Risk Factors Associated With Unplanned Hospital Readmissions in Adults With Cancer
Purpose/Objectives: To identify risk factors associated with 30-day unplanned hospital readmissions in adults with cancer.
Design: Case-control study.
Setting: A teaching hospital in an urban center in the Mid-Atlantic region of the United States.
Sample: 302 adults with solid tumors: 87 readmitted within 30 days (cases) and 215 not readmitted (controls).
Methods: The Conceptual Model of Re-Hospitalization was used as a theoretic framework. Univariate logistic regression and multivariate logistic regression were conducted to identify risk factors for hospital readmission.
Main Research Variables: Risk factors included patient, clinical, hospitalization, and discharge-planning characteristics.
Findings: From November 2011 to November 2012, 29% of patients were readmitted within 30 days after discharge, and a higher percentage of those readmissions occurred within the first week of discharge. Several predictors for hospital readmission were identified in the univariate logistic analysis, but the most relevant in the final multivariate logistic model were moderate to high risk for falls and advanced stage disease (metastatic).
Conclusions: Hospital readmission is an indicator of quality care. Learning about risk factors allows opportunities to prevent hospital readmission by identifying those at high risk and implementing optimal discharge-planning systems and early referrals to palliative care.
Implications for Nursing: Oncology nurses are best positioned to develop strategic plans aimed at improving discharge planning and transitions of care that will decrease unplanned hospital readmissions.
Jump to a section
Hospital readmission is a major issue in the U.S. healthcare system because of an association with inadequate quality care, patient safety, and increased costs (MedPAC, 2007). In the United States, from 2007–2011, the 30-day, all-cause hospital readmission rate among Medicare beneficiaries remained stable at 19%, with a downward trend noted in 2012 (Gerhardt et al., 2013). The costs of 30-day hospital readmissions were estimated to be $17.4 billion (Jencks, Williams, & Coleman, 2009). Although not all hospital readmissions are unplanned, many result from a fragmented health delivery system in which patients receive care by multiple providers in a variety of healthcare settings, which can lead to low-quality care (Pham, Schrag, O’Malley, Wu, & Bach, 2007). Numerous reports have reviewed factors associated with unplanned hospital readmissions in the general population and in patients with cardiovascular disease (Amarasingham et al., 2010; Desai, Stauffer, Feringa, & Schreiner, 2009; Jencks et al., 2009; Kansagara et al., 2011; Kind, Smith, Frytak, & Finch, 2007; Lichtman et al., 2010; Ross et al., 2008), but little research has focused on this issue with patients with cancer.
Patients with cancer experience a variety of medical, psychosocial, and comorbid conditions that may require hospitalization. The Healthcare Cost and Utilization Project (HCUP) reported 4.7 million hospitalizations related to adult cancers in the United States in 2009; of these, 1.2 million identified cancer as the main diagnosis (Price, Stranges, & Elixhauser, 2012). The total cost associated with hospitalizations among adults in 2009 was $20.1 billion, accounting for 6% of hospital costs in adults (Price et al., 2012). Studies of hospital readmission for patients with cancer have focused mostly on patients who have had surgery, particularly for colon, thyroid, and gynecologic cancers (Greenblatt et al., 2010; Henretta, Scalici, Engelhard, & Duska, 2011; Tuggle, Park, Roman, Udelsman, & Sosa, 2010); and not much on patients admitted to medical oncology units (Weaver et al., 2006). Those studies reported mostly on clinical and sociodemographic factors but did not include other items associated with hospital readmissions, such as hospital factors and discharge processes. To fill this gap, the current study identified risk factors associated with 30-day unplanned hospital readmissions in patients with an emphasis on characteristics of the hospitalization and discharge process.
Theoretical Framework
The current study used the Conceptual Model of Re-Hospitalization (Anthony et al., 2005) (see Figure 1). This conceptual model, based on the quality framework proposed by Donabedian (1988), encompasses various components related to high rates of rehospitalization: patient characteristics, including fixed factors (e.g., age, gender) and modifiable factors (e.g., drug or alcohol use, medication adherence); hospital characteristics (e.g., services, clinicians); severity of illness; clinical deterioration; hospitalization (e.g., length of stay, palliative care consultation); discharge process; outpatient care; and characteristics of the primary care provider (PCP) and consultant (e.g., physician specialist). This model attempts to understand the factors associated with rehospitalizations; in particular, it aims to understand those factors related to the hospitalization and the discharge process. For the purpose of the current study, patient characteristics, clinical characteristics, hospitalization, and discharge planning were used (see Figure 2).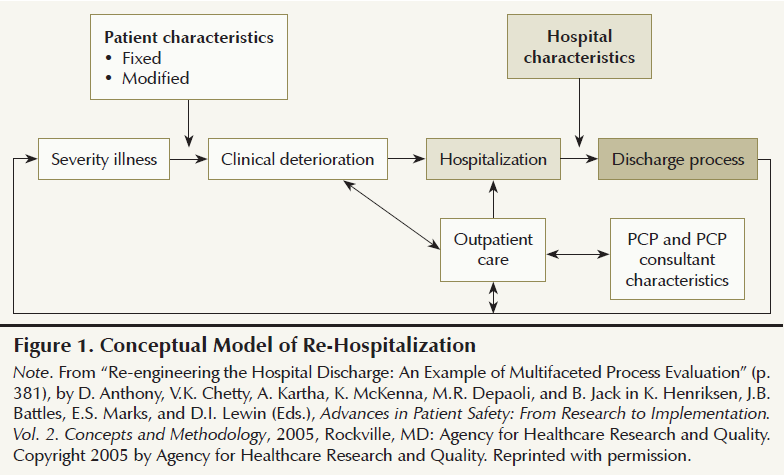
Methods
This hospital-based, case-control study was conducted at Pennsylvania Hospital, a 520-bed acute care teaching hospital in Philadelphia. After institutional review board approval from the University of Pennsylvania was granted, data were obtained from the administrative databases and the electronic medical record.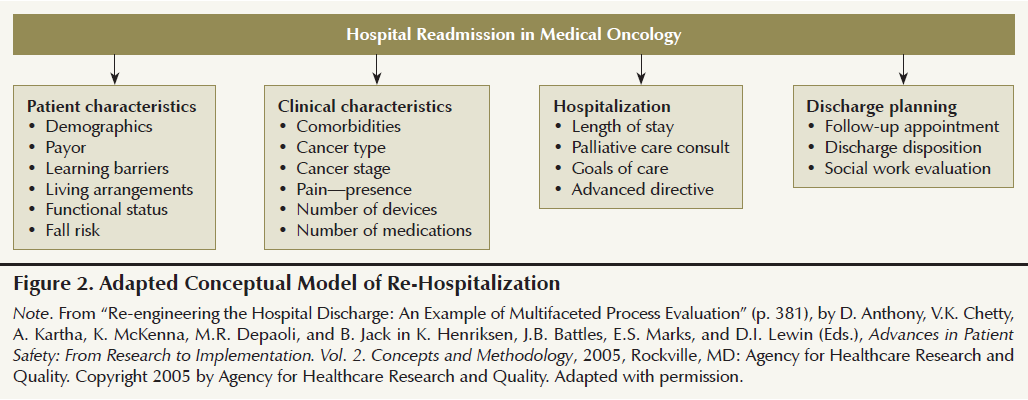
The study used a convenience, nonprobability sample of adult patients with solid tumors who were aged 18 years or older and discharged from the medical oncology unit from November 1, 2011, through November 30, 2012 (see Figure 3). Excluded were individuals with liquid tumors (leukemia, lymphoma, and multiple myeloma) and those with a discharge status of deceased or who had left against medical advice. Cases included adults with solid tumors who were readmitted within 30 days of discharge. Controls included those adults who were not readmitted within 30 days and survived 60 days after discharge.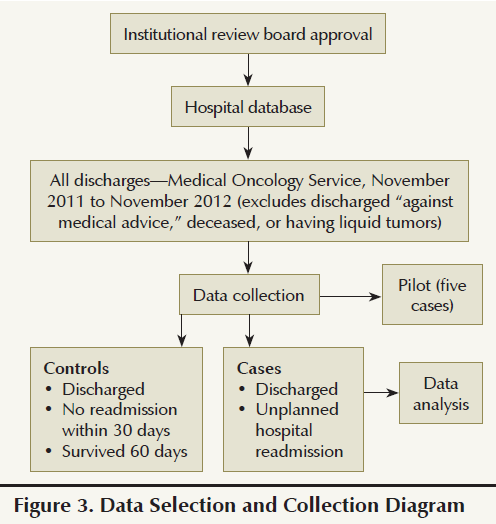
Data were collected electronically and manually in a web-based data collection tool. This tool was developed by the authors to ensure consistency in the data collection process. Reliability and validity tests were not considered necessary because the number of people conducting the data collection was limited to only two trained researchers. Instead, the tool was piloted with five medical records to determine the efficiency of the instrument and verify accessibility to the data. The tool included a total of 24 predictors grouped into four categories: patient characteristics, clinical characteristics, hospitalization, and the discharge process. Patient characteristics comprised demographics (i.e., age, gender, race, marital status, language, and education level), payer, learning barriers (e.g., cognitive limitations, communication limitations, comprehension, hearing problems, language, learning disability, literacy, physical limitations, touch or tactile deficit, visual problems), living arrangements, fall risk, and functional status. Clinical characteristics included cancer type, cancer stage, presence of pain, number of devices (total at the time of discharge), number of medications, and comorbidities. The comorbidities were measured using the Charlson Comorbidity Index (Charlson, Pompei, Ales, & MacKenzie, 1987) with scores of 0 (no comorbidities), 1 (one to two comorbidities), or 2 (three and more comorbidities). Hospitalization characteristics included length of stay (LOS), palliative care consultation during index admission and readmission, goals-of-care discussion during index admission and readmission, and documented advance directives during index admission and readmission. Discharge planning referred to the discharge process, including social work assessment at index admission, scheduled follow-up appointment with medical provider, and discharge disposition to homecare services or other post-acute care facilities. Data from the electronic medical records were coded and entered into a single database.
Data analyses included descriptive statistics, univariate and multivariate logistic regression, and some secondary additional specific cross-tabulations and analyses. Statistic significance was defined as p ≤ 0.05. All statistical analyses were conducted using SAS®, version 9.3.
The analysis followed the pattern for a typical epidemiologic case-control study. The controls were not specifically matched to specific cases on background factors. Instead, all of the available controls were used. First, the cases and controls were profiled on the predictor variables, such as demographics and risk factors. Chi-square and t tests, unadjusted for multiple testing, were used to test for significant differences. Second, univariate regression was conducted with a comparison of the two groups, cases (readmitted) and controls (not readmitted), on the 24 potential predictors. Third, a multivariate model was created using the univariate results for guidance. The initial model used all predictors with an univariate significance of 0.1 or lower. Once the preliminary model was run, it was inspected for the presence of highly correlated (co-linear) variables and nonsignificant predictors. A number of alternative models were then chosen to find a model containing the predictors with the highest odds ratios.
Results
From November 2011 to November 2012, a total of 1,316 patients discharged from the medical oncology service at the teaching hospital occurred. Of those, 394 unique patients with a total of 760 discharges had a coded principal or secondary diagnosis of malignant solid tumor. A complete review of the 394 patients was performed, and 14 were removed from the sample for being unavailable or not having a solid tumor diagnosis. Of the remaining 380 patients, 87 were readmitted within 30 days (cases group). Of the 293 patients who were not readmitted, 78 were excluded because they died within 60 days after discharge, resulting in a total of 215 patients in the controls group (see Figure 4).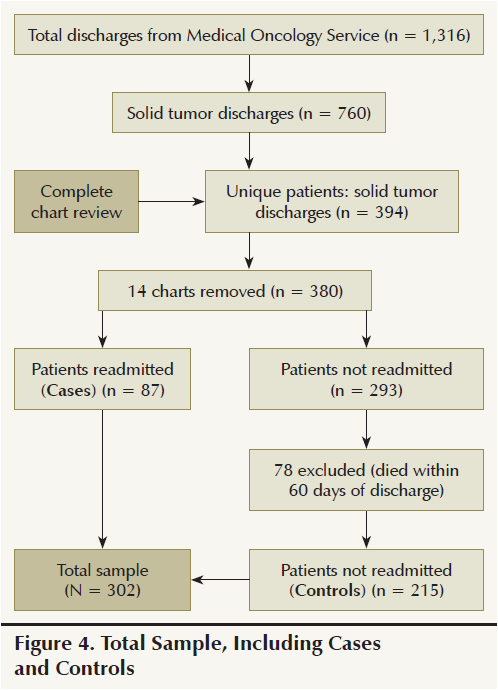
Analysis of Readmissions
Descriptive analysis: Of the 87 patients who experienced hospital readmission within 30 days after discharge, the mean time to readmission was 13.9 days (SD = 8.78). Most readmissions occurred during the first week of discharge (n = 26). Among those readmitted, the most common reasons for readmission were gastrointestinal symptoms (n = 21), pulmonary symptoms (n = 16), and fever or pancytopenia (n = 13); the most common cancer diagnosis was sarcoma (n = 25), followed by gastrointestinal (n = 17) and lung (n = 16). Most patients readmitted had metastatic disease (n = 54).
Profile cases and controls: The characteristics of patients in the cases and controls groups is outlined in Tables 1 and 2. No significant differences were noted in gender, race, marital status, level of education, living arrangements, and learning barriers. The cases group was older (X = 62.6 years) than the controls group (X = 58.6 years) (p = 0.03). A higher percentage of patients in the cases group needed assistance with walking (ambulatory function), moving from one place to another (transfer function), and feeding self (eating function) than those in the controls group, particularly with eating function (cases, 15%; controls, 6%; p < 0.01). Likewise, patients in the cases group were more likely to have a moderate to high risk for falling (55%) than the controls group (38%) (p = 0.007).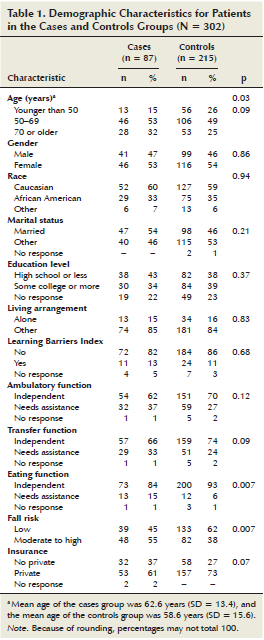
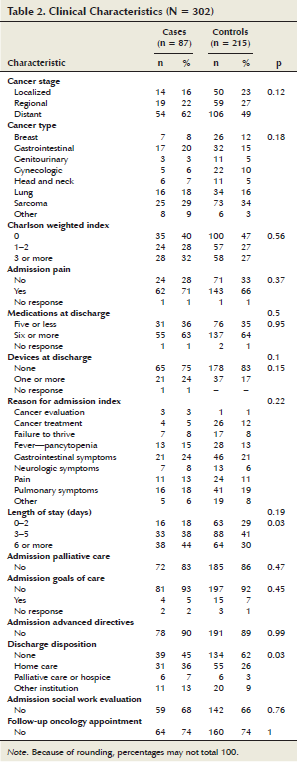
Clinical characteristics for cases and controls differed in that cases were more likely to have metastatic cancer (62%), a higher Charlson weighted index score (32%), and a higher documented pain (72%) during the index admission than controls. The number of devices (e.g., tracheostomy, colostomy, feeding tube, peripherally inserted central catheter) at the time of discharge was higher in the cases (24%) than the controls (17%). No significant differences were noted between the two groups in regard to number of medications at the time of discharge (X = 7.96 medications for cases; X = 7.6 medications for controls) or reasons for admission at the index admission (gastrointestinal and pulmonary symptoms).
Hospitalization characteristics for cases and controls reported that the mean LOS for cases and controls was similar (6.34 days and 5.4 days, respectively). However, the percentage of patients with LOS of six days or more was higher in the cases (44%) than in the controls (30%) (p = 0.03). The majority of patients in both groups did not have palliative care consultation and goals-of-care discussions at the index admission; however, the cases had a slightly higher percentage of palliative care consultations (17%) than the controls (14%) but a lower percentage of goals-of-care discussions (5%) than the controls (7%).
Discharge-planning characteristics for cases and controls reported that patients in the cases group were more likely than the controls group to be discharged with either basic home care (36% versus 26%), palliative care or hospice (7% versus 3%), or to other institutions (13% versus 9%) (p = 0.03). No significant difference was noted between the cases and controls group in regard to social work evaluation and follow-up appointment with an oncologist or other physician at the time of discharge.
Univariate and multivariate logistic regression: The univariate analysis revealed that patients were more likely to be readmitted if the patient was aged 70 years or older (odds ratio [OR] = 2.28, 95% confidence interval [CI] [1.07, 4.85]), needed assistance with eating function (OR = 2.97, 95% CI [1.29, 6.8]), had a moderate to high risk for falls (OR = 1.99, 95% CI [1.2, 3.3]), and had advanced disease (OR = 1.81, 95% CI [0.92, 3.58]). In addition, if LOS during index admission was six days or more (OR = 2.33, 95% CI [1.18, 4.61]), or the patient had been discharged to home care (OR = 1.93, 95% CI [1.09, 3.41]), palliative care, or hospice (OR = 3.43, 95% CI [1.04, 11.24]), risk of readmission was higher (see Table 3).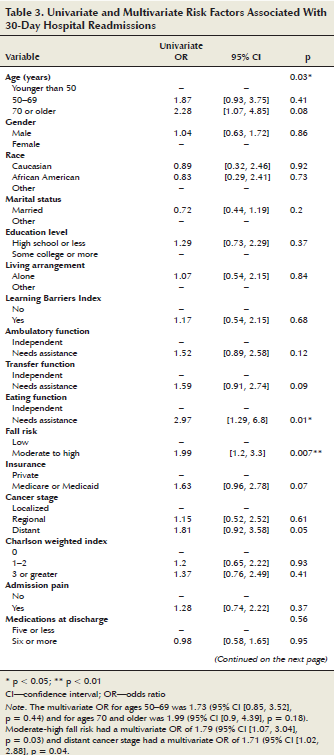
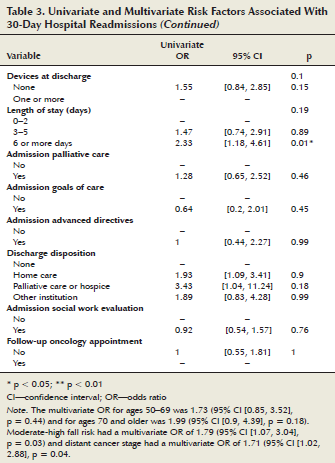
The final multivariate logistic model indicated that fall risk (OR = 1.79, 95% CI [1.07, 3.04], p = 0.03) and advanced cancer stage (OR =1.71, 95% CI [1.02, 2.88], p = 0.04) predicted hospital readmissions. The odds of readmission for patients older than age 70 were nearly twice as high as patients younger than age 50 (OR = 1.99, 95% CI [0.85, 3.5]), but the difference was not statistically significant.
Analysis of Readmissions by Week
A higher percentage of 30-day readmissions occurred within the first week; therefore, an additional descriptive analysis of the predictors was conducted comparing the first week against the other weeks (weeks 2–4) (see Table 4). The day of readmission postdischarge ranged from 0–7 days, with a mean of 3.23 days (SD = 2.25) for patients readmitted in the first week; whereas, for patients readmitted in the other weeks, the mean day of readmission postdischarge was 18.44 days (SD = 6.17).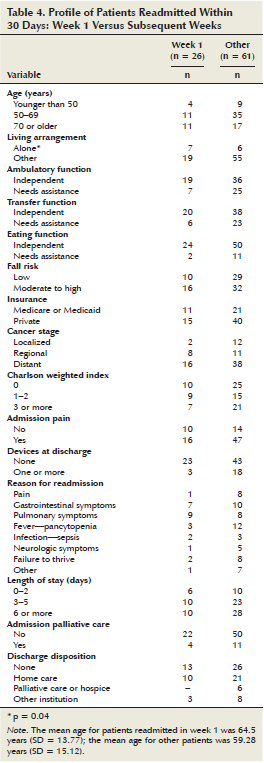
Patients readmitted in the first week were more likely to be aged 70 years or older (42%) than patients readmitted in the other weeks (28%), to live alone (27%) compared to patients readmitted in the other weeks (10%) (p = 0.04), and to be independent in ambulatory function (73%) and transfer function (77%) than patients readmitted in other weeks (58% and 62%, respectively). However, patients readmitted in the first week had a greater moderate to high fall risk (62%) than their counterparts readmitted in the other weeks (52%).
Regarding clinical characteristics, patients readmitted in the first week after discharge were more likely to have a regional cancer stage (e.g., invasion to lymph nodes) (31%), a Charlson Comorbidity Index score of 1–2 (35%), and fewer devices at discharge (12%) than patients readmitted in other weeks (18%, 25%, and 30%, respectively). Patients readmitted in the first week were more likely to have less pain during index admission (38%) than patients admitted in other weeks (23%).
Regarding hospital characteristics, patients readmitted in the first week after discharge were more likely to have a length of stay of 0–2 days (23%) than patient readmitted in other weeks (16%) and less palliative care consultations during index admission (15%) than patients readmitted in other weeks (18%). Regarding discharge-planning characteristics, patients readmitted in the first week after discharge were slightly more likely to be discharged with no homecare arrangements (50%) or with basic home care (38%) than patients readmitted in other weeks (43% and 34%, respectively).
Discussion
Overview of Study
The current study found a 30-day hospital readmission rate of 29% in patients with solid tumors discharged from the medical oncology service in a one-year period. That readmission rate is higher than the national rate for Medicare patients (20%) (Jencks et al., 2009) and higher than readmission rates reported in studies conducted in patients with cancer undergoing surgery (Henretta et al., 2011; Reddy et al., 2009; Rochefort & Tomlinson, 2012). The higher percentage of readmissions occurred within the first week after discharge.
The patients in the cases group (readmitted) were overall in worse health than those in the controls group (nonreadmitted). Patients in the cases group were older; needed more assistance with ambulation, transfers, and eating (p < 0.01); had significant moderate to high risk for falls (p = 0.007); and were more likely to have gastrointestinal cancer, an advanced cancer, a higher Charlson Comorbidity Index score, more complaints of pain at index admission, and more devices at the time of discharge. Patients in the cases group were more likely to have a prolonged LOS (six or more days) and to be discharged with homecare services or palliative or hospice care.
Predictors of Readmission
Multiple regression analysis identified two predictors for unplanned hospital readmission: advanced cancer and moderate to high risk for falls. Regarding advanced cancer, similar findings were reported in studies with patients with cancer undergoing surgery; specifically, patients with thyroid cancer after thyroidectomy and patients with pancreatic cancer after pancreatico-duodenectomy were more likely to be readmitted if they had advanced disease (Tuggle et al., 2010; Yermilov et al., 2009).
No additional studies that included fall risk as a predictor for hospital readmissions were found. However, this factor is extremely important considering its role in patient safety in the older adult population. The 2006 Behavioral Risk Factor Surveillance System (BRFSS) survey conducted by the Centers for Disease Control and Prevention reported that 5.8 million people aged 65 years or older had fallen one or more times in the previous three months (Stevens, Mack, Paulozzi, & Ballesteros, 2008). Another survey of Medicare beneficiaries indicated that seven million fell the year before, and among those who fell, many of them did not report it to their healthcare providers (Stevens et al., 2012). In addition, older adults with cancer are more likely to fall than those without cancer (Spoelstra et al., 2013; Stone, Lawlor, Savva, Bennett, & Kenny, 2012). Falls in patients with cancer have been associated with motor neuropathy induced by chemotherapy (Gewandter et al., 2013), primary brain tumor or brain metastasis, number of falls in the preceding three months, severity of depression, benzodiazepine dose, and cancer-related pain (Stone et al., 2012).
Fall risk may not have been included in other hospital readmission studies because of its similarity to function with activities of daily living (ADLs); however, those two predictors are different. Function is just one of the various factors that may impact fall risk. Fall risk is not only associated with a patient’s functional limitations, but also with a wide range of factors, including poor health, difficulty hearing, poor vision, and depression (Stevens et al., 2012). In this study, analysis of readmissions in week 1 versus other indicated that patients who were readmitted in the first week after discharge were mostly independent in their ability to function with ambulation, transfers, and eating; however, they had a moderate to high risk for falls. This finding suggests that fall risk may be manifested in a more subtle manner than function deficits; therefore, it can be overlooked by healthcare providers.
High-Risk Readmission Profile
The current study identified two high-risk patient profiles for hospital readmission (see Table 5). The 30-day readmission patient profile describes a patient who is frail, older, has metastatic cancer, has multiple comorbidities, needs assistance with ADLs, has a moderate to high risk for falls, experiences more pain during index admission, has more devices at the time of discharge, has a prolonged LOS (six or more days), and has been discharged to either home with homecare services or another institution (hospice or skilled nursing facility). Conversely, the seven-day readmission patient profile describes a patient that, although older, has an overall better performance status, has a regional cancer, has less comorbidities, and does not need assistance with ADLs; however, this patient has a moderate to high risk for falls, lives alone, has a short LOS (0–2 days), and has been discharged home with either no homecare services or basic homecare services.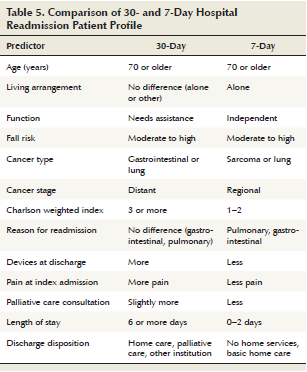
Some studies have failed to report a strong relationship between deficient inpatient care during initial admission and early readmission (Ashton & Wray, 1996), but readmission occurring within the first seven days after discharge is thought to be related to gaps in care during hospitalization, coordination of care, and lack of recognition of patient’s needs postdischarge. Later readmissions are more likely to be related to severity of disease (Joynt & Jha, 2013). In the current study, the fact that patients readmitted during the first week after discharge had a short LOS of two days or less suggests that, more likely, they were discharged prematurely. A study on early discharges after colectomy for cancer reported that very early discharges (LOS of four days or less) significantly increased hospital readmissions (Hendren, Morris, Zhang, & Dimick, 2011). Although early discharges are encouraged, they must be considered with caution, particularly in patients who have a high-risk readmission profile. Findings in the current study suggest that those readmitted within the first week were probably more physically debilitated than they appeared; they had a moderate to high risk for falls despite being independent in their ADLs. Therefore, a more in-depth needs assessment would have been warranted to anticipate the patient’s needs after discharge. Similarly, other studies have reported that older adult patients were discharged home without homecare services despite having high-priority needs, and that discharge disposition referrals varied among healthcare providers depending on the needs-assessment process and the level of expertise of the person conducting the needs assessment (Bowles et al., 2008; Bowles, Foust, & Naylor, 2003; Bowles, Naylor, & Foust, 2002).
Findings from the current study suggests a two-step process to improve identification of patients at high risk for readmission and optimize their discharge planning. The first step is the use of predictors for high-risk readmission assessment which, for the seven-day readmission patient profile, are moderate to high fall risk, being aged 70 years or older, and living alone. The second step is to conduct a comprehensive needs assessment for patients flagged as high risk. Those patients should be reassessed closely during hospitalization to ensure that they are fully ready before their discharge.
Findings from the current study also suggest that palliative care teams be consulted when patients with advanced cancer are admitted to the hospital, particularly those patients who are at high risk for readmission. Inpatient palliative care consultations were found not only to reduce hospital readmissions in general medical patients (Nelson, Chand, Oloimooja, & Rembert, 2011), but also to facilitate transitions of care by improving the discharge process and ensuring appropriate postdischarge follow-up services (Brody, Ciemins, Newman, & Harrington, 2010). The Institute of Medicine (2013) issued a report on high-quality cancer care in which it recommended providing palliative care to patients with advanced cancer that should include goals-of-care conversations, psychosocial support, and opportune referrals to hospice care.
Limitations
This study had limitations intrinsic to any administrative database. Some of the readmissions may not have been captured because some cases may have been admitted to hospitals outside this database. This study used a small sample in a single institution, so findings cannot be generalized to other populations.
Implications for Nursing Practice
This study has significant implications to oncology nursing practice, particularly for nurse clinicians, nurse executives, and nurse scientists. Nurse clinicians are at the forefront of patient care and, as such, they are involved in the discharge planning of patients with cancer. Oncology nurses may use the results of this study to identify patients at high risk for readmission and target nursing interventions and strict discharge planning to this patient cohort. Advanced practice nurses are in a unique position to use evidence-based practice to incorporate models of care that improve transition of care and patient outcomes (Naylor, Aiken, Kurtzman, Olds, & Hirschman, 2011). Nurse executives working at high-level nurse leadership positions evaluate the connections between the new healthcare legislation, the institution’s goals and resources, and clinical outcomes (Glasgow & Zoucha, 2011). By learning about the risk factors associated with 30-day readmission in patients with cancer, nurse executives may use this information as a starting point of a more comprehensive discharge-planning assessment and as part of a strategic plan to address the system failures identified during the hospitalization and the discharge process. The role of the nurse executive as an active participant in various aspects of healthcare reform is described by the American Organization of Nurse Executives (2010).
Nurse researchers are best positioned to identify research questions relevant to clinical practice (Glasgow & Zoucha, 2011). Findings from this study, with regard to risk factors associated with 30-day readmission in patients with cancer, may be used by nurse researchers as basic knowledge to further develop other studies looking at models to reduce hospital readmissions in this patient population. The research nurse’s role and the impact on nursing practice is well supported by the Institute of Medicine (2011), as shown by its recommendation to “expand opportunities for nurses to lead and manage collaborative efforts with physicians and other members of the health care team to conduct research and to redesign and improve practice environments and health systems” (p. 2).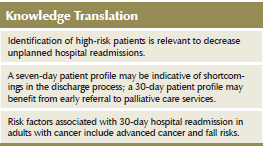
Implications for Future Research
The current study allowed for a thorough chart review and exploration of new factors related to readmissions, which are not usually explored in large-population studies; however, results are only relevant to the one institution. Therefore, additional research on hospital readmissions in larger populations of patients with cancer is needed. Research can be facilitated if a well-structured set of predictors for readmission data collection is built into the institution’s database for large-scale analysis. Additional studies should investigate the impact of new strategies implemented by hospitals to reduce hospital readmissions, particularly the impact of palliative care services on 30-day hospital readmissions.
Finally, quality improvement projects at the institution level are necessary. These projects should develop strategies to (a) identify patients at high risk for readmission using the high-risk readmission profile suggested in the current study, (b) improve the discharge-planning process by innovating current ways of communication among members of the oncology team, and (c) improve coordination of care by creating a transition model that involves collaboration between the inpatient and outpatient oncology teams.
Conclusions
Overall, this study contributed to a better understanding of the multifactorial process of hospital readmissions in patients admitted to medical oncology units (see Figure 5). Two main predictors for hospital readmission were identified: moderate to high risk for falls and advanced cancer stage (metastatic). The higher percentage of 30-day hospital readmissions occurred within the first week of discharge. This analysis revealed two high-risk readmission patient profiles: a seven-day readmission profile and 30-day readmission profile. The seven-day patient profile may be indicative of shortcomings in the discharge process. Early referral of patients with advanced cancer to palliative care teams during hospitalization may improve discharge planning and transitions of care between healthcare settings.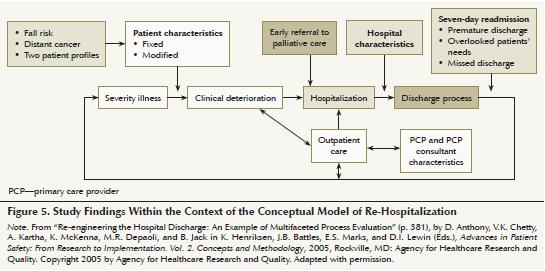
References
Amarasingham, R., Moore, B.J., Tabak, Y.P., Drazner, M.H., Clark, C.A., Zhang, S., . . . Halm, E.A. (2010). An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Medical Care, 48, 981–988. doi:10.1097/MLR.0b013e3181ef60d9
American Organization of Nurse Executives. (2010). AONE guiding principles for future care delivery. Retrieved from www.aone.org/resources/PDFs/AONE_GP_Future_Patient_Care_Delivery_2010.p…
Anthony, D., Chetty, V.K., Kartha, A., McKenna, K., Depaoli, M.R., & Jack, B. (2005). Re-engineering the hospital discharge: An example of a multifaceted process evaluation. In K. Henriksen, J.B. Battles, E.S. Marks, and D.I. Lewin (Eds.), Advances in patient safety: From research to implementation. Vol. 2. Concepts and methodology. Rockville, MD: Agency for Healthcare Research and Quality.
Ashton, C.M., & Wray, N.P. (1996). A conceptual framework for the study of early readmission as an indicator of quality care. Social Science and Medicine, 43, 1533–1541. doi:10.1016/S0277-9536 (96)00049-4
Bowles, K.H., Foust, J.B., & Naylor, M. (2003). Hospital discharge referral decision making: A multidisciplinary decision. Applied Nursing Research, 16(3), 134–143. doi:10.1016/S0897-1897(03)00048-X
Bowles, K.H., Naylor, M.D., & Foust, J.B. (2002). Patient characteristics at hospital discharge and a comparison of home care referral decisions. Journal of the American Geriatrics Society, 50, 336–342. doi:10.1046/j.1532-5415.2002.50067.x
Bowles, K.H., Ratcliffe, S.J., Holmes, J.H., Liberatore, M., Nydick, R., & Naylor, M.D. (2008). Post-acute referral decisions made by multidisciplinary experts compared to hospital clinicians and the patients’ 12-week outcomes. Medical Care, 46, 158–166. doi:10.1097/MLR.0b013e31815b9dc4
Brody, A.A., Ciemins, E., Newman, J., & Harrington, C. (2010). The effects of an inpatient palliative care team of discharge disposition. Journal of Palliative Medicine, 13, 541–548. doi:10.1089/jpm .2009.0300
Charlson, M.E., Pompei, P., Ales, K.L., & MacKenzie, C.R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40, 373–383. doi:10.1016/0021-9681(87)90171-8
Desai, M.M., Stauffer, B.D., Feringa, H.H., & Schreiner, G.C. (2009). Statistical models and patient predictors of readmission for acute myocardial infarction—A systematic review. Cardiovascular Qualitative Outcomes, 2, 500–507. doi:10.1161/circoutcomes.108.832949
Donabedian, A. (1988). The quality of care: How can it be assessed? JAMA, 260, 1743–1748. doi:10.1001/jama.1988.03410120089033
Gerhardt, G., Alshdye, Y., Hickman, P., Oelschlaeger, P., Rollins, E., & Brennan, N. (2013). Data shows reduction in Medicare hospital readmission rates during 2012. Medicare and Medicaid Research Review, 3(2), E1–E11. doi:10.5600/mmrr.003.02.b01
Gewandter, J.S., Fan, L., Magnuson, A., Mustian, K., Peppone, L., Heckler, C., . . . Mohile, S.G. (2013). Falls and functional impairments in cancer survivors with chemotherapy-induced peripheral neuropathy (CINP): A University of Rochester CCOP study. Supportive Care in Cancer, 21, 2059–2066. doi:10.1007/s00520-013-1766-y
Glasgow, M.E., & Zoucha, R. (2011). Role strain in the doctorally prepared advanced practice nurse. In M. Dreher and M.E. Glasgow (Eds.), Role development for doctoral advanced nursing practice (pp. 213–226). New York, NY: Springer.
Greenblatt, D.Y., Weber, S.M., O’Connor, E.S., LoConte, N.K., Liou, J.I., & Smith, M.A. (2010). Readmission after colectomy for cancer predicts one-year mortality. Annals of Surgery, 251, 659–669. doi:10.1097/SLA.0b013e3181d3d27c
Hendren, S., Morris, A.M., Zhang, W., & Dimick, J. (2011). Early discharge and hospital readmission after colectomy for cancer. Diseases of the Colon and Rectum, 54, 1362–1367. doi:10.1097/DCR.0b013e31822b72d3
Henretta, M.S., Scalici, J.M., Engelhard, C.L., & Duska, L.R. (2011). The revolving door: Hospital readmissions of gynecologic oncology patients. Gynecologic Oncology, 122, 479–483. doi:10.1016/j.yg yno.2011.05.011
Institute of Medicine. (2011). The future of nursing: Leading change, advancing health. Retrieved from http://www.iom.edu/Reports/2010/The-Future-of-Nursing-Leading-Change-Ad…
Institute of Medicine. (2013). Delivering high quality cancer care: Charting a new course for a system in crisis. Washington, DC: National Academies Press.
Jencks, S.F., Williams, M.V., & Coleman, E.A. (2009). Rehospitalizations among patients in the Medicare fee-for-service program. New England Journal of Medicine, 360, 1418–1428. doi:10.1056/NEJMsa0803563
Joynt, K.E., & Jha, A.K. (2013). A path forward on Medicare readmissions. New England Journal of Medicine, 368, 1175–1177. doi:10.1056/NEJMp1300122
Kansagara, D., Englander, H., Salanitro, A., Kagen, D., Thoebald, C., Freeman, M., & Kripalani, S. (2011). Risk prediction models for hospital readmission—A systematic review. JAMA, 306, 1688–1698. doi:10.1001/jama.2011.1515
Kind, A.H., Smith, M.A., Frytak, J.R., & Finch, M.D. (2007). Bouncing back: Patterns and predictors of complicated transitions 30 days after hospitalization for acute ischemic stroke. Journal of the American Geriatrics Society, 55, 365–373. doi:10.1111/j.1532-5415.2007.01091.x
Lichtman, J.H., Leifheit-Limson, E.C., Jones, S.B., Watanabe, E., Bernheim, S.M., Phipps, M.S., . . . Goldstein, L.B. (2010). Predictors of hospital readmission after stroke: A systematic review. Stroke, 41, 2525–2533. doi:10.1161/STROKEAHA.110.599159
MedPAC. (2007). Report to Congress: Promoting greater efficiency in Medicare. Retrieved from http://www.caretransitions.org/documents/MedPACreport.pdf
Naylor, M.D., Aiken, L.H., Kurtzman, E.T., Olds, D.M., & Hirschman, K.B. (2011). The importance of transitional care in achieving health reform. Health Affairs, 30, 746–754. doi:10.1377/hlthaff.2011.0041
Nelson, C., Chand, P., Oloimooja, J., & Rembert, G. (2011). Inpatient palliative care consults and the probability of hospital readmission. Permanente Journal, 15(2), 48–51. doi:10.7812/TPP/10-142
Pham, H.H., Schrag, D., O’Malley, A.S., Wu, B., & Bach, P.B. (2007). Care patterns in Medicare and their implications for pay performance. New England Journal of Medicine, 356, 1130–1139. doi:10.1056/NEJMsa063979
Price, R.A., Stranges, E., & Elixhauser, A. (2012). Cancer hospitalizations for adults, 2009. Retrieved from www.hcup-us.ahrq.gov/reports/statbriefs/sb125.jsp
Reddy, D.M., Townsend, C.M., Kuo, Y.F., Freeman, J.L., Goodwin, J.S., & Riall, T.S. (2009). Readmission after pancreatectomy for pancreatic cancer in Medicare patients. Journal of Gastrointestinal Surgery, 13, 1963–1975. doi:10.1007/s11605-009-1006-4
Rochefort, M., & Tomlinson, J.S. (2012). Unexpected readmissions after major cancer surgery: An evaluation of readmissions as a quality of care indicator. Surgical Oncology Clinics of North America, 21, 397–405. doi:10.1016/j.soc.2012.03.004
Ross, J.S., Mulvey, G.K., Stauffer, B., Patlolla, V., Bernheim, S.M, Keenan, P.S., & Krumholz, H.M. (2008). Statistical models and patient predictors of readmission for heart failure. Archives of Internal Medicine, 168, 1371–1386. doi:10.1001/archinte.168.13.1371
Spoelstra, S.L., Given, B.A., Schutte, D.L., Sikorskii, A., You, M., & Given, C.W. (2013). Do older adults with cancer fall more often? A comparative analysis of falls in those with and without cancer [Online exclusive]. Oncology Nursing Forum, 40, E69–E78. doi:10.1188/13.ONF.E69-E78
Stevens, J.A., Ballesteros, M.F., Mack, K.A., Rudd, R.A., DeCaro, E., Adler, G., & Phil, M. (2012). Gender differences in seeking care for falls in the aged Medicare population. American Journal of Preventive Medicine, 43, 59–62. doi:10.1016/j.amepre.2012.03.008
Stevens, J.A., Mack, K.A., Paulozzi, L.J., & Ballesteros, M.F. (2008). Self-reported falls and fall-related injuries among persons aged ≥ 65 years—United States. Journal of Safety Research, 39, 345–349. doi:10.1016/j.jsr.2008.05.002
Stone, C., Lawlor, P.G., Savva, G.M., Bennett, K., & Kenny, R.A. (2012). Prospective study of falls and risk factors for falls in adults with advanced cancer. Journal of Clinical Oncology, 30, 2128–2133.
Tuggle, C.T., Park, L.S., Roman, S., Udelsman, R., & Sosa, J.A. (2010). Rehospitalization among elderly patients with thyroid cancer after thyroidectomy are prevalent and costly. Annals of Surgical Oncology, 17, 2817–2823. doi:10.1245/s10434-1144-7
Weaver, C., Schiech, L., Held-Warmkessel, J., Kedziera, P., Haney, E., DiLullo, G., . . . Barsevick, A. (2006). Risk for unplanned hospital readmission of patients with cancer: Results of a retrospective medical record review [Online exclusive]. Oncology Nursing Forum, 33, E44–E52. doi:10.1188/06.ONF.E44-E52
Yermilov, I., Bentrem, D., Sekeris, E., Sushma, J., Maggard, M.A., Yo, C.Y., & Tomlinson, J.S. (2009). Redmissions following pancreaticoduodenectomy for pancreas cancer: A population-based appraisal. Annals of Surgical Oncology, 16, 554–561.
About the Author(s)
Clara Granda-Cameron, DrNP, CRNP, AOCN®, is a coordinator of the palliative care program in the Abramson Cancer Center at Pennsylvania Hospital; Maryam Behta, PharmD, is a director of clinical performance improvement at the University of Pennsylvania Health System; Mary Hovinga, PhD, MPH, is an associate professor in the Departments of Epidemiology and Biostatistics, and Al Rundio, PhD, DNP, NEA-BC, is an associate dean for post-licensure nursing programs in the College of Nursing and Health Professions, both at Drexel University; and David Mintzer, MD, is a chief in the section of hematology-oncology at the Pennsylvania Hospital, all in Philadelphia, PA. This study was supported, in part, by the APN/DNP Student Fellowship Award from the ONS Foundation. Granda-Cameron can be reached at claritacameron@gmail.com, with copy to editor at ONFEditor@ons.org. (Submitted August 2014. Accepted for publication November 13, 2014.)

