The Relationship Between Health Literacy and Illness Self-Care Management in Turkish Patients With Cancer
Objectives: To determine the relationship between health literacy and illness self-care management in individuals with cancer.
Sample & Setting: 207 individuals with cancer undergoing treatment in the chemotherapy unit of a university hospital in Istanbul, Turkey.
Methods & Variables: Data were collected using a sociodemographic and illness characteristics questionnaire, the European Health Literacy Survey Questionnaire–Turkish Version (HLS-EU-Q-TR), and the Self-Care Management Process in Chronic Illness. Data were analyzed using descriptive statistics, one-way analysis of variance, student t test, Pearson correlation test, and multiple regression analysis.
Results: 86% of individuals displayed an inadequate or problematic to limited level of health literacy. Extended family status and HLS-EU-Q-TR score were significant predictors of self-care management.
Implications for Nursing: Nurses can organize health programs designed to improve the level of health literacy in the population, but they should take into consideration the health literacy levels of their patients.
Jump to a section
Cancer is a public health issue worldwide, and it is the second leading cause of death in the United States and in Turkey (Siegel et al., 2019; Turkey Ministry of Health, 2017). The International Agency for Research on Cancer (2018) reported that 18.1 million individuals worldwide were diagnosed with cancer in 2018 and that 9.6 million cancer deaths occurred that year; in addition, as of 2018, 43.8 million individuals were alive within five years of a cancer diagnosis. The incidence of cancer is rapidly increasing in Turkey, which is creating a significant socioeconomic burden on society, wreaking material and moral havoc, and causing losses and challenges for individuals (Turkey Ministry of Health, 2017).
Because of medical advances and developments in the field of health care, some cases of cancer can now be treated, whereas others can enter a prolonged period of survival where cancer becomes a chronic ailment (Ovayolu & Ovayolu, 2013). However, after diagnosis and while undergoing treatment, individuals with cancer experience various symptoms related to the illness itself and its treatment. Cancer symptoms affect an individual’s general condition, creating stress and deterioration in quality of life (Nichol et al., 2016; Rha et al., 2019). When symptoms are not managed, interruptions in treatment can result (Ovayolu & Ovayolu, 2013). With effective and sustainable illness management, it is possible to diminish illness symptoms, reduce emergency department visits and hospital admissions, limit the physiological and psychological effects of the illness, prevent dependency, and improve quality of life (İncirkuş & Nahcivan, 2015; Zuhur & Özpancar, 2017). Health literacy is reported as an important factor in carrying out effective management of chronic illness (Papadakos et al., 2018; Poureslami et al., 2017; van der Heide et al., 2018).
Background
Cancer treatment can lead to negative physical, emotional, social, and economic outcomes for patients and their families (Ozkaraman et al., 2019). The management of chronic diseases involves not only the steps leading to treatment of the illness but also the planning and implementation of various training and education programs to help the individual acquire the needed skills of self-management (Hançerlioğlu & Aykar, 2018; Zuhur & Özpancar, 2017). Self-management refers to behaviors by which the patient, in cooperation with the healthcare team, manages symptoms following diagnosis and treatment, as well as copes with the side effects of the illness and its treatment, including physical changes; psychosocial results (such as illness-associated sadness, anger, helplessness, crying, hopelessness, and anxiety); and lifestyle adjustments (Papadakos et al., 2018). Self-care behaviors required in the management of chronic illness include maintaining and continuing the treatment, sticking to the recommended diet, and being able to adapt to the lifestyle changes the illness forces the individual to make (Hançerlioğlu & Aykar, 2018).
Patient education is a critical part of comprehensive oncologic care (Luckenbaugh & Moses, 2019). Individuals with cancer are often presented with a great deal of information about the complex cancer treatment process, which is offered to them by numerous healthcare professionals (Lim et al., 2019). Individuals should have a basic level of knowledge about health and healthcare services so that they can make informed decisions about their health (Ozkaraman et al., 2019). The knowledge and competence that individuals apply to complex matters of health is known as health literacy (Sørensen et al., 2012). The World Health Organization (n.d.) describes health literacy as the skills required for individuals to access knowledge, as well as to understand and use that knowledge to achieve improved health and protective services for themselves, their families, and the community. The importance of health literacy is steadily becoming a priority in public health and healthcare services (Sørensen et al., 2012). Studies conducted in Turkey and elsewhere around the world have indicated that health literacy rates are at insufficient levels (Sørensen et al., 2015; Tanrıöver et al., 2014). According to the Turkey Health Literacy Survey, only one-third of the population displays a sufficient or excellent level of health literacy, and about 65% have a problematic or inadequate level of health literacy (Tanrıöver et al., 2014). In contrast, the European Health Literacy Survey, which was conducted in Austria, Bulgaria, Germany, Greece, Ireland, the Netherlands, Poland, and Spain, found that 47% of the population has limited (insufficient or problematic) health literacy (Sørensen et al., 2015). Health literacy has been reported as an important factor in preventing chronic illnesses as well as in carrying out effective management of a given medical condition (Papadakos et al., 2018; Poureslami et al., 2017; van der Heide et al., 2018). A low level of health literacy may lead to diminished rates of participation in one’s own health care and self-management, worsening of medical conditions, and an increase in emergency department and hospital admittances, which causes healthcare service costs to rise (Luckenbaugh & Moses, 2019; Mackey et al., 2016; Papadakos et al., 2018).
Health literacy is particularly important for individuals with cancer. A limited level of health literacy can be a barrier to an individual’s understanding of the risks and benefits of prescribed cancer treatment (Halverson et al., 2015). In addition, a low level of health literacy leads to insufficient understanding of risks of the illness and treatment during cancer follow-up visits, lowers the likelihood of scheduling periodic doctors’ appointments and making regular visits to the hospital, and causes poor or insufficient participation in screening and cancer prevention programs (Levy & Janke, 2016; Rakhshkhorshid et al., 2018). In addition, hypertension, diabetes, and other chronic diseases are more likely to be observed in individuals with a low level of health literacy (Omachi et al., 2013). It has been reported that health literacy is positively correlated with quality of life of individuals with cancer; in addition, increased health literacy increases functional status and one’s general medical condition and reduces symptoms (Halverson et al., 2015; Ozkaraman et al., 2019). It is important in this context to analyze the relationship between health literacy and illness self-care management in individuals with cancer. No studies were found in the literature that have examined this relationship in individuals with cancer in Turkey. The current study is significant because it represents research that was carried out with a large sample group. The aim of this study was to determine the relationship between health literacy and illness self-care management in individuals with cancer. The study sought answers to the following questions:
• What is the level of health literacy among individuals being treated for cancer in Turkey?
• What is the level of illness self-care management among individuals being treated for cancer?
• Is there a relationship between health literacy and sociodemographic and illness characteristics?
• Is there a relationship between illness self-care management and sociodemographic and illness characteristics?
• Is there a relationship between the level of health literacy of individuals being treated for cancer and illness self-care management?
• What are the predictors of illness self-care management among individuals being treated for cancer?
Methods
Sample and Setting
This correlational and cross-sectional study was conducted from February 11 to March 14, 2019, and involved individuals with cancer being treated in the chemotherapy unit of Bezmialem Vakif University, a foundation university in Istanbul, Turkey. An average of 35 patients are treated in this chemotherapy unit each day, and they receive the next cycle of chemotherapy two weeks later. Of the 350 patients who had come to the unit for chemotherapy, 93 did not consent to participating in the research. In addition, the following patients were excluded from study participation: 25 individuals who did not want to complete the questionnaires, 20 individuals with reduced cognitive and perceptive capacities because of aging, and 5 individuals with reduced cognitive and perceptive capacities because of brain metastasis. The study was ultimately conducted with 207 patients with cancer who matched the following inclusion criteria:
• Being a patient with cancer
• Being treated at the study hospital for cancer
• Having no cognitive or mental conditions that would prevent comprehension of the questions asked
• Consenting to participate in the study
Individuals who did not meet these criteria and did not complete the questionnaire were excluded. The university’s ethics committee granted its approval for the study; approval was also obtained from the university hospital. The purpose of the study was explained to patients, and written and verbal consent was obtained. Data were collected by the second and fourth researchers (S.G. and S.M., respectively), who were completing their clinical practice internships in the chemotherapy unit as part of the BSN requirements.
Instruments
Participants completed three questionnaires: (a) a sociodemographic and illness characteristics questionnaire, (b) the European Health Literacy Survey Questionnaire–Turkish Version (HLS-EU-Q-TR), and (c) the Self-Care Management Process in Chronic Illness (SCMP-G). Questionnaires were completed by participants who were currently undergoing chemotherapy treatment via one-on-one interviews conducted by two of the current authors (S.G. and S.M.); each interview lasted about 25 to 30 minutes.
The sociodemographic and illness characteristics questionnaire was developed by the current authors and consisted of 14 items concerning the individual’s age, gender, education, marital status, employment, economic status, family type, place where the individual lived the longest, family history of cancer, type of cancer, time since diagnosis, treatments, relapses, and chronic diseases. In regard to family type, the nuclear family consists of mothers, fathers, and unmarried children, whereas the extended family consists of mothers, fathers, unmarried children, married children, spouses, and grandchildren (Republic of Turkey Ministry of Family and Social Policies, 2011).
Health literacy was measured in the current study by the HLS-EU-Q-TR. The HLS-EU-Q was developed by the European Health Literacy Project Consortium to assess the health literacy of literate individuals aged 15 years or older (Cronbach alpha = 0.97) (HLS-EU Consortium, 2014). The HLS-EU-Q-TR was tested for validity and reliability by Abacıgil et al. (2019) (Cronbach alpha = 0.95). Each item is rated on a scale ranging from 1 (very hard) to 4 (very easy). The code 5 was used for the response “I do not know.” Total possible scores range from 47 to 188. For ease of computation, the total score was standardized using the following formula to produce a range of 0–50, with 0 indicating a low level of health literacy and 50 indicating the highest level of health literacy: formula = index = (arithmetic mean – 1) x [50/3]. In addition, 0–25 represents inadequate health literacy, > 25–33 problematic to limited health literacy, > 33–42 sufficient health literacy, and > 42–50 excellent health literacy. In the current study, the Cronbach alpha for the HLS-EU-Q-TR was 0.93.
The self-care management process in illness was measured in the current study by the SCMP-G, which has a self-protection subscale that looks at the individual’s participation in his or her own health (20 items) and a social protection subscale that looks at the contribution and support of the social environment to the health of the individual (15 items), and was developed by Jones et al. (1986) (Cronbach alpha of 0.78 for the self-protection subscale, 0.78 for the social protection subscale, and 0.75 overall). Hançerlioğlu and Aykar (2018) examined the SCMP-G’s validity and reliability in a Turkish population (Cronbach alpha of 0.83 for the self-protection subscale, 0.68 for the social protection subscale, and 0.85 overall). Both subscales use a five-point Likert-type test ranging from 5 (strongly agree) to 1 (strongly disagree). Items 3, 15, 19, and 28 are reverse-scored. Higher scores indicate increased illness self-management. In the current study, the Cronbach alpha for the self-protection subscale was found to be 0.75, 0.68 for the social protection subscale, and 0.79 overall.
Data Analysis
Data analysis was performed with IBM SPSS Statistics, version 22.0. Statistical analyses corresponded with the research aims and questions. Descriptive statistics, such as means, standard deviations, frequencies, and percentages, were used in the analysis. The normal distribution suitability of the variables was assessed with the Kolmogorov–Smirnov test, which found that the data correspond to normal distribution (p > 0.05). One-way analysis of variance and student t tests were used in the analysis of normally distributed data. Relationships between the HLS-EU-Q-TR and the SCMP-G were assessed with the Pearson correlation test. Multiple regression analysis was used to determine factors affecting illness self-care management of the patients. The results were evaluated at a 95% confidence interval, and significance was accepted as p < 0.05.
Results
Sample Characteristics
The mean age of the 207 individuals with cancer who participated in the current study was 55 years (SD = 12.34, range = 18–83 years), and more than half (n = 106, 51%) were female. The average disease duration was 13.57 months (SD = 16.14, range = 1–75 months). More details concerning demographic characteristics of the participants are shown in Table 1. 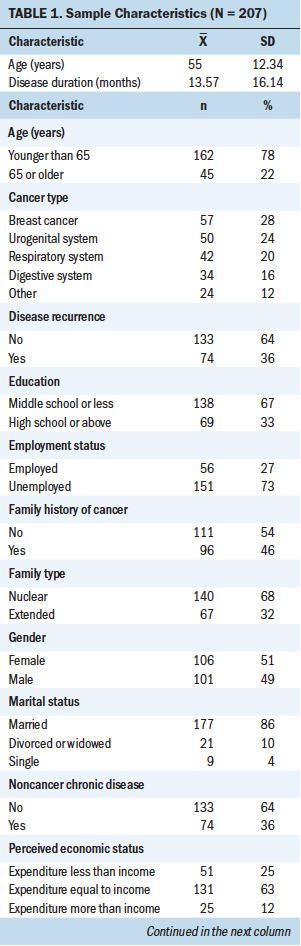
Distribution of Mean HLS-EU-Q-TR and SCMP-G Scores
The mean score on the HLS-EU-Q-TR was 26.31 (SD = 8.32). The self-protection subscale of the SCMP-G had a mean score of 75.23 (SD = 11.1) on a scale of 20–100 (range = 29–95), with higher scores indicating higher self-protection. The social protection subscale of the SCMP-G had a mean score of 46.39 (SD = 9.74) on a scale of 15–75 (range = 19–75), with higher scores indicating higher social protection. The overall mean SCMP-G score was 121.62 (SD = 17.18) on a scale of 35–175 (range 48–157), with higher scores indicating higher illness self-care management. In terms of correlations with the HLS-EU-Q-TR, for the self-protection subscale of the SCMP-G, r = 0.252 (p < 0.001); r = 0.048 for the social protection subscale of the SCMP-G; and r = 0.19 (p < 0.01) for the SCMP-G overall. According to participants’ HLS-EU-Q-TR scores, 38% (n = 79) of the patients had an inadequate level of health literacy, 48% (n = 99) had a problematic to limited level of health literacy, 12% (n = 24) had a sufficient level of health literacy, and 2% (n = 5) had an excellent level of health literacy.
Comparison of Mean HLS-EU-Q-TR and SCMP-G Scores According to Patient Characteristics
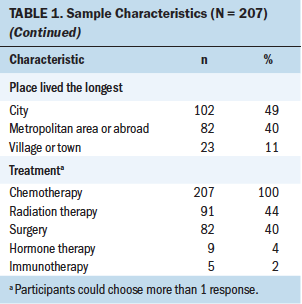
The mean SCMP-G self-protection subscale score of patients at a sufficient to excellent level of health literacy was found to be statistically significantly higher than that of patients at other levels of health literacy (p ≤ 0.001). The mean overall SCMP-G score of patients at an inadequate level of health literacy was significantly lower than that of patients at other levels of health literacy (p < 0.01). No statistical or significant differences were found in the mean SCMP-G social protection subscale scores in terms of patients’ levels of health literacy (p > 0.05) (see Table 2). 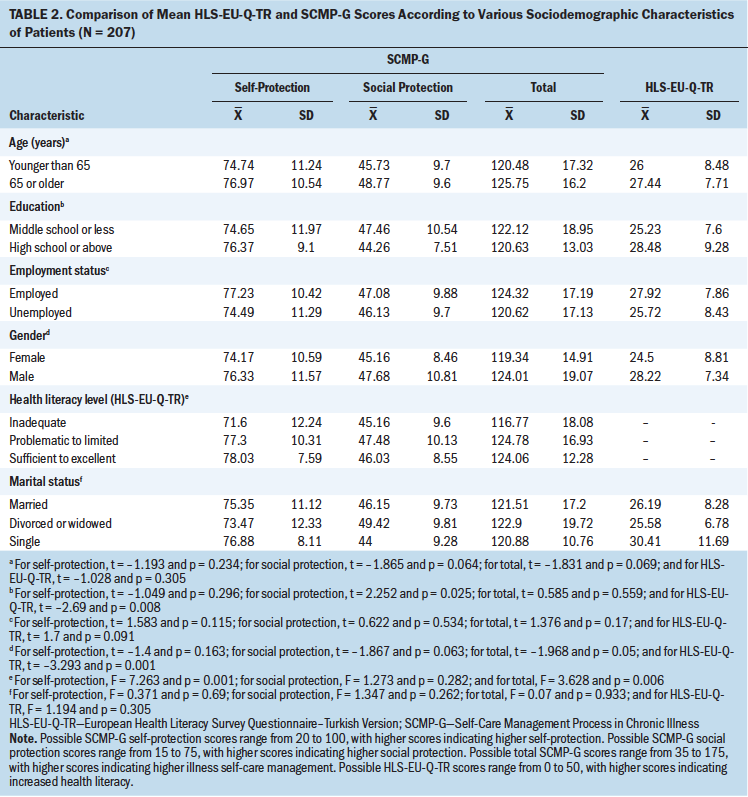
The mean HLS-EU-Q-TR score of the male participants was statistically significantly higher than that of the female participants (p < 0.001). Participants in the study who had received a high school education or above had a significantly higher mean HLS-EU-Q-TR score compared to those with lesser education (p < 0.01).
The mean overall SCMP-G score among the male participants was significantly statistically higher than that of the female participants (p ≤ 0.05). The mean SCMP-G social protection subscale score of those with a middle school education or less was significantly higher than that of those with a high school education or above (p < 0.05). Patients with a high school education or above had an mean overall SCMP-G score that was significantly higher than that of those with a middle school education or less (p < 0.01). The mean SCMP-G social protection subscale score of those living in an extended family and their mean overall SCMP-G score were statistically significantly higher than the same scores of patients who lived in a nuclear family (p < 0.01). The mean SCMP-G self-protection subscale score of patients who had not experienced a relapse and their mean overall SCMP-G score were statistically significantly higher than the same scores of patients who had experienced a relapse (p < 0.05) (see Table 3). 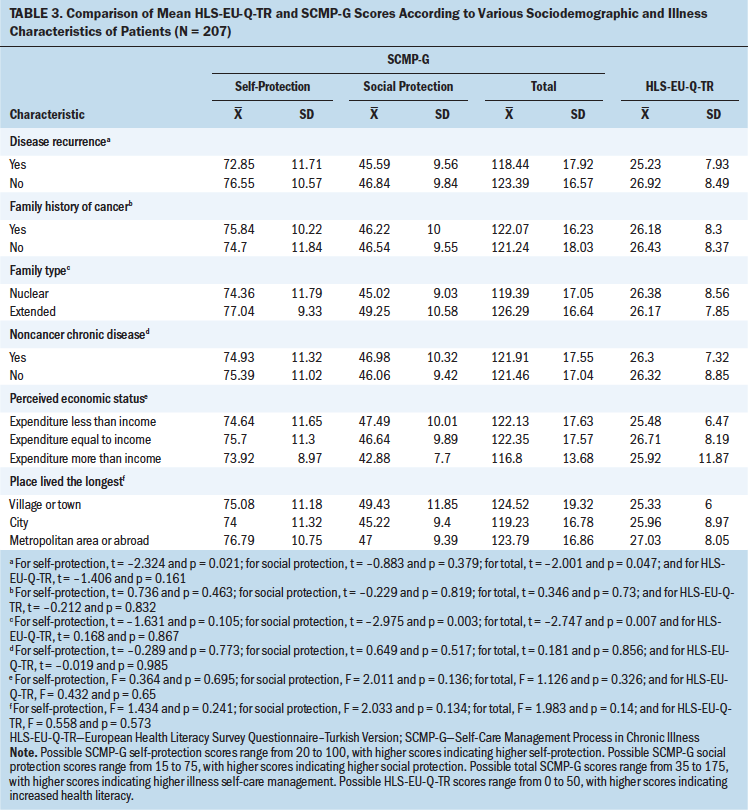
Relationship Between HLS-EU-Q-TR and SCMP-G
A weak positive relationship was found between the SCMP-G self-protection subscale and the HLS-EU-Q-TR (p < 0.001). A very weak positive relationship was found between the overall SCMP-G score and the HLS-EU-Q-TR (p < 0.01). No relationship was found between the SCMP-G social protection subscale and the HLS-EU-Q-TR (p > 0.05).
Determinants of Illness Self-Care Management in Individuals With Cancer
A significant relationship was observed between patients’ illness self-care management and their family structure (b = 0.178, p < 0.05) and the HLS-EU-Q-TR (b = –0.158, p < 0.05). These variables explained 11.8% of total variance (R² = 0.118, p < 0.001). It was determined that extended family status and HLS-EU-Q-TR score were significant predictors of illness self-care management (see Table 4). 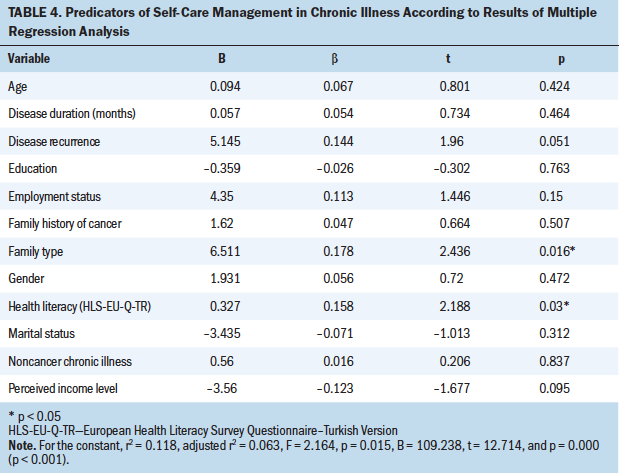
Discussion
Mean Scores for HLS-EU-Q-TR
The mean HLS-EU-Q-TR score of individuals with cancer was 26.31 (SD = 8.32); the health literacy levels of individuals with cancer were at a problematic to limited level. Overall, about 86% of participants in the current study had an inadequate level of health literacy. According to the Turkey Health Literacy Survey, about 65% of the population has a level of health literacy that is problematic or inadequate (Tanrıöver et al., 2014). Findings from the current study reveal that the health literacy of individuals with cancer may be lower than the health literacy of the general population. Because of this, it is important for effective illness management that oncology nurses take into consideration the health literacy levels of patients when organizing training programs about illness self-care management. Contrary to the results of the current study, Ozkaraman et al. (2019) found that individuals with cancer had a sufficient level of health literacy.
Various mean health literacy scores (measured using the HLS-EU-Q) have been reported worldwide: 32.3 (SD = 6.2) in Italy, 35.05 (SD = 6.32) in Finland, 31.4 (SD = 5.8) in Indonesia, 31.6 (SD = 9.3) in Kazakhstan, 32.9 (SD = 7.2) in Malaysia, 31.3 (SD = 8.7) in Myanmar, 34.4 (SD = 6.6) in Taiwan, and 29.6 (SD = 9.1) in Vietnam (Duong et al., 2017; Eronen et al., 2019; Lorini et al., 2019). Although results from the current study are close to the mean health literacy scores in some Asian countries, they are lower than in the other countries. To improve the health of the population and prevent chronic illnesses, interventions to increase health literacy must be made a major priority.
Relationship Between HLS-EU-Q-TR and SCMP-G
As the level of health literacy rose among the patients with cancer in the current study, their self-protection and self-care management improved. Regression analysis demonstrated that the health literacy of individuals with cancer was a significant predictor of illness self-care management. Individuals with a high level of health literacy have a higher level of chronic illness self-care management. Individuals with cancer with an inadequate level of health literacy exhibit lower levels of illness self-care management compared to individuals at other levels of health literacy. Patients with a sufficient to excellent level of health literacy were better at self-protection compared to patients at other levels of health literacy. Similar to results of the current study, Papadakos et al. (2018) reported that health literacy was related to self-care behavior demonstrated by individuals with cancer. It has been reported that when individuals with chronic illnesses have low levels of health literacy, they have difficulty understanding health-related information, practicing self-care, and complying with medical advice and instructions; in addition, they generally have trouble with treatment, which leads to increased costs and increased mortality (Poureslami et al., 2017; Türkoğlu, 2016; Yılmazel & Çetinkaya, 2016).
Mean HLS-EU-Q-TR Scores According to Patient Characteristics
No differences were found in health literacy levels of individuals with cancer in regard to age. However, the Turkey Health Literacy Survey and the European Health Literacy Survey reported that age was a strong predictor of health literacy and that health literacy tended to decline with age (Sørensen et al., 2015; Tanrıöver et al., 2014). This indicates that there is a need for more studies with larger samples to determine the effect of age on health literacy levels among individuals with chronic illnesses.
In the current study, men’s health literacy levels were higher than women’s. Other studies have revealed similar results, asserting that men may have higher levels of health literacy than women (Almaleh et al., 2017; Duong et al., 2017; Lim et al., 2019). However, other research has found the opposite: that women have higher levels of health literacy than men (Güven et al., 2018; Halverson et al., 2015; Malatyali & Biçer, 2018). The Turkey Health Literacy Survey reported that men’s level of health literacy was higher than women’s (Tanrıöver et al., 2014). In the European Health Literacy Survey, it was noted that in all European countries surveyed aside from Bulgaria, Greece, and Spain, age was a significant predictor of health literacy and women had higher levels of health literacy than men (Sørensen et al., 2015). The inadequacy of women’s health literacy levels in Turkey may be explained by women’s lower social status there compared to men.
Individuals with a high school education or above had higher levels of health literacy compared to those who had a middle school education or less. The European Health Literacy Project Consortium reported in its definition of health literacy that health literacy is associated with general literacy (Sørensen et al., 2015). Studies have indicated that graduates of high school or above have higher levels of health literacy (Bayık Temel & Çimen, 2017; Halverson et al., 2015). According to the Turkey Health Literacy Survey, as the level of education increases, the level of health literacy increases as well (Tanrıöver et al., 2014). The European Health Literacy Survey points to education as a significant predictor of health literacy (Sørensen et al., 2015). A low level of education is a risk factor for health literacy, according to the current study and other research.
Mean SCMP-G Scores
According to the SCMP-G scores of individuals with cancer in the current study, self-care levels were moderate; however, this was insufficient for effective illness management. Other studies involving individuals with chronic illnesses reflect similar findings related to illness self-care management (Doğan et al., 2018; Hançerlioğlu & Aykar, 2018; Jones, 2003). With the rise of chronic illnesses around the world and in Turkey, illness management has become a greater priority (Durna & Oğuz, 2018). Chou et al. (2016) reported that among the frequently encountered barriers to self-care among individuals with cancer are limited understanding of treatment, drugs, and side effects; language barriers that prevent communication and hinder decision making; and uncertainty about what questions to ask and what to expect from cancer treatment. Management of chronic illness involves not only treating the condition but also learning skills for self-efficacy through various training and education programs (Doğan et al., 2019). Healthcare professionals, and nurses in particular, play an important role in this because they are in frequent close contact with their patients.
Mean SCMP-G Scores According to Patient Characteristics
Male participants in the current study had a higher level of chronic illness self-care management than the female participants. Altıparmak et al. (2011) reported that there was no difference between men and women in terms of their self-care ability. Chriss et al. (2004) determined that gender was a significant predictor of self-care and that men’s self-care behavior was better than women’s. In Turkish society, where women are generally care providers, men may be in a position to receive more care. In addition, when a woman in Turkey is diagnosed with cancer, the illness is added to the roles she assumes; women in Turkey are often responsible for the health and care of the family (Kaya, 2011).
In the current study, patients who had a high school education or above were better able to exhibit illness self-care management, compared to those with a middle school education or less. Other studies have shown that as the level of education increases, the ability to perform self-care improves (Altıparmak et al., 2011; Callaghan, 2005; Karapehlivan, 2003). The current study also found that social protection was higher in patients with a middle school education or less than in patients with a high school education or above; individuals with less education may have more social support than others. This finding may be explained by the higher participation of individuals with less education in the health of their social environment. More research is needed to determine the impact of education on social protection in illness self-care management.
The current study found that individuals living in an extended family had higher levels of social protection and illness self-care management than those living in nuclear families. The regression analysis showed that family type was a significant predictor of illness self-care management among individuals with cancer and that individuals in an extended family were better at illness self-care management. Studies have found that social support systems (family, friends, and relatives) have a markedly significant impact on self-care ability (Karakurt et al., 2013; Riegel et al., 2011). Altıparmak et al. (2011) reported that although the self-care scores of individuals with cancer living in an extended family were high, this was not statistically significant.
In Turkey, family members play important roles in the care of patients (Bekdemir & İlhan, 2019). In extended families, where many family members live together, there is greater collaboration and solidarity among these family members; consequently, family members may be helpful in caring for individuals with chronic illness. In Turkey, industrialization has led to changes in family structure, primarily a shift from the extended family to the nuclear family (Bayer, 2013; Ünal, 2013). This shift has resulted in a decrease in the number of individuals in a family and changes to the functions of family members. Relations within the family are relatively weak, and solidarity and social support are reduced (Bayer, 2013; Ünal, 2013). Individuals with chronic illness living in an extended family may have better illness management than individuals living in a nuclear family because they are helped by the extended family members.
In Turkey, 70% of families are nuclear families, and 12% are extended families (Republic of Turkey Ministry of Family and Social Policies, 2011). Nurses caring for individuals with cancer should evaluate family types and the social support systems of families. Nurses can play a role in facilitating patients’ access to social support services, particularly by providing guidance and counseling to patients in nuclear families and who have insufficient social support. Facilitating access to social support systems will contribute to effective illness management in individuals with cancer.
In the current study, self-protection and self-care management was higher among individuals who had not experienced a relapse, compared to those who did have a recurrence. This suggests that a relapse may have caused patients to be forced to relive their former difficulties, leading to a lengthened period of treatment and perhaps to a worsened condition; these factors naturally reduce self-care management abilities.
Limitations
Because the research was carried out in a chemotherapy unit and is cross-sectional, the research cannot be generalized. However, a sufficient number of individuals with cancer were included, which was a strength of the study. The study was dependent on the self-evaluations of patients, and no attempt was made to improve the health literacy or illness self-care management of the participants.
Implications for Nursing
Individuals’ health literacy levels should be examined and considered by nurses and other healthcare providers prior to disseminating information related to cancer treatment. Nurses can organize health programs designed to improve the level of health literacy in the population. Such education programs should be made available to the entire population, without discrimination. At the same time, education programs should be organized for the effective management of cancer. It is important that nurses caring for individuals with cancer lead training courses in illness self-care management and consider not only the level of education but also the level of health literacy of patients. The current study showed that family type was a significant predictor of illness self-care management among individuals with cancer. For this reason, nurses should determine the family structures, social support access conditions, and needs of the patients they care for, as well as facilitate patient access to social support services to patients in nuclear families and whose social support is insufficient. 
Conclusion
A majority of the individuals with cancer in the current study were at an inadequate or problematic to limited level of health literacy and their illness self-care management was insufficient. Male participants and those with a high school education or above displayed higher levels of health literacy. Male participants, individuals in extended families, and those who had not experienced a relapse had better illness self-care management abilities. Extended family status and HLS-EU-Q-TR score were significant predictors of chronic illness self-care management.
About the Author(s)
Nesrin İlhan, PhD, RN, is an assistant professor in the Department of Nursing in the Faculty of Health Sciences at Bezmialem Vakif University; Sümeyye Gencer, BSN, is a nurse at Surp Pırgiç Ermeni Hastanesi; Öznur Özdemir, BSN, is a nurse at Bezmialem Vakif University Dragos Hospital; and Seda Maviyildiz, BSN, is a nurse at Bezmialem Vakif University Hospital, all in Istanbul, Turkey. No financial relationships to disclose. All authors contributed to the conceptualization and design, data collection, and manuscript preparation. İlhan provided statistical support and analysis. İlhan can be reached at nilhan@bezmialem.edu.tr, with copy to ONFEditor@ons.org. (Submitted December 2019. Accepted February 2, 2020.)
References
Abacıgil, F., Harlak, H., Okyay, P., Kiraz, D.E., Gursoy Turan, S., Saruhan, G., . . . Beşer, E. (2019). Validity and reliability of the Turkish version of the European Health Literacy Survey Questionnaire. Health Promotion International, 34(4), 658–667. https://doi.org/10.1093/heapro/day020
Almaleh, R., Helmy, Y., Farhat, E., Hasan, H., & Abdelhafez, A. (2017). Assessment of health literacy among outpatient clinics attendees at Ain Shams University Hospitals, Egypt: A cross-sectional study. Public Health, 151, 137–145. https://doi.org/10.1016/j.puhe.2017.06.024
Altıparmak, S., Fadıloğlu, Ç., Gürsoy, Ş.T., & Altıparmak, O. (2011). Kemoterapi tedavisi alan akciğer kanserli hastalarda öz bakım gücü ve yaşam kalitesi ilişkisi [The relationship between quality of life and self-care agency in chemotherapy treated lung cancer patients]. Ege Tıp Dergisi, 50(2), 95–102.
Bayer, A. (2013). Değişen toplumsal yapıda aile [Family in changing social structure]. Şırnak Üniversitesi İlahiyat Fakültesi Dergisi, 4(8), 101–129.
Bayik Temel, A., & Çimen, Z. (2017). Kronik hastaliği olan yaşli bireylerde sağlik okuryazarliği, sağlik algisi ve ilişkili faktörler [Investigation of health literacy, perception of health and related factors in elderly patients with chronic illness]. Ege Üniversitesi Hemşirelik Fakültesi Dergisi, 33(3), 105–125.
Bekdemir, A., & İlhan, N. (2019). Predictors of caregiver burden in caregivers of bedridden patients. Journal of Nursing Research, 27(3), e24. https://doi.org/10.1097/jnr.0000000000000297
Callaghan, D. (2005). Healthy behaviors, self-efficacy, self-care, and basic conditioning factors in older adults. Journal of Community Health Nursing, 22(3), 169–178. https://doi.org/10.1207/s15327655jchn2203_4
Chou, F.-Y., Kuang, L.Y., Lee, J., Yoo, G.J., & Fung, L.-C. (2016). Challenges in cancer self-management of patients with limited English proficiency. Asia-Pacific Journal of Oncology Nursing, 3(3), 259–265. https://doi.org/10.4103/2347-5625.189815
Chriss, P.M., Sheposh, J., Carlson, B., & Riegel, B. (2004). Predictors of successful heart failure self-care maintenance in the first three months after hospitalization. Heart and Lung, 33(6), 345–353. https://doi.org/10.1016/j.hrtlng.2004.03.004
Doğan, M.D., Çadırlı, Ş., Paçaçı, M., & Arslan, Y. (2019). Kronik hastalığı olan bireylerin bakıma ilişkin değerlendirmeleri ve öğrenim gereksinimleri [Care satisfaction and training requirements in patient with chronic disease]. Sağlık ve Hemşirelik Yönetimi Dergisi, 6(1), 22–28. https://doi.org/10.5222/SHYD.2019.39200
Doğan, M.D., Tosun, E., & Tek, A.D. (2018). Kronik hastalıklarda hastalık algısı, yaşam kalitesi, öz-bakım yönetimi [Perception of disease, quality of life, self-care management in chronic illness]. Gümüşhane Üniversitesi Sağlık Bilimleri Dergisi, 7(3), 33–40.
Duong, T.V., Aringazina, A., Baisunova, G., Nurjanah, Pham, T.V., Pham, K.M., . . . Chang, P.W. (2017). Measuring health literacy in Asia: Validation of the HLS-EU-Q47 survey tool in six Asian countries. Journal of Epidemiology, 27(2), 80–86. https://doi.org/10.1016/j.je.2016.09.005
Durna, Z., & Oğuz, G. (2018). Kronik hastalıklar ve yönetimi [Chronic diseases and management of chronic diseases]. In N. Aştı (Ed.), Kronik hastalıklarda bakımın yönetiminde bütüncü yaklaşımla ekip çalışması [Teamwork with holistic approach in the management of care in chronic diseases] (pp. 1–10). Türkiye Klinikleri.
Eronen, J., Paakkari, L., Portegijs, E., Saajanaho, M., & Rantanen, T. (2019). Assessment of health literacy among older Finns. Aging Clinical and Experimental Research, 31, 549–556. https://doi.org/10.1007/s40520-018-1104-9
Güven, D.Y., Bulut, H., & Öztürk, S. (2018). Sağlık bilimleri fakültesi öğrencilerinin sağlık okuryazarlığı düzeylerinin incelenmesi [Examining the health literacy levels of health sciences faculty students]. Tarih Kültür ve Sanat Araştırmaları Dergisi, 7(2), 400–409. https://doi.org/10.7596/taksad.v7i2.1511
Halverson, J.L., Martinez-Donate, A.P., Palta, M., Leal, T., Lubner, S., Walsh, M.C., . . . Trentham-Dietz, A. (2015). Health literacy and health-related quality of life among a population-based sample of cancer patients. Journal of Health Communication: International Perspectives, 20(11), 1320–1329. https://doi.org/10.1080/10810730.2015.1018638
Hançerlioğlu, S., & Aykar, F.Ş. (2018). Kronik hastalıklarda öz bakım yönetimi ölçeği’nin Türkçe’ye uyarlanması, geçerlik ve güvenirliği [Validity and reliability of Turkish version of the self-care management process in chronic illness]. Gümüşhane Üniversitesi Sağlık Bilimleri Dergisi, 7(1), 175–183.
HLS-EU Consortium. (2014). Comparative report of health literacy in eight EU member states. The European Health Literacy Survey HLS-EU (Second revised and extended version). https://cdn1.sph.harvard.edu/wp-content/uploads/sites/135/2015/09/neu_r…
İncirkuş, K., & Nahcivan, N.Ö. (2015). Kronik hastalık yönetimi için bir rehber: Kronik bakım modeli [A guide for chronic disease management: The chronic care model]. Florence Nightingale Hemşirelik Dergisi, 23(1), 66–75.
International Agency for Research on Cancer. (2018). Latest global cancer data: Cancer burden rises to 18.1 million new cases and 9.6 million cancer deaths in 2018 [Press release]. https://www.who.int/cancer/PRGlobocanFinal.pdf
Jones, L.C. (2003). Measuring guarding as a self-care management process in chronic illness: The SCMP-G. In O.L. Strickland & C. Dilorio (Eds.), Measurement of nursing outcomes: Vol. 3. Self care and coping (2nd ed., pp. 150–158). Springer Publishing Company.
Jones, L.C., Hill, K., Honer, K., & McDaniels, S. (1986). Self-care management process used by individuals with chronic illness [Unpublished manuscript].
Karakurt, P., Hacıhasanoğlu, R., & Yıldırım, A. (2013). Diyabetli hastaların öz-bakım gücü ve algıladıkları sosyal desteğin değerlendirilmesi [Evaluation of the self-care agency and perceived social support in patients with diabetes mellitus]. Adnan Menderes Üniversitesi Tıp Fakültesi Dergisi, 14(1),1–9.
Karapehlivan, H.S. (2003). Examining of self-care power and affecting factors in cancer patients [Unpublished master of science dissertation]. Ege University Institute of Health Sciences.
Kaya, Ş.Ş. (2011). Televizyonda kadın, sağlık ve hastalık [Women, health and illness in television]. Journal of Sociological Research, 14(2), 117–150.
Levy, H., & Janke, A. (2016). Health literacy and access to care. Journal of Health Communication, 21(Suppl. 1), 43–50. https://doi.org/10.1080/10810730.2015.1131776
Lim, B.T., Huang, Y.-J., Shepherd, H.L., Shaw, J., Costa, D., Durcinoska, I., . . . Butow, P. (2019). Health literacy and cancer care coordination in Chinese migrant patients and their carers: A cross-sectional survey. Psycho-Oncology, 28(5), 1048–1055. https://doi.org/10.1002/pon.5050
Lorini, C., Lastrucci, V., Mantwill, S., Vettori, V., & Bonaccorsi, G. (2019). Measuring health literacy in Italy: A validation study of the HLS-EU-Q16 and of the HLS-EU-Q6 in Italian language, conducted in Florence and its surroundings. Annali dell’Istituto Superiore di Sanità, 55(1), 10–18. https://doi.org/10.4415/ANN_19_01_04
Luckenbaugh, A.N., & Moses, K.A. (2019). The impact of health literacy on urologic oncology care. Urologic Oncology: Seminars and Original Investigations. Advance online publication. https://doi.org/10.1016/j.urolonc.2019.06.016
Mackey, L.M., Doody, C., Werner, E.L., & Fullen, B. (2016). Self-management skills in chronic disease management: What role does health literacy have? Medical Decision Making, 36(6), 741–759. https://doi.org/10.1177/0272989X16638330
Malatyali, İ., & Biçer, E. (2018). Sağlık okuryazarlık düzeyinin belirlenmesi: Sivas Cumhuriyet Üniversitesi örneği [Determination of health literacy level: The case of Sivas Cumhuriyet University]. Ankara Sağlık Hizmetleri Dergisi, 17(2), 16–27.
Nichol, K., Stacey, D., Kuziemsky, C., & Gifford, W. (2016). Cancer symptom management in the home: A scoping review. Canadian Oncology Nursing Journal, 26(1), 4–10. https://doi.org/10.5737/23688076261411
Omachi, T.A., Sarkar, U., Yelin, E.H., Blanc, P.D., & Katz, P.P. (2013). Lower health literacy is associated with poorer health status and outcomes in chronic obstructive pulmonary disease. Journal of General Internal Medicine, 28, 74–81. https://doi.org/10.1007/s11606-012-2177-3
Ovayolu, Ö., & Ovayolu, N. (2013). Semptom yönetiminde kanit temelli tamamlayici yöntemler [Evidence-based supplementary methods for symptom management]. Erciyes Üniversitesi Sağlık Bilimleri Fakültesi Dergisi, 1(1), 83–98.
Ozkaraman, A, Uzgor, F., Dugum, O., & Peker, S. (2019). The effect of health literacy on self-efficacy and quality of life among Turkish cancer patients. Journal of the Pakistan Medical Association, 69(7), 995–999.
Papadakos, J.K., Hasan, S.M., Barnsley, J., Berta, W., Fazelzad, R., Papadakos, C.J., . . . Howell, D. (2018). Health literacy and cancer self-management behaviors: A scoping review. Cancer, 124(21), 4202–4210. https://doi.org/10.1002/cncr.31733
Poureslami, I., Nimmon, L., Rootman, I., & Fitzgerald, M.J. (2017). Health literacy and chronic disease management: Drawing from expert knowledge to set an agenda. Health Promotion International, 32(4), 743–754. https://doi.org/10.1093/heapro/daw003
Rakhshkhorshid, M., Navaee, M., Nouri, N., & Safarzaii, F. (2018). The association of health literacy with breast cancer knowledge, perception and screening behavior. European Journal of Breast Health, 14(3), 144–147.
Republic of Turkey Ministry of Family and Social Policies. (2011). Türkiye Aile Yapısı Araştırması TAYA 2011 [Turkish Family Structure Survey TAYA 2011]. https://ailevecalisma.gov.tr/uploads/athgm/uploads/pages/indirilebilir-…
Rha, S.Y., Nam, J.M., & Lee, J. (2019). Development and evaluation of the Cancer Symptom Management System: Symptom management improves your LifE (SMILE)—A randomized controlled trial. Supportive Care in Cancer, 28(2), 713–723. https://doi.org/10.1007/s00520-019-04865-3
Riegel, B., Lee, C.S., & Dickson, V.V. (2011). Self care in patients with chronic heart failure. Nature Reviews Cardiology, 8(11), 644–654. https://doi.org/10.1038/nrcardio.2011.95
Siegel, R.L., Miller, K.D., & Jemal, A. (2019). Cancer statistics, 2019. CA: A Cancer Journal for Clinicians, 69(1), 7–34. https://doi.org/10.3322/caac.21551
Sørensen, K., Pelikan, J.M., Röthlin, F., Ganahl, K., Slonska, Z., Doyle, G., . . . Brand, H. (2015). Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). European Journal of Public Health, 25(6), 1053–1058. https://doi.org/10.1093/eurpub/ckv043
Sørensen, K., Van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., & Brand, H. (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12, 80. https://doi.org/10.1186/1471-2458-12-80
Tanriöver, M., Yildirim, H., Ready, F.N.D., Çakir, B., & Akalin, E. (2014). Türkiye Sağlik Okuryazarliği Araştirmasi [Turkey Health Literacy Survey]. Sağlik-Sen Publications.
Turkey Ministry of Health. (2017). Türkiye kanser istatistikleri [Turkey cancer statistics]. https://hsgm.saglik.gov.tr/depo/birimler/kanser-db/istatistik/2014-RAPO…
Türkoğlu, Ç. (2016). Analyzing the relationship between health literacy and self-care ability level: The case of Isparta [Unpublished master of science dissertation]. Süleyman Demirel University.
Ünal, V. (2013). Geleneksel geniş aileden çekirdek aileye geçiş sürecinde boşanma sorunu ve din [The problem of divorce during the transition from extended family to nuclear family and religion]. Journal of International Social Research, 6(26), 588–602.
van der Heide, I., Poureslami, I., Mitic, W., Shum, J., Rootman, I., & FitzGerald, J.M. (2018). Health literacy in chronic disease management: A matter of interaction. Journal of Clinical Epidemiology, 102, 134–138. https://doi.org/10.1016/j.jclinepi.2018.05.010
World Health Organization. (n.d.). The mandate for health literacy. https://www.who.int/healthpromotion/conferences/9gchp/health-literacy/en
Yılmazel, G., & Çetinkaya, F. (2016). Sağlık okuryazarlığının toplum sağlığı açısından önemi [The importance of health literacy for community health]. TAF Preventive Medicine Bulletin, 15(1), 69–74. https://doi.org/10.5455/pmb.1-1448870518
Zuhur, Ş., & Özpancar, N. (2017). Türkiye’de kronik hastalık yönetiminde hemşirelik modellerinin kullanımı: Sistematik derleme [The use of nursing models in the management of chronic diseases in Turkey: A systematic review]. Hemşirelikte Araştirma Geliştirme Dergisi, 19(2), 57–74.


