The Ecology of Patients’ Sexual Health Adjustment After Prostate Cancer Treatment: The Influence of the Social and Healthcare Environment
Purpose: Little empirical research identifies environmental influences on sexual recovery of men with prostate cancer. This secondary qualitative analysis aimed to describe the role of the patients’ environment on their sexual recovery process following prostate cancer surgery.
Participants & Setting: Transcripts of interviews with 8 heterosexual men were randomly selected and analyzed from a sample of 18 at three months postprostatectomy.
Methodologic Approach: The study was based on the social ecological model. Interpretative phenomenological analysis was applied to examine environmental factors affecting sexual recovery through the participant’s perspective.
Findings: The value of trusted connections and support extended beyond the partner to the patient’s social and healthcare networks.
Implications for Nursing: These findings support the need for providers to assess the full constellation of patients’ environmental experiences to better understand sexual recovery.
Jump to a section
Men who undergo radical prostatectomy for prostate cancer frequently experience sexual problems following completion of surgical treatment. These sexuality changes are broadly categorized into physiologic, psychologic, and social dimensions, and all are negatively affected by prostate cancer treatment (Albaugh et al., 2017). Physiologic changes in men with prostate cancer include impotence and orgasmic disorder, which are broadly understood as sexual dysfunction (Wassersug et al., 2017). Psychosocially, survivors navigate emotional and relationship distress, and face stigmatization and social isolation when faced with discussing sexual dysfunction with others, including their partner (Ettridge et al., 2018; Hammond & Montgomery, 2018).
The diversity and prevalence of sexuality issues in men postprostatectomy have led to a growing body of research surrounding the sexual recovery process. Early research focused on the restoration of erectile ability through pro-erectile medications and aids (Matthew et al., 2005). However, although treatments for erectile dysfunction via sexual aids and medications can improve the physical component of sexual loss, these treatments often do not completely improve patients’ sex lives. Long-term use of sexual aids frequently declines because of unaddressed psychosocial barriers (Walker et al., 2014). Long-term quality-of-life, satisfaction, and psychosocial adjustment outcomes in men after prostate cancer are negatively affected by inadequate sexual recovery (Chambers et al., 2017). Some potential preoperative barriers to sexual recovery include developmental sexual losses, underdeveloped sexual coping skills, and stress (Wittmann, Carolan, et al., 2015).
Promotion of sexual recovery requires a similar focus on psychological and social factors pre- and postsurgery (Walker et al., 2015). However, current literature has not focused on social impediments of sexual recovery, which present unique challenges for patients. In addition, prostate cancer survivors with male partners often experience a disproportionate lack of social support, which further affects health outcomes (Capistrant et al., 2016). Given that strong social relationships influence men’s desire to seek primary care for prostate cancer, this could also extend to management of sexuality issues (Forbat et al., 2014).
Literature Review
Previous qualitative research has also found that partners grapple with newfound emotional and relationship changes throughout the process of their partner’s recovery (Tanner et al., 2011). A cross-sectional study of 189 couples found that sexual difficulties in the patient with prostate cancer were associated with increased anxiety in the partner (Chambers et al., 2013). Another cohort study of 119 female and 2 male partners reported that spouses with a negative perception of their caregiving had decreased sexual satisfaction and increased marital distress (Harden et al., 2013). The loss and grief related to a cancer diagnosis and resultant side effects of surgery created stress within the patient–partner dyad (Chambers et al., 2013). In a mixed-methods study, couples demonstrated positive and negative coping with sexual function changes, which involved undertaking a normal grief and mourning process while learning to live with sexual losses and accept sexual aids (Wittmann, Northouse, et al., 2015).
Men often present with a unique subset of emotional responses to sexual losses. Grief and mourning constitute a large component of men’s reactions to their prostate cancer surgery (Wittmann et al., 2011). Processing grief and mourning over the loss of sexuality involves successfully working through subsequent sexual encounters, which creates a sense of competency (Beck et al., 2013). However, effectively addressing these psychosocial components also requires the close involvement of the partner’s perspectives and reactions (Wittmann et al., 2011). Sexual recovery within couples requires addressing fears and concerns about functional loss and subsequent grief, and promotion of coping with the changes in the sexual relationship (Wittmann, Northouse, et al., 2015). There is evidence that embedding the partner comprehensively in the sexual recovery process has improved patient outcomes. A study of 189 patients postprostatectomy found that involving the partner in the recovery process was associated with better use of sexual aids (Chambers et al., 2013). In addition, a study of 17 couples reported that maintaining acceptance, flexibility, and tenacity when faced with the challenges of recovery helped couples the most with adjustment (Beck et al., 2013).
Conceptual Framework
A social ecological model was used for this study to comprehensively embed prostate cancer survivors within a larger social system (McLeroy et al., 1988). The social ecological model broadly considers men within their interpersonal, institutional, and community settings and, as a result, describes an interactive relationship between men and their complete environment (Golden & Earp, 2012). Initiatives have applied social ecological models to improve mental health and quality of life among cancer survivors (Moore et al., 2015). Although populations with cervical and colorectal cancer have been analyzed through the lens of the social ecological model, this approach has not been applied to prostate cancer survivors (Centers for Disease Control and Prevention, 2015; Daley et al., 2011).
Purpose
Although the previously mentioned literature has investigated some of the partner’s role in sexual recovery, research has not been extended to other social or cultural influences. For example, Ezer et al. (2012) measured psychosocial adjustment of men within the first year of prostate cancer but kept the social component only within the couple. Ultimately, there is little research that describes sexual recovery in men with prostate cancer within the context of their familial and work environments in tandem with interactions with their partner and the hospital system. Therefore, the aim of this study was to examine how the patient’s environment affects sexual recovery following prostate cancer surgery.
Methodologic Approach
Philosophical Perspective
The study applied a phenomenologic approach, as presented by the French philosopher Maurice Merleau-Ponty. This philosophic perspective characterizes personal experiences as a connection within a subject–object exchange between the human consciousness and the outside world (Merleau-Ponty, 2014). The strength of this approach is the focused perspective on the lived experience of participants’ embodied sexuality within their perception of the environment (Wilde, 1999). Although sexuality is a lived experience, this approach also considers environmental influences. As such, sexuality is an ideal domain of human experience for study with phenomenologic methods because it is subjectively experienced through the body and emotions, and it is also observed and evaluated intellectually.
Participants and Setting
The data were obtained from a previously completed mixed-methods study (Wittmann, Carolan, et al., 2015). In this previous study, 28 participants with prostate cancer who had elected surgical treatment were recruited from a midwestern academic cancer center. These participants and their partners were contacted by the research coordinator via telephone and consented preoperatively. Of the 28 recruited participants, 20 participants and their partners (couples) completed questionnaires and interviews pre- and postoperatively. For this secondary analysis, transcripts from eight couples were randomly selected from this prior sample, and only the patient’s perspective was analyzed. Sample sizes for phenomenologic analysis are typically small, with five or six participants’ experiences being analyzed in-depth (Morse, 1994).
Data Collection
Participants were interviewed in the previously completed study using a semistructured interview guide to encourage discussion about sexual recovery. The broad topics that were discussed were as follows: description of general changes in sexuality, which included penile changes, sexual desire, arousal, and orgasm; ability to have a sexual relationship or feel close as a couple; changes to communication; intimacy and role changes; general physical, psychological, and emotional effects of the surgery; awareness of available counseling and rehabilitation services; barriers to sexual counseling; and presence of external stressors. Participants and partners were first interviewed together, then the participant and partner were interviewed separately. When the participant was interviewed alone, he was asked whether there was anything that he wanted to discuss privately that was not covered in the couple interview. This secondary analysis was deemed exempt from institutional review board oversight, although institutional review board approval had been obtained for the initial data collection.
Analysis
Given that Merleau-Ponty (2014) does not specify a detailed methodology for analysis of phenomenologic data, this study applied the steps for interpretative phenomenological analysis (IPA), as outlined by Smith (1996). IPA was selected because it examines how participants make sense of their experiences and, in this study, how they interpret the effects of their partner and lived environment (Kalfa et al., 2019; Schantz Laursen, 2017). The steps of IPA are as follows:
• Themes were reviewed and coded from one case.
• Remaining cases were coded for abstraction.
• Higher-level constructs were developed, reflective of the shared experiences among the participants.
• Common experiences and themes were explained, illustrated, and nuanced.
Coding of the transcripts and creation of themes were conducted using ATLAS.ti, version 8.0. The final code and theme lists were reviewed between a clinical expert (D.W.) and a qualitative research expert (D.S.A.). Contradictory and inconsistent themes were reviewed and revised after discussion with the qualitative data expert. Final data interpretation was decided on review and consensus among study team members.
Rigor was maintained through a strict audit trail, which was updated throughout the code generation and organization process. Themes were only added into the final table if they were present in the responses of at least three participants. A reflexivity journal was also maintained to identify personal biases and reactions to the data during the coding process (Chan et al., 2013).
Findings
Participant Characteristics
The average age of the sample was 59 years (SD = 6.12, range = 52–68). The sample was well educated and married, with a mean marriage length of 37 years (SD = 6.8, range = 25–42). Most men had moderately aggressive prostate cancer, and all had undergone nerve-sparing surgery. Additional participant demographic and clinical characteristics are provided in Table 1. 
Interview Themes
Themes and subthemes with exemplar quotes are presented in Figures 1, 2, and 3. The three major themes of the participants’ lived environment were partner dynamics, experiencing demands, and receiving support and advice. These themes captured how participants experienced the outside world and how the participants’ changing sexuality was perceived. In these themes, the factors outside of the participants’ direct control exerted their own influence on the participants’ recovery. 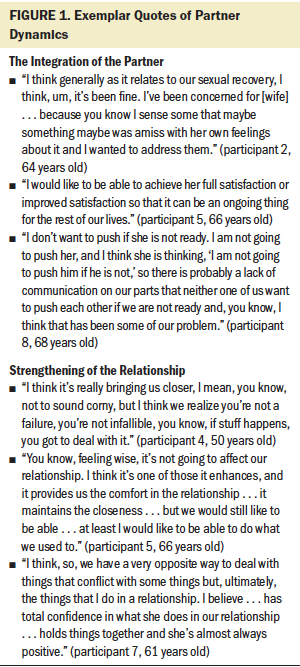
Theme 1: Partner Dynamics
The role of the partner emerged as an inextricable component of recovery for the participants interviewed. All eight participants reported that their partner changed their outlook and approach to managing sexual recovery issues. This theme was separated into the following two subthemes: the integration of the partner and the overall strengthening of the relationship. 
The integration of the partner: Participants wanted to improve their sexuality and changing body with their partner’s full support, and they wished to keep their partner’s sexual needs in mind during the entire process. One participant wanted to ensure that his wife could have satisfactory orgasms (participant 5). For another participant, addressing his wife’s concerns was equally important for his own sexual recovery (participant 2). Two participants appreciated the power of communication and compromise. In particular, one participant wanted to remain cognizant of his wife’s divergent work schedule so they could plan time for sexual activity (participant 8). Another participant elaborated that the surgery created additional preparation for sexual activity, and this was important to communicate to his partner at the outset. Participants also discussed what they expected from their partners. One participant needed his wife to take a more active role in their sex life (participant 6). Another participant desired more openness and affection from his partner, elaborating that guarded emotions from his wife reduced the desire to implement sexual aids, like vacuum devices (participant 8). This participant further detailed that the daunting task of working on sexuality made him and his partner hesitant to pressure each other. Overall, these relationship dynamics highlighted the importance of involvement, communication, and consensus during navigation of recovery issues. 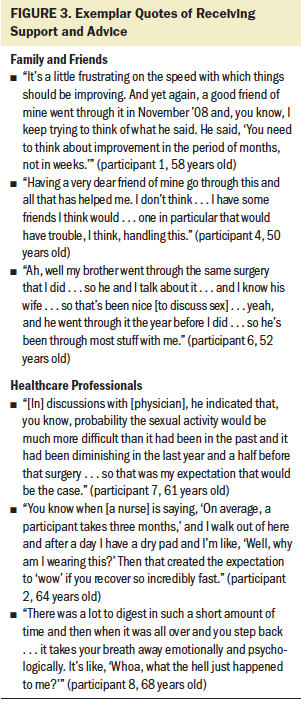
Strengthening of the relationship: Three participants reported that the journey of recovery had strengthened their relationship and brought them closer as a couple. Participants saw themselves and their wives as a team “in this together,” and this presented in different ways across the transcripts. One participant described how the process of recovery had brought them closer (participant 4). This participant also expressed that “they didn’t have to recover from anything” because his partner did not view him any differently. Another participant was confident that the journey to improve their sex life would not negatively affect his relationship (participant 5). Participants appreciated the instrumental role their partner played in the recovery process. One expressed how confident and positive his wife was, and how she would “tie things together” (participant 7). For this participant, his wife provided strength and inspiration with her positive attitude even when faced with struggles and failures during recovery. Several participants also disclosed that they did not feel diminished in their masculinity because of the strong relationship they had with their partner.
Theme 2: Experiencing Demands
The second overarching theme encompassed the responsibilities outside of the participant–partner dyad and included the participant’s work and family roles. All eight participants reported that their commitments to their extended family, children, and siblings would reduce time for sexual recovery. In addition, the exhaustion and stress from these outside responsibilities made participants feel mentally and physically exhausted, which also impaired the ability to perform sexual activities or engage intimately with their partner.
Family responsibilities: Participants described several familial causes of stress, including children, teenagers, and extended family. One participant shared that he only had 10–15 minutes a day at a maximum to work with a penis pump in the shower and that the rest of the day was taken up by children and other responsibilities (participant 7). Another participant had older adult family members to care for and disclosed that those responsibilities increased stress and exhaustion (participant 2). Two participants had children present in the home, which made it harder to engage in sexual activity because of privacy concerns (participant 8). One participant mentioned a daughter who required constant attention because of pertinent medical and mental health needs (participant 2). Another described the process of trying to find assistance to take care of his daughter’s needs so he and his wife could spend quality time alone (participant 8).
Work responsibilities: Participants reported that work made finding physical and mental space for sexual activities challenging. One participant elaborated that he was assuming more roles at work and that this exhausted him and drained his desire for sexual activity (participant 2). Another participant was considering a part-time job in the afternoon and on weekends and worried that too much distraction could take away from time to work on sexual recovery (participant 8). A third participant discussed how working nonstop as a dentist made penile rehabilitation more difficult because of a lack of energy (participant 1). This patient further expressed that it was difficult to prioritize competing obligations. Conversely, some participants who were not working had more time to work on sexual recovery. One participant noted that he and his partner had more free time for intimacy because they were retired (participant 4). Across the transcripts, social and employment responsibilities ultimately created competition in participants’ busy schedules, and sexual recovery was often left behind.
Theme 3: Receiving Support and Advice
The third theme that emerged from the interviews detailed the supportive role that family members and healthcare professionals played in the recovery process. This contrasted with the demands exhibited by family members in previous themes. Family and friends provided support while also exacting demands on the participants’ time. In addition, participants mentioned the support systems that were in place in the hospital setting, particularly in the preoperative phase.
Family and friends: Participants elaborated that family members were helpful in navigating difficulties and disappointments. Two participants developed the expectations of how their body should change or behave compared to other men in their social circles. Their perception of recovery was also based on their family members’ experience of regaining erectile function and confidence with sexual activity (participants 4 and 8). One participant described how hearing advice from his friend led him to compare his progress to others’, which inspired him with his own progress on his recovery (participant 1). Another participant shared this when talking to his brother who had gone through a prostatectomy, elaborating that “I am farther along now than he ever was at this point after his surgery” (participant 4). Other participants shared that friends would provide more general advice, although there was some variation on this theme. In addition, one participant shared that his male friends would abstain from discussion of sexual issues. The sensitive nature of sexual health made it difficult for some to connect with others on their struggles.
Healthcare professionals: In addition to family and friends, five participants felt that the support from the hospital was instrumental in promoting their recovery (participants 1, 2, 3, 4, and 7). One participant’s physician told him that sexual activity would be more difficult than in the past and, as such, he expected that going forward (participant 1). Another participant recalled the conversations he had with his physician after the surgery when he had difficulties with using sexual devices (participant 7). Several participants described the instrumental role played by their nurse during the recovery process. One patient recalled the conversation he had with his nurse regarding how long it would be before he would have an erection suitable for intercourse (participant 3). A second participant experienced a similar interaction with his nurse who told him how long it may take to recover an erection (participant 2). A third participant mentioned the valuable instruction he received from his nurse in regard to using a vacuum pump (participant 4).
There were also some institutional effects noted in the transcripts. One participant stated that his hospital education sessions prepared him for “everything that was going to happen” (participant 6). In contrast, two participants disclosed that they had received so much information that it was difficult to digest and process it. These two participants also added that although they received adequate information preoperatively, it did not feel personalized to their individual situation (participants 4 and 8). One of these participants elaborated that the lack of personal information left him unprepared when faced with the sexual side effects of the surgery (participant 4). Across the transcripts, participants valued the role that support systems played in celebrating the successes and managing the failures in recovery.
Discussion
This study illuminates the complex relationship between environmental influences on sexual recovery in men with prostate cancer. The findings from this study tie together a network of intrapersonal and community-level factors and provide some insight into institutional factors surrounding receipt of sexual recovery information. This research builds on a previous qualitative study that applied a phenomenologic approach to sexuality following prostate cancer surgery (Schantz Laursen, 2017). This previous study found that lack of control and function, sense of self, intimate relations, and redefining sexuality were the main themes experienced by participants. However, the study did not explore outside environmental factors. As such, this work builds on previous sexual recovery models by contributing the effects of environmental experiences, recognizing the ecological framework that places survivors within a larger social and support context.
Men in this sample often compared themselves to other men who had experienced similar surgery-related changes to sexual function. Sexual recovery was less focused on improvement of physical characteristics, such as penis size, and more on the speed and time to return to sexual activity. This was a unique finding that, to the authors’ understanding, has not been previously identified. Comparison with others in this fashion may constitute an important environmental factor that influences how men cope with loss and subsequent recovery. Part of this coping may involve a redefinition of masculinity and sexuality, which has been discussed in previously conducted cancer literature (Reese et al., 2010). Coping as a product of social support has been interconnected in previous quality-of-life literature, particularly in the dyadic context, but has not been previously studied in other social contexts (Lim et al., 2014).
An institutional-level finding was the substantial amount of information received before discharge from the hospital setting, which left participants feeling overwhelmed when facing their own recovery issues. These findings are, in part, supported by previous qualitative research in men that found that patients desire a more person-centered approach to supportive care and education (Paterson et al., 2017). The importance of individualized sexual health–focused information and guidance was a finding in these transcripts and is also supported by a previous cross-sectional study in which 75% of men desired discussion with a provider specifically trained in sexual health issues (Grondhuis Palacios et al., 2018). However, additional research is needed to improve mechanisms for improving delivery of education regarding sexual health issues in this population.
The protective nature of the patients’ partners in this study corroborates previous work with couples postprostatectomy, in which men felt they had sufficient emotional support from their partner in managing prostate cancer (O’Shaughnessy et al., 2013). Although the influence of the partner was a key finding from this study, comments from partners were not included in this analysis to exclusively capture the experiences of the participants in congruence with interpretive phenomenology. However, previous studies have found that cancer is distressing for patients and their partners, who are both faced with challenges in navigating diminished sexuality (Wittman, Northouse, et al., 2015) and cancer overall (Lim et al., 2014). As such, future research could aim to understand the role of the environment on influencing partners’ perceptions of their loved one’s recovery from prostate cancer.
Limitations
The results of the current study should be considered within the context of some limitations. The sample was predominantly Caucasian, which limits the study’s applicability to men of other races and cultures that differ in expression of sexuality. The average age of the sample was 59 years, which is younger than the current mean age of diagnosis for prostate cancer, which is age 66 years (Rawla, 2019). The younger age is typical of men who come to this midwestern tertiary cancer center for treatment and, therefore, is not fully representative of the average cohort of men with prostate cancer. All participants were interviewed in two stages: first with the partner present, and afterward with the partner absent. It is uncertain whether having a partner present during interviews influences how the participant engages and answers questions, particularly regarding sensitive information such as sexuality (Norlyk et al., 2016). However, none of the participants included in this study changed their narrative when they were interviewed alone as compared to with their partner. The sample was also made up entirely of heterosexual couples, so the results of this study should not be applied to single men or gay men. Lastly, there were some components of the ecological framework that this study was unable to address because of limitations of the data. These were largely institutional-level factors, such as insurance status or access to a male sexual health clinic.
Implications for Nursing
The ability to provide compassionate and accurate sexual health counseling for patients postprostatectomy is a crucial part of postsurgical care, and nurses often play a vital role in this trajectory. Across several transcripts, nurses were described as an important environmental factor that molded the participants’ perceptions of normal recovery. Based on the themes from these interviews, fully assessing the complete context in which a patient attempts to undergo sexual recovery may provide a helpful addition to the usual functional assessment and, as a result, may help patients achieve optimal outcomes (Walker et al., 2014). Nurses can assist couples in advance of prostate cancer treatment by providing information and support within the context of the couple, promoting persistence throughout the recovery process, and facilitating communication within the couple toward their shared goals of sexuality (Beck et al., 2013; Walker et al., 2014). 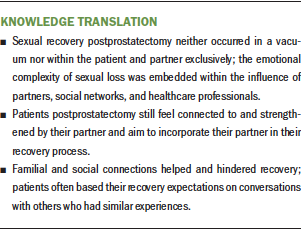
Conclusion
This study explored sexual recovery experiences of patients who undergo prostate cancer surgery. Most of the sexual recovery process occurred through the patient–partner dyad, but sexual recovery was positively and negatively affected by social and healthcare networks. These findings describe the interaction between men with a complex network of environmental influences within an ecological framework, including interpersonal and community factors. Assessment of the expanded constellation of these experiences will be key in understanding the individual patient’s recovery pathway.
About the Author(s)
Asa Benjamin Smith, BSN, RN, is a PhD candidate in the School of Nursing, Daniela Wittmann, PhD, LMSW, is an associate professor in the Department of Urology, and Denise Saint Arnault, PhD, RN, FAAN, is an associate professor in the School of Nursing, all at the University of Michigan in Ann Arbor. No financial relationships to disclose. All authors contributed to the conceptualization and design, provided analysis, and contributed to the manuscript preparation. Wittmann completed the data collection. Smith can be reached at smiasa@umich.edu, with copy to ONFEditor@ons.org. (Submitted December 2019. Accepted February 20, 2020.)
References
Albaugh, J.A., Sufrin, N., Lapin, B.R., Petkewicz, J., & Tenfelde, S. (2017). Life after prostate cancer treatment: A mixed methods study of the experiences of men with sexual dysfunction and their partners. BMC Urology, 17(1), 45. https://doi.org/10.1186/s12894-017-0231-5
Beck, A.M., Robinson, J.W., & Carlson, L.E. (2013). Sexual values as the key to maintaining satisfying sex after prostate cancer treatment: The physical pleasure-relational intimacy model of sexual motivation. Archives of Sexual Behavior, 42(8), 1637–1647. https://doi.org/10.1007/s10508-013-0168-z
Capistrant, B.D., Torres, B., Merengwa, E., West, W.G., Mitteldorf, D., & Rosser, B.R.S. (2016). Caregiving and social support for gay and bisexual men with prostate cancer. Psycho-Oncology, 25(11), 1329–1336. https://doi.org/10.1002/pon.4249
Chambers, S.K., Ng, S.K., Baade, P., Aitken, J.F., Hyde, M.K., Wittert, G., . . . Dunn, J. (2017). Trajectories of quality of life, life satisfaction, and psychological adjustment after prostate cancer. Psycho-Oncology, 26(10), 1576–1585. https://doi.org/10.1002/pon.4342
Chambers, S.K., Schover, L., Nielsen, L., Halford, K., Clutton, S., Gardiner, R.A., . . . Occhipinti, S. (2013). Couple distress after localised prostate cancer. Supportive Care in Cancer, 21(11), 2967–2976. https://doi.org/10.1007/s00520-013-1868-6
Chan, Z.C.Y., Fung, Y.L., & Chien, W.T. (2013). Bracketing in phenomenology: Only undertaken in the data collection and analysis process. Qualitative Report, 18(30), 59.
Centers for Disease Control and Prevention. (2015). Colorectal cancer control program: Social ecological model. U.S. Department of Health and Human Services. https://bit.ly/2XWMUr9
Daley, E., Alio, A., Anstey, E.H., Chandler, R., Dyer, K., & Helmy, H. (2011). Examining barriers to cervical cancer screening and treatment in Florida through a socio-ecological lens. Journal of Community Health, 36(1), 121–131. https://doi.org/10.1007/s10900-010-9289-7
Ettridge, K.A., Bowden, J.A., Chambers, S.K., Smith, D.P., Murphy, M., Evans, S.M., . . . Miller, C.L. (2018). “Prostate cancer is far more hidden . . . ”: Perceptions of stigma, social isolation and help-seeking among men with prostate cancer. European Journal of Cancer Care, 27(2), e12790. https://doi.org/10.1111/ecc.12790
Ezer, H., Chachamovich, J.R., Saad, F., Aprikian, A., & Souhami, L. (2012). Psychosocial adjustment of men during the first year of prostate cancer. Cancer Nursing, 35(2), 141–147. https://doi.org/10.1097/ncc.0b013e31821f1b81
Forbat, L., Place, M., Hubbard, G., Leung, H., & Kelly, D. (2014). The role of interpersonal relationships in men’s attendance in primary care: Qualitative findings in a cohort of men with prostate cancer. Supportive Care in Cancer, 22(2), 409–415. https://doi.org/10.1007/s00520-013-1989-y
Golden, S.D., & Earp, J.A.L. (2012). Social ecological approaches to individuals and their contexts: Twenty years of Health Education and Behavior health promotion interventions. Health Education and Behavior, 39(3), 364–372. https://doi.org/10.1177/1090198111418634
Grondhuis Palacios, L.A., Krouwel, E.M., den Oudsten, B.L., den Ouden, M.E.M., Kloens, G.J., van Duijn, G., . . . Elzevier, H.W. (2018). Suitable sexual health care according to men with prostate cancer and their partners. Supportive Care in Cancer, 26(12), 4169–4176. https://doi.org/10.1007/s00520-018-4290-2
Hammond, A., & Montgomery, K. (2018). Systematic review and thematic synthesis of quality of life in partners of patients with prostate cancer. Urologic Nursing, 38(4), 194–206. https://doi.org/10.7257/1053-816X.2018.38.4.194
Harden, J.K., Sanda, M.G., Wei, J.T., Yarandi, H., Hembroff, L., Hardy, J., & Northouse, L.L. (2013). Partners’ long-term appraisal of their caregiving experience, marital satisfaction, sexual satisfaction, and quality of life 2 years after prostate cancer treatment. Cancer Nursing, 36(2), 104–113. https://doi.org/10.1097/ncc.0b013e3182567c03
Kalfa, S., Koelmeyer, L., Taksa, L., Winch, C., Viveros, H., Gollan, P.J., . . . Boyages, J. (2019). Work experiences of Australian cancer survivors with lymphoedema: A qualitative study. Health and Social Care in the Community, 27(4), 848–855. https://doi.org/10.1111/hsc.12698
Lim, J.W., Shon, E.J., Paek, M., & Daly, B. (2014). The dyadic effects of coping and resilience on psychological distress for cancer survivor couples. Supportive Care in Cancer, 22(12), 3209–3217. https://doi.org/10.1007/s00520-014-2334-9
Matthew, A.G., Goldman, A., Trachtenberg, J., Robinson, J., Horsburgh, S., Currie, K., & Ritvo, P. (2005). Sexual dysfunction after radical prostatectomy: Prevalence, treatments, restricted use of treatments and distress. Journal of Urology, 174(6), 2105–2110. https://doi.org/10.1097/01.ju.0000181206.16447.e2
McLeroy, K.R., Bibeau, D., Steckler, A., & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351–377. https://doi.org/10.1177/109019818801500401
Merleau-Ponty, M. (2014). Phenomenology of perception (D.A. Landes, Trans.). Routledge. (Original work published 1945)
Moore, A.R., Buchanan, N.D., Fairley, T.L., & Smith, J.L. (2015). Public health action model for cancer survivorship. American Journal of Preventive Medicine, 49(6), S470–S476. https://doi.org/10.1016/j.amepre.2015.09.001
Morse, J.M. (1994). Designing funded qualitative research. In N.K. Denzin & Y.S. Lincoln (Eds.), Handbook of qualitative research (2nd ed., pp. 220–235). Sage.
Norlyk, A., Haahr, A., & Hall, E. (2016). Interviewing with or without the partner present? An underexposed dilemma between ethics and methodology in nursing research. Journal of Advanced Nursing, 72(4), 936–945. https://doi.org/10.1111/jan.12871
O’Shaughnessy, P.K., Ireland, C., Pelentsov, L., Thomas, L.A., & Esterman, A.J. (2013). Impaired sexual function and prostate cancer: A mixed method investigation into the experiences of men and their partners. Journal of Clinical Nursing, 22(23–24), 3492–3502. https://doi.org/10.1111/jocn.12190
Paterson, C., Grzegorz Kata, S., Nandwani, G., Chaudhury, D.D., & Nabi, G. (2017). Unmet supportive care needs of men with locally advanced and metastatic prostate cancer on hormonal treatment: A mixed methods study. Cancer Nursing, 40(6), 497–507. https://doi.org/10.1097/ncc.0000000000000482
Rawla, P. (2019). Epidemiology of prostate cancer. World Journal of Oncology, 10(2), 63–89. https://doi.org/10.14740/wjon1191
Reese, J.B., Keefe, F.J., Somers, T.J., & Abernethy, A.P. (2010). Coping with sexual concerns after cancer: The use of flexible coping. Supportive Care in Cancer, 18(7), 785–800. https://doi.org/10.1007/s00520-010-0819-8
Schantz Laursen, B. (2017). Sexuality in men after prostate cancer surgery: A qualitative interview study. Scandinavian Journal of Caring Sciences, 31(1), 120–127. https://doi.org/10.1111/scs.12328
Smith, J.A. (1996). Beyond the divide between cognition and discourse: Using interpretative phenomenological analysis in health psychology. Psychology and Health, 11(2), 261–271. https://doi.org/10.1080/08870449608400256
Tanner, T., Galbraith, M., & Hays, L. (2011). From a woman’s perspective: Life as a partner of a prostate cancer survivor. Journal of Midwifery and Women’s Health, 56(2), 154–160. https://doi.org/10.1111/j.1542-2011.2010.00017.x
Walker, L.M., Beck, A.M., Hampton, A.J., & Robinson, J.W. (2014). A biopsychosocial approach to sexual recovery after prostate cancer treatment: Suggestions for oncology nursing practice. Canadian Oncology Nursing Journal, 24(4), 256–271. https://doi.org/10.5737/1181912x244256263
Walker, L.M., Wassersug, R.J., & Robinson, J.W. (2015). Psychosocial perspectives on sexual recovery after prostate cancer treatment. Nature Reviews Urology, 12(3), 167–176. https://doi.org/10.1038/nrurol.2015.29
Wassersug, R.J., Westle, A., & Dowsett, G.W. (2017). Men’s sexual and relational adaptations to erectile dysfunction after prostate cancer treatment. International Journal of Sexual Health, 29(1), 69–79. https://doi.org/10.1080/19317611.2016.1204403
Wilde, M.H. (1999). Why embodiment now? Advances in Nursing Science, 22(2), 25–38.
Wittmann, D., Carolan, M., Given, B., Skolarus, T.A., Crossley, H., An, L., . . . Montie, J.E. (2015). What couples say about their recovery of sexual intimacy after prostatectomy: Toward the development of a conceptual model of couples’ sexual recovery after surgery for prostate cancer. Journal of Sexual Medicine, 12(2), 494–504. https://doi.org/10.1111/jsm.12732
Wittmann, D., Foley, S., & Balon, R. (2011). A biopsychosocial approach to sexual recovery after prostate cancer surgery: The role of grief and mourning. Journal of Sex and Marital Therapy, 37(2), 130–144. https://doi.org/10.1080/0092623x.2011.560538
Wittmann, D., Northouse, L., Crossley, H., Miller, D., Dunn, R., Nidetz, J., . . . Montie, J.E. (2015). A pilot study of potential pre-operative barriers to couples’ sexual recovery after radical prostatectomy for prostate cancer. Journal of Sex and Marital Therapy, 41(2), 155–168. https://doi.org/10.1080/0092623X.2013.842194




