Using Web-Based Interventions to Support Caregivers of Patients With Cancer: A Systematic Review
Purpose/Objectives: To explore the literature to examine the physical, social, psychological, financial, usability, and feasibility outcomes of web-based interventions on caregivers of people with cancer and to identify potential trends in this body of evidence.
Data Sources: PubMed, CINAHL®, PsycINFO®, and Inspec.
Data Synthesis: Six articles met inclusion criteria. Across studies, most caregivers were middle-aged female spouses with some college attendance who felt “somewhat comfortable” using the Internet. Caregiver interventions used single- and multicomponent services and reduced negative mood.
Conclusions: Web-based caregiver interventions can be beneficial in offering information and support and may positively influence the social and psychological outcomes in this population.
Implications for Nursing: Many studies described caregiver Internet usage and interventional perceptions and needs, but few have examined the impact of web-based interventions on caregivers. More research is needed to produce high-quality evidence in this population.
Jump to a section
An estimated 1.66 million individuals will be diagnosed with cancer in the United States in 2015 (American Cancer Society, 2015). Many will require aid from a family caregiver, contributing to about 66 million people who serve as unpaid caregivers to someone who is ill, disabled, or older aged (National Alliance for Caregiving & AARP, 2009). The responsibilities of caregivers of patients with cancer can include physical care and mobility assistance, management of symptoms, distribution of medications and monitoring side effects, providing emotional support, decision making, and communication with family members about disease status and progression. Although unpaid caregivers often attain satisfaction from engaging in these responsibilities to reduce suffering for their loved ones, caregiving is associated with physical, social, and emotional burdens such as increased blood pressure, heart attack scares, arthritis flare-ups, acid reflux, headaches, role strain, isolation, anxiety, sexual issues, fatigue, and added demands that can affect work performance (Collins & Swartz, 2011; Evercare & National Alliance for Caregiving, 2006; Stenberg, Ruland, & Miaskowski, 2010). Caregivers also have significantly higher levels of depression than their non-caregiver counterparts (Pinquart & Sörensen, 2003). In addition to the concomitant morbidities, caregiving can greatly influence mortality. According to a seminal study by Schulz and Beach (1999), strained elderly spousal caregivers were 63% more likely to die within four years than non-caregivers. Caregiving reduces work productivity by 19% and increases the likelihood of the caregiver leaving the workplace, resulting in a loss of wages, health insurance, job benefits, retirement savings or investments, and Social Security benefits (Family Caregiver Alliance, 2012). The negative impact of caregiving reported throughout the literature necessitates the need for interventional services.
Background
Gaugler et al. (2009) suggested that having adequate support networks could help to prevent feelings of loneliness, isolation, and other depressive symptoms associated with cancer care. Traditional interventions to address caregiver burdens, delivered in person or by telephone, have been widely studied. These interventions can encompass a variety of modalities including psychoeducation, problem solving and skills building, supportive therapy, family or couples therapy, cognitive-behavioral therapy, complementary and alternative medicine, and existential therapy (Applebaum & Breitbart, 2013). Several systematic reviews and meta-analyses have shown the positive effects of traditional interventions on caregiver psychological and emotional health, well-being, knowledge of disease process and required care, quality of life, ability to cope, and self-efficacy (Applebaum & Breitbart, 2013; Northouse, Katapodi, Song, Zhang, & Mood, 2010; Sörensen, Pinquart, & Duberstein, 2002).
Although traditional interventions have proven to be beneficial, they can be time-consuming and expensive for caregivers. Caregivers may not want to or be able to find respite care while they attend sessions, and attendance may require that the caregiver take time off work. A systematic review of interventions for cancer caregivers (Applebaum & Breitbart, 2013) revealed a growing number of interventions for this population but identified caregivers of patients with cancer as underserved and difficult to reach, suggesting that alternate modalities, such as the Internet, may be a solution to address this disparity. The time and financial commitment associated with traditional interventions are barriers to cancer caregivers who seek help for physical, social, and emotional burdens and present a gap in healthcare delivery for this population.
Web-based interventions have the potential to reduce these barriers by offering tailored information that is convenient, timely, and delivered at the preference of the user (DuBenske, Gustafson, Shaw, & Cleary, 2010). Traditional interventions may be adapted to web-based interventions, fulfilling caregiver needs in more practical ways by reducing time, financial restrictions, or other difficulties that may limit access. In other populations, web-based interventions have been successful in addressing these issues. For example, the Comprehensive Health Enhancement Support System (CHESS) intervention, first developed in 1989 and now web-based, is an intervention that consists of information, communication, and coaching, and has been widely studied in various populations (Robbins, 1999), including people with HIV (Temesgen, Knappe-Langworthy, St. Marie, Smith, & Dierkhising, 2006), people with alcohol dependence (McTavish, Chih, Shah, & Gustafson, 2012), and women with breast cancer (Owens & Robbins, 1996). The CHESS intervention has shown that underprivileged populations use the program about the same amount as more affluent populations (Gustafson et al., 2002), thus helping to bridge the financial gap in care. In addition, other web-based interventions have been proven to be efficacious in chronic health conditions. A meta-analysis of formal computer-mediated support groups showed that participation in a web-based support intervention comprised of educational and group communication components led to increased social support, decreased depression, increased quality of life, and increased self-efficacy for patients who are managing their health conditions (Rains & Young, 2009). Web-based interventions have been effective in these other populations and may also be beneficial for cancer caregivers.
Although the Internet has the potential to address inadequacies in the current healthcare system, little research has been conducted that examines outcomes of web-based interventions in cancer caregivers. The specific benefits and challenges of web-based interventions have yet to be comprehensively addressed in the literature. Determining how this modality may affect caregivers is critical to providing clinicians with the knowledge needed to mitigate or eliminate the negative sequelae linked to caregiving. Therefore, the purpose of this review was to explore the nursing, psychological, social science, and technology literature to examine the physical, social, psychological, and financial outcomes of web-based informational and supportive interventions in caregivers of patients with cancer and to identify trends in this body of evidence regarding feasibility and usability.
Methods
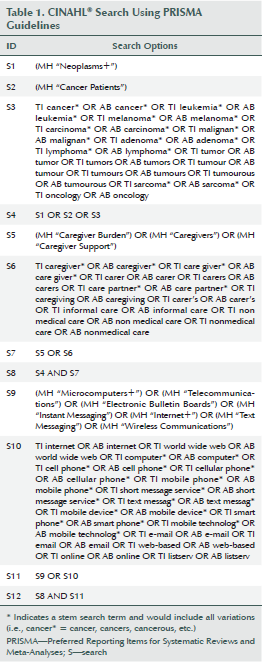
Electronic searches were performed in PubMed, EBSCOhost CINAHL®, Ovid PsycINFO®, and Inspec (Engineering Village) from the earliest available dates in each database through February 1, 2014. The searches used subject headings and free-text terms to represent the main topic concepts (caregivers, cancer, web-based), and were developed in collaboration with a medical librarian. The CINAHL search can be viewed in Table 1. Reference lists of eligible articles were reviewed to identify additional studies not captured by the initial searches.
Articles were included if they (a) reported on studies of caregivers of adult patients with cancer aged 18 years or older, (b) were published in English, (c) were published before February 1, 2014, (d) examined web-based informational or supportive interventions for cancer caregivers, and (e) were quantitative. Web-based informational or supportive interventions were defined as those that used the Internet for delivery, such as online support groups, caregiver forums, virtual communities, smartphone applications, or online platforms for caregiver information. Mixed-methods studies were included based on their quantitative element. Qualitative studies, conference abstracts, dissertations, case studies, and studies that examined caregivers of pediatric patients or used telemedicine or telephone-based interventions were excluded. Systematic reviews and meta-analyses generated by the searches were reviewed to identify additional sources of original studies.
Two independent reviewers screened all records for inclusion using an eligibility form. Using a data extraction form, two reviewers extracted data from included studies. Information extracted from each article included study, participant, and outcome characteristics. Both reviewers independently read each record and identified relevant evidence regarding the categories of interest. The quality of included articles was assessed independently by two reviewers using the McMaster Quality Assessment Tool for Quantitative Studies (Effective Public Health Practice Project [EPHPP], 2010; Thomas, Ciliska, Dobbins, & Micucci, 2004). All disagreements regarding inclusion, data extraction, and quality assessment were resolved by consensus.
Results
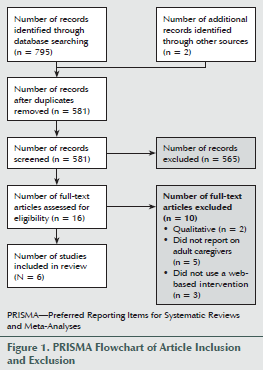
A total of 795 articles were captured by the literature searches with two additional records retrieved from reference list review. After deletion of duplicates, titles and abstracts of 581 articles were screened for inclusion. Sixteen full-text articles were screened to confirm eligibility, with 10 failing to meet inclusion criteria during in-depth review. Six studies were included in the systematic review (see Figure 1). Percent agreement for article inclusion among screeners was 99.48%.
The included articles were limited in generalizability and quality. Half of the studies described random assignment. All six studies had weak global ratings based on the McMaster tool (EPHPP, 2010). Withdrawal and attrition was not described in two studies (Farnham et al., 2002; Zulman et al., 2012), two studies had an attrition rate of 21%–40% (Chih et al., 2013; Scott & Beatty, 2013), and an additional two studies reported attrition rates of greater than 40% (DuBenske et al., 2014; Namkoong et al., 2012). Initial percent agreement among screeners for article quality was 33%. Variations in screening were because of oversight and differences in interpretation of study and McMaster criteria (EPHPP, 2010). All discrepancies were reconciled by a process of consensus discussion that was implemented according to the instruction manual for the tool (EPHPP, 2009), resulting in 100% agreement.
Characteristics of Studies
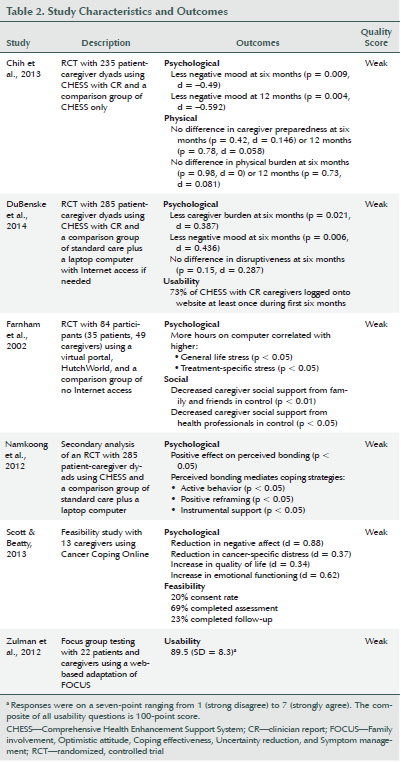
Study design differed among the six articles. Three of the studies (Chih et al., 2013; DuBenske et al., 2014; Farnham et al., 2002) described random assignment to intervention and control groups, one study (Namkoong et al., 2012) was a secondary analysis of a randomized, controlled trial, one study (Scott & Beatty, 2013) described feasibility testing, and one study (Zulman et al., 2012) described focus group testing with reported quantitative data. The number of participants in each study ranged from 13–285.
Each of the studies involved administering an intervention over the Internet, but the approaches varied, ranging from single- to multicomponent modalities. Three studies used CHESS, one study used a virtual portal (HutchWorld), one study used a web-based cognitive behavioral therapy program (Cancer Coping Online), and one study reported on a web-based adaptation of the Family involvement, Optimistic attitude, Coping effectiveness, Uncertainty reduction, and Symptom management (FOCUS) program. Table 2 outlines the characteristics of each study.
CHESS is a multicomponent intervention, consisting of information, communication, and coaching and training services (Chih et al., 2013; DuBenske et al., 2014; Namkoong et al., 2012). Information services included frequently asked questions, links to full-text articles, a resource directory for local and national services, links for high-quality websites, summaries of recent cancer news and research, personal stories of patients and caregivers, and caregiver tips (DuBenske et al., 2014). Communication services included bulletin board discussion groups, question-and-answer services with a cancer specialist, personal bulletin board and interactive websites, and clinician report (DuBenske et al., 2014). Coaching and training services include data about the patient’s health status, decision aids, cognitive behavioral therapy principles, healthy communication techniques, and guidance for creating an action plan (DuBenske et al., 2014).
The virtual portal, HutchWorld, is a multicomponent intervention composed of a social interaction service, information, and diversionary activities within a three-dimensional environment that was modeled after an outpatient lobby (Farnham et al., 2002). Social interaction tools allowed users to engage in communication via messaging systems, bulletin boards, sending e-gifts and emails, and creating a page on a website (Farnham et al., 2002). Information was provided on HutchWorld through a “web pane” and included contact information, links to the Hutch website, and other cancer-related websites (Farnham et al., 2002). Diversionary activities included playing online games, browsing the Internet, and interacting with sculptures in the three-dimensional environment to create music (Farnham et al., 2002).
Cancer Coping Online is a single-component information intervention (Scott & Beatty, 2013). This intervention is a password-protected cognitive behavioral therapy program consisting of psychoeducation, worksheets, and survivor testimonials (Scott & Beatty, 2013). The program was developed for patients, so caregivers were asked to take the patient’s perspective for sections of the program that were not directly related to caregiving (Scott & Beatty, 2013).
FOCUS is a multicomponent information and support program for patients with cancer and caregivers (Zulman et al., 2012). The program includes five core modules, including family involvement, optimistic attitude, coping effectiveness, uncertainty reduction, and symptom management. The traditional form of the intervention is delivered by nurses during three home visits and two telephone calls; however, the web-based adaptation provides communication and support via the Internet (Zulman et al., 2012). The program directs questions to patients and caregivers individually and together. The intervention provided tailored feedback based on user response (Zulman et al., 2012).
Caregiver Demographics
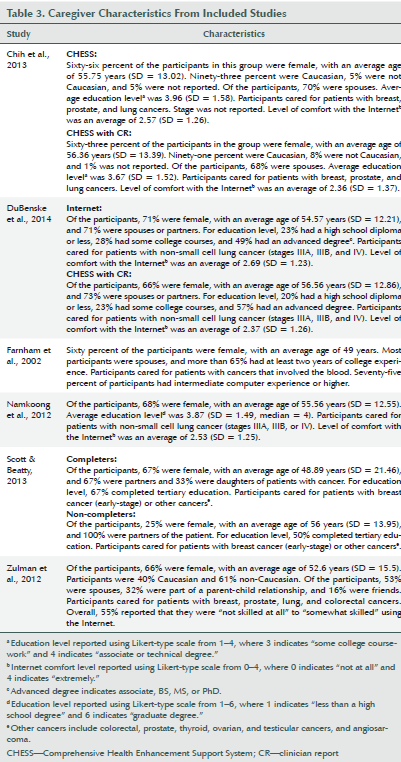
All six articles provided basic information about caregiver participants, including the mean caregiver age, gender, and type of cancer that the patient had. Across studies, the mean caregiver age ranged from 48.9–56.6 years. A majority of caregiver participants were female, with proportions of female participants ranging from 60%–71%. Articles reported on caregivers of patients with breast, prostate, lung, blood, colorectal, thyroid, ovarian, and testicular cancers, with half of the studies reporting on patients with lung cancer. The second most commonly reported demographics were caregiver relationship, education level, and comfort level with the Internet, with five of six articles reporting on each of these categories. Across all five studies that reported results on caregiver relationship, spouse or partner was the most common role, ranging from 53%–73% of participants. Other caregiver roles included parent-child and friend. Studies that reported caregiver education level revealed that most caregivers were fairly educated, with a majority reporting having attended at least some college. Among the studies that reported level of comfort with the Internet, a majority of caregivers considered themselves to have intermediate computer and Internet experience and felt “somewhat comfortable” using the Internet. Caregiver demographics of each study are summarized in Table 3.
Caregiver Outcomes
Articles reported on psychological (Chih et al., 2013; DuBenske et al., 2014; Farnham et al., 2002; Namkoong et al., 2012; Scott & Beatty, 2013), physical (Chih et al., 2013), social (Farnham et al., 2002), usability (DuBenske et al., 2014; Zulman et al., 2012), and feasibility (Scott & Beatty, 2013) outcomes.
Five of the six articles reported on psychological outcomes for caregivers, including negative mood, caregiver burden, stress, coping strategies, and quality of life. Three of those studies (Chih et al., 2013; DuBenske et al., 2014; Scott & Beatty, 2013) showed reduced negative mood in caregivers who used web-based interventions. Effect sizes of outcomes were assessed for each study as appropriate and were measured using Cohen’s d. This effect size measures the mean differences between two groups. If not reported, effect sizes were calculated using standard equations, with d = 0.2, d = 0.5, and d = 0.8 indicating small, moderate, and large effects, respectively (Polit & Beck, 2008). Dubenske et al. (2014) found that CHESS with caregiver report (CR) has a modest effect on reduction of caregiver burden (d = 0.387) and negative mood (d = 0.436) at six months. In addition, a calculated effect size using data from Chih et al. (2013) also indicated that CHESS with CR has a small-to-moderate effect on reduction of negative mood (d = –0.49) at six months and demonstrated a moderate reduction of negative mood at 12 months (d =–0.592). Scott and Beatty (2013) found that Cancer Coping Online has a large effect on reducing negative mood (d = 0.88). It was not possible to quantify effect sizes for three of the studies (Farnham et al., 2002; Namkoong et al., 2012; Zulman et al., 2012) because calculations were not appropriate; one article (Namkoong et al., 2012) was a secondary analysis of data from the article by DuBenske et al. (2014), one report (Farnham et al., 2002) did not differentiate between patient and caregiver data in the results, and one (Zulman et al., 2012) did not provide enough information for calculation.
Multicomponent inter-ventions (e.g., CHESS, HutchWorld) and single-component interventions (e.g., Cancer Coping Online) affected psychological or social outcomes, such as reduced negative mood and stress in caregivers and social support from family, friends, and healthcare providers, suggesting that information alone or with supportive services, coaching and training, or distraction techniques may improve outcomes in caregivers.
Two of the six studies reported on usability outcomes (DuBenske et al., 2014; Zulman et al., 2012). DuBenske et al. (2014) reported on the number of logins, and Zulman et al. (2012) reported a usability score based on focus group testing. Only one of the studies (Scott & Beatty, 2013) reported on feasibility.
Discussion
The authors searched four databases, screened 581 articles, and conducted an in-depth review of the six articles identified as testing a web-based intervention on caregivers of adults with cancer. The resulting systematic review offers preliminary evidence about the impact of web-based interventions on caregivers of patients with cancer. The authors found that this body of work supports the adaptation of cancer caregiver interventions to a web-based format.
Several of the studies reviewed demonstrated that web-based interventions may positively influence caregivers with regard to social and psychological outcomes, suggesting that caregivers may benefit from this intervention modality. This is a significant finding given the increasing prevalence of technology and societal acceptance and use of the Internet. Healthcare providers can use this evidence to help guide clinical practice to offer beneficial and effective interventions to caregivers.
Although this body of literature is in its early phase of development, the effect sizes for web-based interventions are comparable to those of traditional interventions in this population (Northouse et al., 2010; Sörensen et al., 2002). Northouse et al. (2010) showed that traditional interventions in caregivers of patients with cancer had a significant reduction in caregiver burden (Hedges’ g = 0.22), improvement in the ability to cope (Hedges’ g = 0.47), increase in self-efficacy (Hedges’ g = 0.25), and improvement in aspects of quality of life (Hedges’ g = 0.2 for distress and anxiety and marital-family relationships; Hedges’ g = 0.39 for social functioning). Sörensen et al. (2002) showed that psychoeducation and psychotherapeutic interventions have significant effects on caregiver burden (Hedges’ g = –0.12 and –0.31, respectively) caregiver depression (Hedges’ g = –0.43 and –0.29, respectively), caregiver well-being (Hedges’ g = 0.5 and 0.37, respectively), caregivers’ ability and knowledge (Hedges’ g = 0.53 and 0.42, respectively), and care recipients’ symptoms (Hedges’ g = –0.24 and –0.19, respectively). The review also showed that supportive interventions have a significant positive effect on caregiver burden (Hedges’ g = –0.35) and caregivers’ ability and knowledge to provide appropriate care (Hedges’ g = 0.29). These effect sizes, particularly for reducing caregiver burden and improving caregiver mood, corroborate the results of Chih et al. (2013), Dubenske et al. (2014), and Scott and Beatty (2013). These findings suggest that the interventional modality may not affect the efficacy on caregivers, which supports web-based interventions as an effective alternative to traditional interventions for caregivers.
In terms of translating these findings into practice, the reviewed studies demonstrated that a majority of caregivers were middle-aged female spouses or partners, which is consistent with the existing caregiving literature (Hsu et al., 2014; National Alliance for Caregiving & AARP, 2009; Ugalde, Krishnasamy, & Schofield, 2014). Healthcare providers can use these demographic findings to help identify caregivers who may benefit the most from interventions. This information can encourage caregiver health promotion in the clinical setting.
The potential “dosing” of web-based interventions for caregivers of patients with cancer remains unclear from the reviewed studies. It is difficult to determine the most effective regimen for use of these interventions to reduce the risk of negative sequelae in this population. The included studies differed in protocol timing, with some studies requiring that caregivers use the intervention weekly and others dictating no requirements for login. In addition, only two studies (DuBenske et al., 2014; Zulman et al., 2012) reported on usability outcomes. Because of the lack of homogeneity across studies with regard to the optimal use of web-based interventions, a recommendation for a “dosing regimen” for healthcare providers to offer to caregivers cannot be made.
Limitations
This systematic review was conducted in February 2014 and included articles published before that date. Consequently, web-based interventions for caregivers that were published after February 1, 2014, were not included. Although a rigorous search string was developed, it is possible that not all relevant articles were retrieved. Publication bias may also be a limitation of this study because studies that report significant differences may be more likely to be published than those with negative findings. It was not possible to do a meta-analysis across studies because the measures and outcomes were not homogeneous.
Implications for Practice
Healthcare providers are encouraged to be consumers and implementers of research. However, the rapid proliferation of studies poses a major challenge to staying up to date. This review aggregates the best available evidence regarding use of web-based interventions by caregivers of patients with cancer. Until more definitive, high-quality evidence is generated, the results of this review may guide clinical decision making and provide a source for appropriate resources to mitigate the negative effects of caregiving, ultimately helping to improve caregiver well-being. Although translation into practice is limited because of the paucity of existing literature and because a conclusive benefit of web-based interventions in this population cannot be determined, healthcare providers may consider offering this modality to caregivers to promote health. It cannot be concluded from this limited review that web-based interventions are safe for caregivers, but this modality may offer more benefit than harm to caregivers. Web-based interventions could be offered by providers during routine visits in outpatient clinics, homecare settings, and during hospitalizations.
Despite the potential advantages that web-based interventions may offer, the ability to directly translate these findings to practice is limited because of the lack of evidence currently available in the literature. Many studies describe Internet usage of cancer caregivers (James et al., 2007; Kinnane & Milne, 2010), caregiver information and emotional needs concerning a web-based intervention (Arber et al., 2010; Cho et al., 2011; Dolce, 2011; Linssen et al., 2007), and caregiver perceptions of web-based interventions (Chung & Kim, 2007), but few have actually implemented web-based interventions in this population. More studies should be conducted that examine the impact of web-based interventions on caregiver physical, social, and psychological outcomes.
Of the six studies identified in this review, none reported findings about financial outcomes, such as missed work time, loss of benefits and wages, and social security. Because healthcare policy is changing, studies could focus on this gap in the literature. To further examine the outcomes of web-based interventions and to better serve caregivers, future studies should target various caregiving populations, such as caregivers coping with a loved one’s metastatic disease or caregivers of patients with highly complex care needs (e.g., those undergoing bone marrow transplantation). Studies could also explore how cultural differences and caregiver diversity (e.g., adult children caring for parents versus spouse caring for spouse) may affect web-based intervention usage and outcomes.
Although statistically significant findings regarding web-based interventions for caregivers may help to guide a change in practice, researchers should recognize that the publishing of negative findings, or findings that are not statistically significant, are equally valuable as the knowledge base is built in this area.
[[{"type":"media","view_mode":"media_original","fid":"19551","attributes":{"alt":"","class":"media-image","height":"202","typeof":"foaf:Image","width":"365"}}]]
Conclusions
This systematic review of the published literature for web-based interventions of caregivers offers evidence that these interventions may positively influence the social and psychological outcomes in this population. Caregiver interventions can be beneficial in offering information and support, and the limited existing literature supports the adaptation of caregiver interventions to a web-based format.
Caregivers of patients with cancer face many challenges. Supporting these caregivers is important to help ensure that they have the needed tools and resources to provide the best possible care to their loved ones.
References
American Cancer Society. (2015). Cancer facts and figures, 2015. Atlanta, GA: Author.
Applebaum, A.J., & Breitbart, W. (2013). Care for the cancer caregiver: A systematic review. Palliative and Supportive Care, 11, 231–252. doi:10.1017/S1478951512000594
Arber, A., Hutson, N., Guerrero, D., Wilson, S., Lucas, C., & Faithfull, S. (2010). Carers of patients with a primary malignant brain tumour: Are their information needs being met? British Journal of Neuroscience Nursing, 6, 329–334. doi:10.12968/bjnn.2010.6.7.79227
Chih, M.Y., DuBenske, L.L., Hawkins, R.P., Brown, R.L., Dinauer, S.K., Cleary, J.F., & Gustafson, D.H. (2013). Communicating advanced cancer patients’ symptoms via the Internet: A pooled analysis of two randomized trials examining caregiver preparedness, physical burden, and negative mood. Palliative Medicine, 27, 533–543. doi:10.1177/0269216312457213
Cho, J., Noh, H.I., Ha, M.H., Kang, S.N., Choi, J.Y., & Chang, Y.J. (2011). What kind of cancer information do Internet users need? Supportive Care in Cancer, 19, 1465–1469. doi:10.1007/s00520-010-1057-9
Chung, D.S., & Kim, S. (2007). Blogging activity among cancer patients and their companions: Uses, gratifications, and predictors of outcomes. Journal of the American Society for Information Science and Technology, 59, 297–306. doi:10.1002/asi.20751
Collins, L.G., & Swartz, K. (2011). Caregiver care. American Family Physician, 83, 1309–1317.
Dolce, M.C. (2011). The Internet as a source of health information: Experiences of cancer survivors and caregivers with healthcare providers. Oncology Nursing Forum, 38, 353–359. doi:10.1188/11.ONF.353-359
DuBenske, L.L., Gustafson, D.H., Namkoong, K., Hawkins, R.P., Atwood, A.K., Brown, R.L., . . . Cleary, J.F. (2014). CHESS improves cancer caregivers’ burden and mood: Results of an eHealth RCT. Health Psychology, 33, 1261–1272.
DuBenske, L.L., Gustafson, D.H., Shaw, B.R., & Cleary, J.F. (2010). Web-based cancer communication and decision making systems: Connecting patients, caregivers, and clinicians for improved health outcomes. Medical Decision Making, 30, 732–744. doi:10.1177/0272989X10386382
Effective Public Health Practice Project. (2009). Quality assessment tool for quantitative studies dictionary. Retrieved from http://www.ephpp.ca/PDF/QADictionary_dec2009.pdf
Effective Public Health Practice Project. (2010). Quality assessment tool for quantitative studies. Retrieved from http://www.ephpp.ca/PDF/Quality%20Assessment%20Tool_2010_2.pdf
Evercare & National Alliance for Caregiving. (2006). Study of caregivers in decline: A close-up look at the health risks of caring for a loved one. Retrieved from http://www.caregiving.org/data/Caregivers%20in%20Decline%20Study-FINAL-…
Family Caregiver Alliance. (2012). Selected caregiver statistics. Retrieved from http://www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=439
Farnham, S., Cheng, L., Stone, L., Zaner-Godsey, M., Hibbeln, C., Syrjala, K., . . . Abrams, J. (2002, April). HutchWorld: Clinical study of computer-mediated social support for cancer patients and their caregivers. Paper presented at Proceedings of the SIGCHI Conference on Human Factors in Computing Systems: Changing Our World, Changing Ourselves, Minneapolis, MN. doi:10.1145/503376.503444
Gaugler, J.E., Linder, J., Given, C.W., Kataria, R., Tucker, G., & Regine, W.F. (2009). Family cancer caregiving and negative outcomes: The direct and mediational effects of psychosocial resources. Journal of Family Nursing, 15, 417–444. doi:10.1177/1074840709347111
Gustafson, D.H., Hawkins, R.P., Boberg, E.W., McTavish, F., Owens, B., Wise, M., . . . Pingree, S. (2002). CHESS: 10 years of research and development in consumer health informatics for broad populations, including the underserved. International Journal of Medical Informatics, 65, 169–177. doi:10.1016/S1386-5056(02)00048-5
Hsu, T., Loscalzo, M., Ramani, R., Forman, S., Popplewell, L., Clark, K., . . . Hurria, A. (2014). Factors associated with high burden in caregivers of older adults with cancer. Cancer, 120, 2927–2935. doi:10.1002/cncr.28765
James, N., Daniels, H., Rahman, R., McConkey, C., Derry, J., & Young, A. (2007). A study of information seeking by cancer patients and their carers. Clinical Oncology, 19, 356–362. doi:10.1016/j.clon.2007.02.005
Kinnane, N.A., & Milne, D.J. (2010). The role of the Internet in supporting and informing carers of people with cancer: A literature review. Supportive Care in Cancer, 18, 1123–1136. doi:10.1007/s00520-010-0863-4
Linssen, C., Schook, R.M., The, A.M., Lammers, E., Festen, J., & Postmus, P.E. (2007). A web site on lung cancer: Who are the users and what are they looking for? Journal of Thoracic Oncology, 2, 813–818. doi:10.1097/JTO.0b013e31811f472a
McTavish, F.M., Chih, M.Y., Shah, D., & Gustafson, D.H. (2012). How patients recovering from alcoholism use a smartphone intervention. Journal of Dual Diagnosis, 8, 294–304. doi:10.1080/15504263.2012.723312
Namkoong, K., DuBenske, L.L., Shaw, B.R., Gustafson, D.H., Hawkins, R.P., Shah, D.V., . . . Cleary, J.F. (2012). Creating a bond between caregivers online: Effect on caregivers’ coping strategies. Journal of Health Communication, 17, 125–140. doi:10.1080/10810730.2011.585687
National Alliance for Caregiving & AARP. (2009). Caregiving in the U.S. 2009. Retrieved from http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf
Northouse, L.L., Katapodi, M.C., Song, L., Zhang, L., & Mood, D.W. (2010). Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA: A Cancer Journal for Clinicians, 60, 317–339.
Owens, B.H., & Robbins, K.C. (1996). CHESS: Comprehensive Health Enhancement Support System for women with breast cancer. Plastic Surgical Nursing, 16(3), 172–175. doi:10.1097/00006527-199623000-00009
Pinquart, M., & Sörenson, S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 18, 250–267. doi:10.1037/0882-7974.18.2.250
Polit, D.F., & Beck, C.T. (2008). Using inferential statistics to test hypotheses. In D.F. Polit & C.T. Beck (Eds.), Nursing research: Generating and assessing evidence for nursing practice (pp. 583–613). Philadelphia, PA: Lippincott Williams and Wilkins.
Rains, S., & Young, V. (2009). A meta-analysis of research on formal computer-mediated support groups: Examining group characteristics and health outcomes. Human Communication Research, 35, 309–336. doi:10.1111/j.1468-2958.2009.01353.x
Robbins, K.C. (1999). CHESS: The Comprehensive Health Enhancement Support System. A computer based program for patients and families. Connecticut Nursing News, 72(1), 14.
Schulz, R., & Beach, S.R. (1999). Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA, 282, 2215–2219. doi:10.1001/jama.282.23.2215
Scott, K., & Beatty, L. (2013). Feasibility study of a self-guided cognitive behaviour therapy Internet intervention for cancer carers. Australian Journal of Primary Health, 19, 270–274. doi:10.1071/PY13025
Sörensen, S., Pinquart, M., & Duberstein, P. (2002). How effective are interventions with caregivers? An updated meta-analysis. Gerontologist, 42, 356–372. doi:10.1093/geront/42.3.356
Stenberg, U., Ruland, C., & Miaskowski, C. (2010). Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology, 19, 1013–1025. doi:10.1002/pon.1670
Temesgen, Z., Knappe-Langworthy, J.E., St. Marie, M.M., Smith, B.A., & Dierkhising, R.A. (2006). Comprehensive Health Enhancement Support System (CHESS) for people with HIV infection. AIDS and Behavior, 10, 35–40. doi:10.1007/s10461-005-9026-x
Thomas, B.H., Ciliska, D., Dobbins, M., & Micucci, S. (2004). A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews on Evidence-Based Nursing, 1, 176–184. doi:10.1111/j.1524-475X.2004.04006.x
Ugalde, A., Krishnasamy, M., & Schofield, P. (2014). The relationship between self-efficacy and anxiety and general distress in caregivers of people with advanced cancer. Journal of Palliative Medicine, 17, 939–941. doi:10.1089/jpm.2013.0338
Zulman, D.M., Schafenacker, A., Barr, K.L., Moore, I.T., Fisher, J., McCurdy, K., . . . Northouse, L. (2012). Adapting an in-person patient-caregiver communication intervention to a tailored web-based format. Psycho-Oncology, 21, 336–341. doi:10.1002/pon.1900
About the Author(s)
Donna J. Kaltenbaugh, DNP, CRNP, FNP-BC, is a recent graduate from the Department of Health Promotion and Development; Mary Lou Klem, PhD, MLIS, is a faculty librarian in the Health Sciences Library System; Lu Hu, MSN, is a graduate student in the Department of Health and Community Systems; Eleanor Turi is an undergraduate research assistant in the School of Nursing; Alice J. Haines, DNP, RN, CMSRN, is an assistant professor in the Department of Acute/Tertiary Care; and Jennifer Hagerty Lingler, PhD, CRNP, is an assistant professor in the Department of Health and Community Systems, all at the University of Pittsburgh in Pennsylvania. This study was supported, in part, by a grant from the Greater Pittsburgh Nursing Research Conference. Lingler can be reached at linglerj@pitt.edu, with copy to editor at ONFEditor@ons.org. (Submitted August 2014. Accepted for publication October 6, 2014.)

