COVID-19 Anxiety and Colorectal Cancer Screening Attitudes Among Adult Men in Turkey
Objectives: To examine the relationship between levels of anxiety about COVID-19 and attitudes toward colorectal cancer screening in adult men in Turkey.
Sample & Setting: The participants in this study were 188 adult men, aged 50–70 years, who were not diagnosed with cancer, and who could use social media. The researchers shared the link to the study forms through social media, and data were collected between February 2021 and May 2021.
Methods & Variables: A personal information form, the Coronavirus Anxiety Scale, and the Attitude Scale for Cancer Screening were used to collect descriptive research data.
Results: Participants had mean scores of 1.04 (SD = 2.12) for the Coronavirus Anxiety Scale and 95.28 (SD = 16.91) for the Attitude Scale for Cancer Screening. There was no significant correlation between the scores (p > 0.05). Family structure and the reasons for applying for colorectal cancer screening were significantly related to participation in colorectal cancer screening programs (p < 0.05).
Implications for Nursing: Individualized screening models can be used to prevent the deferral of cancer screenings. To ensure early diagnosis of colorectal cancer, nurses should be encouraged to use telehealth applications and help individuals perform immunochemical tests at home.
Jump to a section
COVID-19, caused by the SARS-CoV-2 virus, was first observed in Wuhan, China. It was recognized as a pandemic by the World Health Organization (WHO) on March 11th, 2020 (Dai et al., 2020; Portnoy et al., 2020). COVID-19 rapidly spread throughout the world. Because of its virulence and the uncertainty about its course, treatment, and efficacy of protective measures, social life changed dramatically. This has had a negative impact on the physical and psychological well-being of individuals (Akkuzu et al., 2020). Psychological problems caused or exacerbated by the COVID-19 pandemic include fear, anxiety, stress, mood changes, deterioration of health, workforce losses, economic problems, and education problems (Lee, 2020). The WHO expressed concerns about the mental health impact and psychosocial consequences of the pandemic (World Health Organization, 2020).
Large-scale studies on individuals at risk for COVID-19 infection have found significant levels of traumatic stress (73%), depression (51%), anxiety (45%), and insomnia (36%) (Liu et al., 2020). Globally, studies have also found increased levels of anxiety, depression, loneliness, drug and alcohol misuse, suicide, and self-harm during the pandemic (Li et al., 2020; Moukaddam & Shah, 2020; Yao et al., 2020). The COVID-19 pandemic has also limited the admission of adults and elderly individuals to healthcare institutions for the diagnosis and treatment of chronic diseases (Çölgeçen & Çölgeçen, 2020; Göksu & Kumcağiz, 2020; Tekpınar et al., 2018; Thornhill & Fincher, 2014; Wang et al., 2020).
Colorectal cancer has the fourth-highest incidence (20%) of all cancer types (Global Cancer Observatory, 2020). Although it is more common in men than in women, it ranks third (11%) among all causes of cancer-related death. Researchers predict that approximately two million people will be diagnosed with colorectal cancer in 2020, and this will increase further in 2040 (Global Cancer Observatory, 2020; Ilgaz & Gözüm, 2014). Early diagnosis of colorectal cancer increases survival rates, making cancer screening vitally important (Fidaner, 2007; Kaya et al., 2017). Screening programs for colorectal cancers can help detect and treat premalignant lesions and cancer cells at an early stage (Ergül et al., 2013; Ilgaz & Gözüm, 2014; Mayir et al., 2018; Öztürk et al., 2019). The National Cancer Screening Program, carried out in line with WHO recommendations, includes fecal occult blood tests (FOBT) every two years and colonoscopy tests every 10 years for adult men and women aged 50–70 years (Ersoy & Saatçi, 2017; Republic of Turkey Ministry of Health, 2015).
The COVID-19 pandemic has had a profound effect on public health. During the early part of the pandemic, fear and anxiety about COVID-19 contagion led to a decrease in the rate of adults applying for preventive and therapeutic services (Argulian, 2020). Hinterberger et al. (2021) evaluated the impact of pandemic restrictions on screening colonoscopies and determined that, compared to the previous year, there was a significant decrease in the number of patients who underwent colonoscopy.
Researchers estimate that changes and limitations in health services, such as the lack or postponement of cancer screenings and treatments, will have serious long-term consequences (Kadakuntla et al., 2021). One study examined colorectal cancer screening by FOBT in Australia, Canada, and the Netherlands. The authors concluded that the disruption to the administration of screening tests would have a significant effect on colorectal cancer incidence and mortality rates between the years 2020 and 2050 (de Jonge et al., 2021).
Individuals’ attitudes toward cancer screening may vary depending on complex physical, biologic, environmental, and psychological factors (Öztürk et al., 2019; Republic of Turkey Ministry of Health, 2015). The COVID-19 pandemic may also affect individuals’ attitudes toward cancer screening. Some studies have examined attitudes toward colorectal cancer screening and the factors that prevent individuals from being screened. Research has been conducted to examine the colorectal cancer screening behaviors of women during the COVID-19 pandemic (Gemalmaz et al., 2015; Kiviniemi et al., 2011; Wilkins et al., 2012). However, to date, no research has investigated the relationship between COVID-19 anxiety and attitudes toward colorectal cancer screening in adult men. Because the incidence and mortality rates of colorectal cancer are higher in men, determining the existence and extent of any correlation could contribute to the literature. This study aimed to examine the correlation between levels of anxiety about COVID-19 and attitudes toward colorectal cancer screening in adult men. The authors also examined the factors that affect attitudes toward colorectal cancer screening during the COVID-19 pandemic.
Methods
This descriptive study was conducted to examine the relationship between COVID-19 anxiety levels and attitudes toward colorectal cancer screening in adult men.
Settings and Recruitment
After permission was obtained from the ethics committee, reliable online survey platforms were selected. For data confidentiality, the authors created a web-based questionnaire. The questionnaire was shared with adult men aged 50–70 years (the age range for colorectal cancer screening according to the National Cancer Screening Program) via social media and a popular messaging application. Before filling out the questionnaire, participants read a text explaining the purpose and rationale of the research. After reading the text, participants consented by answering “yes” to a question about voluntary participation. After the questionnaires were completed, the authors transferred the data to Excel and then to IBM SPSS Statistics, version 21.0, for analysis.
Sample
Participants were adult men aged 50–70 years who were not diagnosed with colorectal cancer. The sample size was calculated using a probabilistic multiple regression analysis calculator with 90% power, 0.15 effect size (moderate), and 5% type I error level, considering the number of independent variables. According to calculations, it was necessary to reach at least 179 individuals (Soper, 2016). The authors reached a total of 239 individuals with the questionnaires. Of these, 188 (79%) individuals answered all the questions and met the inclusion criteria. Participation inclusion criteria were as follows: (a) men aged 50–70 years, (b) volunteered to participate in this study, (c) literate, and (d) able to use social media. Participants were excluded who had a history of colorectal cancer, had psychological problems that precluded participation, and who did not consent to participate in the study.
Ethical Considerations
The study was approved by the Non-Interventional Clinical Research Ethics Committee of İzmir Bakırçay University and was performed in accordance with the Declaration of Helsinki. Before filling out the questionnaire, participants read a text explaining the purpose and rationale of the research. After reading the text, participants consented by answering “yes” to a question about voluntary participation. Participants were informed that they could withdraw from the study at any time without stating a reason.
Data Collection
The researchers shared a link to the online questionnaire on social media and a widely used instant messaging application. Data collection occurred between February 2021 and May 2021. The authors collected data using a personal information form, the Coronavirus Anxiety Scale (CAS), and the Attitude Scale for Cancer Screening (ASCS).
Personal information form: The personal information form was developed by the authors based on the relevant literature. This form consists of 16 questions in two parts. The first part contains nine questions about sociodemographic characteristics, including marital status, education, employment, income, family, and history of intestinal diseases. The second part consists of seven questions about participants’ colorectal cancer screening practices (Akkuzu et al., 2020; Dai et al., 2020; Göksu & Kumcağız, 2020; Lee, 2020; Portnoy et al., 2020).
CAS: The CAS was developed by Lee (2020) to quickly and reliably assess the presence and severity of dysfunctional anxiety symptoms that may arise as psychological reactions to COVID-19 (Lee, 2020). It is a five-point Likert-type scale that consists of five items. Each item is scored from 0 to 4, and there are no reversed items. A higher score indicates a higher level of anxiety. A study by Akkuzu et al. (2020) tested the internal consistency of this scale and found a Cronbach’s alpha of 0.93 (Akkuzu et al., 2020). In this study, the authors found a Cronbach’s alpha of 0.86.
ASCS: This scale was developed by Öztürk et al. (2019) to measure attitudes toward cancer screening. It is a five-point Likert-type scale with one dimension and 24 items. The scores range from 1 (strongly disagree) to 5 (strongly agree). The total score for the ASCS ranges from 24 to 120, with higher scores indicating more positive attitudes toward cancer screening. Öztürk et al. (2019) found a Cronbach’s alpha of 0.95 for the scale, and the authors of this study found a value of 0.92 (Kaya et al., 2017; Öztürk et al., 2019).
Data Analysis
The authors used descriptive statistics for continuous variables (mean and SD) and frequency distributions for categorical variables. The Shapiro–Wilk test, histogram, and normal Q-Q plot were used to test normality. A one-way analysis of variance and an independent sample t test were used to evaluate the differences between sociodemographic characteristics, independent variables, and the ASCS mean scores among participants. Pearson correlation analysis was used to evaluate the difference between the mean scores from the CAS and the ASCS. All statistical analyses were carried out using IBM SPSS Statistics, version 21.0. For all analyses, p < 0.05 was considered significant.
Results
The mean age of participants was 55.63 (SD = 4.63). Most participants were single (89%), employed (65%), and had a nuclear family (89%). Nuclear family refers to a family type consisting of married couples and their children. Extended family refers to a family type that includes grandparents and other relatives in addition to married couples and their children. Nearly half of the participants (46%) had a bachelor’s degree, nearly half had equal income and expenses (49%), and more than half (59%) lived in urban areas (see Table 1).

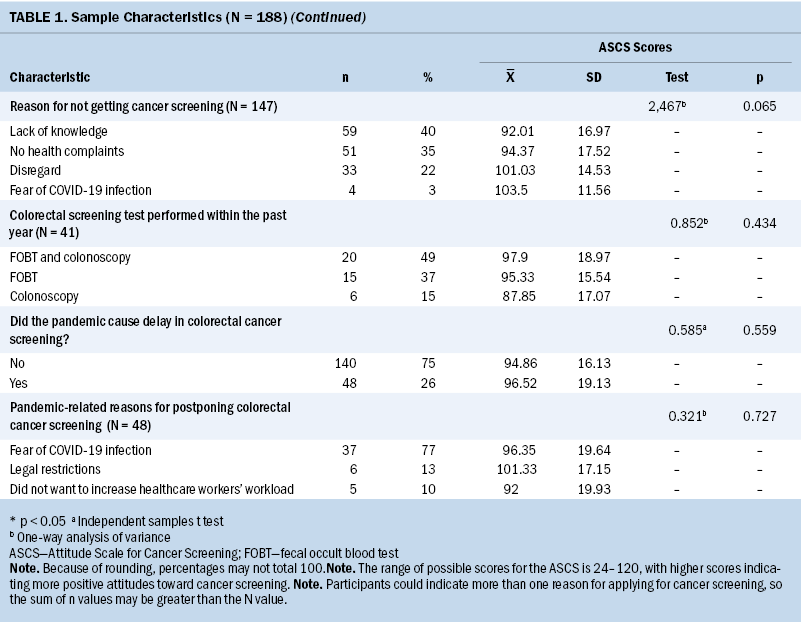
Most participants (91%) and their first-degree relatives (88%) did not have intestinal disease. Of those who were diagnosed with intestinal disease, a significant portion (41%) had a history of polyps. In addition, most of the participants had never had a colorectal cancer screening test before (78%). Participants indicated that having a family history of cancer (24%), seeing themselves at risk because of age (24%), having health complaints (26%), and being recommended to do so by healthcare personnel (29%) would be reasons to seek testing for cancer. Those who had never had a colorectal cancer screening test expressed that their reasons were a lack of knowledge about the subject (40%) or lack of health complaints (35%).
Of those who had undergone colorectal cancer screening in the last year, those who had screening had FOBT (37%), colonoscopy (15%), or both tests (49%). In addition, most of the participants reported that they did not delay screening because of the pandemic (75%). Of those who postponed colorectal cancer screening during the pandemic, most did so because of fear of COVID-19 infection (77%).
Mean scores were 1.04 (SD = 2.12) for the CAS and 95.28 (SD = 16.91) for the ASCS. There was no significant correlation between the scale scores (p > 0.05).
When the mean ASCS scores were examined according to demographic characteristics, the authors found that individuals with nuclear families had higher mean scores on ASCS than individuals with extended families, with a statistically significant difference (p < 0.05). In addition, individuals who applied for cancer screening for the first time because of health complaints had higher ASCS mean scores than those who had a family history of cancer, who had a test because of their age, or who had a test by the recommendation of healthcare personnel (p < 0.05).
Discussion
Participants in this study had above-average positive attitudes toward cancer screening, but three-fourths of the participants had never undergone colorectal cancer screening before or during the pandemic. D’Ovidio et al. (2021) evaluated the effect of the pandemic on colorectal cancer screening programs and reported a decrease in patient participation in screening programs during the pandemic, in keeping with the findings of this study (D’Ovidio et al., 2021). Uninterrupted provision of screening programs affects individuals’ attitudes toward cancer screening. The disruptions in care caused by the pandemic may have had a negative effect on participation in screening programs.
The most important factors in the successful implementation of cancer screening programs are public awareness and attitudes toward cancer screening. Nurses play a crucial role in increasing the public’s awareness about the importance of early diagnosis and in developing positive attitudes toward cancer screening. The WHO (2017) recommends that nurses take key parts in practices aimed at protecting and improving public health. Nurses should provide information about the benefits and risks of the practices used for the early detection of cancer. In addition, nurses can guide research on cancer screening and develop strategies to increase participation in cancer screening programs (Benito et al., 2017).
According to research conducted before the pandemic, participants showed varying attitudes toward colorectal cancer screening. Attitudes were affected by complex factors, including education, age, advice of healthcare professionals, and overall healthcare literacy (Chaka et al., 2018; Gözüyeni et al., 2019; Şen & Öztürk, 2020). The authors observed that sociodemographic characteristics such as marital status, education, employment, income, and place of residence did not affect participants’ attitudes toward cancer screening. However, individuals with nuclear families had more positive attitudes toward cancer screening than those with extended families (p < 0.05). In contrast to this study, previous research found associations between participation in cancer screening and sociodemographic characteristics such as education, income, and financial security (Chaka et al., 2018; Gözüyeşil et al., 2019; Şen & Öztürk, 2020). Wong (2021) examined the knowledge, attitudes, and practices of individuals regarding colorectal cancer screening and reported that financial security was associated with improved attitudes and practices related to cancer screening (Wong, 2021). Bal et al. (2014) noted a correlation between education and screening participation.
Most participants or their first-degree relatives did not have a diagnosis of bowel disease, which may have contributed to a lack of awareness about cancer screening (p > 0.05). This lack of awareness may account for the low trend of participation in screening programs. Studies have shown that negative family history can lead to insufficient awareness about screening for colorectal cancers (Bal, 2014; Cooper & Gelb, 2016; Honein-AbouHaidar et al., 2016). Although the literature seems to support the findings of this study, the authors believe that there is a need for informative activities to increase public awareness about cancer screening.
In this study, one in five participants had had a screening test at least once. Their reasons for applying for screening were, in order of frequency, recommendations of healthcare personnel, having health complaints, being at risk because of age, and having a family history of cancer. Participants who had not screened for cancer were found to have insufficient knowledge about the subject, no health complaints, or indifference to screening. Individuals who had a screening test because of health complaints had more positive attitudes toward cancer screening. The authors believe that having health complaints increases the perception of disease risk and affects the likelihood of admission to healthcare services. Being informed about the risks of cancer and being directed to screening programs after presenting to healthcare institutions are some of the most important factors that affect participation in screening (Altun, 2020b; Tfaily et al., 2019;). Altun (2020b) found that most individuals who had colorectal cancer screening (68%) were tested on the recommendation of a physician, and fewer (18%) had the test on their own accord. Raising awareness about the severity of the disease and the benefits of screening programs, with the necessary information and guidance, can help positively affect patients’ attitudes toward cancer screening, eliciting healthier preventive behaviors.
Most participants had never had a screening test for colorectal cancer before or during the COVID-19 pandemic. Approximately half of the participants who had had a screening test had undergone both colonoscopy and FOBT. The literature states that individuals tend to prefer FOBT because it is faster, easier, and causes less pain and embarrassment. Colonoscopy is preferred in cases where definitive results are needed, because of physician recommendation, and when there is suspicion of disease (Cooper & Gelb, 2016; Şahin & Üner, 2015). Initiatives to reduce pain and negative experiences related to colorectal cancer screening procedures will encourage individuals to participate in rescreening programs when necessary.
The authors determined that most of the participants did not postpone their colorectal cancer screenings during the COVID-19 pandemic. Those who postponed their screenings did so because of fear of COVID-19 infection, legal restrictions, or a desire to not increase the burden on healthcare personnel. Research has found that the COVID-19 pandemic negatively affected patient access to preventive and therapeutic healthcare services as a result of socioeconomic problems, legal restrictions, the need to care for relatives, and fear of contagion (Kadakuntla et al., 2021). Because of the decrease in applications for primary healthcare services, the decreased number of individuals undergoing FOBT or colonoscopy, and the delay of colonoscopy procedures in individuals with positive FOBT results, there will inevitably be increased diagnoses of colorectal cancers, with a higher incidence at advanced stages. Accelerating the transition to telehealth applications, using electronic records to identify and track patients in need of screening, directing individuals to use at-home FOBT kits, delivering these tests to people by mail if necessary, and only directing high-risk patients to colonoscopy based on FOBT results, are some of the successful strategies for improving the efficacy of colorectal cancer screening. Nurses should take a leading role in conducting research to detect any shortcomings in screening programs and implement screening strategies (Bestari & Joewono, 2021; Levin et al., 2018; Sharpless, 2020; Somsouk et al., 2020).
In keeping with previous research, participants in this study had low levels of COVID-19 anxiety (Altun, 2020a; Erdoğdu et al., 2020, Sağlam et al., 2020). Recent epidemiological studies have found a higher prevalence of COVID-19–related anxiety, depression, and stress among women than among men (Ahmed et al., 2020; Huang & Zhao, 2020; Moghanibashi-Mansourieh, 2020; Salari et al., 2020). However, this study was conducted relatively early in the pandemic, and the sample group consisted of adult men aged 50–70 years, which may account for these findings.
Most participants had not undergone cancer screening. In this context, this study’s findings indicate that COVID-19 anxiety levels do not affect attitudes toward cancer screening and that awareness about the importance of cancer screening and early diagnosis is insufficient. Many participants had little education and lived in rural areas, which may have resulted in lack of awareness about cancer screening.
Limitations
According to epidemiological studies, the fact that this research was conducted earlier in the pandemic may have affected individuals’ COVID-19 anxiety levels.
Implications for Nursing
Nurses play a key role in preventing the long-term negative consequences of delays to colorectal cancer screening during the COVID-19 pandemic. It is important for nurses to organize training programs and provide counseling on the risk factors of colorectal cancer, the importance of early diagnosis, and screening programs. This can help increase public awareness and prevent cancer incidence and mortality rates from increasing. During the pandemic, individualized screening models can be used to prevent the deferral of cancer screenings. Nurses should encourage individuals to perform immunochemical tests at home, allowing for early diagnosis of colorectal cancer. In addition, the use of telehealth applications should be strengthened to reduce applications to screening centers and face-to-face meetings, creating more options for individuals who cannot access healthcare institutions.
Conclusion
In this study, adult men aged 50–70 years expressed low levels of anxiety toward the COVID-19 pandemic and above-average positive attitudes toward cancer screening. COVID-19 anxiety levels did not affect participants’ attitudes toward cancer screening. Most participants had never undergone colorectal cancer screening. Nurses should organize patient education programs and provide counseling for the public about the risk factors of cancer, the importance of early diagnosis, and participation in cancer screening programs.
The authors gratefully acknowledge the nurses who participated in this study.
About the Authors
Ayşegül Çelik, PhD, RN, is an assistant professor, Derya Çinar, PhD, RN, is an assistant professor, Nazan Kiliç Akça, PhD, RN, is an associate professor, Pinar Zorba Bahceli, PhD, RN, is an assistant professor, and Aslıhan Öztürk, MD, RN, is a research assistant, all in in the Department of Nursing in the Faculty of Health Sciences at İzmir Bakırçay University in İzmir, Turkey. No financial relationships to disclose. All authors contributed to the conceptualization, design, and manuscript preparation. Çelik, Çinar, and Öztürk completed the data collection. Çelik and Akça provided statistical support and analysis. Öztürk can be reached at aslihan.ozturk@bakircay.edu.tr, with copy to ONFEditor@ons.org. (Submitted October 2021. Accepted February 7, 2022.)
References
Ahmed, M.Z., Ahmed, O., Aibao, Z., Hanbin, S., Siyu, L., & Ahmad, A. (2020). Epidemic of COVID-19 in China and associated psychological problems. Asian Journal of Psychiatry, 51, 102092. https://doi.org/10.1016/j.ajp.2020.102092
Akkuzu, H., Yumuşak, F.N., Karaman, G., Ladikli, N., Türkkan, Z., & Bahadır, E. (2020). Koronavirüs Kaygı Ölçeği’nin Türkçe güvenirlik ve geçerlik çalışması [Turkish reliability and validity study of the Coronavirus Anxiety Scale]. Kıbrıs Türk Psikiyatri ve Psikoloji Dergisi, 2(2), 63–67. https://doi.org/10.35365/ctjpp.20.2.09
Altun, Y. (2020a). COVİD-19 pandemisinde kaygı durumu ve hijyen davranışları [Anxiety and hygiene behavior during the COVID-19 pandemic]. STED/Sürekli Tıp Eğitimi Dergisi, 29(5), 312–317. https://doi.org/10.17942/sted.777035
Altun, Y. (2020b). Factors influencing women’s participation in cancer screening. Turkish Journal of Family Medicine and Primary Care, 14(2), 210–215. https://doi.org/10.21763/tjfmpc.645578
Argulian E., (2020). Anticipating the “second wave” of health care strain in the COVID-19 pandemic. JACC Case Reports, 2(5), 845–846. https://doi.org/10.1016/j.jaccas.2020.04.005
Bal, M.D. (2014). Kadınların pap smear testi yaptırma durumlarının sağlık inanç modeli ölçeği ile değerlendirilmesi [Evaluation of women having pap smear test by Health Belief Model Scale]. Clinical and Experimental Health Sciences, 4(3), 133–138.
Bestari, M.B., & Joewono, I.R. (2021). Screening colonoscopy for colon cancer in women during COVID-19 pandemic. Acta Medica Indonesiana, 53(1), 132–139.
Chaka, B., Sayed, A.R., Goeieman, B., & Rayne, S. (2018). A survey of knowledge and attitudes relating to cervical and breast cancer among women in Ethiopia. BMC Public Health, 18(1), 1–8. https://doi.org/10.1186/s12889-018-5958-8
Cooper, C.P., & Gelb, C.A. (2016). Opportunities to expand colorectal cancer screening participation. Journal of Women’s Health, 25(10), 990–995. https://doi.org/10.1089/jwh.2016.6049
Çölgeçen, Y., & Çölgeçen, H. (2020). COVID-19 pandemisine bağlı yaşanan kaygı düzeylerinin değerlendirilmesi: Türkiye örneği [Evaluation of anxiety levels arising from COVID-19 pandemic: The case of Turkey]. Electronic Turkish Studies, 15(4).
Dai, M., Liu, D., Liu, M., Zhou, F., Li, G., Chen, Z., . . . Cai, H. (2020). Patients with cancer appear more vulnerable to SARS-CoV-2: A multicenter study during the COVID-19 outbreak. Cancer Discovery, 10(6), 783–791. https://doi.org/10.1158/2159-8290.CD-20-0422
de Jonge, L., Worthington, J., van Wifferen, F., Iragorri, N., Peterse, E., Lew, J.B., . . . Lansdorp-Vogelaar, I. (2021). Impact of the COVID-19 pandemic on faecal immunochemical test-based colorectal cancer screening programmes in Australia, Canada, and the Netherlands: A comparative modelling study. The Lancet Gastroenterology & Hepatology, 6(4), 304–314. https://doi.org/10.1016/S2468-1253(21)00003-0
D’Ovidio, V., Lucidi, C., Bruno, G., Lisi, D., Miglioresi, L., & Bazuro, M.E. (2021). Impact of COVID-19 pandemic on colorectal cancer screening program. Clinical Colorectal Cancer, 20(1), e5–e11. https://doi.org/10.1016/j.clcc.2020.07.006
Erdoğdu, Y., Koçoğlu, F., & Sevim, C. (2020). COVID-19 pandemisi sürecinde anksiyete ile umutsuzluk düzeylerinin psikososyal ve demografik değişkenlere göre incelenmesi [Investigation of anxiety and hopelessness levels according to psychosocial and demographic variables during the COVID-19 pandemic]. Klinik Psikiyatri Dergisi, 23(1), 24–37. https://doi.org/10.5505/kpd.2020.35403
Ergül, B., Sarıkaya, M., Doğan, Z., & Filik, L. (2013). Kolorektal kanserli hastaların asemptomatik birinci derece yakınlarının kolonoskopik değerlendirme sonuçları: Tek merkezli prospektif çalışma [Colonoscopic assessment results of asymptomatic first-degree relatives of patients with colorectal cancer: A single center prospective study]. Endoscopy Gastrointestinal, 21(2), 36–38.
Ersoy, E., & Saatçi, E. (2017). Kanser taramaları: İhtilaflar [Cancer screening: Controversies]. Türkiye Aile Hekimliği Dergisi, 21(3), 96–100. https://doi.org/10.15511/tahd.17.00396
Fidaner, C. (2007). Kanserde erken yakalama: Erken tanı ve taramalar [Early detection in cancer: Early diagnosis and screenings]. A.M. Tuncer (Ed.), Türkiye’de kanser kontrolü [Cancer control in Turkey]. Onur Matbaacılık.
Gemalmaz, A. (2015). Aydın merkez ilçede kolorektal kanser taramasına ilişkin bilgi, tutum ve engeller [Knowledge, attitudes and barriers to colorectal cancer screening in the central district of Aydın]. Türkiye Aile Hekimliği Dergisi, 19(1), 37–48. https://doi.org/10.15511/tahd.15.01037
Global Cancer Observatory. (2020). Cancer Today. https://gco.iarc.fr
Göksu, Ö., & Kumcağız, H. (2020). COVID-19 salgınında bireylerde algılanan stres düzeyi ve kaygı düzeyleri [Perceived stress level and anxiety levels in individuals in the COVID-19 outbreak]. Electronic Turkish Studies, 15(4). https://doi.org/10.7827/TurkishStudies.44397
Gözüyeşil, E., Arıöz Düzgün, A., & Ünal Aslan, K. (2019). Kadınların serviks kanserinden korunma ve erken tanıya yönelik tutumlarının değerlendirilmesi [Evaluation of women’s attitudes toward prevention of cervical cancer and early diagnosis]. Sürekli Tıp Eğitimi Dergisi, 28(4), 229–238. https://doi.org/10.17942/sted.444170
Hinterberger, A., Jiricka, L., Waldmann, E.A., Penz, D., Majcher, B., Asaturi, A., . . . Ferlitsch, M. (2021). Impact of restrictions due to COVID-19 on a quality-assured screening colonoscopy program. Endoscopy International Open, 9(9), E1315–E1320. https://doi.org/10.1055/a-1497-1123
Honein-AbouHaidar, G.N., Kastner, M., Vuong, V., Perrier, L., Daly, C., Rabeneck, L., . . . Baxter, N.N. (2016). Systematic review and meta-study synthesis of qualitative studies evaluating facilitators and parriers to participation in colorectal cancer screening. Cancer Epidemiology, Biomarkers & Prevention, 25(6), 907–917. https://doi.org/10.1158/1055-9965.EPI-15-0990
Huang, Y., & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research, 288, 112954. https://doi.org/10.1016/j.psychres.2020.112954
Ilgaz, A.E., & Gözüm, S. (2014). Kanser taramalarında öncelikli hedef birinci derece akrabalar [Primary target first-degree relatives in cancer screening]. Dokuz Eylül Üniversitesi Hemşirelik Fakültesi Elektronik Dergisi, 7(4), 345–353.
Ilgaz, A.E., & Gözüm, S. (2018). Determination of colorectal cancer risk levels, colorectal cancer screening rates and factors affecting participation in screening of ındividuals working in agriculture in Turkey. Cancer Nursing, 41(4), E46–E54. https://doi.org/10.1097/NCC.00000000000000053
Kadakuntla, A., Wang, T., Medgyesy, K., Rrapi, E., Litynski, J., Adynski, G., & Tadros, M. (2021). Colorectal cancer screening in the COVID-19 era. World Journal of Gastrointestinal Oncology, 13(4), 238–251. https://doi.org/10.4251/wjgo.v13.i4.238
Kaya, C., Üstü, Y., Özyörük, E., Aydemir, Ö., Şimşek, Ç., & Şahin, A.D. (2017). Sağlık çalışanlarının kanser taramaları hakkındaki bilgi, tutum ve davranışlarının değerlendirilmesi [Evaluation of knowledge, attitudes and behaviors of healthcare professionals about cancer screening]. Ankara Medical Journal, 17(1), 73–83.
Kiviniemi, M.T., Bennett, A., Zaiter, M., & Marshall, J.R. (2011). Individual-level factors in colorectal cancer screening: A review of the literature on the relation of individual-level health behavior constructs and screening behavior. Psycho-Oncology, 20(10), 1023–1033. https://doi.org/10.1002/pon.1865
Lee, S.A. (2020). Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Studies, 44(7), 393–401. https://doi.org/10.1080/07481187.2020.1748481
Levin, T.R., Corley, D.A., Jensen, C.D., Schottinger, J.E., Quinn, V.P., Zauber, A.G., . . . Doubeni, C.A. Effects of organized colorectal cancer screening on cancer incidence and mortality in a large community-based population. Gastroenterology, 155(5), 1383–1391. https://doi.org/10.1053/j.gastro.2018.07.017
Li, W., Yang, Y., Liu, Z.H., Zhao, Y.J., Zhang, Q., Zhang, L., . . . Xiang, Y.T. (2020). Progression of mental health services during the COVID-19 Outbreak in China. International Journal of Biological Sciences, 16(10), 1732–1738. https://doi.org/10.7150/ijbs.45120
Liu, S., Yang, L., Zhang, C., Xiang, Y., Liu, Z., Hu, S., & Zhang, B. (2020). Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry, 7(4), e17–e18. https://doi.org/10.1016/S2215-0366(20)30077-8
Mayir, B., Ensari, C.Ö., Durhan, A., & Çöpelci, Y. (2018). Kolorektal kanser tarama amaçlı yapılan gaytada gizli kan testi pozitif saptanan hastalarda kolonoskopi bulguları [Colonoscopy findings in patients with positive stool occult blood test performed for colorectal cancer screening]. Turkish Journal of Colorectal Disease, 28(1), 27.
Moghanibashi-Mansourieh, A. (2020). Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian Journal of Psychiatry, 51, 102076. https://doi.org/10.1016/j.ajp.2020.102076
Moukaddam, N., & Shah, A. (2020). Psychiatrists beware! The impact of COVID-19 and pandemics on mental health. Psychiatric Times, 37(3).
Öztürk, E.N.Y., Uyar, M., & Şahin, T.K. (2019). Kanser Taramalarına Yönelik Tutum Ölçeği geliştirilmesi [Developing Attitude Scale Toward Cancer Screening]. 3 International 21 National Public Health Congress.
Portnoy, J., Waller, M., & Elliott, T. (2020). Telemedicine in the era of COVID-19. Journal of Allergy and Clinical Immunology in Practice, 8(5), 1489–1491. https://doi.org/10.1016/j.jaip.2020.03.008
Republic of Turkey Ministry of Health. (2015). Aile Hekimliği Uygulamasında Önerilen Periyodik Sağlık Muayeneleri ve Tarama Testleri [Periodic health examinations and screening tests recommended in family medicine practice]. https://hsgm.saglik.gov.tr/depo/birimler/Toplum_Sagligi_Hizmetleri_ve_E…
Republic of Turkey Ministry of Health. (2017). Kanser Taramaları [Cancer screenings]. https://hsgm.saglik.gov.tr/tr/kanser-taramalari
Sağlam, Ö., Salman, Ö., & Kök, B.E. (2020). İstanbul Eğitim ve Araştırma Hastanesi’ne Başvuran ve Cevizlibağ Atatürk Kız Öğrenci Yurdu’nda Karantinaya Alınan Şüpheli ve Kesin COVİD-19 Tanısı Alan Bireylerin Uykusuzluk, Anksiyete ve Depresyon Düzeylerinin Ölçülmesi [Measuring the insomnia, anxiety and depression levels of individuals admitted to Istanbul Training and Research Hospital and quarantined in Cevizlibağ Atatürk Girls’ dormitory with suspected and definitive COVID-19 diagnosis]. Türkiye Sosyal Hizmet Araştırmaları Dergisi, 4(3), 73–81.
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Mohammadi, M., . . . Khaledi-Paveh, B. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health, 16(1), 175–183. https://doi.org/10.1186/s12992-020-00589-w
Şahin, N.Ş., & Üner, B.A. (2015). Aydın merkez ilçede kolorektal kanser taramasına ilişkin bilgi, tutum ve engeller [Knowledge, attitudes and barriers to colorectal cancer screening in the central district of Aydın]. Türkiye Aile Hekimliği Dergisi, 19(1), 37–48.
Şen, S.K., & Öztürk, Y.K. (2020). Sağlık Algısı ile Kanser Taraması Farkındalığı Arasındaki İlişki [The relationship between health perception and cancer screening awareness]. Türkiye Aile Hekimliği Dergisi, 24(4), 175–183.
Sharpless, N.E. (2020). COVID-19 and cancer. Science, 368(6497), 1290. https://doi.org/10.1126/science.abd3377
Somsouk, M., Rachocki, C., Mannalithara, A., Garcia, D., Laleau, V., Grimes, B., . . . Ladabaum, U. (2020). Effectiveness and cost of organized outreach for colorectal cancer screening: A randomized, controlled trial. Journal of the National Cancer Institute, 112(3), 305–313. https://doi.org/10.1093/jnci/djz110
Soper, D.S. (2016). Free statistics calculators. [Software]. https://www.danielsoper.com/statcalc
Taşkın, C., Dağhan, Ş., & Kalkım, A. (2014). Yaşlı bireylerin kolorektal kanserin riskleri ve erken tanısına yönelik bilgi düzeylerinin ve bu kanserle ilişkili risklerinin incelenmesi [Investigation of the knowledge level of elderly individuals about the risks and early diagnosis of colorectal cancer and the risks associated with this cancer]. Süleyman Demirel Üniversitesi Sağlık Bilimleri Dergisi, 5(3), 88–93.
Tekpınar, H., Özen, M., & Aşık, Z. (2018). Aile Hekimliği polikliniğine başvuran hastaların kanser taramalarına ilişkin yaklaşımlarının değerlendirilmesi [Evaluation of the approaches to cancer screening of patients who applied to the Family Medicine outpatient clinic]. Türkiye Aile Hekimliği Dergisi, 22(1), 28–36. https://doi.org/%2010.15511/tahd.18.00128
Tfaily, M.A., Naamani, D., Kassir, A., Sleiman, S., Ouattara, M., Moacdieh, M.P., & Jaffa, M.A. (2019). Awareness of colorectal cancer and attitudes toward its screening guidelines in Lebanon. Annals of Global Health, 85(1), 75. https://doi.org/10.5334/aogh.2437
Thornhill, R., & Fincher, C.L. (2014). The parasite-stress theory of sociality, the behavioral immune system, and human social and cognitive uniqueness. Evolutionary Behavioral Sciences, 8(4), 257–264. https://psycnet.apa.org/doi/10.1037/ebs0000020
Yao, H., Chen, J., & Xu, Y. (2020). Patients with mental health disorders in the COVID-19 epidemic. The Lancet, 7(4), e21. https://doi.org/10.1016/S22150366(20)30090-0
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C.S., & Ho, R.C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. https://doi.org/10.3390/ijerph17051729
Wilkins, T., Gillies, R.A., Harbuck, S., Garren, J., Looney, S.W., & Schade, R.R. (2012). Racial disparities and barriers to colorectal cancer screening in rural areas. Journal of the American Board of Family Medicine, 25(3), 308–317. https://doi.org/10.3122/jabfm.2012.03.100307
Wong, F.M. (2021). Factors associated with knowledge, attitudes, and practice toward colorectal cancer and its screening among people aged 50–75 years. International Journal of Environmental Research and Public Health, 18(8), 4100. https://doi.org/10.3390/ijerph18084100
World Health Organization. (2017). Enhancing the role of community health nursing for universal health coverage. https://apps.who.int/iris/bitstream/handle/10665/255047/9789241511896-e…
World Health Organization. (2020). Mental health and psychosocial considerations during the COVID-19 outbreak. https://apps.who.int/iris/handle/10665/331490




