Update to 2019–2022 ONS Research Agenda: Rapid Review to Address Structural Racism and Health Inequities
Purpose: The Oncology Nursing Society (ONS) formed a team to develop a necessary expansion of the 2019–2022 ONS Research Agenda, with a focus on racism and cancer care disparities.
Methods: A multimethod consensus-building approach was used to develop and refine the research priorities. A panel of oncology nurse scientists and equity scholars with expertise in health disparities conducted a rapid review of the literature, consulted with experts and oncology nurses, and reviewed priorities from funding agencies.
Results: Critical gaps in the literature were identified and used to develop priority areas for oncology nursing research, practice, and workforce development.
Synthesis: This is the first article in a two-part series that discusses structural racism and health inequities within oncology nursing. In this article, three priority areas for oncology nursing research are presented; in the second article, strategies to improve cancer disparities and equity and diversity in the oncology workforce are described.
Implications for Research: Research priorities are presented to inform future research that will provide methods and tools to increase health equity and reduce structural racism in oncology nursing practice, research, education, policy, and advocacy.
Jump to a section
The goal of this article is to use the rapid review methodology (Hamel et al., 2021) to disseminate research priorities to guide future oncology nursing scholarship, research, education, practice, healthcare policy, and advocacy related to racism and cancer care disparities. The resulting priorities, which supplement the 2019–2022 Oncology Nursing Society (ONS) Research Agenda (Von Ah et al., 2019), introduce research priorities for knowledge discovery, translational research, and policy analysis. ONS, during its 40-plus–year history, has been committed to providing oncology nurses—practitioners, educators, scientists, and other oncology partners—with evidence-based, practical, and educational resources to grow and strengthen the science of nursing and improve cancer care outcomes. This dedication is explicitly stated in the ONS mission to promote excellence in oncology nursing and quality cancer care and the organization’s vision to lead the transformation of cancer care. For the past 19 years, nursing has been ranked as the most trusted and ethical profession in the United States (Nurse.org, 2021). Combining this distinction with ONS’s history of promoting excellence and transformation, ONS is uniquely situated to address racism in cancer care.
Background
ONS is reaffirming its commitment to creating and sustaining a culture of diversity, equity, and inclusion in oncology nursing science. Acknowledging that historical initiatives are not enough, ONS recognizes the need for intentional strategies to mitigate gaps in racial and health inequities. There is a critical need to understand and address the immediate and cumulative effects of structural racism in oncology on patients, the workforce, educators, and nurse scientists. Traditionally, ONS has identified and disseminated contemporary research priorities needed to advance cancer care. These research priorities provide a focus for oncology nurses’ research, scholarship, leadership, and health policy efforts to advance quality cancer care. ONS’s 2019–2022 research priorities identify health disparities as one of the three overarching priority areas, specifically calling for research to focus on the following: (a) improved representation in clinical trials, (b) social determinants of health, and (c) the use of technology and telehealth to improve access to care. Informed by evolving understandings of how structural racism leads to health disparities, as evident in the disproportionate impact COVID-19 has on communities of color and the widespread outcry in 2020–2021 for racial equity that followed the murders of George Floyd, Breonna Taylor, Ahmaud Arbery, and many other people of color who continue to be victimized, ONS’s 2019–2022 research priorities are being expanded, and additional research needs focused on the role of structural racism on health inequities in oncology are identified in this article.
Methods
A multimethod consensus-building approach was used to identify research priorities related to racism, inclusivity, and health equity in every aspect of cancer care. The rapid response approach (Hamel et al., 2021) was chosen to update the 2019–2022 research priorities; it was essential for ONS to have a dynamic process in place to ensure that the ONS Research Agenda keeps pace with contemporary research issues that often arise in a rapidly changing scientific landscape (Von Ah et al., 2019).
A diverse rapid response research team (RRRT) of oncology nurse scientists and equity scholars (the authors of the current article) was assembled in June 2020. The RRRT’s process was informed, in part, by critical race theory (CRT) (Delgado & Stefancic, 2012). CRT is a methodology that originated in legal studies and is now used to guide researchers of health disparities (Ford & Airhihenbuwa, 2010). CRT explains that racism is a deeply embedded and integral part of society; therefore, it is necessary for health disparities research to be grounded in the experiences of marginalized populations and to use community-engaged approaches, and for researchers to employ critical self-reflection (Ford & Airhihenbuwa, 2010).
Guided by CRT, the RRRT first reviewed and discussed the history and current pervasiveness of racism in nursing and oncology. The RRRT discussed the nature of racism in ordinary life and explored their personal race consciousness as oncology nurse scientists, academics, and humans. Next, multiple RRRT discussions ensued to “center the margins” (Ford & Airhihenbuwa, 2010), in which the researchers listened to and shared either their personal experiences as nurses of color and/or as health disparities researchers in oncology nursing science. These discussions were informed by rapid reviews of the literature. A rapid review is a methodology in which a synthesis of knowledge is conducted to obtain information in a timely manner, whereas the process of a traditional systematic review may be streamlined (Hamel et al., 2021). The RRRT conducted searches in CINAHL®, MEDLINE®, and PubMed® using search terms related to cancer, disparities, racism, nursing, and underrepresented minority and historically marginalized populations. Relevant literature reviews and seminal works published at any time, but primarily from 2015 to 2021, were reviewed and synthesized by the team to generate an initial list of potential research priorities. As additional relevant articles were published, they were added to the body of literature throughout the team’s synthesis process. Ultimately, more than 200 articles were reviewed by the team and then discussed to identify overall gaps and research priorities.
The list of potential research priorities was sent via an anonymous electronic survey to nurse researchers from across the country, representatives from funding agencies, and ONS membership. The survey was disseminated using a multiuse URL to quickly gather information from a broad audience; consequently, a response rate could not be determined because a final number of survey recipients was not recorded and the number of survey recipients was unknown. In addition, because the focus was quickly gaining input from a broad audience, a formal survey that assessed detailed demographics of recipients was not employed. Determined by self-report of categorical response options, respondents (N = 35) ranged in age from 30 years to older than 69 years; had worked from 1 to more than 30 years in nursing; were 90% female; and were 68% White, 20% Black/African American, and 3% Asian, with 9% of respondents checking “other” in terms of race/ethnicity. Respondents were asked to respond within one week to endorse the priorities that represented the most important topics needed to advance oncology nursing science related to addressing racism, inclusiveness, and health equity in cancer care. Respondents could also suggest additional priorities. The RRRT reviewed response data to refine the potential priority list and solicit written and verbal feedback from a COVID-19 RRRT (Zanville et al., 2021), ONS leadership, and the ONS Board of Directors, using an iterative process to determine the final research priorities presented in this article.
Results
Key Concepts
Terminology: The lexicon used around race and ethnicity is important and nuanced, requiring continued learning and thoughtful attention. Several high-impact journals have attempted to provide scientific authors with best practices around reporting race and ethnicity in publications, offering helpful suggestions while recognizing no finite conclusions (Boyd et al., 2020; Flanagin et al., 2021). The authors of the current article recognize that accurate terminology is important and variable depending on numerous factors, including setting; individual, geographic, and generational preferences; and how the meaning ascribed to words changes over time. Terms related to race and ethnicity in this article are intentional and have been carefully selected based on the aforementioned publications and factors, combined with extensive dialogue about divergent personal preferences and opinions of specific terms within the authorship team.
“People of color” is used in this article to refer to African Americans, Asian Americans, Native Americans, Pacific Islander Americans, multicultural Americans, Latino Americans, and any individuals who are not White, in acknowledgment of historical and current White centering and superiority that has created systemic racism, in which the White race benefits the most. In addition, “people of color” is used only when the authors acknowledge a common experience or phenomenon that exists among people of color that is different as compared to that of White people. “People of color” is not used in this article for convenience or simplicity. “Black, Indigenous, and people of color,” or “BIPOC,” is not used because of sensitivities and controversies around if and how “BIPOC” brings forth the unique marginalization and violence that has been inflicted specifically on Black and Indigenous people in comparison to other people of color. “Minority” is not used because it means “less than” and is often inappropriately used to refer to people of color for convenience or when they are not, in fact, respectively underrepresented (Williams, 2020). For example, it is inappropriate to refer to a study sample as 60% minority when 60% of participants were Black and 40% were White; in this study, the Black participants are not underrepresented. In addition, Black, Brown, and Indigenous people are numerically the global majority (Lee et al., 2021).
“Underrepresented minority” is used only when a referenced group is indeed statistically proportionally underrepresented in the respective referenced circumstance. “Caucasian” is not used because the inception of this word is debated to be tied to ideals of White superiority described in the first recorded written definitions of racial categories by Johann Friedrich Blumenbach in the 1700s (Michael, 2017; Rambachan, 2018).
In every circumstance, the most specific and accurate terminology possible is used to describe exactly the people who are being referenced. For example, “Black” is not blanketly used in place of “African American” for simplicity; “African American” is used when the authors are specifically referring to Black people of African descent. When citing specific statistics or publications, the terms reported in the respective publication are used. The authors wish to acknowledge that some readers’ personal experiences, beliefs, and practices will conflict with terminology used in this article and that the authors’ use of terminology is expected to be malleable to time and context. Therefore, the authors recommend and personally commit to paying continued attention to the meaning and impact of language, using specific words to describe who they are referring to, and adapting word usage over time, as appropriate.
Race and racism: An understanding of how structural racism has led to inequities in cancer occurrence and treatment among people of color is needed before sustainable and substantive changes can be made to rectify the aforementioned inequities. This article, therefore, includes a review of the impact of race and racism in oncology and nursing, as well as the need for related research, beginning with the words “race” and “racism.”
The term “race,” first recorded in the mid- to late 1500s, is often related to the phenotypical traits of an individual, such as skin color or facial features. Race is often mentioned with but should not be confused with the term “ethnicity,” which is defined as a social construct that refers to having cultural commonalities, such as language, religion, and cultural traditions (Ford & Kelly, 2005; LaVeist, 1994). Ethnicity and culture can vary greatly among individuals who are assigned to the same race. Race, as further differentiated from ethnicity, is a social construct that elicits certain social attitudes and perceptions toward a group of people; these perceptions are referred to as racism (Blank et al., 2004). However, others have argued that the separation of race and ethnicity is arbitrary and that race/ethnicity should be considered as one variable (Flanagin et al., 2021).
There are many forms of racism. Often, racism has been thought of as personally mediated or interpersonal, which refers to intentional or unintentional discrimination, prejudice, and differential actions toward a person, based on their race (Jones, 2000). Although all forms of racism are damaging, particularly problematic is structural racism, because it is a fundamental cause of numerous health disparities in the United States (Borrell et al., 2021; Churchwell et al., 2020). Structural racism, also termed systemic or institutionalized racism, refers to normative and often legal disparities, by race, in access to goods, services, and opportunities. These differences then perpetuate an inherent advantage for privileged groups and a disadvantage for marginalized groups (DiAngelo, 2012; Jones, 2000). Structural racism often operates as inaction, with no identifiable actor. It manifests as deeply embedded operational and organizational processes and procedures within a range of mutually reinforcing systems, including education, health care, social services, criminal justice, employment, income, home ownership, and wealth, that can result in health inequities (Bailey et al., 2017; Gkiouleka et al., 2018; Krieger, 2012).
Cancer disparities: Documentation of oncology epidemiology began in the 1920s, when cancer was believed to be a disease of educated, middle- and upper-class White people and it was thought that people of color were immune due to a “primitive nature” (p. 5) and life spans too short to reach the so-called “cancer age” (p. 2) (Wailoo, 2011). These unfounded theories contributed to the exclusion of people of color in early cancer research and contribute to the lack of applicability of such research today. It is evident that institutional racist structures have affected health research, including oncology research (Karamanou et al., 2016).
Today, people of color, particularly Black and African Americans, face a number of disparities related to cancer as compared to White Americans. For example, Black/African American men are more likely to be diagnosed and die of prostate and colorectal cancer than any other racial/ethnic group. Black/African American women are more likely to die of breast cancer and colorectal cancer compared to White women (National Cancer Institute Surveillance, Epidemiology, and End Results Program, n.d.). Black/African American men are twice as likely as White men to die of prostate cancer and have the highest prostate cancer mortality among all racial/ethnic groups (National Cancer Institute Surveillance, Epidemiology, and End Results Program, n.d.). Hispanic and Black/African American women have higher rates of cervical cancer as compared to women of other racial/ethnic groups, with Black/African American women having the highest rates of death from the disease. American Indians/Alaska Natives have higher death rates from kidney cancer than any other racial/ethnic group. American Indians/Alaska Natives have the highest rates of liver and intrahepatic bile duct cancer, followed by Hispanics/Latinxs and Asian/Pacific Islanders (National Cancer Institute Surveillance, Epidemiology, and End Results Program, n.d.). Because of structural racism, socioeconomics, and environmental factors, African Americans in particular are disadvantaged, and these factors affect their ability to receive timely and appropriate cancer prevention, detection, treatment, and survivorship measures (American Cancer Society, 2019).
Research Gaps
The literature reveals that mistrust, created by the individuals, structures, and systems of health care and research, is a well-documented barrier for people of color in clinical research (Hamel et al., 2016; Salman et al., 2016). Compounding this, medical research and experimentation has a history of mistreatment and violence against Black people in America that has not been addressed (Washington, 2006). For example, James Marion Sims is celebrated as the father of gynecology, despite his surgical experimentation on Black children without anesthesia (e.g., using cobbler’s tools to pry a baby’s skull bones into different positions, perfecting a surgery of abrading and suturing fistulas on Black girls) (Sims, 1884; Washington, 2006). As recently as 1961, Fannie Lou Hamer, one of many African American victims of involuntary sterilization, was told that a uterine tumor would be removed but received a hysterectomy instead (DeMuth, 1964; Hartmann, 1995). Horrific historical actions of White people created mistrust of the medical profession among people of color. This mistrust is perpetuated today through racist structures and systems that nurses must deconstruct. As a result, people of color, who may be among those in most urgent need of cancer care and resources, are the least likely to seek care and participate in clinical trials.
When people of color do seek medical care, they are treated in healthcare systems that were originally designed for White people, resulting in patients of color receiving information that is not tailored to them and having unmet needs (Asare et al., 2018; Haynes-Maslow et al., 2016; Lewis-Thames et al., 2020). Decades of advocacy focused exclusively on White individuals with cancer have created and perpetuated structural differences in awareness, access, funding, and research benefiting White people while excluding people of color (Wailoo, 2011). For example, most current and historical breast cancer research is focused primarily on estrogen-positive disease, which is more prevalent in White women, yet African American women are more commonly diagnosed with estrogen-negative disease (Feagin & Bennefield, 2014). Other instances of White-centric oncology studies include a lack of leukemia research involving Black children (Eche & Aronowitz, 2020); genomics research excluding racially and ethnically diverse samples (Spratt et al., 2016); and thyroid cancer research not addressing racial disparities because of a lack of inclusion and poor reporting of individual-level risk factors in racially and ethnically diverse individuals (Keane et al., 2017). Many of these disparities are related to underrepresentation of racially and ethnically diverse samples in clinical trials.
As cancer research has evolved to address disparities that exist between racial and ethnic groups, the experiences and perspectives of people of color remain limited. People of color remain underrepresented in cancer research (Nazha et al., 2019). Few cancer studies use true community-based participatory research (CBPR) methodology in which members of historically marginalized and underrepresented racial and ethnic communities are engaged in all facets of the research process, including performing a needs-based assessment, defining the problem, establishing the research questions and designing study methods with the needs and preferences of the community in mind, engaging participants, interpreting results in terms of the community’s perspectives, and disseminating the results of the research to all relevant members of the community—in short, centering the voices of community members in all phases of the research process (Kirk et al., 2017).
In summary, this rapid review identified several gaps in current oncology nursing research that need to be addressed, including the need to develop an understanding of how to (a) remove and replace the racist systems and structures that have created mistrust among communities of color, (b) conduct research that will effectively mitigate cancer disparities, and (c) engage more racially and ethnically representative communities in current medical research. To address these gaps, three priority areas for future research are presented, along with specific recommendations to achieve each.
Priority Area 1: Design and Test Studies That Restore Trust and Promote Inclusiveness in Cancer Research
Recommendation 1: Conduct Studies Informed by CRT
This priority expands recommendations related to diverse racial and ethnic research representation in the 2019–2022 ONS Research Agenda (Von Ah et al., 2019). Strategies to increase enrollment and retention of racially and ethnically diverse populations are essential to increasing the generalizability of research findings (Hamel et al., 2016; Rivers et al., 2019; Salman et al., 2016; Williams et al., 2019). Nurses must understand how they relate to people they include in research studies and have an understanding of populations’ histories. The American Academy of Nursing calls for this understanding to begin by incorporating CRT into nursing education (American Academy of Nursing Institute for Nursing Leadership, 2021). Again, CRT explains that racism is a deeply embedded part of society; therefore, it is necessary for health disparities research to be grounded in the experiences of marginalized populations and to use community-engaged approaches, as well as for researchers to employ critical self-reflection (Ford & Airhihenbuwa, 2010). This understanding is fundamental to nurses effectively building trust and conducting research that includes people of color.
In addition, when conducting research that includes people of color, scientists must take care not to ascribe homogeneity to all members of a large community. Rather, scientists must recognize key differences in the experiences and health among subgroups. For example, the experience of an American-born Black individual is likely to be substantively different than that of an African-born Black individual (Consedine et al., 2015); the same is likely, then, to be true of Black people from Latinx countries. It is critical to understand these differences, including geographic differences, within the United States. For example, Amuta-Jimenez, Smith, and Brown (2020) identified that the number of Black immigrant women is increasing in the United States and that they often are at increased risk for cancer disparities. Because of cultural differences between Black immigrant women and American-born Black women, an understanding unique to Black immigrant women is needed for their appropriate and effective inclusion in research (Amuta-Jimenez, Jacobs, & Smith, 2020; Amuta-Jimenez, Smith, & Brown, 2020).
Recommendation 2: Develop, Test, and Evaluate Interventions to Improve Bidirectional Communication and Shared Decision-Making
Shared decision-making has been highlighted by the Agency for Healthcare Research and Quality, the National Academy of Medicine, and the Patient Protection and Affordable Care Act as the gold standard for communicating health information between patient and provider (Hawley & Morris, 2017). Understanding and identifying complex barriers to effective communication between patient and provider can inform cancer clinical trial recruitment and retention models (Hamel et al., 2016; Salman et al., 2016). There is an inherent multifaceted complexity in developing and testing communication and shared decision-making interventions to promote participation in cancer clinical trials (Hawley & Morris, 2017; Salman et al., 2016; Wenzel et al., 2015). Interventions are needed to target factors that influence bidirectional communication, such as providers’ attitudes, bias, communication style, and consideration of patient preferences, as well as patients’ values, beliefs, fears, and literacy (Hamel et al., 2016; Hawley & Morris, 2017; Salman et al., 2016; Wenzel et al., 2015).
Priority Area 2: Design and Test Studies Focused on the Impact of Social Determinants of Health on Cancer Disparities
Recommendation 1: Design and Test Multilevel Interventions That Target Social Determinants of Health
This recommendation expands those related to studying social determinants of health in the 2019–2022 ONS Research Agenda (Von Ah et al., 2019). Social determinants of health refer to access to health services, environments (physical and social), and economic and political structures (Solar & Irwin, 2010). Mid- and downstream social determinants of health refer to factors such as education and neighborhood safety. Relationships between these factors and health outcomes are well established. Future research is needed to determine how upstream social determinants of health, such as policy, legislation, and governance, create structural challenges and barriers for patients with cancer to receive optimal prevention and treatment outcomes (Solar & Irwin, 2010). Golden & Wendel (2020) note that attempts to add social determinants of health into existing biomedical models of practice cannot generate effective interventions to decrease the impact of oppression and discrimination; such attempts may hinder the ability of new health concepts to develop and broaden. As a result, studies should be designed with a multilevel mechanism approach (structural, cultural, and individual) as opposed to with a single-mechanism focus, allowing for a better understanding of the intersecting factors (racism and discrimination) that influence health (Williams et al., 2019). The National Institute on Minority Health and Health Disparities (2017) Research Framework (see Table 1) provides a blueprint to guide researchers in conducting multilevel research; it specifies five domains of influence on health (i.e., biologic, behavioral, physical/built environment, sociocultural environment, and healthcare system) and four levels of influence on health (i.e., individual, interpersonal, community, and societal). 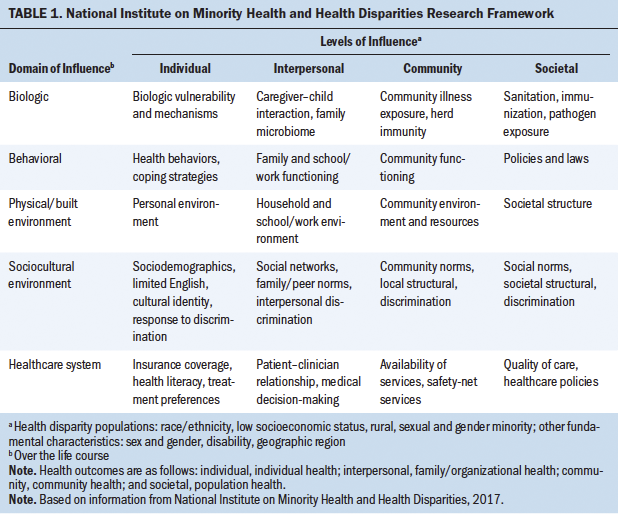
Recommendation 2: Focus Interventions That Target Modifiable Cancer Risk Factors on Addressing Social Determinants of Health
This priority expands recommendations related to modifiable behaviors (e.g., diet, physical activity) in the 2019–2022 ONS Research Agenda (Von Ah et al., 2019). Preventable and modifiable risk factors for cancer include first- and secondhand smoke, excess body weight, alcohol intake, high consumption of red and processed meat, high sodium intake, low consumption of fruits and vegetables, physical inactivity, ultraviolet radiation, and cancer-associated infections (e.g., Helicobacter pylori, hepatitis B and C, HIV, human papillomavirus [HPV]) (Islami et al., 2018). The lack of progress toward ameliorating inequity in cancer control has meant that, historically, behavioral health interventions have tended to focus on individual “problem” behaviors (e.g., failure to adhere to diet and exercise plans) rather than the reasons leading to the inability of people of color to engage in cancer prevention behaviors (Cogburn, 2019). Historically, people of color may have experienced factors such as lack of proximity and access to affordable fresh foods; lack of safe places to engage in physical activity; and White societal devaluation of their cultural, religious, and spiritual beliefs. For example, a need to focus on structural and societal, rather than individual, barriers has been identified to increase rates of HPV vaccination among people of color (Amboree & Darkoh, 2020). It has also been observed that factors known to influence physical activity are greater among Black survivors of breast cancer as compared to White survivors of breast cancer (Hirschey et al., 2018). These findings indicate a need for interventions focused on environmental and structural factors, such as bias in provider interactions; financial and food insecurity; and access to transportation, safe spaces for physical activity, and cancer screening.
Recommendation 3: Validate and Adopt Screening Measures to Assess Social Determinants of Health
Accurate and valid measurement of social determinants of health is critical in conducting such research. Scientists should leverage the PhenX Toolkit collection of measures to assess social determinants of health (Hamilton et al., 2011). The National Institute on Minority Health and Health Disparities (2020) has called for widespread adoption of PhenX as the standard assessment of social determinants of health in behavioral, clinical, and translational research. Adoption of standard measurement will facilitate analysis across studies, greater collaboration among scientists, and larger sample sizes to conduct assessments with greater statistical power through meta-analyses. Ultimately, these standard measures will increase understanding of how social determinants of health operate to affect health, allow scientists to test the mechanisms of impact in multilevel interventions, and provide a common language for the interpretation of results.
Importantly, race should be measured in disparities research as a social determinant of health. Race is a sociopolitical variable historically used to assign privilege, access, and power that operates daily as a social determinant of health (Bonham et al., 2018). Race must not be confused with genetics, which refers to the study of the composition of genes and variants within a person (Borrell et al., 2021). The Human Genome Project revealed no genetic basis of race and solidified that race should not be operationalized as a biologic variable (Boyd et al., 2020; Mohsen, 2020; Witherspoon et al., 2007). However, a few instances have been identified in which a genetic variant is more prevalent among people assigned to a certain race and associated with disease, warranting more frequent genetic testing. For example, the 8q24 variant associated with prostate cancer is more frequently present in Black men (Borrell et al., 2021). However, this does not mean that 8q24 is a “Black” variant. In fact, there can be more genetic variation among people assigned to the same race than between people assigned to difference races (Mohsen, 2020). It is essential that researchers understand the complex relationships between race and genetics, and then use the correct variable to explore a given research question (Borrell et al., 2021).
Priority Area 3: Design and Test Community-Based Cancer Prevention and Control Interventions
Recommendation 1: Evaluate Interventions Delivered in Collaboration With Communities
It is critical to form partnerships with community members who are familiar with the particular barriers and facilitators of health, as well as to identify and implement interventions aimed at structural barriers to care, such as access. Researchers can work with lay navigators and community health centers to increase the efficacy and sustainability of interventions. For example, in the 1990s, Harold Freeman founded a patient navigation model to decrease cancer disparities among poor and uninsured people by working with lay health navigators in Harlem to improve patient navigation and cancer screening (Freeman & Rodriguez, 2011). Partnerships with faith-based organizations have also proven successful for cancer education, prevention, screening, and early detection in Black communities (Heiney et al., 2016). Examples of community organizations that may be important clinical partners are included in Figure 1. 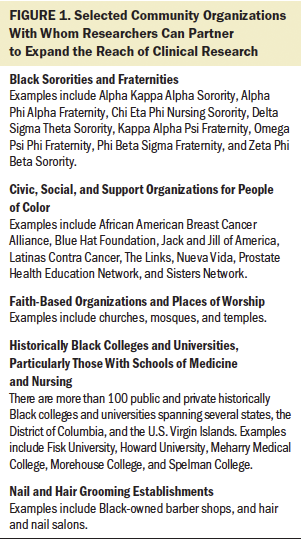
Recommendation 2: Identify and Intervene on Modifiable Barriers and Facilitators to the Adoption, Implementation, and Sustainability of Evidence-Based Interventions in Communities
Providing understandable and accessible knowledge of prevention strategies to all communities, particularly historically marginalized communities, should be a key strategy for community-based programs. For example, modifiable barriers to uptake of the HPV vaccine have been identified as not receiving provider recommendations, medical mistrust, inadequate knowledge and awareness, spiritual and religious beliefs, an external locus of healthcare control, and fear (Amboree & Darkoh, 2020; Lahijani et al., 2021). Consequently, implementation studies focused on factors such as improved provider communication, trust-building, and consideration of cultural beliefs are needed to improve the uptake of evidence-based intervention in historically marginalized and underserved communities.
Recommendation 3: Center the Experiences of Target Populations in the Design, Testing, Evaluation, and Dissemination of Research
Research should be guided by a socio-ecologic perspective that is focused on addressing the social and structural causes of poor health outcomes (American Academy of Nursing Institute for Nursing Leadership, 2021). Examples of theories that may guide such research include critical theory, hermeneutic theory, and design thinking (Golden & Wendel, 2020). Building partnerships among underserved and historically marginalized communities is integral to this research. Such research should be guided by CBPR approaches that follow the eight principles of CBPR. CBPR approaches include community members in the entire research process, from problem identification through dissemination of results to the community for whom the research was designed to benefit (Kirk et al., 2017). As a result, the experiences of those who are affected by health disparities are centered in research to create effective and sustainable interventions that build the capacity of communities to sustain the health of their members. Finally, research teams should be led by or, at minimum, include scientific investigators who personally identify with the racial and ethnic makeup of a respective research sample (Salman et al., 2016). Recommendations to increase the number of nurse scientists of color will be covered in depth in the second article of this two-part series (Jones et al., 2021). 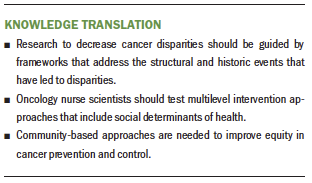
Limitations
The development of future research priorities can be strengthened by soliciting input from patients and community members when complex social issues, such as structural racism and equity, are being addressed. A lack of community engagement is a weakness in the development of these research priorities. An additional weakness of this work is that a multiuse URL was employed to distribute the electronic survey; as a result, it is not possible to determine how many surveys were sent or the response rate. Community engagement and more diverse perspectives can be better leveraged in the development of future research priorities through methods such as formal surveys, focus groups, and consultations from existing patient advisory councils and community advisory boards.
Conclusion
These priorities can be used as a blueprint for oncology nurse scientists, practitioners, and organizations to develop and test interventions. Of note, these scientific inquiries should be implemented through the lens of racial equity and inclusiveness. Multilevel approaches, guided by CRT, are needed to achieve equity in cancer care and mitigate cancer disparities. Accordingly, research findings may lead to the shifting of paradigms and the empowering of nurse scientists to deconstruct structural racism in oncology care and practice. Antiracism work to achieve health equity is forever ongoing and requires continual cultural sensitivity and personal education. These understandings can be strengthened through interprofessional partnerships with organizations who are also establishing commitments to antiracist frameworks and research, such as the American College of Physicians, American Heart Association, American Society of Clinical Oncology, Association of American Medical Colleges, and National Institutes of Health (Association of American Medical Colleges, n.d.; Churchwell et al., 2020; Collins, 2021; McMasters, 2021; Pierce, 2020; Serchen et al., 2020).
Policy change is needed to support the conduct and dissemination of research to mitigate structural racism and achieve health equity in oncology nursing. Nursing journals should implement author and reviewer guidelines that ensure that all manuscripts are sensitive to racism (Boyd et al., 2020; Flanagin et al., 2021). For example, when reporting participant demographics, “White” should not be used as a normative value. In addition, oncology nursing should continue to develop, with researchers applying for funding for cancer disparities research, such as the Oncology Nursing Foundation RE42 research grant. A meaningful change in the conduct and impact of oncology nursing research on racism and health inequities needs to be supported by improved racial and ethnic representation and sensitivity in the oncology nursing workforce, which will be addressed in the second article of this two-part series (Jones et al., 2021).
About the Author(s)
Randy A. Jones, PhD, RN, FAAN, is a professor in the School of Nursing at the University of Virginia (UVA) and the assistant director of community outreach and engagement at the UVA Emily Couric Cancer Center, both in Charlottesville; Rachel Hirschey, PhD, RN, is an assistant professor in the School of Nursing at the University of North Carolina at Chapel Hill and an associate member of the Lineberger Comprehensive Cancer Center in Durham, NC; Grace Campbell, PhD, MSW, RN, CNL, CRRN, FARN, is an assistant professor in the School of Nursing at Duquesne University and an adjunct assistant professor in the Department of Obstetrics, Gynecology, and Reproductive Sciences in the School of Medicine at the University of Pittsburgh, both in Pittsburgh, PA; Mary E. Cooley, PhD, RN, FAAN, is a lecturer in psychiatry at Harvard Medical School and a nurse scientist in Nursing and Patient Care at the Dana-Farber Cancer Institute, both in Boston, MA; Robin Lally, PhD, RN, AOCN®, FAAN, is the interim associate dean for research and the Bertha L. Pankratz Professor of Nursing in the College of Nursing at the University of Nebraska Medical Center and a member at the Fred and Pamela Buffett Cancer Center, both in Omaha, NE; Darryl Somayaji, PhD, MSN, CNS, CCRC, is an assistant professor in the School of Nursing at the University at Buffalo and an adjunct assistant professor of oncology at Roswell Park Comprehensive Cancer Center, both in Buffalo, NY; Erik K. Rueter, PMP, PMI-ACP, was, at the time of this writing, a project manager at the Oncology Nursing Society in Pittsburgh, PA; and Mary Magee Gullatte, PhD, RN, ANP-BC, AOCN®, LSSYB, FAAN, is the corporate director of nursing evidence-based practice and research at Emory Healthcare and an adjunct faculty member at the Nell Hodgson Woodruff School of Nursing at Emory University, both in Atlanta, GA. This review was funded, in part, by a grant from the National Institute on Minority Health and Health Disparities (1K23MD015719-01; principal investigator: Hirschey). Jones, Hirschey, Campbell, Cooley, Somayaji, Rueter, and Gullatte contributed to the conceptualization and design. Jones, Hirschey, Campbell, Cooley, Lally, and Somayaji completed the data collection. Hirschey, Campbell, Somayaji, and Rueter provided the analysis. All authors contributed to the manuscript preparation. Jones and Hirschey are dual first authors. Rueter and Gullatte are dual senior authors. Hirschey can be reached at hirschey@unc.edu, with copy to ONFEditor@ons.org. (Submitted February 2021. Accepted June 28, 2021.)

