Factors Influencing Surveillance Mammography Adherence Among Breast Cancer Survivors
Problem Identification: Many breast cancer survivors fail to engage in surveillance mammography to detect new and recurrent cancers. This review identifies factors promoting or inhibiting breast cancer survivors’ participation in recommended surveillance mammography.
Literature Search: This integrative review included all English-language studies published from 2000 to 2017, identified in CINAHL®, PsycINFO®, Embase®, and MEDLINE® via PubMed®.
Data Evaluation: 23 studies met the inclusion criteria and were analyzed and synthesized.
Synthesis: 19 factors influencing mammography adherence were identified and organized into a conceptual model with two major categories: individual factors and healthcare system. Sixteen individual factors represented sociodemographic, clinical, psychological, or health behavior characteristics. All three healthcare system factors related to healthcare accessibility and availability.
Implications for Research: The new model of predictors of mammography adherence can provide guidance for identifying individuals at greatest risk for nonadherence, as well as development of new interventions to address barriers to regular mammography screening, to promote early detection of new and recurrent cancers and improved survival rates.
Jump to a section
Continued surveillance is essential for early detection of new and recurrent cancers, yet many breast cancer survivors fail to engage in appropriate follow-up. A study of 27,212 survivors found that 19% had no breast imaging at five years after treatment, based on administrative claims data (Ruddy et al., 2018). The proportion of women participating in imaging decreased over time, even among women with insurance. The authors concluded that a better understanding of the factors associated with imaging was needed to improve adherence. Other studies have reported similar findings regarding nonadherence worsening over time (Doubeni et al., 2006; Field et al., 2008; Wirtz et al., 2014).
The purpose of this integrative review was to identify a comprehensive set of factors that promote or inhibit participation in recommended surveillance mammography after completing treatment for breast cancer. The authors found only two previous literature reviews focusing specifically on surveillance mammography in breast cancer survivors. Grunfeld et al. (2002) performed a comprehensive review similar to the current one, covering publications from January 1980 to August 1999. The current search covers the subsequent time period from 2000 to 2017. Another review covered the period from 1980 to 2005 but was limited only to psychosocial factors influencing adherence (Magai, Consedine, Neugut, & Hershman, 2007). Other reviews on mammography exist, but they focus on healthy women (Jerome-D’Emilia, 2015; Schueler, Chu, & Smith-Bindman, 2008). Healthy women are likely to differ in significant ways from those who have experienced diagnosis and treatment for breast cancer, as shown by Duffy, Clark, and Allsworth (2006) in a matched cohort study comparing cancer survivors with women never diagnosed with cancer.
Breast cancer is the most commonly diagnosed cancer in women, accounting for 30% of all female cancers in the United States (Siegel, Miller, & Jemal, 2019). In addition, the breast cancer incidence rate is growing rapidly worldwide, accounting for about 2.1 million new cancer cases in 2018 (Ferlay et al., 2019; Siegel et al., 2019). Breast cancer is also the most commonly diagnosed cancer in women in the United States. In 2018, breast cancer was estimated to account for 24% of all new cancer cases in women and 15% of cancer mortality among women (Ferlay et al., 2019). According to statistics from the National Cancer Institute’s (2019) Surveillance, Epidemiology, and End Results Program (SEER), newly diagnosed cases of breast cancer in 2019 were expected to total 268,600. The United States has experienced a reduction (on average, 1.8% each year from 2007 to 2016) in the breast cancer death rate (National Cancer Institute, 2019).
The National Comprehensive Cancer Network guidelines (Gradishar et al., 2018) recommend annual mammography for breast cancer survivors. A variety of factors have been shown to affect adherence to these recommendations. For example, health-related quality of life has been associated with women’s decision making related to follow-up care (Andersen, Bowen, Morea, Stein, & Baker, 2009), and patient symptoms such as depression have been shown to be barriers to participation in such care (Holden, Ramirez, & Gallion, 2014). Challenges such as insurance difficulties and fear of recurrence are among the factors impeding breast cancer survivors’ participation in follow-up cancer screenings (Tejeda et al., 2013).
Methods
Whittemore and Knafl’s (2005) five-stage framework was the methodologic strategy guiding this integrative review. The initial stage, problem identification, involved definition of the problem and purpose of the review to allow identification of variables of interest and appropriate data collection techniques. The second stage involved performance of a literature search, which was aided by a health sciences research librarian who guided selection of well-defined search terms and strategies for various databases. In the third stage, a data evaluation strategy was developed according to the characteristics of the studies identified, allowing for accurate and comprehensive assessment. In the fourth stage, data analysis was performed; this analytical method included data reduction, display, and comparison; drawing of conclusions; and verification of the outcomes. In the fifth and final stage, the outcomes of the integrative review were synthesized in this article.
The criteria for studies to be included in this integrative review were as follows:
• The study sample consisted of breast cancer survivors.
• Factors influencing surveillance mammography adherence were assessed.
• The study was a primary source addressing original research.
• The study was published in English from 2000 to 2017 in a peer-reviewed journal.
Studies were retrieved by searching four databases: CINAHL®, Embase®, PsycINFO®, and MEDLINE® via PubMed®. Keywords used to conduct the search were breast neoplasms, survivors, mammography, and cancer screening. Because each database employs different Medical Subject Heading (MeSH) terms, a research librarian guided identification of the MeSH terms likely to provide the most productive and accurate searches. The searches yielded large numbers of studies, but most did not meet all the inclusion criteria. Specifically, the process resulted in the retrieval of 537 studies in MEDLINE via PubMed, 170 in CINAHL, 199 in Embase, and 106 in PsycINFO, for a total of 1,012 publications. Of these, 989 were excluded either because they were duplicates or because they failed to meet the inclusion criteria. Many studies did not specifically focus on surveillance mammography adherence (instead addressing clinical follow-up, other imaging tests, or general survivor care), some used “screening” to refer to a procedure that was not specific to surveillance mammography for breast cancer, others had samples with other types of cancer or combined multiple types of cancer into one sample, others were literature reviews rather than original research studies, and a few were published in languages other than English. Finally, 23 studies were found to fulfill all the inclusion criteria. Figure 1 provides a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram summarizing the study selection process. The full text of each of the 23 studies was reviewed, and the findings presented were analyzed to identify significant data that were directly relevant to surveillance mammography adherence. These data were then synthesized to identify factors influencing adherence. 
Results
Regarding year of publication, 2 of the 23 studies were published from 2000 to 2005, 9 from 2006 to 2011, and 12 from 2012 to 2017, indicating a trend of growing research interest in surveillance mammography adherence. Of the countries supplying sample populations, the United States was the dominant setting in having 20 studies, with Italy, Australia, and the Netherlands having only one each. As for the research design, 22 studies had a quantitative design and 1 had a mixed-method design. 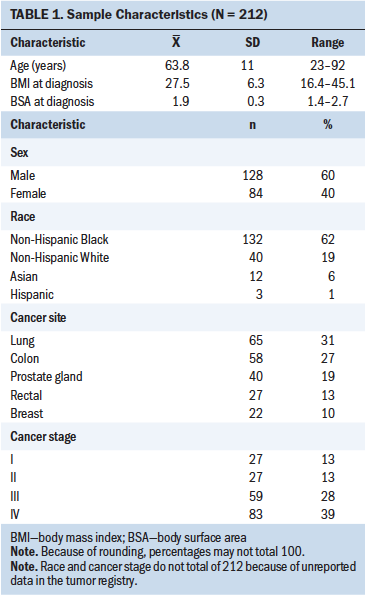
Factors Influencing Surveillance Mammography Adherence
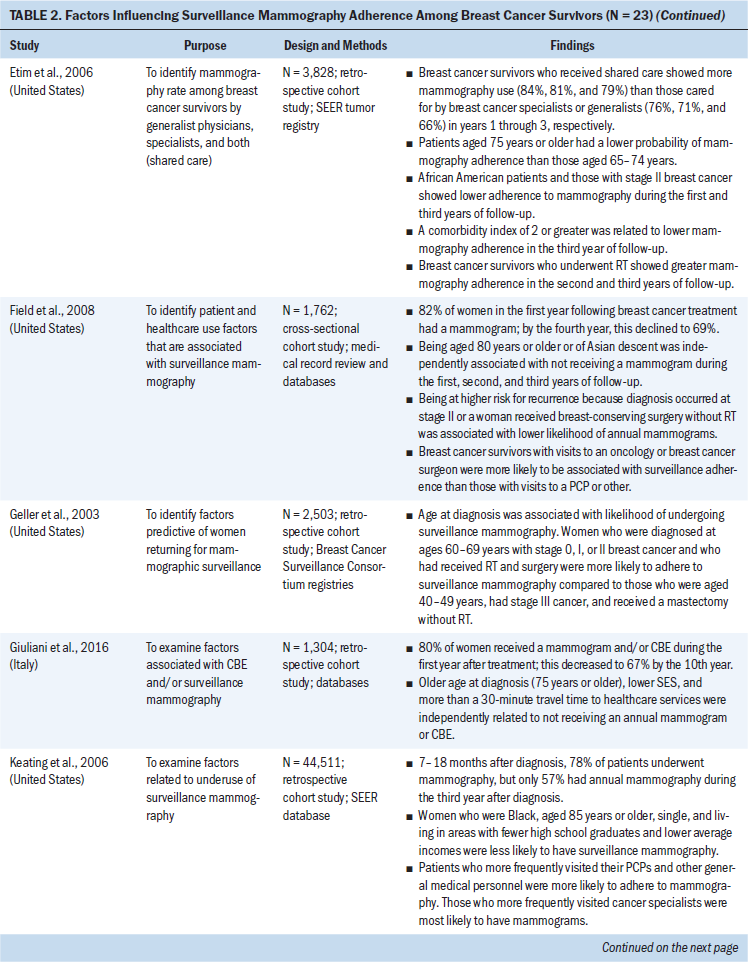
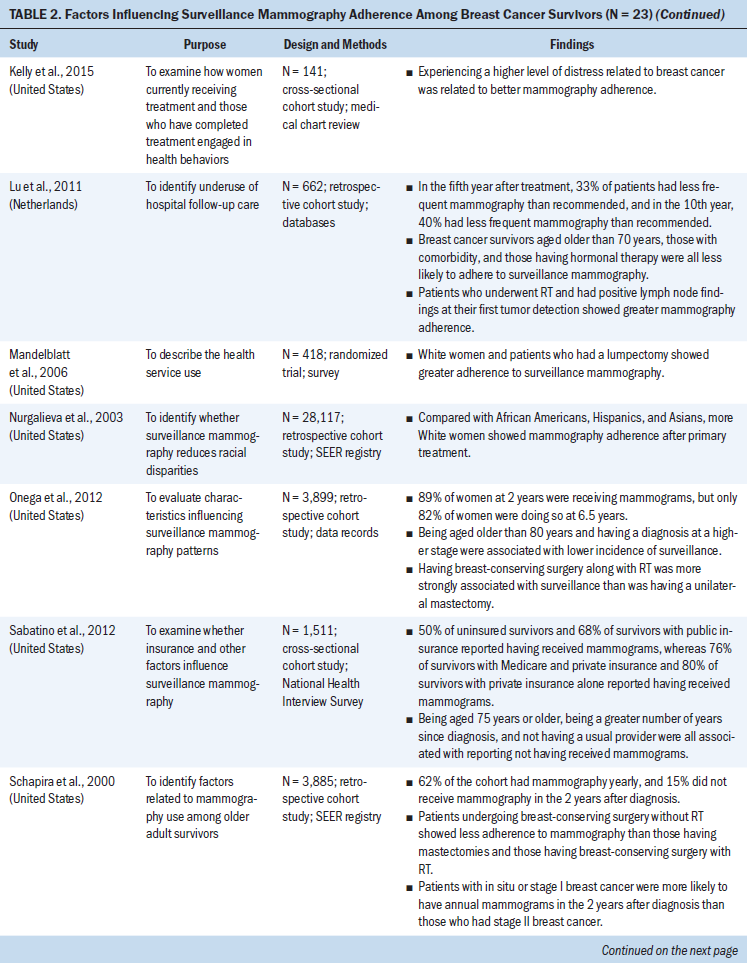
Synthesis of the review results yielded 19 factors influencing surveillance mammography adherence in breast cancer survivors. Table 1 lists these factors and the number of studies that found them to be significantly associated with mammography adherence, either positively or negatively. Table 2 provides more detailed information for each study reviewed. These 19 factors were then organized into a conceptual model, as shown in Figure 2, to summarize the findings across the 23 studies. 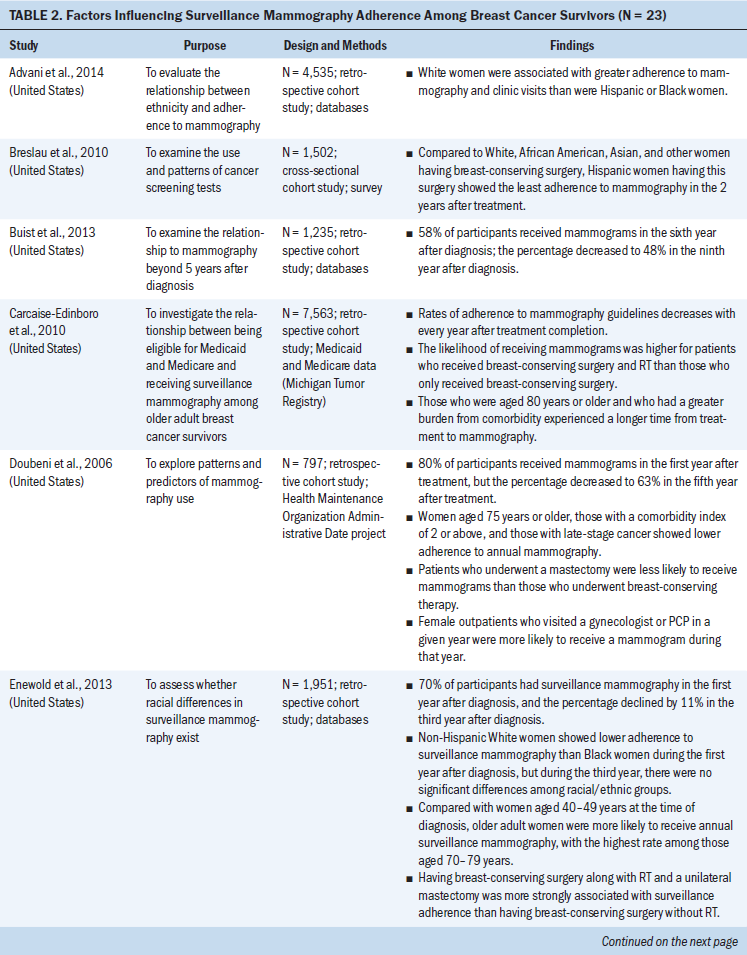
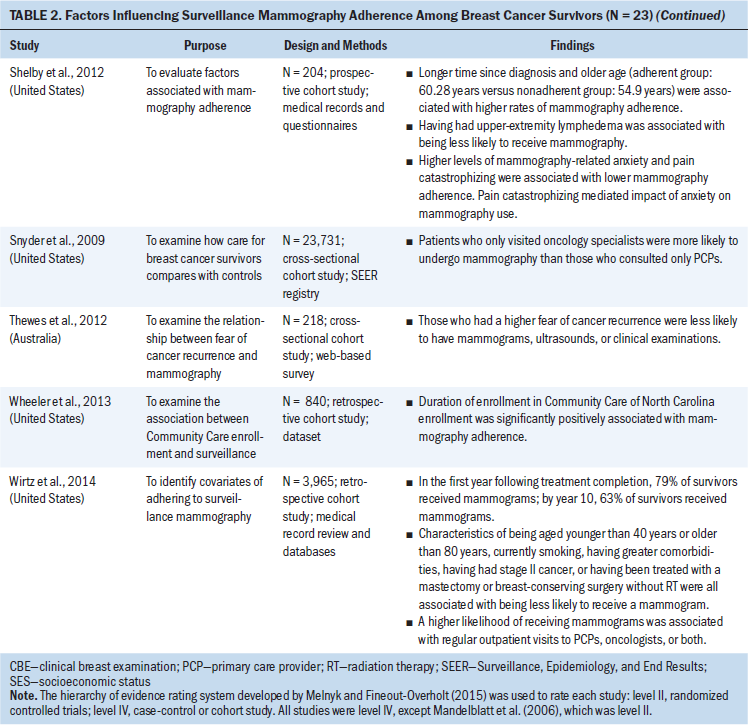
In this conceptual model, the factors were broadly grouped into two major categories, in terms of whether they related primarily to the women themselves (individual factors) or the healthcare system. A total of 16 factors were considered individual factors, which were organized into four categories: sociodemographic, clinical, psychological, and health behavior characteristics. Three factors were categorized under healthcare system factors, all of which related to healthcare accessibility and availability. 
Individual Factors Influencing Surveillance Mammography Adherence
Sociodemographic characteristics: This review revealed four sociodemographic factors influencing surveillance mammography adherence: age; ethnicity; socioeconomic status, including insurance coverage and type; and marital status. Age was the most commonly reported, with 13 of 23 studies finding age associated with adherence. However, across the 13 studies, the nature of the relationship was not straightforward; some studies found adherence decreasing with age and others the reverse. Taking all of the studies together, it appears that women at both ends of the age continuum behave differently from those in the middle. For example, in a large retrospective cohort study of 3,965 women, Wirtz et al. (2014) found the lowest rates of adherence among survivors aged younger than 40 years and older than 79 years. Similarly, in a large SEER data study of 44,511 women, those aged 65–69 years had a higher rate of mammography adherence than those aged 85 years or older (Keating, Landrum, Guadagnoli, Winer, & Ayanian, 2006), even though the overall trend for the entire dataset was for adherence to decrease with increasing age. Nine additional studies reported the lowest adherence in patients aged older than 70, 75, 80, or 85 years (Carcaise-Edinboro, Bradley, & Dahman, 2010; Doubeni et al., 2006; Etim, Schellhase, Sparapani, & Nattinger, 2006; Field et al., 2008; Giuliani et al., 2016; Keating et al., 2006; Lu et al., 2011; Onega et al., 2012; Sabatino, Thompson, Richardson, & Miller, 2012). For the middle of the age continuum, mammography adherence appears to increase with increasing age. For example, a prospective study showed lowest adherence in the group with a mean age of 50.9 years and highest adherence in the group with a mean age of 60.28 years (Shelby et al., 2012). Further support for this idea was found in two studies that reported the highest adherence in the age ranges of 60–69 and 70–79 years, as compared to 40–49 years (Enewold et al., 2013; Geller et al., 2003).
Ethnicity was a key factor related to mammography adherence in eight studies (Advani et al., 2014; Breslau et al., 2010; Enewold et al., 2013; Etim et al., 2006; Field et al., 2008; Keating et al., 2006; Mandelblatt et al., 2006; Nurgalieva et al., 2013). In five of these studies, African American women showed lower adherence to surveillance mammography than Caucasian women (Advani et al., 2014; Etim et al., 2006; Keating et al., 2006; Mandelblatt et al., 2006; Nurgalieva et al., 2013). The other three studies did not find lower mammography adherence in African American women (Breslau et al., 2010; Enewold et al., 2013; Field et al., 2008). For example, Enewold et al. (2013) reported that during the first year after breast cancer diagnosis, African American women had higher adherence than non-Hispanic Caucasian women, but during the third year, there were no significant differences among ethnic groups.
Economic disadvantage specifically was shown to be a key factor in three studies, measured in terms of place of residence and health insurance. Living in a low-income neighborhood was associated with lower adherence (Giuliani et al., 2016; Keating et al., 2006). Higher adherence was associated with Medicare and private insurance compared to public insurance (Sabatino et al., 2012). One study also identified marital status as a key factor. Specifically, unmarried women were less likely to adhere to surveillance mammography than married women (Keating et al., 2006).
Clinical characteristics: The review revealed seven clinical variables associated with mammography adherence: number of years since diagnosis or treatment completion, type of surgery with or without radiation therapy, cancer stage, comorbid conditions, lymphedema, hormonal therapy, and positive lymph node stage findings. Number of years since diagnosis or treatment completion was associated with surveillance mammography adherence in 13 studies (Buist et al., 2013; Carcaise-Edinboro et al., 2010; Doubeni et al., 2006; Enewold et al., 2013; Field et al., 2008; Giuliani et al., 2016; Keating et al., 2006; Lu et al., 2011; Onega et al., 2012; Sabatino et al., 2012; Schapira, McAuliffe, & Nattinger, 2000; Shelby et al., 2012; Wirtz et al., 2014). The results were consistent regardless of the time point used (diagnosis or treatment completion); all 13 studies reported that longer time since diagnosis or treatment completion was related to lower rates of mammography adherence.
In addition, type of surgery and radiation therapy were both related to surveillance mammography adherence in 11 studies (Carcaise-Edinboro et al., 2010; Doubeni et al., 2006; Enewold et al., 2013; Etim et al., 2006; Field et al., 2008; Geller et al., 2003; Lu et al., 2011; Mandelblatt et al., 2006; Onega et al., 2012; Schapira et al., 2000; Wirtz et al., 2014). Some studies combined surgery type and radiation therapy together for the analysis, and others analyzed the effect of each separately. In general, women who received radiation therapy were more likely to adhere to mammography (Etim et al., 2006; Geller et al., 2003; Lu et al., 2011; Schapira et al., 2000; Wirtz et al., 2014). For example, in a large retrospective study of 2,503 women, Geller et al. (2003) reported that patients who underwent radiation therapy were 2.3 times more likely to adhere to mammography than those who did not undergo radiation therapy. Similarly, adherence was higher in women receiving breast-conserving surgery with radiation therapy, as compared with breast-conserving surgery alone (Carcaise-Edinboro et al., 2010; Doubeni et al., 2006; Enewold et al., 2013; Field et al., 2008; Onega et al., 2012). One study found that survivors receiving endocrine therapy showed lower surveillance mammography adherence (Lu et al., 2011).
All studies reviewed were consistent regarding the effects of breast cancer stage and comorbid conditions. Eight studies showed that survivors with higher-stage cancer at diagnosis were significantly less likely to adhere to surveillance mammography (Doubeni et al., 2006; Etim et al., 2006; Field et al., 2008; Geller et al., 2003; Lu et al., 2011; Onega et al., 2012; Schapira et al., 2000; Wirtz et al., 2014). Regarding comorbid conditions, five studies found that having comorbidities and/or having more severe comorbidities were associated with being less likely to adhere to surveillance mammography (Carcaise-Edinboro et al., 2010; Doubeni et al., 2006; Etim et al., 2006; Lu et al., 2011; Wirtz et al., 2014). Similarly, one study (Shelby et al., 2012) found that upper-extremity lymphedema was associated with lower mammography adherence.
Psychological characteristics: The review revealed four psychological factors affecting mammography adherence: distress specific to breast cancer, fear of recurrence, mammography-related anticipatory anxiety, and worry about mammography pain. One study (Kelly, Bhattacharya, Dickinson, & Hazard, 2015) found that higher distress specific to breast cancer was associated with greater mammography adherence, showing distress to be a motivator in these women (average age = 58.5 years). In contrast, another study (Thewes et al., 2012) reported that higher fear of recurrence was associated with lower adherence. The latter study focused exclusively on younger women (aged 18–45 years) and only early-stage disease (stages 0–II). Fear of recurrence was significantly higher than previously reported in patients of mixed ages and diagnoses. Although higher fear of recurrence was associated with fewer mammograms (and ultrasounds) in this study, it also was associated with a higher frequency of breast self-examinations and unscheduled visits to healthcare providers. Although these two studies (Kelly et al., 2015; Thewes et al., 2012) focused on different types of psychological dysphoria, it is important to note that younger women may experience stronger levels of dysphoria, and lower levels of fear/distress may motivate adherence, while higher levels may be immobilizing.
One study assessed specific mammography-related concerns (Shelby et al., 2012), finding that higher levels of mammography-related anticipatory anxiety and worry about mammography pain were both associated with lower adherence. Actual pain experienced during mammography was not associated with lower adherence, although 95% reported it (55% mild and 40% moderate or severe). Instead, it was thoughts about pain during the mammogram itself that was significantly associated with lower adherence, such as fear that the pain would get worse.
Health behavior: The review revealed one health behavior factor associated with mammography adherence, which was that current smokers are less likely to be adherent (Wirtz et al., 2014). Of note, the effect was only seen for current smokers; there was no effect for former smokers who were not currently smoking.
Healthcare System Factors Influencing Surveillance Mammography Adherence
Three healthcare factors influenced surveillance mammography adherence, all of which depend on healthcare accessibility and availability: healthcare provider, enrollment in a medical home program, and travel time to access health care. Seven studies showed that visiting a healthcare provider was a predictor of mammography adherence (Doubeni et al., 2006; Etim et al., 2006; Field et al., 2008; Keating et al., 2006; Sabatino et al., 2012; Snyder et al., 2009; Wirtz et al., 2014). Generally, across the seven studies, seeing any provider during the year increased the likelihood of adherence. Three studies also showed an effect for type of provider, with increased surveillance mammography in women visiting cancer specialists, such as medical oncologists, general surgeons, and radiation oncologists (Field et al., 2008; Keating et al., 2006; Snyder et al., 2009).
Only two additional studies reported effects for healthcare accessibility and availability. One study (Wheeler et al., 2013) found that enrollment in a medical home program resulted in significantly better annual mammography adherence. These breast cancer survivors were vulnerable populations who were insured by Medicaid and were provided with primary care case management. The other study showed that lower adherence to annual surveillance mammography was independently related to having to travel longer than 30 minutes to access healthcare services (Giuliani et al., 2016).
Discussion
Twenty-three original research studies (published from 2000 to 2017) were reviewed to identify factors that either promote or inhibit participation in surveillance mammography in breast cancer survivors. Nineteen factors were identified from the review, which formed the basis for a new conceptual model of predictors of mammography adherence. In this conceptual model, the factors are grouped according to whether they related primarily to the women themselves (individual factors) or the healthcare system.
Individual Factors
Four sociodemographic characteristics were identified as influencing factors, including age, ethnicity, socioeconomic status, and marital status. Regarding age, studies revealed that older adult breast cancer survivors were less likely to adhere to surveillance mammography. Even among older adult breast cancer survivors, it has been shown that having mammograms within a one- or two-year time interval results in lower mortality rates, as compared with no mammograms (Schootman, Jeffe, Lian, Aft, & Gillanders, 2008). The growing risks of recurrence and mortality with advancing age highlight the need for greater clinical attention to older adult survivors, as well as additional research on how to increase their mammography adherence.
Ethnicity was also a key factor related to adherence to surveillance mammography in the studies reviewed. For example, African American women were less likely than Caucasian women to be adherent (Advani et al., 2014; Mandelblatt et al., 2006; Nurgalieva et al., 2013). Ethnicity is a complex factor; it not only influences mammography adherence, but is also associated with persistent variations in cancer incidence and mortality in the United States. The most recent data available show that breast cancer mortality in non-Hispanic African American women is 8% higher than in non-Hispanic Caucasian women, even though non-Hispanic African American women have a 4% lower incidence (Siegel et al., 2019). The co-occurrence of economic disadvantage and ethnicity in the United States makes it difficult or impossible to disentangle them, but the negative effect on mammography adherence is clear. The studies reviewed also showed that living in a low-income neighborhood and having public health insurance or no health insurance was associated with nonadherence.
Regarding clinical factors, greater passage of time since diagnosis or treatment completion was related to lower rates of surveillance mammography adherence in all 13 studies reviewed. Although studies varied in the time parameters used, the relationship was consistent: the longer the time since diagnosis, the less likely women were to be adherent. Given the risk of recurrence or second primary cancers, there is a need for increased efforts to promote regular surveillance in long-term survivors.
Survivors who received radiation therapy were significantly more likely to adhere to surveillance mammography (10 studies), and those with a higher cancer stage at diagnosis were less likely (8 studies) to adhere. The two clinical factors are interrelated, because breast-conserving surgery with radiation therapy is normally an option only for women with earlier-stage disease. In addition, the number and severity of comorbidities decreased the likelihood of adherence (eight studies). Upper-extremity lymphedema also was found to be associated with nonadherence. Previous studies have reported that lymphedema was related to physical and functional status, including disability (Pyszel, Malyszczak, Pyszel, Andrzejak, & Szuba, 2006) and reduced function, lessened strength, fatigue, and arm pain (Taghian, Miller, Jammallo, O’Toole, & Skolny, 2014). The clinical picture across the reviewed studies suggests that women with the worst health are least likely to be adherent to mammography, so they are in greatest need of additional efforts to increase surveillance for new and recurrent cancers.
Regarding psychological factors, higher levels of breast cancer distress were a motivator for adherence in cancer survivors, but very high levels of fear of recurrence appear to be immobilizing. The highest levels of fear occurred in younger women. Fear of breast cancer recurrence can be amplified or reactivated by several triggers, such as follow-up medical visits and the experience of physical symptoms (Gil et al., 2004). In addition, the fear can be long-lasting, with breast cancer survivors experiencing fear of recurrence over long-term periods of survival (Koch, Jansen, Brenner, & Arndt, 2013). Additional research is needed to better understand the nature of psychological dysphoria, to assist patients in managing and mitigating feelings of fear and distress, particularly for those experiencing immobilizing levels.
Regarding health behavior, the single characteristic affecting adherence was being a current smoker. In the general population, cigarette smoking and breast and cervical cancer screening have been found to be related on a fairly consistent basis across ethnicities, with current smokers being less likely to report having had a recent mammogram (Selvin & Brett, 2003). There is not enough evidence to conclude that current smoking directly influences surveillance mammography adherence, but as one aspect of health behavior, smoking could serve as a risk factor to help identify patients at higher risk for nonadherence.
Healthcare System Factors
Regarding healthcare accessibility, eight studies showed that having a regular healthcare provider or medical home increased mammography adherence, even among low-income women. Seeing any provider during the previous year increased adherence, with visits to cancer specialists having the strongest effect. Needing to travel longer than 30 minutes to healthcare services had a negative effect on adherence. In a related study, Kukar, Watroba, Miller, Kumar, and Edge (2014) observed that the type of healthcare provider visited influenced the regularity of survivorship care. The current review adds to the growing body of evidence showing the importance of a medical home, conveniently located, particularly in terms of promoting early detection of new and recurrent cancers.
Limitations
The current literature review focused only on factors affecting breast cancer survivors’ adherence to surveillance mammography and did not address many other vital follow-up procedures. Although the approach allowed identification of key factors affecting mammography adherence, survivorship care for breast cancer takes many forms and can include general preventive care, comorbidity management, general clinical breast examinations by healthcare providers, and screening for other cancers. Future studies may examine whether the factors identified in this study influence participation in a broader range of survivorship care activities.
The authors limited their search to studies published in English. Of the 23 studies reviewed, U.S. studies were by far the most common (87%). U.S. healthcare systems and policies differ from those of other countries, and healthcare availability and accessibility play important roles in surveillance mammography adherence, which limits generalizability to other countries and cultures. Barriers and facilitators for cancer screening may differ by nationality and ethnicity (Hirth, Laz, Rahman, & Berenson, 2016; Yaghjyan, Wolin, Chang, & Colditz, 2014).
Implications for Nursing
Based on the integrative review presented in this article, a new conceptual model of predictors of mammography adherence was developed, encompassing the 19 factors found to influence adherence to mammography in breast cancer survivors. The model captures the most current understanding of the factors that either promote or inhibit participation in mammography, as recommended for early detection of new and recurrent cancers. In clinical practice, the model may be used to create profiles of individuals at greatest risk for nonadherence, which then could be used to create screeners to identify women who may benefit from additional follow-up. In addition, the model provides a starting point for future research, to guide new studies examining the effect of these factors in greater detail, as well as to develop and test interventions to mitigate their negative effects.
Many of the individual factors identified in this review are not amenable to change, such as age, ethnicity, years since diagnosis, cancer stage, type of treatment, and poor health status. Awareness of these factors may be valuable in clinical practice for taking preemptive action, by identifying women likely to be at higher risk for nonadherence. For instance, assistance in finding low-cost or no-cost mammograms may be provided to women with low incomes or without adequate health insurance before they even complete treatment. Other individual factors may be directly amenable to nursing intervention, such as fear of recurrence, distress related to breast cancer, and mammography-related anxiety. Because very high levels of these dysphoric states can be immobilizing, therapeutic strategies to manage these emotions may result in an increased ability to participate in screening at regular recommended intervals.
Healthcare system factors also provide a means for potentially increasing mammography adherence in cancer survivors. One of the most powerful facilitators was having a medical home, with a healthcare provider who was seen on an annual basis. Interventions that increase access to and engagement in primary health care provided by nurses and physicians are particularly promising for increasing adherence in breast cancer survivors.
Given that nonadherence tends to increase over time, there is a need for ongoing education about the crucial importance of continuing mammography for early detection of new and recurrent cancers. The consistency of this finding across studies shows that the current educational efforts are not effective enough and new innovative approaches are needed to engage patients and their families more effectively.
The review revealed steadily growing scientific interest in surveillance mammography adherence, with increasing numbers of studies published over time, and U.S. studies being by far the most common. Considering that breast cancer is the most commonly diagnosed cancer in women worldwide, and given the importance of mammography in early detection of recurrence, additional research is urgently needed beyond the United States to investigate the potentially large differences in adherence barriers and facilitators between cultures and healthcare systems in other countries as well. 
Conclusion
Covering an 18-year span, this integrative review contributes to a more comprehensive understanding of factors influencing adherence and their multidimensional nature. Nineteen key factors influencing surveillance mammography adherence were identified and subsequently synthesized into a new conceptual model of predictors of adherence in breast cancer survivors. The detailed information provided in this review, along with the new model, provide guidance for clinical practice and future research, both in helping to identify individuals at greatest risk for nonadherence, as well as developing new interventions to address barriers to regular mammography screening. Ultimately, the model can be used in survivorship care to improve breast cancer survivors’ adherence to surveillance mammography and, therefore, can contribute to early detection of new and recurrent cancers and improved survival rates.
The authors gratefully acknowledge the assistance of Rebecca Raszewski, MS, AHIP, with the database search performed for this study. They also gratefully acknowledge Jon Mann, MA, for editorial assistance.
About the Author(s)
Min Kyeong Jang, PhD, KOAPN, RN, is a postdoctoral fellow and Patricia E. Hershberger, PhD, RN, FNP-BC, FAAN, is an associate professor, both in the College of Nursing at the University of Illinois at Chicago; Sue Kim, PhD, RN, is a professor in the Mo-Im Kim Nursing Research Institute in the College of Nursing at Yonsei University in Seoul Korea; and Eileen G. Collins, PhD, RN, FAACVPR, FAAN, ATSF, is a professor and associate dean for research, Lauretta T. Quinn, PhD, RN, FAAN, FAHA, CDE, is a clinical professor, Chang Gi Park, PhD, is an assistant research professor and senior biostatistician, and Carol Estwing Ferrans, PhD, RN, FAAN, is a professor and the Harriet H. Werley Endowed Chair in Nursing Research, all in the College of Nursing at the University of Illinois at Chicago. This study was funded, in part, by the National Institute of Nursing Research of the National Institutes of Health (K24NR015340), the Sigma Alpha Lambda Chapter, and the PhD Research Award from the College of Nursing at the University of Illinois at Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Jang, Hershberger, Kim, Collins, and Ferrans contributed to the conceptualization and design. Jang, Hershberger, and Ferrans completed the data collection. Jang, Hershberger, and Park provided statistical support. Jang, Hershberger, Kim, Park, and Ferrans provided the analysis. All authors contributed to the manuscript preparation. Jang can be reached at mjang21@uic.edu, with copy to ONFEditor@ons.org. (Submitted January 2019. Accepted April 1, 2019.)
References
Advani, P.S., Ying, J., Theriault, R., Melhem-Bertrand, A., Moulder, S., Bedrosian, I., . . . Brewster, A.M. (2014). Ethnic disparities in adherence to breast cancer survivorship surveillance care. Cancer, 120, 894–900. https://doi.org/10.1002/cncr.28490
Andersen, M.R., Bowen, D.J., Morea, J., Stein, K.D., & Baker, F. (2009). Involvement in decision-making and breast cancer survivor quality of life. Health Psychology, 28, 29–37. https://doi.org/10.1037/0278-6133.28.1.29
Breslau, E.S., Jeffery, D.D., Davis, W.W., Moser, R.P., McNeel, T.S., & Hawley, S. (2010). Cancer screening practices among racially and ethnically diverse breast cancer survivors: Results from the 2001 and 2003 California Health Interview Survey. Journal of Cancer Survivorship, 4, 1–14. https://doi.org/10.1007/s11764-009-0102-5
Buist, D.S., Bosco, J.L., Silliman, R.A., Gold, H.T., Field, T., Yood, M.U., . . . Lash, T.L. (2013). Long-term surveillance mammography and mortality in older women with a history of early stage invasive breast cancer. Breast Cancer Research and Treatment, 142, 153–163. https://doi.org/10.1007/s10549-013-2720-x
Carcaise-Edinboro, P., Bradley, C.J., & Dahman, B. (2010). Surveillance mammography for Medicaid/Medicare breast cancer patients. Journal of Cancer Survivorship, 4, 59–66. https://doi.org/10.1007/s11764-009-0107-0
Doubeni, C.A., Field, T.S., Ulcickas Yood, M., Rolnick, S.J., Quessenberry, C.P., Fouayzi, H., . . . Wei, F. (2006). Patterns and predictors of mammography utilization among breast cancer survivors. Cancer, 106, 2482–2488. https://doi.org/10.1002/cncr.21893
Duffy, C.M., Clark, M.A., & Allsworth, J.E. (2006). Health maintenance and screening in breast cancer survivors in the United States. Cancer Detection and Prevention, 30, 52–57. https://doi.org/10.1016/j.cdp.2005.06.012
Enewold, L., McGlynn, K.A., Zahm, S.H., Jatoi, I., Anderson, W.F., Gill, A.A., . . . Zhu, K. (2013). Surveillance mammography among female Department of Defense beneficiaries: A study by race and ethnicity. Cancer, 119, 3531–3538. https://doi.org/10.1002/cncr.28242
Etim, A.E., Schellhase, K.G., Sparapani, R., & Nattinger, A.B. (2006). Effect of model of care delivery on mammography use among elderly breast cancer survivors. Breast Cancer Research and Treatment, 96, 293–299. https://doi.org/10.1007/s10549-005-9141-4
Ferlay, J., Colombet, M., Soerjomataram, I., Mathers, C., Parkin, D.M., Piñeros, M., . . . Bray, F. (2019). Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. International Journal of Cancer, 144, 1941–1953. https://doi.org/10.1002/ijc.31937
Field, T.S., Doubeni, C., Fox, M.P., Buist, D.S., Wei, F., Geiger, A.M., . . . Silliman, R.A. (2008). Under utilization of surveillance mammography among older breast cancer survivors. Journal of General Internal Medicine, 23, 158–163. https://doi.org/10.1007/s11606-007-0471-2
Geller, B.M., Kerlikowske, K., Carney, P.A., Abraham, L.A., Yankaskas, B.C., Taplin, S.H., . . . Barlow, W.E. (2003). Mammography surveillance following breast cancer. Breast Cancer Research and Treatment, 81, 107–115. https://doi.org/10.1023/a:1025794629878
Gil, K.L., Mishel, M., Belyea, M., Germino, B., Porter, L.S., LaNey, I.C., & Stewart, J. (2004). Triggers of uncertainty about recurrence and long-term treatment side effects in older African American and Caucasian breast cancer survivors. Oncology Nursing Forum, 31, 633–639. https://doi.org/10.1188/04.onf.633-639
Giuliani, O., Mancini, S., Puliti, D., Caranci, N., Ravaioli, A., Vattiato, R., . . . Falcini, F. (2016). Patterns and determinants of receipt of follow-up mammography and/or clinical examination in a cohort of Italian breast cancer survivors. Breast Cancer Research and Treatment, 158, 543–551. https://doi.org/10.1007/s10549-016-3895-8
Gradishar, W.J., Anderson, B.O., Balassanian, R., Blair, S.L., Burstein, H.J., Cyr, A., . . . Shead, D.A. (2018). Breast cancer, version 4.2017, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network, 16, 310–320. https://doi.org/10.6004/jnccn.2018.0012
Grunfeld, E., Noorani, H., McGahan, L., Paszat, L., Coyle, D., van Walraven, C., . . . Sawka, C. (2002). Surveillance mammography after treatment of primary breast cancer: A systematic review. Breast, 11, 228–235. https://doi.org/10.1054/brst.2001.0404
Hirth, J.M., Laz, T.H., Rahman, M., & Berenson, A.B. (2016). Racial/ethnic differences affecting adherence to cancer screening guidelines among women. Journal of Women’s Health, 25, 371–380. https://doi.org/10.1089/jwh.2015.5270
Holden, A.E., Ramirez, A.G., & Gallion, K. (2014). Depressive symptoms in Latina breast cancer survivors: A barrier to cancer screening. Health Psychology, 33, 242–248. https://doi.org/10.1037/a0032685
Jerome-D’Emilia, B. (2015). A systematic review of barriers and facilitators to mammography in Hispanic women. Journal of Transcultural Nursing, 26, 73–82. https://doi.org/10.1177/1043659614530761
Keating, N.L., Landrum, M.B., Guadagnoli, E., Winer, E.P., & Ayanian, J.Z. (2006). Factors related to underuse of surveillance mammography among breast cancer survivors. Journal of Clinical Oncology, 24, 85–94. https://doi.org/10.1200/jco.2005.02.4174
Kelly, K.M., Bhattacharya, R., Dickinson, S., & Hazard, H. (2015). Health behaviors among breast cancer patients and survivors. Cancer Nursing, 38(3), E27–E34. https://doi.org/10.1097/NCC.0000000000000167
Koch, L., Jansen, L., Brenner, H., & Arndt, V. (2013). Fear of recurrence and disease progression in long-term (≥ 5 years) cancer survivors—A systematic review of quantitative studies. Psycho-Oncology, 22, 1–11. https://doi.org/10.1002/pon.3022
Kukar, M., Watroba, N., Miller, A., Kumar, S., & Edge, S.B. (2014). Fostering coordinated survivorship care in breast cancer: Who is lost to follow-up? Journal of Cancer Survivorship, 8, 199–204. https://doi.org/10.1007/s11764-013-0323-5
Lu, W., Jansen, L., Schaapveld, M., Baas, P.C., Wiggers, T., & De Bock, G.H. (2011). Underuse of long-term routine hospital follow-up care in patients with a history of breast cancer? BMC Cancer, 11, 279. https://doi.org/10.1186/1471-2407-11-279
Magai, C., Consedine, N., Neugut, A.I., & Hershman, D.L. (2007). Common psychosocial factors underlying breast cancer screening and breast cancer treatment adherence: A conceptual review and synthesis. Journal of Women’s Health, 16, 11–23. https://doi.org/10.1089/jwh.2006.0024
Mandelblatt, J.S., Lawrence, W.F., Cullen, J., Stanton, A.L., Krupnick, J.L., Kwan, L., & Ganz, P.A. (2006). Patterns of care in early-stage breast cancer survivors in the first year after cessation of active treatment. Journal of Clinical Oncology, 24, 77–84. https://doi.org/10.1200/jco.2005.02.2681
Melnyk, B.M., & Fineout-Overholt, E. (2015). Box 1.3: Rating system for the hierarchy of evidence for intervention/treatment questions. Evidence-based practice in nursing and healthcare: A guide to best practice (3rd ed., p. 11). Philadelphia, PA: Wolters Kluwer Health
National Cancer Institute. (2019). Cancer stat facts: Female breast cancer. Retrieved from http://seer.cancer.gov/statfacts/html/breast.html
Nurgalieva, Z.Z., Franzini, L., Morgan, R., Vernon, S.W., Liu, C.C., & Du, X.L. (2013). Surveillance mammography use after treatment of primary breast cancer and racial disparities in survival. Medical Oncology, 30, 691. https://doi.org/10.1007/s12032-013-0691-8
Onega, T., Weiss, J., diFlorio, R., MacKenzie, T., Goodrich, M., & Poplack, S. (2012). Evaluating surveillance breast imaging and biopsy in older breast cancer survivors. International Journal of Breast Cancer, 2012, 347646. https://doi.org/10.1155/2012/347646
Pyszel, A., Malyszczak, K., Pyszel, K., Andrzejak, R., & Szuba, A. (2006). Disability, psychological distress and quality of life in breast cancer survivors with arm lymphedema. Lymphology, 39, 185–192.
Ruddy, K.J., Sangaralingham, L., Freedman, R.A., Mougalian, S.S., Neuman, H., Greenberg, C., . . . Shah, N.D. (2018). Adherence to guidelines for breast surveillance in breast cancer survivors. Journal of the National Comprehensive Cancer Network, 16, 526–534. https://doi.org/10.6004/jnccn.2018.7001
Sabatino, S.A., Thompson, T.D., Richardson, L.C., & Miller, J. (2012). Health insurance and other factors associated with mammography surveillance among breast cancer survivors: Results from a national survey. Medical Care, 50, 270–276. https://doi.org/10.1097/mlr.0b013e318244d294
Schapira, M.M., McAuliffe, T.L., & Nattinger, A.B. (2000). Underutilization of mammography in older breast cancer survivors. Medical Care, 38, 281–289. https://doi.org/10.1097/00005650-200003000-00005
Schootman, M., Jeffe, D.B., Lian, M., Aft, R., & Gillanders, W.E. (2008). Surveillance mammography and the risk of death among elderly breast cancer patients. Breast Cancer Research and Treatment, 111, 489–496. https://doi.org/10.1007/s10549-007-9795-1
Schueler, K.M., Chu, P.W., & Smith-Bindman, R. (2008). Factors associated with mammography utilization: A systematic quantitative review of the literature. Journal of Women’s Health, 17, 1477–1498. https://doi.org/10.1089/jwh.2007.0603
Selvin, E., & Brett, K.M. (2003). Breast and cervical cancer screening: Sociodemographic predictors among White, Black, and Hispanic women. American Journal of Public Health, 93, 618–623. https://doi.org/10.2105/ajph.93.4.618
Shelby, R.A., Scipio, C.D., Somers, T.J., Soo, M.S., Weinfurt, K.P., & Keefe, F.J. (2012). Prospective study of factors predicting adherence to surveillance mammography in women treated for breast cancer. Journal of Clinical Oncology, 30, 813–819. https://doi.org/10.1200/jco.2010.34.4333
Siegel, R.L., Miller, K.D., & Jemal, A. (2019). Cancer statistics, 2019. CA: A Cancer Journal for Clinicians, 69, 7–34. https://doi.org/10.3322/caac.21551
Snyder, C.F., Frick, K.D., Kantsiper, M.E., Peairs, K.S., Herbert, R.J., Blackford, A.L., . . . Earle, C.C. (2009). Prevention, screening, and surveillance care for breast cancer survivors compared with controls: Changes from 1998 to 2002. Journal of Clinical Oncology, 27, 1054–1061. https://doi.org/10.1200/jco.2008.18.0950
Taghian, N.R., Miller, C.L., Jammallo, L.S., O’Toole, J., & Skolny, M.N. (2014). Lymphedema following breast cancer treatment and impact on quality of life: A review. Critical Reviews in Oncology/Hematology, 92, 227–234. https://doi.org/10.1016/j.critrevonc.2014.06.004
Tejeda, S., Darnell, J.S., Cho, Y.I., Stolley, M.R., Markossian, T.W., & Calhoun, E.A. (2013). Patient barriers to follow-up care for breast and cervical cancer abnormalities. Journal of Women’s Health, 22, 507–517. https://doi.org/10.1089/jwh.2012.3590
Thewes, B., Butow, P., Bell, M.L., Beith, J., Stuart-Harris, R., Grossi, M., . . . Dalley, D. (2012). Fear of cancer recurrence in young women with a history of early-stage breast cancer: A cross-sectional study of prevalence and association with health behaviours. Supportive Care in Cancer, 20, 2651–2659. https://doi.org/10.1007/s00520-011-1371-x
Wheeler, S.B., Kohler, R.E., Goyal, R.K., Lich, K.H., Lin, C.C., Moore, A., . . . Domino, M.E. (2013). Is medical home enrollment associated with receipt of guideline-concordant follow-up care among low-income breast cancer survivors? Medical Care, 51, 494–502. https://doi.org/10.1097/mlr.0b013e31828d4d0c
Whittemore, R., & Knafl, K. (2005). The integrative review: Updated methodology. Journal of Advanced Nursing, 52, 546–553.
Wirtz, H.S., Boudreau, D.M., Gralow, J.R., Barlow, W.E., Gray, S., Bowles, E.J., & Buist, D.S. (2014). Factors associated with long-term adherence to annual surveillance mammography among breast cancer survivors. Breast Cancer Research and Treatment, 143, 541–550. https://doi.org/10.1007/s10549-013-2816-3
Yaghjyan, L., Wolin, K., Chang, S.H., & Colditz, G. (2014). Racial disparities in healthy behaviors and cancer screening among breast cancer survivors and women without cancer: National Health Interview Survey 2005. Cancer Causes and Control, 25, 605–614. https://doi.org/10.1007/s10552-014-0365-7




