Impact of Perceived Stigma in People Newly Diagnosed With Lung Cancer: A Cross-Sectional Analysis
Objectives: To investigate perceived stigma and its possible associations with treatment expectations and preferences in newly diagnosed patients with lung cancer.
Sample & Setting: 274 patients with lung cancer diagnosed in the previous four months at oncology and respiratory outpatient clinics in Australia.
Methods & Variables: Participants completed a self-report survey about perceived lung cancer stigma and treatment expectations and preferences.
Results: A mean perceived stigma score of 52 of a possible 124 was reported, which is lower than scores reported in other studies using the same measure; the current study determined that perceived lung cancer stigma was observed less frequently. Significantly higher scores were observed in participants who were younger or who had a history of smoking. Perceived lung cancer stigma was significantly related to treatment expectations. No relationship was found between perceived lung cancer stigma and treatment preferences.
Implications for Nursing: Healthcare providers are in a key position to provide support and communicate empathetically with patients to minimize potential stigma experiences.
Jump to a section
Lung cancer is a disease frequently diagnosed in the advanced stages, with treatment often focused on management of symptoms and enhancement of quality of life rather than on curative interventions (Langendijk et al., 2000; Stinchcombe & Socinski, 2009). Weighing the potential risks and benefits of treatment, and whether it is seen as worthwhile, is an important consideration when making treatment decisions (Blinman, Alam, Duric, McLachlan, & Stockler, 2010).
In accordance with the provision of patient-centered care, identifying the patient’s attitudes and preferences regarding treatment becomes an important aspect of the decision-making process. A systematic review by Schmidt, Damm, Prenzler, Golpon, and Welte (2015) found that people with lung cancer commonly placed greater value on treatment that extended life rather than on treatment that improved quality of life. Despite this, most people with lung cancer reportedly prefer to take a more passive approach to their treatment decisions (Schmidt et al., 2015). People with lung cancer also have inaccurate treatment expectations and misconceptions of treatment being curative instead of alleviating symptoms (Weeks et al., 2012). Patients may feel unable to make informed decisions about their care that aligns with their values or may be uncomfortable with expressing their wishes.
The patient–provider relationship can be a critical element that influences treatment decisions and expectations (Lin et al., 2014). For example, a qualitative study by Sharf, Stelljes, and Gordon (2005) found that people with lung cancer may refuse treatment because of distrust toward medical procedures and uncertainty around the recommendations given by their healthcare providers. The ways in which treatment options are communicated to the patient may also have an impact on treatment expectations. Anecdotal evidence suggests that healthcare providers may be pessimistic about lung cancer treatment (Hamann et al., 2013; Wassenaar et al., 2007) and that patients themselves can view treatment as being pointless (Sharf et al., 2005). People with lung cancer have also reported experiencing negative responses from their healthcare provider in relation to smoking behavior (Hamann et al., 2014). The role of stigma should also be considered, with perceived lung cancer stigma found to be associated with poor patient–provider communication (Shen, Hamann, Thomas, & Ostroff, 2016).
Health-related stigma refers to a set of negative views or beliefs that usually manifests because of a particular undesirable feature associated with an illness or to behaviors associated with such illness (Weiss, Ramakrishna, & Somma, 2006). According to modified labeling theory, when individuals are diagnosed with a condition (e.g., lung cancer), social perceptions of that illness become personally relevant and foster negative internalized feelings (Link, Cullen, Struening, Shrout, & Dohrenwend, 1989). The impact of being labeled, by others or by themselves, may contribute to poor psychosocial and health-related outcomes for those affected. Although this theory is commonly used in relation to the stigma of mental health conditions, it also has relevance to cancer. People diagnosed with lung cancer commonly report experiences of perceived stigma (Chambers et al., 2012), partly as a result of the known links between smoking and lung cancer. Patients, regardless of their smoking history, have reported feeling stigmatized by family, friends, and healthcare providers (Chapple, Ziebland, & McPherson, 2004). Awareness of the negative public perceptions associated with lung cancer also leads patients to attribute feelings of guilt and self-blame to their diagnosis (Dirkse & Giese-Davis, 2012). Lung cancer stigma has been linked to various psychosocial (e.g., anxiety, depression, poorer quality of life, social isolation) (Rose, Paul, Boyes, Kelly, & Roach, 2017) and health-related outcomes (e.g., delays in seeking medical help) (Carter-Harris, Hermann, Schreiber, Weaver, & Rawl, 2014).
Perceived lung cancer stigma is a clinically important issue to examine because of its potential association with adverse patient outcomes (Rose et al., 2017). Little is known about how perceived lung cancer stigma affects patients’ views on their cancer treatment. A better understanding of how the stigmatization process potentially interacts with treatment decision making would assist in ensuring that patients with lung cancer receive the best possible care that aligns with their needs and preferences. The purposes of this study were as follows:
• Describe in people newly diagnosed with lung cancer their (a) level of perceived lung cancer stigma and assess whether scores are associated with selected participant characteristics; (b) treatment expectations related to providing a cure, extending life, and relieving symptoms; and (c) treatment preferences related to extending life and relieving symptoms.
• Examine in people newly diagnosed with lung cancer (a) the relationship between perceived lung cancer stigma and treatment expectations and preferences and (b) whether preferred decision-making involvement and satisfaction in treatment recommendations play a mediating role in the potential relationship between perceived lung cancer stigma and treatment expectations and preferences.
The authors hypothesized that participants with greater perceived lung cancer stigma would report low treatment expectations and treatment that reflected a desire for pain relief rather than for life extension, after controlling for selected covariates.
Methods
A prospective cross-sectional study was conducted. This study was nestled within the baseline phase of a randomized, controlled trial exploring the benefits of three approaches (online versus telephone versus mailed contact) to providing psychosocial support to people newly diagnosed with lung cancer (Paul et al., 2016). As a result, this study used the same eligibility criteria as the trial; adults who had received a primary diagnosis of lung cancer within the past four months and were proficient in English were eligible to participate in the study. Potential participants were identified and invited by clinic staff or a research assistant (under the direction of clinic staff) during scheduled respiratory and oncology appointments at outpatient clinics (n = 31) in Australia from September 2014 to December 2016. Consenting participants were asked to complete a self-report survey. As many as two reminders (via mail and telephone) at two-week intervals were provided to nonrespondents to minimize attrition.
Measures
The survey was pilot-tested with 10 volunteers; it sought opinions about the clarity and sensitivity of instructions and items, completeness of response options, and format and length. Characteristics were measured by asking for the following:
• Age
• Gender
• Marital status
• Education
• Employment
• Aboriginal or Torres Strait Islander status
• Language at home
• Socioeconomic status (i.e., private health insurance or concession card [issued by the Australian government, entitling the user to health services and treatment at a reduced cost])
• Smoking status
• Lung cancer information
Independent variable: Perceived lung cancer stigma was measured using the 31-item Cataldo Lung Cancer Stigma Scale (CLCSS) (Cataldo, Slaughter, Jahan, Pongquan, & Hwang, 2011), which assesses four domains: (a) stigma/shame, (b) social isolation, (c) discrimination, and (d) smoking. Responses were provided on a four-point Likert-type scale ranging from 1 (strongly disagree) to 4 (strongly agree), and subscores were calculated for a total score. Total scores had a possible range of 31–124, with higher scores indicating greater perceived stigma. The CLCSS has been shown to be a valid and reliable instrument in a sample of patients with lung cancer (Cronbach alpha of 0.96 for the total scale, 0.97 for the stigma/shame domain, 0.98 for the social isolation domain, 0.95 for the discrimination domain, and 0.75 for the smoking domain) (Cataldo et al., 2011).
Dependent variables: Treatment expectations were measured using items adapted and modified from the CanCORS (Cancer Care Outcomes and Research Surveillance Consortium) study (Malin et al., 2006). Participants were asked the following questions:
• “Do you feel treatment will help you live longer?”
• “Do you feel treatment will cure your cancer?”
• “Do you feel treatment will help you with symptoms you were having because of your cancer?”
Participants responded to these questions on a five-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree); individual question scores were calculated to provide a total score with a possible range of 3–15. Higher scores indicated more positive treatment expectations.
Treatment preferences were measured using an item adapted from the CanCORS study (Malin et al., 2006) that asked participants to complete the statement “If you had to make a choice now, would you prefer to have treatment that” with “extends life as much as possible” or “relieves pain or discomfort as much as possible.” Another possible response was “do not know.” Responses were collapsed into “extends life” and “relieves pain” for regression modeling.
Mediating variables: Participants’ preferred involvement in cancer treatment decision making was measured using the Control Preferences Scale (Degner, Sloan, & Venkatesh, 1997). Responses were categorized as “patient-controlled,” “physician-controlled,” or “shared control.”
Satisfaction with treatment recommendations was measured using an author-developed item: “I believe the doctor(s) have offered me all the possible treatment options.” Participants responded to this item using a five-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicated greater satisfaction.
Sample Size
Based on previous findings (Malin et al., 2006), the probability of the outcome (negative treatment expectations and preferences) was estimated to be about 40%. A sample of 300 participants had 80% power to find a statistically significant effect at the 5% significance level if the odds ratio (OR) associated with a 10-unit increase in stigma is at least 1.2. This means that each 10-unit increase in stigma is associated with a 20% increase in the odds of the outcome (or about a 12.5% increase in risk). A sample size of about 300 would also provide the study with sufficient power to find small to medium mediation effect sizes (Fritz & MacKinnon, 2007).
Statistical Analysis
Descriptive statistics (means, standard deviations [SDs], and ranges for continuous variables; frequencies and percentages for categorical variables) were performed to report sample characteristics, perceived lung cancer stigma, and treatment expectations and preferences. Linear regression was used to assess whether age, gender, and smoking status affected perceived lung cancer stigma scores.
The association between perceived lung cancer stigma and treatment expectations was examined using quantile regression (normality of residuals was not met), and the association between stigma and treatment preferences was examined using binary logistic regression. Assumptions of linear (unusual and influential data, normality of residuals, heteroscedasticity, multicollinearity, and nonlinearity) and ordinal (proportional odds assumption) regression modeling were checked. Potential confounding was examined using adjusted regression modeling; confounders included sociodemographic and disease-related covariates chosen a priori based on clinical knowledge and existing literature. Crude and adjusted beta coefficients (quantile regression), ORs (ordinal regression), 95% confidence intervals (CIs), and p values are reported for the regression models.
Mediation of the relationship between perceived lung cancer stigma and treatment expectations and preferences through preferred involvement in decision making, as well as satisfaction with treatment recommendations, was explored per the methodology of Preacher and Hayes (2004).
Stata, version 14.1, was used for all statistical analyses; p values of less than 0.05 were considered indicative of significant differences. When more than 10% of the responses from the CLCSS were missing, the case was removed from analysis.
Ethical Considerations
Ethical approval was obtained from the human research ethics committees of the following entities: Epworth HealthCare, Greenslopes Private Hospital, Hunter New England Local Health District, St. John of God Health Care, Uniting HealthCare, University of Newcastle, and University of Tasmania. Participants provided informed written consent.
Results
A total of 401 patients were eligible and approached for participation. Of these, 28 did not respond to the invitation even after the reminders, and 22 declined to participate. Of the remaining 351 who consented, 274 completed the study survey (68% response rate). No significant differences were noted between those who did and who did not consent to participate in terms of gender. The mean age of participants was 67.3 years (SD = 8.9), with a range of 37–87 years. Tables 1 and 2 further describe participant characteristics. 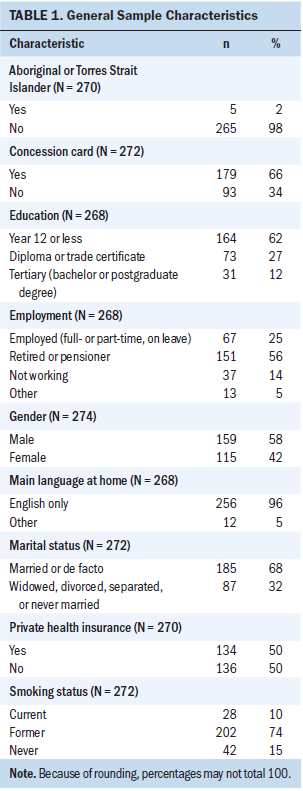
Perceived Stigma and Treatment Expectations and Preferences
Descriptive statistics of the study variables are provided in Table 3. Overall, participants reported a mean perceived lung cancer stigma score of 52 of a possible 124 (SD = 15). Higher scores were significantly associated with being younger in age (beta = –0.394, p < 0.001) and having a history of smoking (beta = –10.083, p < 0.001). In terms of treatment expectations, participants reported a mean score of 10.4 of a possible 15 (SD = 2.6); a majority of participants (n = 211, 77%) either agreed or strongly agreed that treatment would help them live longer. Regarding treatment preferences, 65% of participants (n = 170) reported that they wanted treatment to extend life, and 21% (n = 55) reported that they wanted treatment to assist with symptoms. 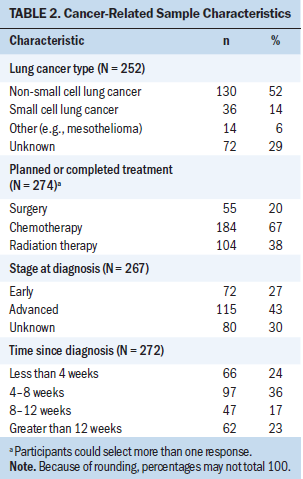
Associations Between Perceived Stigma and Treatment Expectations and Preferences
A significant positive relationship was found between perceived lung cancer stigma and treatment expectations (p = 0.049) (see Table 4). After adjusting for gender, age, education, socioeconomic status, smoking status, and lung cancer stage, this relationship was no longer significant. Perceived lung cancer stigma alone was found to explain 1.2% of the variability in treatment expectation scores (pseudo R2 = 0.012), and after adjusting for all other confounders, 8.1% of the variability was explained (pseudo R2 = 0.0813). Mediation of the relationship through either preferred involvement in treatment decision making or satisfaction with treatment recommendations was not supported. 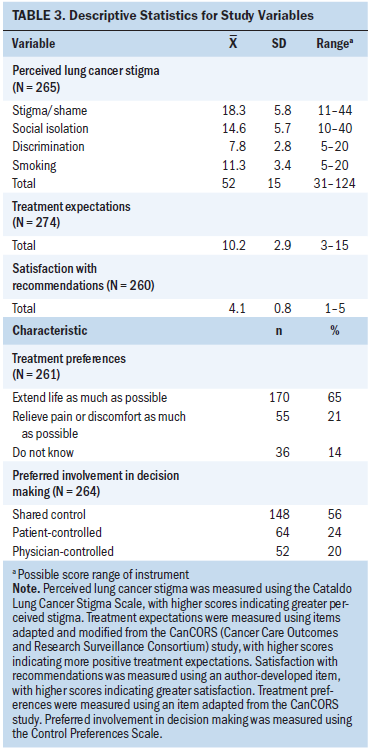
The relationship between perceived lung cancer stigma and treatment preferences was not statistically significant (OR = 0.996, 95% CI [0.975, 1.016], p = 0.676, results for confounders not shown). Mediation through involvement in treatment decision making or satisfaction with treatment recommendations was, as a result, not tested. 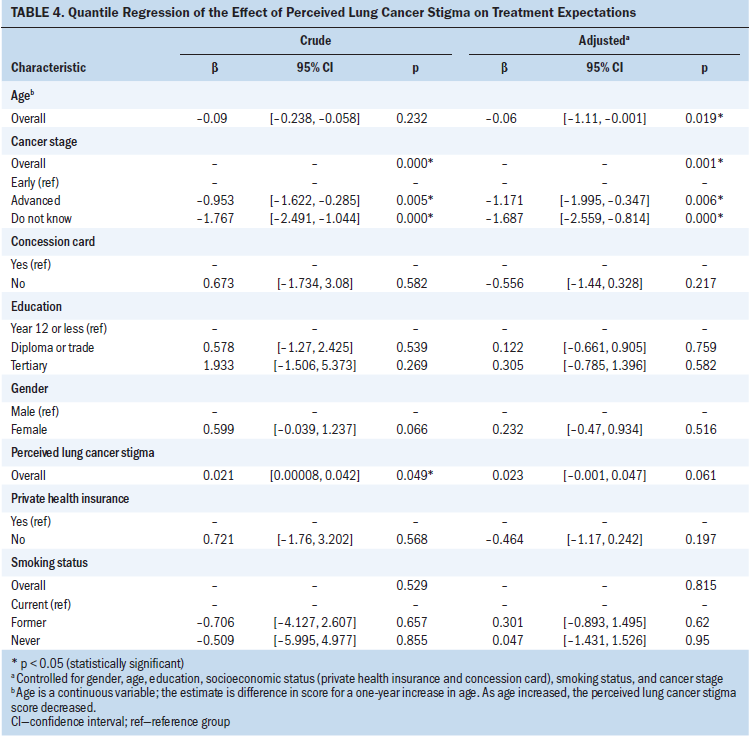
Discussion
Contrary to previous research, the current study found that perceived lung cancer stigma was experienced less frequently. Participants in the current study reported a mean perceived lung cancer stigma score of 52, which is considerably lower than that of other studies using the same measure, with scores ranging from 69–103 (Brown Johnson, Brodsky, & Cataldo, 2014; Carter-Harris et al., 2014; Cataldo & Brodsky, 2013; Cataldo et al., 2011). This difference may be attributable to various factors. For example, the current study focused on participants who were recently diagnosed. Although previous studies may have also included patients recently diagnosed, the time since diagnosis was not reported. Given the short length of time since diagnosis, participants in the current study may not have yet been exposed to potentially stigmatizing experiences. Because lung cancer stigma has yet to be explored longitudinally, it is difficult to determine when individuals may experience stigma during the stages of cancer diagnosis, treatment, and ongoing survivorship (if at all). However, a longitudinal study of people newly diagnosed with lung cancer found that, over time, more patients in the cohort reported depressive symptoms (Sullivan et al., 2016). Because perceived lung cancer stigma has been shown to be associated with outcomes such as depression, stigma may also manifest over time.
Differences in sampling also were noted. Some strengths of the current study were the large sample size (participants were actively recruited via outpatient clinics) and the strong response rate. Previous studies (Brown Johnson et al., 2014; Carter-Harris et al., 2014; Cataldo & Brodsky, 2013; Cataldo et al., 2011) used convenience sampling methods, which can be more vulnerable to selection bias and compromise the representativeness of the sample. The sample in the current study had a higher proportion of male participants and people aged 60 years or older, which is more reflective of the overall population of patients with lung cancer (Australian Institute of Health and Welfare, 2014). Older men may exhibit stoic attitudes, opting to keep feelings to themselves and “putting on a brave face” (Tod, Craven, & Allmark, 2008, p. 340). The other studies had predominantly female and younger samples (Brown Johnson et al., 2014; Carter-Harris et al., 2014; Cataldo & Brodsky, 2013; Cataldo et al., 2011); younger people (men and women) and women (including younger and older age brackets) have been noted to be more likely to report higher levels of distress (Hulbert-Williams, Neal, Morrison, Hood, & Wilkinson, 2012; Trask & Griffith, 2004).
Participants with a history of smoking or who were younger in age reported greater perceived lung cancer stigma. The role of smoking status and stigma is unsurprising and has been frequently alluded to in the literature. Patients who disclose their lung cancer diagnosis are commonly assumed to be smokers (Hamann et al., 2014; Tod et al., 2008), and studies have found that patients with lung cancer with a history of smoking report feelings of blame, shame, guilt, anger, and regret (Criswell, Owen, Thornton, & Stanton, 2016; Hamann et al., 2014). These feelings may stem from the perceived responsibility of disease onset, which can influence responses from others (e.g., sympathy, pity, assistance) and, in turn, how patients view themselves (Weiner, Perry, & Magnusson, 1988). The relationship between perceived stigma and younger age may be attributable to public health initiatives aimed at denormalizing smoking (Bayer, 2008). The health implications of smoking are now well documented, with younger populations being more aware of the risks when beginning to smoke compared to their older counterparts. A qualitative study of young adults reported that nonsmokers perceived smoking to be illogical and self-destructive and, as a result, would respond harshly to smokers (McCool, Hoek, Edwards, Thomson, & Gifford, 2013).
The finding that perceived lung cancer stigma was not associated with treatment preferences or expectations when controlling for confounders is promising. The sample in this study had favorable expectations of treatment; most participants believed that therapy would help them live longer and would assist with symptoms. This finding is consistent with other studies that have explored patient expectations of radiation therapy and chemotherapy in advanced- stage lung cancer (Chen et al., 2013; Weeks et al., 2012). One-third of the current sample also reported an expectation that treatment would provide a cure. Although optimism may confer significant health benefits (e.g., improved quality of life) (Wrosch & Scheier, 2003), it should be balanced with a realistic understanding of treatment. Studies have reported that a contrast exists between physician and patient views and preferences for treatment (Chu et al., 2007; Davidson et al., 2011). As a result, patients need to express their preferences. Most participants in the current study indicated a preference for making decisions with their healthcare provider or on their own, suggesting that they may have felt adequately supported, informed, and comfortable when considering their treatment choices. The benefits of decisional involvement have been acknowledged (e.g., improved quality of life, greater social and physical functioning) (Hack, Degner, Watson, & Sinha, 2006).
However, the direct association of perceived lung cancer stigma with treatment expectations is of particular interest. Qualitative data suggest that pessimistic treatment expectations may cause patients to delay seeking medical help (Tod et al., 2008). Consequently, the possible influence of perceived lung cancer stigma in patients should be recognized. Care may need to be taken with how lung cancer is portrayed via population health initiatives, such as anti-tobacco campaigns. These campaigns can, at times, be confronting and graphic and highlight the poor prognosis associated with lung cancer. For patients, viewing these campaigns may be upsetting and distressing (Chapple et al., 2004), and they may lead to feelings of hopelessness because of the frequent focus on fatalism (Tod et al., 2008). Anti-tobacco campaigns may need to weigh public benefits against the potential detriments and offer more balanced media messages.
Care also is needed within the patient–provider relationship, particularly if pessimistic views about lung cancer exist, as suggested by anecdotal evidence (Hamann et al., 2013; Wassenaar et al., 2007). Exposure to negative attitudes from healthcare providers during consultations may affect the exchange of information about treatment, as well as influence patient perceptions and the role that patients take in their care planning. Perceived stigma can impede critical opportunities in facilitating an open dialogue between patients and healthcare providers to promote best possible care (Tod et al., 2008).
Limitations
Various limitations of this study need to be noted. Because the sample consisted only of people with English language ability sufficient to complete a survey, the data are not generalized to patients who do not speak English. Exploring experiences and opinions across different cultures would assist in understanding the scope of perceived stigma but also in providing culturally sensitive support. The current sample consisted only of patients who were within four months of diagnosis at the time of recruitment; therefore, the data do not reflect the experiences of patients at all stages of the cancer journey. This study used a cross-sectional design; causality cannot be determined. Given the nature of the findings, exploring whether perceived lung cancer stigma is experienced later in a patient’s journey would be beneficial to assess best timing of support services to improve patient outcomes. A large proportion of the sample was recruited by outpatient clinic staff. It is possible that more optimistic patients were selectively invited for participation; however, attempts to minimize this were made by approaching consecutive patients who met eligibility.
Implications for Nursing
The findings of this study have important implications for practice and research. In this study, the sample of people newly diagnosed with lung cancer reported low scores of perceived stigma. This is encouraging for healthcare providers because it suggests that specifically addressing stigma in treatment-related discussions is not generally necessary for all patients. Younger participants or those with a history of smoking were more likely to report higher stigma scores. Nurses may need to display particular sensitivity and clarity when assessing or discussing smoking history to minimize the likelihood that perceived stigma interferes with the rapport between nurses and patients. In addition, nurses should consider how emotions related to a lung cancer diagnosis can affect the patient, given that perceived lung cancer stigma has been found to be associated with poor psychosocial outcomes. Stigma-related perceptions could be included in assessments of patients’ well-being, and attempts could be made to ensure that oncology counselors or social workers are also aware of these issues.
Another implication of this study is the importance of effective patient–provider communication. Good patient–provider communication has been found to be associated with low levels of perceived lung cancer stigma (Shen et al., 2016). Healthcare providers, through their communication, are in a key position to influence patients’ understanding and outlook regarding their treatment. Information concerning treatment should not only be delivered appropriately for sustained understanding in patients but also empathetically to minimize any potential stigma. Various communication practices (e.g., displaying respect; showing empathy and being encouraging; listening, clarifying, and summarizing information; checking for understanding and endorsing question-asking) can promote favorable outcomes in patients (Baile & Aaron, 2005).
Additional research is still needed to assess patient experiences with lung cancer stigma and the needs of these patients. Although interventions for lung cancer stigma may not be pertinent for people soon after diagnosis, understanding the possible effects that this stigma can have on patients during their cancer journey warrants further exploration. 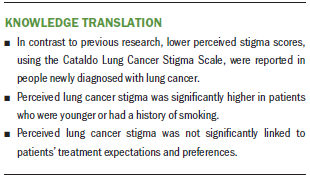
Conclusion
Findings from this study provide additional evidence in the growing lung cancer stigma literature. The lower scores of perceived lung cancer stigma reported by the sample indicate the varied experiences of people with lung cancer; these scores may be reflective of the timing of diagnosis or of various characteristics (e.g., gender, age, behavior such as smoking status). The finding that perceived lung cancer stigma is not associated with treatment expectations or preferences is encouraging, particularly when considering previous reports of the adverse psychosocial and clinical outcomes that perceived stigma may impose on patients with lung cancer. However, to aid understanding, it is essential that perceived stigma be measured at various points of the cancer trajectory. Therefore, investigating longitudinal experiences will be important in consolidating interpretations. [[{"fid":"47406","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
The authors gratefully acknowledge all participants for their involvement in the study, the clinics and their staff for their assistance with recruitment, the volunteers for their input in refining the survey, Paula Bridge, BPsych(Hons), and Della Roach, BBiomedSc(Hons), from the Priority Research Centre for Health Behavior for their assistance with participant recruitment, and Christopher Oldmeadow, PhD, from the Clinical Research Design, Information Technology, and Statistical Support unit at the Hunter Medical Research Institute for statistical advice.
About the Author(s)
Shiho Rose, BFoodScHumNut, is a PhD candidate in the School of Medicine and Public Health; Brian Kelly, BMed, PhD, FRANZCP, FAChPM, is the director of clinical science in the Centre for Brain and Mental Health Research; Allison Boyes, PhD, MPH, BA, is a research fellow, and Martine Cox, BNutDiet, is a research assistant, both in the School of Medicine and Public Health, all at the University of Newcastle in Callaghan, New South Wales, Australia; Kerrin Palazzi, MPH, is a statistician at the Hunter Medical Research Institute in New Lambton Heights, New South Wales; and Christine Paul, PhD, is a professor in the School of Medicine and Public Health at the University of Newcastle. This research was supported by funding from a National Health and Medical Research Council (NHMRC) Partnerships for Better Health grant (APP1055408) and infrastructure funding from the Hunter Medical Research Institute. During the writing of this article, Rose was supported by a University of Newcastle Research Postgraduate Scholarship and a Hunter Cancer Research Alliance statistical support grant, Boyes was supported by an NHMRC Early Career Fellowship (APP1073317) and a Cancer Institute NSW Early Career Fellowship (13/ECF/1-37), and Paul was supported by a NHMRC Career Development Fellowship (APP1061335) and a Hunter Medical Research Institute Fellowship. Rose, Kelly, Boyes, and Paul contributed to the conceptualization and design. Rose and Cox completed the data collection. Palazzi provided statistical support. Rose and Palazzi provided the analysis. All authors contributed to the manuscript preparation. Rose can be reached at shiho.rose@newcastle.edu.au, with copy to ONFEditor@ons.org. (Submitted November 2017. Accepted May 14, 2018.)
References
Australian Institute of Health and Welfare. (2014). Cancer in Australia: An overview, 2014. Retrieved from https://www.aihw.gov.au/getmedia/79c940b1-2438-45c8-99e2-a4b593253ccd/1…
Baile, W.F., & Aaron, J. (2005). Patient-physician communication in oncology: Past, present, and future. Current Opinion in Oncology, 17, 331–335.
Bayer, R. (2008). Stigma and the ethics of public health: Not can we but should we. Social Science and Medicine, 67, 463–472. https://doi.org/10.1016/j.socscimed.2008.03.017
Blinman, P., Alam, M., Duric, V., McLachlan, S.-A., & Stockler, M.R. (2010). Patients’ preferences for chemotherapy in non-small-cell lung cancer: A systematic review. Lung Cancer, 69, 141–147. https://doi.org/10.1016/j.lungcan.2010.05.001
Brown Johnson, C.G., Brodsky, J.L., & Cataldo, J.K. (2014). Lung cancer stigma, anxiety, depression, and quality of life. Journal of Psychosocial Oncology, 32, 59–73. https://doi.org/10.1080/07347332.2013.855963
Carter-Harris, L., Hermann, C.P., Schreiber, J., Weaver, M.T., & Rawl, S.M. (2014). Lung cancer stigma predicts timing of medical help–seeking behavior [Online exclusive]. Oncology Nursing Forum, 41, E203–E210. https://doi.org/10.1188/14.ONF.E203-E210
Cataldo, J.K., & Brodsky, J.L. (2013). Lung cancer stigma, anxiety, depression and symptom severity. Oncology, 85, 33–40. https://doi.org/10.1159/000350834
Cataldo, J.K., Slaughter, R., Jahan, T M., Pongquan, V.L., & Hwang, W.J. (2011). Measuring stigma in people with lung cancer: Psychometric testing of the Cataldo Lung Cancer Stigma Scale [Online exclusive]. Oncology Nursing Forum, 38, E46–E54. https://doi.org/10.1188/11.ONF.E46-E54
Chambers, S.K., Dunn, J., Occhipinti, S., Hughes, S., Baade, P., Sinclair, S., . . . O’Connell, D.L. (2012). A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BMC Cancer, 12, 184. https://doi.org/10.1186/1471-2407-12-184
Chapple, A., Ziebland, S., & McPherson, A. (2004). Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. BMJ, 328, 1470. https://doi.org/10.1136/bmj.38111.639734.7C
Chen, A.B., Cronin, A., Weeks, J.C., Chrischilles, E.A., Malin, J., Hayman, J.A., & Schrag, D. (2013). Expectations about the effectiveness of radiation therapy among patients with incurable lung cancer. Journal of Clinical Oncology, 31, 2730–2735. https://doi.org/10.1200/JCO.2012.48.5748
Chu, D.-T., Kim, S.-W., Kuo, H.-P., Ozacar, R., Salajka, F., Krishnamurthy, S., . . . Wang, L. (2007). Patient attitudes towards chemotherapy as assessed by patient versus physician: A prospective observational study in advanced non-small cell lung cancer. Lung Cancer, 56, 433–443. https://doi.org/10.1016/j.lungcan.2007.01.028
Criswell, K.R., Owen, J.E., Thornton, A.A., & Stanton, A.L. (2016). Personal responsibility, regret, and medical stigma among individuals living with lung cancer. Journal of Behavioral Medicine, 39, 241–253. https://doi.org/10.1007/s10865-015-9686-6
Davidson, P.M., Jiwa, M., Goldsmith, A.J., McGrath, S.J., DiGiacomo, M., Phillips, J.L., . . . Currow, D.C. (2011). Decisions for lung cancer chemotherapy: The influence of physician and patient factors. Supportive Care in Cancer, 19, 1261–1266. https://doi.org/10.1007/s00520-011-1176-y
Degner, L.F., Sloan, J.A., & Venkatesh, P. (1997). The Control Preferences Scale. Canadian Journal of Nursing Research, 29(3), 21–43.
Dirkse, D., & Giese-Davis, J. (2012). Shame and guilt in lung cancer: The stigma of lung cancer. Oncology Exchange, 11, S-10–S-12.
Fritz, M.S., & MacKinnon, D.P. (2007). Required sample size to detect the mediated effect. Psychological Science, 18, 233–239. https://doi.org/10.1111/j.1467-9280.2007.01882.x
Hack, T.F., Degner, L.F., Watson, P., & Sinha, L. (2006). Do patients benefit from participating in medical decision making? Longitudinal follow-up of women with breast cancer. Psycho-Oncology, 15, 9–19. https://doi.org/10.1002/pon.907
Hamann, H.A., Lee, J.-W., Schiller, J.H., Horn, L., Wagner, L.I., Chang, V.T.-S., & Fisch, M.J. (2013). Clinician perceptions of care difficulty, quality of life, and symptom reports for lung cancer patients: An analysis from the Symptom Outcomes and Practice Patterns (SOAPP) study. Journal of Thoracic Oncology, 8, 1474–1483. https://doi.org/10.1097/01.JTO.0000437501.83763.5d
Hamann, H.A., Ostroff, J.S., Marks, E.G., Gerber, D.E., Schiller, J.H., & Lee, S.J. (2014). Stigma among patients with lung cancer: A patient-reported measurement model. Psycho-Oncology, 23, 81–92. https://doi.org/10.1002/pon.3371
Hulbert-Williams, N., Neal, R., Morrison, V., Hood, K., & Wilkinson, C. (2012). Anxiety, depression and quality of life after cancer diagnosis: What psychosocial variables best predict how patients adjust? Psycho-Oncology, 21, 857–867. https://doi.org/10.1002/pon.1980
Langendijk, J.A., ten Velde, G.P., Aaronson, N.K., de Jong, J.M., Muller, M.J., & Wouters, E.F. (2000). Quality of life after palliative radiotherapy in non-small cell lung cancer: A prospective study. International Journal of Radiation Oncology, Biology, Physics, 47, 149–155.
Lin, J.J., Lake, J., Wall, M.M., Berman, A.R., Salazar-Schicchi, J., Powell, C., . . . Wisnivesky, J.P. (2014). Association of patient–provider communication domains with lung cancer treatment. Journal of Thoracic Oncology, 9, 1249–1254. https://doi.org/10.1097/JTO.0000000000000281
Link, B.G., Cullen, F.T., Struening, E., Shrout, P.E., & Dohrenwend, B.P. (1989). A modified labeling theory approach to mental disorders: An empirical assessment. American Sociological Review, 54, 400–423. https://doi.org/10.2307/2095613
Malin, J.L., Ko, C., Ayanian, J.Z., Harrington, D., Nerenz, D.R., Kahn, K.L., . . . Ganz, P.A. (2006). Understanding cancer patients’ experience and outcomes: Development and pilot study of the cancer care outcomes research and surveillance patient survey. Supportive Care in Cancer, 14, 837–848. https://doi.org/10.1007/s00520-005-0902-8
McCool, J., Hoek, J., Edwards, R., Thomson, G., & Gifford, H. (2013). Crossing the smoking divide for young adults: Expressions of stigma and identity among smokers and nonsmokers. Nicotine and Tobacco Research, 15, 552–556. https://doi.org/10.1093/ntr/nts136
Paul, C.L., Boyes, A.W., O’Brien, L., Baker, A.L., Henskens, F.A., Roos, I., . . . Banker, D. (2016). Protocol for a randomized controlled trial of proactive web-based versus telephone-based information and support: Can electronic platforms deliver effective care for lung cancer patients? JMIR Research Protocols, 5(4), e202. https://doi.org/10.2196/resprot.6248
Preacher, K.J., & Hayes, A.F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, and Computers, 36, 717–731.
Rose, S., Paul, C., Boyes, A., Kelly, B., & Roach, D. (2017). Stigma-related experiences in non-communicable respiratory diseases: A systematic review. Chronic Respiratory Disease, 14, 199–216. https://doi.org/10.1177/1479972316680847
Schmidt, K., Damm, K., Prenzler, A., Golpon, H., & Welte, T. (2015). Preferences of lung cancer patients for treatment and decision making: A systematic literature review. European Journal of Cancer Care, 25, 580–591. https://doi.org/10.1111/ecc.12425
Sharf, B.F., Stelljes, L.A., & Gordon, H.S. (2005). ‘A little bitty spot and I’m a big man’: Patients’ perspectives on refusing diagnosis or treatment for lung cancer. Psycho-Oncology, 14, 636–646. https://doi.org/10.1002/pon.885
Shen, M.J., Hamann, H.A., Thomas, A.J., & Ostroff, J.S. (2016). Association between patient-provider communication and lung cancer stigma. Supportive Care in Cancer, 24, 2093–2099. https://doi.org/10.1007/s00520-015-3014-0
Stinchcombe, T.E., & Socinski, M.A. (2009). Current treatments for advanced stage non-small cell lung cancer. Proceedings of the American Thoracic Society, 6, 233–241. https://doi.org/10.1513/pats.200809-110LC
Sullivan, D.R., Forsberg, C.W., Ganzini, L., Au, D.H., Gould, M.K., Provenzale, D., & Slatore, C.G. (2016). Longitudinal changes in depression symptoms and survival among patients with lung cancer: A national cohort assessment. Journal of Clinical Oncology, 34, 3984–3991. https://doi.org/10.1200/JCO.2016.66.8459
Tod, A.M., Craven, J., & Allmark, P. (2008). Diagnostic delay in lung cancer: A qualitative study. Journal of Advanced Nursing, 61, 336–343. https://doi.org/10.1111/j.1365-2648.2007.04542.x
Trask, P.C., & Griffith, K.A. (2004). The identification of empirically derived cancer patient subgroups using psychosocial variables. Journal of Psychosomatic Research, 57, 287–295. https://doi.org/10.1016/j.jpsychores.2004.01.005
Wassenaar, T.R., Eickhoff, J.C., Jarzemsky, D.R., Smith, S.S., Larson, M.L., & Schiller, J.H. (2007). Differences in primary care clinicians’ approach to non-small cell lung cancer patients compared with breast cancer. Journal of Thoracic Oncology, 2, 722–728. https://doi.org/10.1097/JTO.0b013e3180cc2599
Weeks, J.C., Catalano, P.J., Cronin, A., Finkelman, M.D., Mack, J.W., Keating, N.L., & Schrag, D. (2012). Patients’ expectations about effects of chemotherapy for advanced cancer. New England Journal of Medicine, 367, 1616–1625. https://doi.org/10.1056/NEJMoa1204410
Weiner, B., Perry, R.P., & Magnusson, J. (1988). An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology, 55, 738–748.
Weiss, M.G., Ramakrishna, J., & Somma, D. (2006). Health-related stigma: Rethinking concepts and interventions. Psychology, Health and Medicine, 11, 277–287. https://doi.org/10.1080/13548500600595053
Wrosch, C., & Scheier, M.F. (2003). Personality and quality of life: The importance of optimism and goal adjustment. Quality of Life Research, 12(Suppl. 1), 59–72.




