligning with the holidays. Therefore, the current authors were unable to evaluate nurses’ reported compassion satisfaction and fatigue scores following the holidays.
Implications for Nursing
Nurses working with children and adolescents with cancer often feel that they are compelled or have a personal calling to do so. This sense of purpose and passion may explain why nurses experienced compassion fatigue and satisfaction simultaneously. Nurses are notorious for caring for others while often neglecting their own self-care. This concept was reinforced by the American Nurses Association’s (n.d.) declaration of 2017 as the “Year of the Healthy Nurse,” which encouraged nurses to create and maintain a work–life balance. In addition to individual prioritization of self-care, organizations have a key role to play in fostering a healthy work environment. Given that pediatric oncology nurses are at high risk of experiencing compassion fatigue, it is essential that healthcare organizations educate staff about this risk and provide resources for prevention and treatment. Additional research should be conducted regarding the promotion of healthy coping mechanisms when difficult patient and clinical situations are encountered. An ongoing self-care program requires support from administrators and resources and may require dedicated personnel. Offering an array of interventions allows nurses the flexibility to develop individualized self-care plans. As a result, health administrators play an integral role in supporting nurses with grief and bereavement and in role-related stress, work–life balance, and healthy coping styles while promoting the growth of resilience. 
Conclusion
Pediatric oncology nurses are susceptible to compassion fatigue. To reduce compassion fatigue in inpatient pediatric oncology nurses at the current authors’ institution, a pilot intervention program was implemented. To the authors’ knowledge, this is the first reported organizational compassion fatigue intervention targeting pediatric oncology nurses. A variety of organizational, educational, and self-care resources were provided to participants, allowing nurses to adapt self-care techniques to their individual preferences. Through a six-month pilot program, nurses’ levels of compassion fatigue were reduced, demonstrating the benefit of an ongoing compassion fatigue program. Since the completion of the pilot, several administration-led initiatives have been developed to combat compassion fatigue and foster resilience, perhaps the most significant being the development of an interprofessional resilience center. Additional work is recommended to further explore the roles of coping, resilience, and ongoing organizational and unit-focused interventions in pediatric oncology.
About the Author(s)
Courtney E. Sullivan, MSN, RN, CPNP-AC, CPHON®, is a global nursing project coordinator, Amber-Rose King, BSN, RN, CPN, is a pediatric oncology nurse, Joni Holdiness, BSN, RN, CPN, is a quality of life and palliative care nurse, Judith Durrell, BSN, CPHON®, CPN, is an RN, Kristin K. Roberts, BSN, RN, CPN, is a pediatric oncology nurse, and Christopher Spencer, RN, MSN, CNP, is a unit manager, all at the St. Jude Children’s Research Hospital in Memphis, TN; Joshua Roberts, MSN, RN, is a system director of nursing administration at the Baptist Memorial Health Care Corporation in Memphis; Susan W. Ogg, MSN, RN, is a research nurse at the St. Jude Children’s Research Hospital; Meredith W. Moreland, BSN, RN, is an RN at Emory Healthcare in Atlanta, GA; Emily K. Browne, DNP, RN, CPNP, is the director of the transition oncology program, Carla Cartwright, RD, CNSC, LDN, is a clinical dietitian, Valerie McLaughlin Crabtree, PhD, is the chief of psychosocial services, Justin N. Baker, MD, is chief of the Division of Quality of Life and Palliative Care, Mark Brown, MDiv, BCC, is a chaplain, April Sykes, MPH, is a senior biostatistician, and Belinda N. Mandrell, PhD, RN, PNP, is the director of the Division of Nursing Research, all at the St. Jude Children’s Research Hospital. This research was funded by a St. Jude Auxiliary Cancer Center Support Grant for National Cancer Institute–designated cancer centers (CA21765) from the National Cancer Institute and by the American Lebanese Syrian Associated Charities. Sullivan, King, Holdiness, Durrell, K. Roberts, J. Roberts, Browne, Cartwright, Crabtree, Baker, Browne, and Mandrell contributed to the conceptualization and design. Sullivan, Holdiness, Durrell, K. Roberts, J. Roberts, Ogg, Moreland, Brown, and Mandrell completed the data collection. Sykes and Mandrell provided statistical support. Crabtree, Sykes, and Mandrell provided the analysis. Sullivan, King, Holdiness, Spencer, Cartwright, Baker, Sykes, and Mandrell contributed to the manuscript preparation. Sullivan can be reached at courtney.sullivan@stjude.org, with copy to ONFEditor@ons.org. (Submitted September 2018. Accepted December 4, 2018.)
References
American Nurses Association. (n.d.). Resources to support nurses to take control of their health. Retrieved from https://www.nursingworld.org/practice-policy/hnhn/2017-year-of-the-heal…
Aycock, N., & Boyle, D. (2009). Interventions to manage compassion fatigue in oncology nurses. Clinical Journal of Oncology Nursing, 13, 183–191. https://doi.org/10.1188/09.CJON.183-191
Carver, C.S. (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4, 92–100. https://doi.org/10.1207/s15327558ijbm0401_6
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates.
Connor, K.M., & Davidson, J.R. (2003). Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety, 18, 76–82. doi:10.1002/da.10113
Figley, C.R. (1995). Compassion fatigue as secondary traumatic stress disorder: An overview. In C.R. Figley (Ed.), Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized (pp. 1–20). New York, NY: Brunner-Routledge.
Figley, C.R. (2002). Compassion fatigue: Psychotherapists’ chronic lack of self care. Journal of Clinical Psychology, 58, 1433–1441. https://doi.org/10.1002/jclp.10090
Gonzalo, A. (2011). Theoretical foundations in nursing: The Neuman Systems Model. Retrieved from http://nursingtheories.weebly.com/betty-neuman.html
Gooch, K. (2015, December 18). 3 steps to improve the lives of nurses through the holidays. Becker’s Hospital Review. Retrieved from https://www.beckershospitalreview.com/human-capital-and-risk/3-steps-to…
Grafton, E., Gillespie, B., & Henderson, S. (2010). Resilience: The power within. Oncology Nursing Forum, 37, 698–705. https://doi.org/10.1188/10.ONF.698-705
Hinds, P.S., Puckett, P., Donohoe, M., Milligan, M., Payne, K., Phipps, S., . . . Martin, G.A. (1994). The impact of a grief workshop for pediatric oncology nurses on their grief and perceived stress. Journal of Pediatric Nursing, 9, 388–397.
Hooper, C., Craig, J., Janvrin, D.R., Wetsel, M.A., & Reimels, E. (2010). Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected inpatient specialties. Journal of Emergency Nursing, 36, 420–427. https://doi.org/10.1016/j.jen.2009.11.027
Maslach, C., Schaufeli, W.B., & Leiter, M.P. (2001). Job burnout. Annual Review of Psychology, 52, 397–422. https://doi.org/10.1146/annurev.psych.52.1.397
McSteen, K.L. (2010). Compassion fatigue in oncology nursing: A witness to suffering. Oncology Nurse Advisor. Retrieved from http://media.oncologynurseadvisor.com/documents/32/ona_ce_1010-1012_795…
Morrison, C.F. (2012). Retention and satisfaction on BMT: An evidence-based practice project [Abstract 495]. Biology of Blood and Marrow Transplantation, 18(Suppl.), S385. https://doi.org/10.1016/j.bbmt.2011.12.493
Neuman, B. (1980). The Betty Neuman Health-Care Systems Model: A total person approach to patient problems. In J.P. Riehl & C. Roy (Eds.), Conceptual models for nursing practice (pp. 119–134). New York, NY: Appleton-Century-Crofts.
Panos, A. (2007). Understanding and preventing compassion fatigue: A handout for professionals. Retrieved from http://www.giftfromwithin.org/html/prvntcf.html
Pfifferling, J.-H., & Gilley, K. (2000). Overcoming compassion fatigue. Family Practice Management, 7(4), 39–44.
Phillips, D., Barker, G.E, & Brewer, K.M. (2010). Christmas and New Year as risk factors for death. Social Science and Medicine, 71, 1463–1471. https://doi.org/10.1016/j.socscimed.2010.07.024
Potter, P., Deshields, T., Berger, J.A., Clarke, M., Olsen, S., & Chen, L. (2013). Evaluation of a compassion fatigue resiliency program for oncology nurses. Oncology Nursing Forum, 40, 180–187. https://doi.org/10.1188/13.ONF.180-187
Potter, P., Deshields, T., Divanbeigi, J., Berger, J., Cipriano, D., Norris, L., & Olsen, S. (2010). Compassion fatigue and burnout: Prevalence among oncology nurses [Online exclusive]. Clinical Journal of Oncology Nursing, 14, E56–E62. https://doi.org/10.1188/10.CJON.E56-E62
Roberts, K.E., & Boyle, L.A. (2005). End-of-life education in the pediatric intensive care unit. Critical Care Nurse, 25, 51–57.
Rourke, M.T. (2007). Compassion fatigue in pediatric palliative care providers. Pediatric Clinics of North America, 54, 631–644. https://doi.org/10.1016/j.pcl.2007.07.004
Stamm, B.H. (2010). The concise ProQOL manual (2nd ed.). Retrieved from https://www.proqol.org/uploads/ProQOL_Concise_2ndEd_12-2010.pdf
Schwartz Center. (n.d.). Schwartz Rounds®. Retrieved from http://www.theschwartzcenter.org/supporting-caregivers/schwartz%20-cent…
Vaishnavi, S., Connor, K., & Davidson, J.R. (2007). An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: Psychometric properties and applications in psychopharmacological trials. Psychiatry Research, 152, 293–297. https://doi.org/10.1016/j.psychres.2007.01.006
Yoder, E.A. (2010). Compassion fatigue in nurses. Applied Nursing Research, 23, 191–197. https://doi.org/10.1016/j.apnr.2008.09.003
Zander, M., Hutton, A., & King, L. (2010). Coping and resilience factors in pediatric oncology nurses. Journal of Pediatric Oncology Nursing, 27, 94–108.




