Impact of a Hematologic Malignancy Diagnosis and Treatment on Patients and Their Family Caregivers
Objectives: Hematologic malignancies (HMs) are life-threatening cancers that frequently entail aggressive, long, inpatient treatment protocols. This can result in numerous concurrent symptoms and decreased quality of life for patients and can affect family caregivers (FCs). This study examined the impact of an HM diagnosis on patients and on their FCs.
Sample & Setting: A descriptive design was used to explore the experiences of 28 newly diagnosed patients and their FCs. All patients were receiving treatment on an inpatient acute oncology unit at a National Cancer Institute–designated cancer center.
Methods & Variables: Semistructured, separate interviews with patients and FCs were recorded and transcribed verbatim. Textual and content analyses were conducted to generate common themes.
Results: Patients and FCs reported how diagnosis and treatment affected them physically, emotionally, logistically, and financially. They described the effects of their experiences with the health system and providers in areas such as diagnostic process, trust in the medical team, support needs, and hospitalization.
Implications for Nursing: Understanding the parallel experiences of patients with HMs and their designated FCs allows researchers to develop targeted interventions and enables clinicians to provide personalized patient- and family-centered care.
Jump to a section
Hematologic malignancies (HMs) are a heterogeneous group of cancers that affect the blood, bone marrow, and lymph nodes. Many HMs are aggressive cancers requiring prompt treatment for control and survival. Patients with HM commonly require sudden and protracted hospital stays for the diagnosis and treatment of their disease. These hospitalizations frequently last for at least three to four weeks with ongoing monthly admissions for several days at a time thereafter.
Because of the intense treatment and inherent threat associated with aggressive cancers, it is perhaps not surprising that patients with HM experience high levels of symptom burden and cancer-related distress (Albrecht, 2014; Carlson et al., 2004; Manitta et al., 2011). The distress of the diagnosis and the intensity of the treatment may negatively affect physical and psychological health; these can also reduce physical function, which undermines patients’ quality of life and ability to accomplish daily activities such as work, household management, parenting, and recreational activities (Albrecht et al., 2017; Klepin et al., 2016; Leak Bryant et al., 2015; LeBlanc et al., 2015). Unfortunately, patients with HM may not receive the supportive care needed to address these challenges. For example, one study showed that although nearly half the patients with HM reported significant cancer-related distress, the majority did not seek or receive treatment for it; more often, they relied on the immediate medical team and their own family and social network for support (Carlson et al., 2004).
Family systems theory describes the family as a social system that is necessary for the survival and welfare of its individual members (Carr, 2015). No single individual in a family exists in isolation, so significant life events such as HM diagnosis and treatment can affect other family members (Wright & Leahey, 2005). Reorganizations must occur as well as changes in family members’ roles and routines as a result of significant illness. For example, there may be a reduction in the patient’s responsibilities (e.g., employment, household chores, parenting) that are absorbed by another person, which may generate elevated levels of stress for the family or a specific family member. As such, and in congruence with the stress associated with the illness itself, the family members’ mental and physical resources are more likely to become depleted, making adaptation more challenging and intensifying the effects of the disease on both the patient and their family.
One family member or close friend often takes on the key, informal role of family caregiver (FC). The FC is the person who voluntarily assists the patient with pragmatic needs and helps to manage physical and psychological challenges related to the disease and treatment, all while navigating the healthcare system (Frambes et al., 2018; Kent et al., 2016). As such, FCs may be particularly affected by the illness, experiencing not only emotional challenges but also added practical (e.g., household management) and logistical (e.g., attending and traveling to and from appointments) responsibilities and the accompanying stress. The negative side effects of HM treatment often require patients to be supported by FCs, particularly when care transitions into the home. This can place significant strain on FCs, who frequently endure their own physical and psychological challenges as a result of their loved one’s illness (Williams, 2018).
There are limited data on the effects of an HM diagnosis on adult patients and FCs, particularly regarding their individual experiences in tandem. Much of the current data on patient and caregiver experiences, as well as caregiver burden exist for populations with heart failure, dementia, pediatric cancer, solid tumors, and bone marrow transplantations. In these populations, FCs experience depression, financial stress, and social isolation (Adelman et al., 2014; Fife et al., 2009; Saunders, 2008) as well as poor health outcomes (Pressler et al., 2013). For individuals diagnosed with HM for whom cure is a long-term treatment goal, hematopoietic stem cell transplantation may be necessary. Current evidence demonstrates the significant effects that this treatment has on patients and their family members (Applebaum et al., 2016).
After diagnosis and during treatment, both the patient with HM and their designated FC experience changes in their environments, household responsibilities, and stress levels. These changes may undermine each individual’s healthy adaptation and contribute to the effect on the family as a whole in terms of environmental comfort and physical, emotional, logistical, and financial adjustment. Patients diagnosed with HM face the prospect of a long course of aggressive treatments, which may exacerbate the challenges and confer risk on the long-term health and well-being of these patients and their FCs.
However, little is known about the specific and unique experiences of patients with HM and FCs. The purpose of this study is to describe the impact of a new HM diagnosis on patients and their FCs. It leverages a descriptive study design that analyzes qualitative data to understand how an HM diagnosis affects patients and their FCs, and uses quantitative data to enumerate similarities and differences in participant experiences. The time from HM diagnosis through treatment can be highly stressful, complicated, and ambiguous because of the labile nature and potential mortality of the illness. It is important to investigate the experiences of patients and their FCs to develop a deeper understanding of the challenges they each face. This knowledge will contribute to research and tailored interventions to help alleviate barriers and distress among patients with HM and their close family.
Methods
A descriptive qualitative study design (Sandelowski, 2010) was applied to capture the experiences of patients with HM and their FCs during the initiation of treatment. The cross-sectional data reported in this article were collected as part of a longitudinal descriptive study exploring the individual experiences and informational needs of patients with HM and their designated FCs during the initial diagnosis and treatment.
Sample and Setting
The study was approved by the institutional review board and conducted at a National Cancer Institute–designated cancer center in the mid-Atlantic region of the United States. Patients with HM who were aged 18 years or older, diagnosed with a HM in the past three months, and able to read, write, and speak English were recruited from an inpatient oncology unit. Patients with HM who agreed to participate in the study identified their unpaid primary support person, or FC, who was also invited to participate. The researchers were employed by the university connected with the study site but were not part of the participants’ medical or psychosocial teams.
Data Collection
Patients with HM and their FCs each provided informed consent, reported demographics, and completed two questionnaires and interviews. The first questionnaire and interview took place within three months of diagnosis, and the second occurred approximately six weeks after the initial interview. All participants were compensated $25 for each interview.
This report focuses on the findings from the initial semistructured interviews. Patients and FCs were interviewed separately and privately, in either a hospital room or other spare space within the inpatient cancer center. If it was more convenient for participants, there was an option to complete the interviews via telephone. Trained graduate students used an interview guide developed for this study to complete the interviews. Patients and FCs were asked questions related to their experiences with the diagnosis and initiation of treatment within specific quality-of-life domains (e.g., “How are you eating? How are you sleeping? How is your energy? How are your social supports? Are financial strains related to this new diagnosis?”). The FCs were asked additional questions related to their preparedness for the caregiver role (e.g., “How prepared do you feel to take on the role of caregiver?”), and challenges associated with providing care (“What have been the biggest challenges you’ve faced since the diagnosis?”). Follow-up prompts were used when necessary to further understand the participants’ experiences and perspectives. The research team reviewed the first two interviews to ensure that the questions were eliciting responses related to the aims of this study. After this review, enrollment and data collection continued alongside ongoing assessments monitoring for accuracy and saturation.
Data Analysis
An inductive thematic analysis was used to facilitate the identification of meaning that participants placed on their experiences (Sandelowski, 2010). All interviews were audio recorded and later transcribed verbatim with the exception of identifying information, which was replaced by a general descriptor (e.g., a patient’s name would be replaced by “[patient name]”). Once data saturation was reached and accuracy of transcripts was confirmed, the deidentified data were uploaded to NVivo, version 12 for analysis. Three study team members participated in the data analysis and coding. The transcripts were read and reread to ensure data immersion. Line-by-line analysis was completed, and preliminary inductive codes were assigned to the data. The data reduction process included a review of common categories and themes. The study team identified, reviewed, and discussed the categories and themes until consensus was reached. During this process, a codebook was created for codes, definitions, and examples of themes identified in the interviews. The iterative questioning, debriefing among the study team, review of data to ensure the interview questions provided rich responses, and creation of a working document detailing the audits and study-related decisions were all approaches applied to ensure rigor and trustworthiness of the analysis and findings (Lincoln & Guba, 1985).
Findings
Twenty-eight patients and 28 FCs who completed initial interviews were included in the analysis. Demographic characteristics are presented in Table 1. Most of the participating patients were diagnosed with acute leukemia (n = 25). They ranged in age from 20–76 years (mean = 53.39, SD = 16.67) and identified mostly as White (n = 19) and men (n = 16). Most FCs were spouses of patients (n = 19), women (n = 19), and White (n = 19); they ranged in age from 29–76 years (mean = 54.29, SD = 15.19).

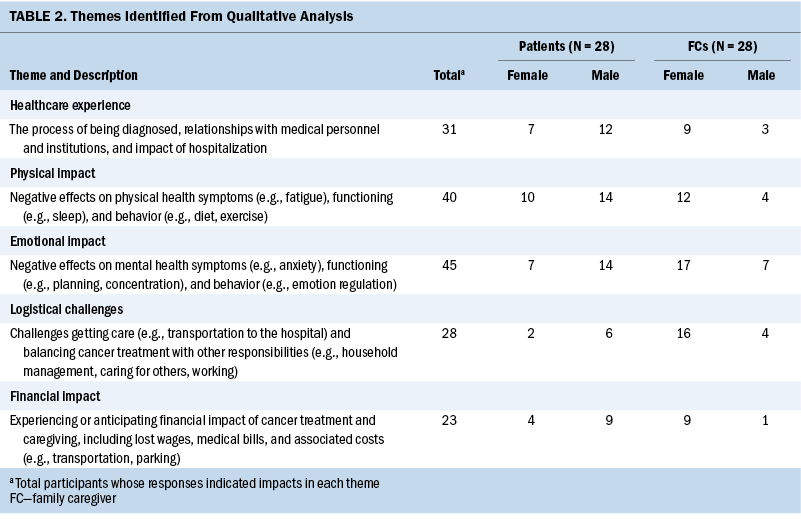
Patients and FCs spent between 10 and 60 minutes each responding to interview questions (mean = 21 minutes for patients; mean = 19 minutes for FCs). The data analysis revealed five key themes that chronicled the individual experiences of patients and FCs. Themes and frequencies are presented in Table 2.
Healthcare Experience
In this study, 19 patients with HM and 12 FCs valued the relationship they had with the hematology-oncology team. In particular, they described compassion as a leading indicator of quality care. Patients and FCs spoke directly about the positive difference it made for them when their medical teams (a) had good bedside manner, (b) spent time describing the diagnosis in terms the patient and FC could understand, (c) kept the patient and FC informed as to the next steps of the treatment plan, (d) maintained consistency in doctors they saw on rotation, and (e) apprised them of available resources, such as social services (e.g., to assist them with financing the treatment).
[The hospital staff] has been fantastic. The doctors don’t even have that uppity attitude. They are down to earth, open, and honest. It’s been wonderful. (patient 119)
This is a teaching hospital and everyone has had a great bedside manner. They don’t mind explaining the process of his condition, what they are doing to treat it, and what the side effects are. (FC 113)
Ultimately, patients with HM and their FCs indicated that approachability in the hematology-oncology team aided in overall trust, increased comfort in decision-making, and abated stress.
Patients and their FCs spoke about negative interactions related to the overall healthcare experience. They shared concerns about delayed referrals to skilled hematology-oncology services for further patient workup, diagnosis, or treatment. Both groups shared challenges with nutrition during hospital stays related to inconsistent, incorrect, or unappetizing food orders, which resulted in families incurring additional expenses when having to purchase food from hospital restaurants. One FC commented,
The kitchen here is horrible . . . there have been times he’s ordered his meal and he’s waited two hours for his tray to come up only to get something that wasn’t what he ordered and we’ve talked to the nurses about that and they said it’s a problem with all of the patients. (FC 138)
Participants in this study also shared concerns regarding the lack of showers and comfortable places for the FC to sleep. The frequent sleep interruptions related to treatment and care were also negative experiences shared by participants. Some participants felt that the hematology-oncology team was inaccessible, which led to perceptions of an understaffed hospital and lack of communication between doctors and nurses during rotations. In addition, some participants shared concerns regarding cursory examinations and strained rapport with providers.
Getting information has been hard. Getting the same story twice has been impossible, so you never really know what’s going on. (FC 138)
Negative experiences were particularly challenging because patients and FCs not only had limited knowledge of the diagnosis, but also struggled to meet many of their basic needs including food, hygiene, and sleep.
Physical Impact
The majority of patient (n = 24) and FC (n = 16) participants reported that the HM diagnosis and treatment had taken a toll on their physical health and well-being. The patients reported concerns with temperature variations as well as treatment-related side effects such as fever, exhaustion, frequent urination, and difficulties with mobility, concentration, memory, eating, sleeping, and breathing.
Trying to keep my platelets up, but the body is going to do what it’s going to do. I’ve been tired, sleeping a lot, and had chills a couple of times. One time it scared [the hospital staff] ‘cause my temperature went from 98 to 101. (patient 134)
Similarly, FCs also reported their own feelings of exhaustion and difficulties with concentration, memory, eating, and sleeping. Many FCs said that the physical toll resulted from being overwhelmed and putting the patient before themselves.
Your concentration is off. I’ve got this little brain, it’s like a BB in a box car, and it can’t take so much information, and [hospital staff’s] just loading with information. Stuff you’ve never heard of—blood types. Trying to take all this in is hard. (FC 122)
Emotional Impact
Patients with HM (n = 21) and FCs (n = 24) both reported significant emotional burdens, such as heightened levels of distress, worries about each other’s physical and psychological well-being, negative emotions about having to place their lives on hold, current and anticipated impacts of the disease on the rest of the family, and frequent reminders of death. Patients mentioned that the diagnosis and treatment contributed to their deteriorating mental health and increased feelings of loneliness as they missed social environments (e.g., work, church) and events (e.g., reunions, funerals, holidays). Patients who had struggled with trauma or mental health difficulties prior to cancer seemed particularly vulnerable.
Being away from my family. I went through so many tragedies in my [life] and already, I was going through depression because of the tragedies that I’ve been trying to overcome. This is just one more thing added to it. (patient 101)
FCs reported feeling overwhelmed and emotionally upset by the added responsibilities of caretaking and managing life at home. One participant said, “It’s very evident. It’s very emotionally draining, physically draining” (FC 105). Some examples included not wanting to leave the patient alone at the hospital, having to cancel trips, prioritizing the patient’s needs above their own, and balancing caregiving with other responsibilities. One participant noted, “I think the hardest part is the guilt of not being there” (FC 127). In addition, FCs reported that it was difficult to manage patients’ negative emotions and related behaviors such as lashing out or expressing lack of will to live, which in turn contributed to FCs’ sadness and distress.
[Patient’s] gotten to the point where, I guess it must be that his anxiety level is so high, he’s just acting nuts and that’s making it really hard for me too. He’s always either angry or everything annoys him. (FC 138)
Logistical Challenges
A few patient participants (n = 8) expressed concern over the logistics of their futures because of their current hospitalization, such as an inability to attend important events, delays returning to school or work, and management of child or pet care. Patients also indicated feelings of loneliness caused by the distance between the hospital and home, which limited the number and frequency of visitors.
I want to go home. This is the only area they have that treats my type of leukemia. So, I have to travel an hour and a half away to get treatment and I don’t even drive. I don’t know how this is all going to work out. (patient 116)
Logistical challenges were a far more active and significant challenge for the FC participants in this study (n = 20). FCs frequently needed to manage multiple roles such as FC, parent, employee, and student, and they reported difficulties balancing these roles while the patient was in the hospital. For example, many reported frustration with the travel back and forth to the hospital. This contributed to feeling the need to be in two places at once, because they were the main caregiver to the patient while also having home- and job-related responsibilities. One FC said, “I’m [at the hospital] every day and every night, so everything [at home] is just sitting there and I am running back and forth” (FC 105).
For patients and FCs with dependent children, parenting during HM treatment was challenging. In these instances, the patient and FC participants shared childcare challenges such as managing children’s schedules, aiding in school assignments, and navigating children’s understanding and emotional reactions to cancer.
Financial Impact
Both current (e.g., spending more money than usual on takeout food, gas, and medical expenses) and anticipated (e.g., job security, paying bills, making mortgage or rent, lapses in insurance coverage) financial impacts were reported by patient (n = 13) and FC (n = 10) participants. In many cases, the patient was the sole financial provider, which created unique challenges for the FC, as they were often forced to take on finance-related roles within their family unit. For example, FCs who did not work or had only worked part-time were now financially supporting their families.
I work part-time and [the patient] is the sole breadwinner, and insurance is through him, and I’ve got people saying, “You’re going to have to downsize and find a full-time job,” and I’m like . . . I just gotta get through today. (FC 139)
In addition, some FCs did not previously manage the finances and now needed to learn how to pay bills and perform other finance-related tasks, particularly in a remote environment (e.g., paying bills online). FCs reported feeling overwhelmed and concerned about paperwork related to patient care (e.g., social security, disability, Medicare) as they were limited in time and understanding of the process. According to one FC, “I’ve never paid the bills. I don’t even know where money is in our names. I’ve not even thought about it. He pays all bills autopay . . . I’m totally unprepared” (FC 108).
Discussion
Findings highlighted the individual experiences of patients with HM and their FCs. Although patients and FCs were interviewed separately, both groups shared many similar experiences pertaining to their healthcare experience, living conditions, and general well-being. These similarities, particularly the positive, may support the family’s healthy adaptation to the illness, because going through a shared experience brings people closer (Eggenberger & Nelms, 2007). However, stark differences in the impact of the disease were observed between the two groups in areas of emotional coping, housekeeping abilities, and preparedness, in which FCs shared more specific and overwhelming challenges. For example, because of the nature of the health event, the health and well-being of the patient was prioritized, while the FC had to make sacrifices and take on responsibilities that negatively affected their mental and physical health. This had the potential to create an imbalance in the relationship, influence interactions, and contribute to challenges that could undermine a healthy family adaptation to the illness (Ybema et al., 2002). Understanding the similar yet unique challenges that patients with HM and their FCs face during the initial diagnosis and treatment is important for current clinical care and developing future interventions to support family-centered care.
Quality of care and communication with the healthcare team were important factors that affected the participants’ experiences from diagnosis through treatment. For example, the patients with HM and their FCs reported less trust in the care they received when their primary care physician did not promptly diagnose or refer the patient to a specialist. The patients and FCs also reported feeling that they had lost time in this process, which increased the overall distress for all participants. A diagnosis of HM such as acute leukemia requires a complex and invasive diagnostic process. Sometimes the signs and symptoms are vague, and other times they are medical emergencies. Combined, these factors make diagnosis challenging for clinicians and upsetting for patients and families who are already distressed over a serious health concern (Danhauer et al., 2013; Kurtin, 2019). To ease this distress for patients and FCs, it would be beneficial for clinicians in all settings to apply patient-centered communication (Teutsch, 2003) with skilled interprofessional teams that include a care coordinator to facilitate diagnosis and transition to a tertiary cancer center, where treatment is most likely to occur.
In addition, the patients and FCs reported that hospital living conditions could be improved, particularly by allowing more opportunities to sleep. Sleep-related problems are common symptoms experienced by at least one-third of individuals with cancer and are nearly universal among individuals admitted to the hospital (DuBose & Hadi, 2016). Disturbed sleep negatively affects quality of life (Dahiya et al., 2013; Stepanski & Burgess, 2007) and contributes to immune system suppression (Theobald, 2004). Although patients indicated understanding that interrupted sleep was part of their care, limiting the number of unnecessary interruptions, including visits from housekeeping and clustering clinical care, could benefit patients. Negotiating or altering care delivery routines, such as delaying routine laboratory draws until after 5 am and limiting vital sign monitoring in stable patients for most of the late night and early morning hours, may be necessary. In addition, FCs may benefit from improved hospital conditions such as regularly accessible restrooms with showers. This could aid in alleviating FC burden in terms of logistics and financial resources associated with traveling back and forth to the hospital. This is important to consider because the FC assumes a significant amount of the home responsibilities. Reducing the stress and burden for FCs while they provide essential support to patients may mitigate additional distress for patients and their families.
Some of the most-discussed home stressors for the FCs in this study were increased financial and parenting responsibilities, most often reported by the female participants. Many FCs were limited in their knowledge of household finances and medical bills, and found navigating these fiscal matters stressful. Interventions aimed at increasing FCs’ financial literacy and assisting them in navigating the healthcare system could be valuable to patients and FCs. Ensuring access to interprofessional care coordination that includes nurse navigators and social workers early in the diagnostic process is an essential component for both the patient and FC (Kurtin, 2019). In addition to finances, parenting-related stressors such as scheduling children’s activities, disruptions to routine, access to child care, conversations about cancer, and division of parenting responsibilities were reported as being distressing for patients and FCs with children living at home. Many found this overwhelming, and it contributed to reduced self-care and heightened feelings of guilt when having to choose between being a FC to the patient with HM or being an active parent. Interventions aimed at supporting parents during cancer diagnosis and treatment would benefit the family unit.
Finally, cancer diagnosis and treatment can be traumatizing for patients and their FCs (Saeedi-Saedi et al., 2015). For example, one study suggested that the emotional toll (e.g., anxiety, depression) cancer evokes for the patient is associated with the emotional distress experienced by the FC (Tan et al., 2018). Both patients and FCs reported being in a state of constant ambiguity because of the volatility of the cancer diagnosis and treatment. They also expressed concern for each other’s well-being in terms of self-care, mental health, and patient survival (Tan et al., 2018). The FCs prioritized the needs of the patient above their own and paused their lives to be present for the patient. In addition, the HM diagnosis brought up memories of past traumas such as the death of a loved one for many participants. Patients and FCs reported reflecting on past losses, which increased their emotional distress and concern for the patient’s survival. Interventions aimed at managing distress, promoting psychological and physical health, and finding support could help attenuate patient and FC trauma and distress.
Several limitations of the study must be noted. The data were collected from patients and FCs within three months of diagnosis. Because this was within the induction period of treatment, the patient and FC were in an acute phase of the disease. Their interview responses were limited to the things they had experienced up to that point. Some challenges (e.g., medical bills, effects on employment, social and relationship effects) and disease stressors (e.g., secondary effects of treatments, relapsed or refractory disease) may not have been present yet. Finally, these findings are limited in their generalizability because of the limited study population (mostly White and diagnosed with acute leukemia).
Implications for Nursing
This work adds to the growing body of literature that helps clinicians understand the complex and multifaceted experience of newly diagnosed patients with HM and their FCs. Having a better comprehension of the patient and FC experiences allows clinicians to better tailor clinical encounters to support the needs of patients and their families. It also provides information for researchers to develop tailored patient- and family-centered interventions aimed at filling voids in care from the time of diagnosis through the disease trajectory. Patients and families alike often need repeated interventions to educate them on their disease and its potential progression, particularly because of the labile symptoms experienced by many individuals with an HM diagnosis. This will also allow for the development of rapport and trust with the care team regarding care delivery, which will improve patients’ and FCs’ experience with the healthcare system.
Nursing has an important role in navigation and care coordination. The interprofessional team, including physical therapy, rehabilitation, social work, and other key specialties such as palliative care, also provide valuable resources and support to patients with HM and their families. The development of tailored nursing interventions that target psychosocial support would be beneficial for patients and FCs alike.

Conclusion
The findings from this study contribute to an understanding of the complex effects of an HM diagnosis on patients and their FCs. Findings from this study can help guide the patient-focused and family-centered care provided by hematology-oncology clinicians. The challenges experienced by patients and FCs in this population suggest that not only the patient, but also the FC, would likely benefit from early palliative care referrals. In addition, these findings can inform future interventions aimed at FC role preparation, patient and FC burden prevention, and mental health care for patients and FCs. Ultimately, the findings from this study support the need for tailored supportive care interventions that foster positive adjustment and health outcomes for both patients and their FCs.
About the Authors
Rebecca Hoppe, MS, is a doctoral student, and Marcia A. Winter, PhD, is an associate professor, both at Virginia Commonwealth University in Richmond; Katherine Graap, BSN, RN, OCN®, is a nurse practitioner student in Adult-Gerontology, and Tara A. Albrecht, PhD, ACNP-BC, ACHPN®, RN, is an assistant professor in the School of Nursing, both at Duke University in Durham, NC. Parts of this study were funded by the VCU Massey Cancer Center Tina L. Bachas Nursing Award Program and the Susan White Holsworth Palliative Care Scholar funds. Hoppe, Winter, and Albrecht contributed to the conceptualization and design. Hoppe and Winter completed the data collection. Hoppe provided statistical support. All authors provided the analysis and contributed to the manuscript preparation.Winter can be reached at mawinter@vcu.edu, with copy to ONFEditor@ons.org. (Submitted August 2021. Accepted February 12, 2022.)
References
Adelman, R.D., Tmanova, L.L., Delgado, D., Dion, S., & Lachs, M.S. (2014). Caregiver burden: A clinical review. JAMA, 311(10), 1052–1060. https://doi.org/10.1001/jama.2014.304
Albrecht T.A. (2014). Physiologic and psychological symptoms experienced by adults with acute leukemia: An integrative literature review. Oncology Nursing Forum, 41(3), 286–295. https://doi.org/10.1188/14.ONF.286-295
Albrecht, T.A., Boyiadzis, M., Elswick, R.K., Jr., Starkweather, A., & Rosenzweig, M. (2017). Symptom management and psychosocial needs of adults with acute myeloid leukemia during induction treatment: A pilot study. Cancer Nursing, 40(6), E31–E38. https://doi.org/10.1097/NCC.0000000000000428
Applebaum, A.J., Bevans, M., Son, T., Evans, K., Hernandez, M., Giralt, S., & DuHamel, K. (2016). A scoping review of caregiver burden during allogeneic HSCT: Lessons learned and future directions. Bone Marrow Transplantation, 51(11), 1416–1422. https://doi.org/10.1038/bmt.2016.164
Carlson, L.E., Angen, M., Cullum, J., Goodey, E., Koopmans, J., Lamont, L., . . . Bultz, B.D. (2004). High levels of untreated distress and fatigue in cancer patients. British Journal of Cancer, 90(12), 2297–2304. https://doi.org/10.1038/sj.bjc.6601887
Carr, A. (2015). The evolution of systems theory. In T.L. Sexton & J. Lebow (Eds.), Handbook of family therapy: The science and practice of working with families and couples (pp. 13–29). Routledge. https://doi.org/10.4324/9780203123584-2
Dahiya, S., Ahluwalia, M.S., & Walia, H.K. (2013). Sleep disturbances in cancer patients: Underrecognized and undertreated. Cleveland Clinic Journal of Medicine, 80(11), 722–732. https://doi.org/10.3949/ccjm.80a.12170
Danhauer, S.C., Russell, G.B., Tedeschi, R.G., Jesse, M.T., Vishnevsky, T., Daley, K., . . . Powell, B.L. (2013). A longitudinal investigation of posttraumatic growth in adult patients undergoing treatment for acute leukemia. Journal of Clinical Psychology in Medical Settings, 20(1), 13–24. https://doi.org/10.1007/s10880-012-9304-5
DuBose, J.R., & Hadi, K. (2016). Improving inpatient environments to support patient sleep. International Journal for Quality in Health Care, 28(5), 540–553. https://doi.org/10.1093/intqhc/mzw079
Eggenberger, S.K., & Nelms, T.P. (2007). Being family: The family experience when an adult member is hospitalized with a critical illness. Journal of Clinical Nursing, 16(9), 1618–1628. https://doi.org/10.1111/j.1365-2702.2007.01659.x
Fife, B.L., Monahan, P.O., Abonour, R., Wood, L.L., & Stump, T.E. (2009). Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplantation, 43(12), 959–966. https://doi.org/10.1038/bmt.2008.405
Frambes, D., Given, B., Lehto, R., Sikorskii, A., & Wyatt, G. (2018). Informal caregivers of cancer patients: Review of interventions, care activities, and outcomes. Western Journal of Nursing Research, 40(7), 1069–1097. https://doi.org/10.1177/0193945917699364
Kent, E.E., Rowland, J.H., Northouse, L., Litzelman, K., Chou, W.-Y.S., Shelburne, N., . . . Huss, K. (2016). Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer, 122(13), 1987–1995. https://doi.org/10.1002/cncr.29939
Klepin, H.D., Tooze, J.A., Pardee, T.S., Ellis, L.R., Berenzon, D., Mihalko, S.L., . . . Kritchevsky, S.B. (2016). Effect of intensive chemotherapy on physical, cognitive, and emotional health of older adults with acute myeloid leukemia. Journal of the American Geriatrics Society, 64(10), 1988–1995. https://doi.org/10.1111/jgs.14301
Kurtin, S. (2019). Interdisciplinary management of acute leukemia across the continuum of care. Seminars in Oncology Nursing, 35(6), 150953. https://doi.org/10.1016/j.soncn.2019.150953
Leak Bryant, A., Lee Walton, A., Shaw-Kokot, J., Mayer, D.K., & Reeve, B.B. (2015). Patient-reported symptoms and quality of life in adults with acute leukemia: A systematic review. Oncology Nursing Forum, 42(2), E91–E101. https://doi.org/10.1188/15.ONF.E91-E101
LeBlanc, T.W., Smith, J.M., & Currow, D.C. (2015). Symptom burden of haematological malignancies as death approaches in a community palliative care service: A retrospective cohort study of a consecutive case series. Lancet Haematology, 2(8), 334–338. https://doi.org/10.1016/s2352-3026(15)00111-8
Lincoln, Y., & Guba, E.G. (1985). Naturalistic inquiry. SAGE Publications.
Manitta, V., Zordan, R., Cole-Sinclair, M., Nandurkar, H., & Philip, J. (2011). The symptom burden of patients with hematological malignancy: A cross-sectional observational study. Journal of Pain and Symptom Management, 42(3), 432–442. https://doi.org/10.1016/j.jpainsymman.2010.12.008
Pressler, S.J., Gradus-Pizlo, I., Chubinski, S.D., Smith, G., Wheeler, S., Sloan, R., & Jung, M. (2013). Family caregivers of patients with heart failure: A longitudinal study. Journal of Cardiovascular Nursing, 28(5), 417–428. https://doi.org/10.1097/JCN.0b013e3182563877
Saeedi-Saedi, H., Shahidsales, S., Koochak-Pour, M., Sabahi, E., & Moridi, I. (2015). Evaluation of emotional distress in breast cancer patients. Iranian Journal of Cancer Prevention, 8(1), 36–41.
Sandelowski, M. (2010). What’s in a name? Qualitative description revisited. Research in Nursing & Health, 33(1), 77–84. https://doi.org/10.1002/nur.20362
Saunders, M.M. (2008). Factors associated with caregiver burden in heart failure family caregivers. Western Journal of Nursing Research, 30(8), 943–959. https://doi.org/10.1177/0193945908319990
Stepanski, E.J., & Burgess, H.J. (2007). Sleep and cancer. Sleep Medicine Clinics, 2(1), 67–75. https://doi.org/10.1016/j.jsmc.2006.11.011
Tan, J.-Y., Molassiotis, A., Lloyd-Williams, M., & Yorke, J. (2018). Burden, emotional distress and quality of life among informal caregivers of lung cancer patients: An exploratory study. European Journal of Cancer Care, 27(1), e12691. https://doi.org/10.1111/ecc.12691
Teutsch, C. (2003). Patient-doctor communication. The Medical Clinics of North America, 87(5), 1115–1145. https://doi.org/10.1016/s0025-7125(03)00066-x
Theobald, D.E. (2004). Cancer pain, fatigue, distress, and insomnia in cancer patients. Clinical Cornerstone, 6(1, Suppl. D), S15–S21. https://doi.org/10.1016/S1098-3597(05)80003-1
Williams, A. (2018). Family caregivers to adults with cancer: The consequences of caring. In U. Goerling & A. Mehnert (Eds.) Psycho-Oncology: Recent results in cancer research (Vol. 210, pp. 87–103). Springer, Cham. https://doi.org/10.1007/978-3-319-64310-6_6
Wright, L.M., & Leahey, M. (2005). Nurses and families: A guide to family assessment and intervention (4th ed.) F.A. Davis Company.
Ybema, J.F., Kuijer, R.G., Hagedoorn, M., & Buunk, B.P. (2002). Caregiver burnout among intimate partners of patients with a severe illness: An equity perspective. Personal Relationships, 9(1), 73–88. https://doi.org/10.1111/1475-6811.00005



