Unintended Pregnancy: A Systematic Review of Contraception Use and Counseling in Women With Cancer
Background: Women with past or current cancer diagnoses can benefit from planning pregnancies to optimize maternal health and birth outcomes.
Objectives: The purpose of this systematic review is to identify unmet needs for family planning services among women with cancer by describing the prevalence of contraception counseling, contraception use, unintended pregnancy, and abortion.
Methods: Using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, 16 studies were included.
Findings: Women with cancer experience unintended pregnancy and abortion throughout their care. Not all women reported receiving contraception counseling, and many reported inconsistencies between contraception counseling desired and received. A prominent theme was uncertainty about fertility status. Use of highly effective contraceptive methods was low to moderate in eight patient populations.
Jump to a section
Unintended pregnancy can disrupt treatment and recovery for women of reproductive age with cancer. About 13% of all cancers occur in people aged younger than 50 years (American Cancer Society, 2017). Although some cancers and treatments impair fertility, many women with cancer are physically capable of conceiving. Cancer- and treatment-associated risks during pregnancy may be avoided by delaying pregnancy until treatment is complete and the woman is in remission (Laurence, Gbolade, Morgan, & Glaser, 2004; Royal College of Obstetricians and Gynecologists, 2011). Because unintended pregnancies, including unwanted pregnancies and those occurring sooner than desired, account for about 45% of all pregnancies in the United States (Finer & Zolna, 2016), investigating unintended pregnancy is imperative among patient populations at heightened risk for health complications. Little is known about unintended pregnancy, abortion, contraception use, and contraception counseling in the context of cancer care.
Describing the prevalence of contraception counseling, contraception use, abortion, and unplanned pregnancy will clarify unmet family-planning needs among women with cancer. Identifying patient preferences about contraception services is key to delivering evidence-based, patient-centered care (Patient-Centered Outcomes Research Institute, 2013; Spring, 2007). This review investigates the experiences and perspectives of women with cancer (referring to cisgender women with a current or past cancer diagnosis in childhood or adulthood) relating to pregnancy prevention during the cancer care continuum (encompassing diagnosis, treatment, and survivorship) (Taplin et al., 2012). The review addresses the following research questions:
• How prevalent are unintended pregnancy and abortion among women with cancer?
• What are the clinical needs and preferences of women with cancer related to contraception counseling?
• What contraception methods are women using across the cancer care continuum?
Methods
PubMed and CINAHL® were searched for English-language, peer-reviewed articles published in a 15-year span from January 1, 2000, to October 1, 2015. MeSH (medical subject heading) terms were used in PubMed. Search strings were: (“Neoplasms”[MeSH] or cancer or neoplasm) AND (“Contraception”[MeSH]) AND (patient OR patients OR survivor OR survivors OR survivorship) OR (“Pregnancy, Unwanted”[MeSH] or “unwanted pregnancy”) OR (“Pregnancy, Unplanned”[MeSH] or “unplanned pregnancy” or “mistimed pregnancy” or “unintended pregnancy”) OR (pregnancy or pregnant) OR (“Reproductive Health”[MeSH]) OR (“Family Planning Services”[MeSH]) OR “sexual health”). The computerized search was supplemented by hand searches of the reference lists of articles included in the review. After titles and abstracts were selected, full-text articles were reviewed. Inclusion criteria were (a) quantitative and qualitative empirical findings about contraception use, contraception counseling, unintended pregnancy, or induced abortion; (b) sample containing adolescent and premenopausal adult women capable of getting pregnant who were not seeking pregnancy; and (c) sample containing women with past and current cancer diagnosis, including adult and childhood cancers. Reviews, case reports, opinions, guidelines, commentaries, or abstracts of conference presentations were excluded. Reports were excluded if they exclusively described infertility, fertility preservation, sexuality, sexual function, sexual desire, or sexually transmitted infections, which were outside the scope of this review.
No articles were excluded based on quality because the purpose of the study was to describe the state of the science. However, quality and validity considerations are presented by weighing the generalizability and credibility of each study’s findings. Results were synthesized by organizing findings in a table, performing thematic analysis, and evaluating patterns across reports. Variation in study design, outcomes collected, and populations sampled precluded meta-analysis, requiring a narrative synthesis approach.
[[{"type":"media","view_mode":"media_original","fid":"31126","attributes":{"alt":"","class":"media-image","height":"426","typeof":"foaf:Image","width":"749"}}]]
Results
The search strategy produced 657 articles, of which 228 were duplicates and 429 were unique. After titles and abstracts were reviewed, 42 articles remained eligible. The full text of the 42 remaining articles was screened. Twenty-six records were excluded because they were not empirical work; they did not include women with cancer of reproductive age; or they did not discuss contraception, contraception counseling, unintended pregnancy, or abortion. Sixteen articles were eligible for inclusion. Tables 1 and 2 describe the studies and aspects of their design that may affect quality and validity. Cancer registries from which participants were sampled are summarized in Figure 1. 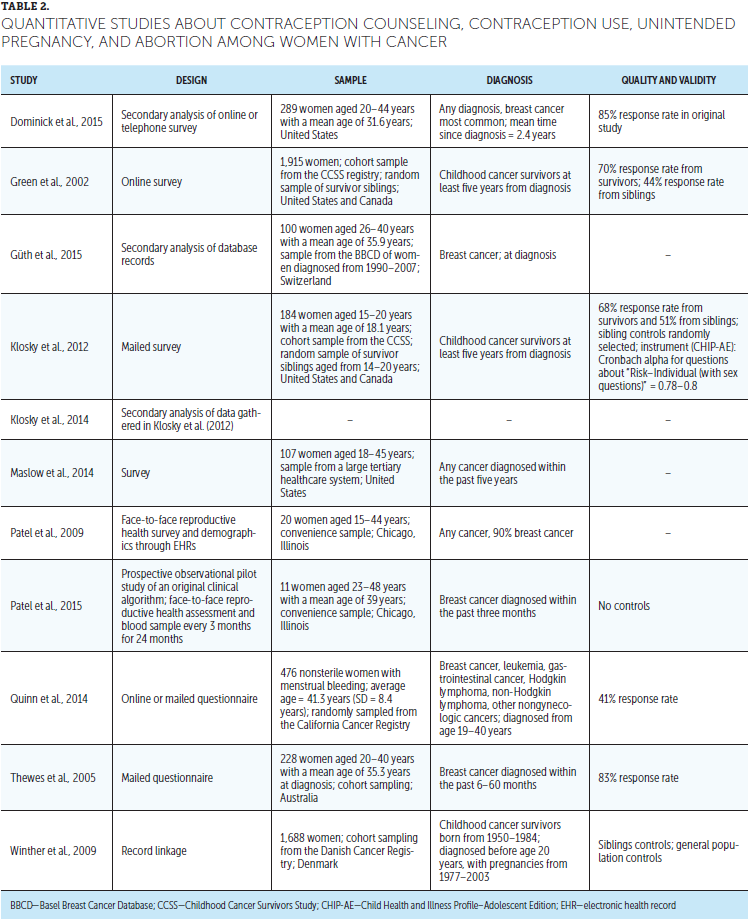
Prevalence of Unintended Pregnancy and Abortion
No studies captured the overall rate of unintended pregnancy or abortion among women with cancer. Five studies documented the occurrence of unintended pregnancies throughout the cancer care continuum, from cancer diagnosis to the end of treatment (Güth, Huang, Bitzer, Tirri, & Moffat, 2015; Patel et al., 2015), in the years following diagnosis with cancer (Connell, Patterson, & Newman, 2006; Dominick et al., 2015), and five years after diagnosis (Zebrack, Casillas, Nohr, Adams, & Zeltzer, 2004).
[[{"type":"media","view_mode":"media_original","fid":"31131","attributes":{"alt":"","class":"media-image","height":"655","typeof":"foaf:Image","width":"364"}}]]
Rates of abortion among cancer survivors were compared to healthy control groups in two studies, which demonstrated different patterns of abortion use in American and Danish samples. In an American study, 17% of 4,029 pregnancies reported by 1,915 survivors of childhood cancer ended in abortion, and cancer survivors had abortions at higher rates than healthy siblings (Green et al., 2002). Conversely, in a Danish study, the percentage of pregnancies that ended with abortions was similar among cancer survivors (20%), their healthy siblings (19%), and the general population of Denmark (20%) (Winther, Boice, Svendsen, Frederiksen, & Olsen, 2009). In addition, both studies noted exceptions to the overall patterns. In the United States, survivors of non-Hodgkin lymphoma had fewer abortions than their siblings, and, in Denmark, survivors of bone cancer had more abortions than their healthy siblings and the general population. Explaining those trends was outside the scope of both studies. In the Danish study, more than 92% of abortions occurred in the first trimester, and the small percentage of second-trimester abortions was attributed to maternal or fetal health indications by the similar percentages of cancer survivors, sibling controls, and population controls.
Women with cancer discussed their perspectives on abortion in four studies. In a sample of Turkish women diagnosed with breast cancer in the past year, the majority said they would have an abortion if they became pregnant, but a minority said their religious views precluded termination (Karaöz, Aksu, & Küçük, 2010). Eight of 20 American women indicated they would terminate if pregnant during treatment (Patel et al., 2009), and 3 of 5 women with unintended pregnancies in another study did choose to have an abortion (Dominick et al., 2015). One Australian woman with an unintended pregnancy was considering an abortion but did not disclose her final decision to the authors (Connell et al., 2006).
Contraception Counseling Needs and Preferences
Contraception during treatment was endorsed as “very important” by 81% of cancer survivors (N = 107) (Maslow et al., 2014). Women acknowledged that they were overloaded with information at diagnosis but contended that they needed the information early to make treatment decisions and that fertility issues became an increasingly high priority over time (Thewes et al., 2005; Thewes, Meiser, Rickard, & Friedlander, 2003). Women expressed uncertainty about the tradeoffs of contraception, fearing that pregnancy and hormonal contraception threatened their health (Connell et al., 2006). In a study of reproductive-aged Swiss women with breast cancer, the authors calculated that 62 of 100 participants needed contraception counseling at time of cancer diagnosis; women were considered in need of contraception counseling at diagnosis if they were not using a highly effective contraception method or if they were using a method that had potential safety issues for women with cancer (Güth et al., 2015). About 17% of women in an Australian sample (N = 228) never had their question, “What should I do about contraception?” answered during their cancer care (Thewes et al., 2005).
A prominent theme was uncertainty about ability to conceive and need for contraception. Women with breast cancer expressed frustration about this uncertainty and described fertility as the aspect of cancer treatment least in their control (Thewes et al., 2003). Misconceptions among women with cancer included the belief that women could not get pregnant after cancer treatment (Connell et al., 2006; Patel et al., 2009). Despite having no clinical diagnosis of infertility, some women believed they were infertile and, because of that belief, did not use contraception during treatment (Maslow et al., 2014; Zebrack et al., 2004), which led to unintended pregnancy (Zebrack et al., 2004). Some women reported that providers discussed fertility status with them (Zebrack et al., 2004), but pretreatment general counseling about fertility did not diminish the risk of unintended pregnancy after controlling for age and desire to parent (Quinn, Letourneau, & Rosen, 2014).
Women described discrepancies between the contraception counseling received and desired. Nurses or physicians who specialized in oncology were the most desired source of contraception counseling by Turkish women with breast cancer, who expressed fear of receiving inaccurate information from other sources; however, 8 of these 20 women recalled getting contraceptive counseling from nurses or physicians outside the oncology clinic (Karaöz et al., 2010). An individual consultation with a fertility or menopause specialist was the preferred source among Australian women with breast cancer, most of whom recalled getting contraceptive counseling from their oncology team (Thewes et al., 2003, 2005).
Contraception counseling generally fostered contraception use. Maslow et al. (2014) found that 65% of their sample received contraception counseling, and women who had contraception counseling had almost seven times greater odds of using highly effective methods than women who had no counseling. Dominick et al. (2015) found that 56% of their sample reported receipt of contraception counseling since diagnosis, and users of highly effective contraception methods were more likely to have received family planning counseling than users of less effective methods.
Contraception Methods
At every stage of the cancer care continuum, women were sexually active without desiring to conceive and without using contraception, which equates to a risk for unintended pregnancy. Among women with cancer, use of highly effective contraception methods was sporadic and was highest after an intervention to improve reproductive health service delivery was pilot tested (Patel et al., 2015). In a sample of women with various cancers, 40 of 107 women (37%) affirmed that they were sexually active during treatment and, of those 40 sexually active women, 6 used no contraception (Maslow et al., 2014). In two studies, women stopped taking estrogen-containing oral contraceptive pills when diagnosed with breast cancer (Güth et al., 2015; Maslow et al., 2014), rendering them unprotected from unintended pregnancy in absence of contraception counseling and initiation of a new method. Of the women surveyed by Patel et al. (2009), 9 of 20 women were sexually active without contraception, but only 4 of those 9 women desired pregnancy at that time. Klosky et al. (2012) and Klosky et al. (2014) found that 11 of 75 female survivors of childhood cancer reported use of no contraception the last time they had sex, which was not significantly different from the rate reported by their healthy siblings. In another study among survivors of nongynecologic cancers, 58 of 275 women (21%) did not use contraception, despite not desiring pregnancy and having resumed menstruation, which was used as a proxy for fertility (Quinn et al., 2014). When Dominick et al. (2015) compared a cancer survivor sample to the general population, as described by the 2006–2010 National Survey for Family Growth, cancer survivors were significantly less likely to use highly effective contraception than women in the general population. In addition, 10% of survivors were not using contraception while sexually active, despite not seeking pregnancy, which was not significantly different but trending higher than the 8% of women in the general population (Dominick et al., 2015). As a point of comparison with more recent analyses, no contraception was used by 10% of sexually active American women aged 15–44 years who were not seeking pregnancy, pregnant, postpartum, or noncontraceptively sterile (Guttmacher Institute, 2016). Factors associated with not using contraception included being at risk for emotional discomfort or low self-esteem (Klosky et al., 2014); being partnered (Dominick et al., 2015; Quinn et al., 2014); age, with odds increasing by 7% with each additional year (Quinn et al., 2014); and not having graduated college (Quinn et al., 2014).
Discussion
The data available indicate that women with cancer are not consistently using contraception in alignment with their pregnancy goals, thereby experiencing unintended pregnancy and having an abortion. Misconceptions and confusion about the effect of cancer on fertility are pervasive. Women’s uncertainty was not consistently addressed by contraception counseling, and women expressed dissatisfaction with the source and content. The primary implication for practice is that women with cancer or cancer history need more effective family planning service delivery, including contraception counseling and contraception provision.
Using contraception to time pregnancies for periods of better health is highly relevant to women with a recent cancer diagnosis, survivors of cancer in adulthood, and survivors of childhood cancer. Pregnancy during cancer is often possible but rife with uncertainty. Because few large cohort studies or randomized clinical trials have addressed questions about pregnancy during cancer, the available evidence is somewhat limited (Morice, Uzan, & Uzan, 2012). Pregnancy does not always directly affect cancer prognosis (Stensheim, Møller, van Dijk, & Fosså, 2009), but cancer treatment options can pose great threats to fetal health and declining treatment can affect recovery. Ionizing radiation used for staging and therapy can cause significant damage to the fetus at 0.1–0.2 Gy; although many conventional radiographic examination techniques deliver less than 0.1 Gy to the fetus, pelvic or abdominal computed tomography can deliver 0.1–0.4 Gy (Kal & Struikmans, 2005). In a 2012 literature review, Amant, Loibl, Neven, and Van Calsteren found that most pregnant women can safely undergo anesthesia and surgery for cancer treatment, but pain can stimulate preterm labor. Breast cancer hormonal therapy with tamoxifen (Nolvadex®) is contraindicated during the first trimester, with some evidence of it being less dangerous later in pregnancy. All chemotherapy is contraindicated for the first 10 weeks of gestation, and certain types are contraindicated throughout pregnancy, particularly methotrexate (Trexall®), a well-known abortifacient. Chemotherapy can cause hematopoietic suppression, so women were advised to plan on ending three weeks before delivery to minimize the risks of excessive bleeding and infection at the time of delivery. However, anticipating the delivery date can be challenging because women with cancer are at risk for preterm birth.
About 80% of childhood cancer survivors are achieving a five-year survival (Phillips et al., 2015). However, Oeffinger et al. (2006) found that 73% of survivors of childhood cancer have additional chronic health conditions later in life, and 42% have severe, disabling, life-threatening, or terminal conditions. Contraception can be understood as a valuable tool for timing pregnancies for periods of better health, which also provides women desiring children an opportunity to initiate preconception care and early prenatal care to further optimize fetal outcomes.
Unintended pregnancy should be paid more attention in the context of cancer care, given the evidence synthesized in this current review, which builds on the body of literature about the prevalence and challenges of unintended pregnancy among women managing other chronic illnesses (Choquet, Du Pasquier Fediaevsky, & Manfredi, 1997; Chor, Rankin, Harwood, & Handler, 2011; Miauton, Narring, & Michaud, 2003; Suris & Parera, 2005; Suris, Resnick, Cassuto, & Blum, 1996). Recognition is increasing that reproductive health issues are amenable to intervention in the time from cancer diagnosis to treatment, as well as later in survivorship. Multiple studies indicate that most women of reproductive age want to have children in the future (Gonçalves, Sehovic, & Quinn, 2013; Salem et al., 2013; Schover, Rybicki, Martin, & Bringelsen, 1999), and the American Society of Clinical Oncology (ASCO) recommends that women diagnosed with cancer receive fertility preservation before treatment (Loren et al., 2013). Like fertility preservation, contraception counseling is time sensitive; unintended pregnancies during active cancer management can complicate and limit treatment options. Nurses can deliver more patient-centered care by initiating conversations about pregnancy during cancer and then providing support, education, and resources based on women’s clinical factors, reproductive goals, and contraception preferences. Nurses seeking to improve their understanding of these issues may use resources listed in Figure 2. One resource specifically designed for nurses is Enriching Communication Skills for Health Professionals in Oncofertility, an eight-week online training about the information and counseling skills necessary to fulfill the ASCO recommendations for reproductive health care (Vadaparampil et al., 2016). 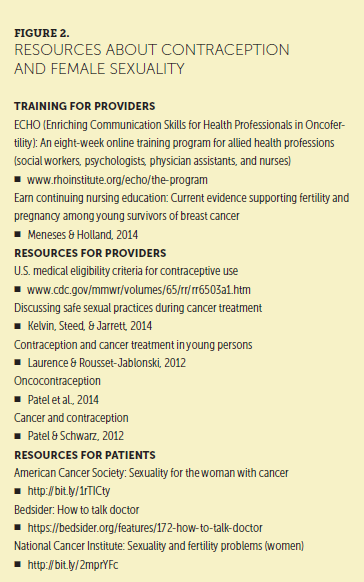
Limitations
The findings are fragmented because the studies vary by size, rigor, sample, setting, and focus. The 2000–2015 time frame was used to increase the number of studies eligible for inclusion; consequently, some of the research is dated. Comparing rates of contraception use or unintended pregnancy was challenging because the denominator—the number of women potentially at risk for unintended pregnancy—is not determined in a standardized way. Some studies only included women who were menstruating, but this excludes women who have not yet menstruated but may get pregnant with the first ovulation and fails to exclude women who have occult ovarian failure while menstruating. Other studies did not document pregnancy intentions, masking desire or ambivalence that can influence contraception choices. Contraception survey questions like, “used method to prevent pregnancy or sexually transmitted disease at last intercourse” or “pregnancy prevention at last intercourse,” are commonly asked of youth but do not capture long-term use, and more effective contraception methods were not distinguished from less effective methods (Klosky et al., 2012, 2014). However, this review shows the current state of knowledge, which can be difficult to extract from the scholarly literature because so much discourse around contraception and cancer concerns whether contraception causes cancer, not the management of pregnancy and fertility.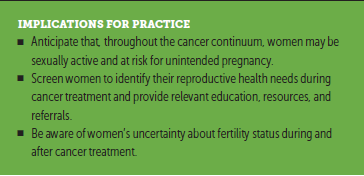
Conclusion
This systematic review identifies a problem in cancer management. Women with cancer are receiving inadequate contraception services and experiencing unintended pregnancy. When women consistently use contraception throughout the cancer care continuum, they can avail themselves of more cancer treatment options and pursue their reproductive life plans while managing their health. Improving reproductive health care for women with cancer has potential to improve cancer management and survivorship care.
The author gratefully acknowledges Beth Black, PhD, RN, for her feedback and editing.
[[{"type":"media","view_mode":"media_original","fid":"31141","attributes":{"alt":"","class":"media-image","height":"351","typeof":"foaf:Image","width":"366"}}]]
About the Author(s)
Laura Elizabeth Britton, BSN, RN, is a doctoral candidate in the School of Nursing at the University of North Carolina in Chapel Hill. The author takes full responsibility for this content. Britton is a Hillman Scholar in Nursing Innovation and Jonas Nurse Leader Scholar. During the writing of this article, Britton was also supported by a National Institutes of Health/National Institutes of Nursing Research grant (T32NR007091-20; principal investigator: Sheila Judge Santacroce, PhD, RN, CPNP, FAANP). The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Mention of specific products and opinions related to those products do not indicate or imply endorsement by the Oncology Nursing Society. Britton can be reached at lbritton@email.unc.edu, with copy to editor at CJONEditor@ons.org. (Submitted May 2016. Accepted August 8, 2016.)
References
Amant, F., Loibl, S., Neven, P., & Van Calsteren, K. (2012). Breast cancer in pregnancy. Lancet, 379, 570–579. doi:10.1016/S0140-6736(11)61092-1
American Cancer Society. (2017). Cancer facts and figures 2017. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
Choquet, M., Du Pasquier Fediaevsky, L., & Manfredi, R. (1997). Sexual behavior among adolescents reporting chronic conditions: A French national survey. Journal of Adolescent Health, 20, 62–67. doi:10.1016/S1054-139X(96)00091-2
Chor, J., Rankin, K., Harwood, B., & Handler, A. (2011). Unintended pregnancy and postpartum contraceptive use in women with and without chronic medical disease who experienced a live birth. Contraception, 84, 57–63. doi:10.1016/j.contraception.2010.11.018
Connell, S., Patterson, C., & Newman, B. (2006). A qualitative analysis of reproductive issues raised by young Australian women with breast cancer. Health Care for Women International, 27, 94–110. doi:10.1080/07399330500377580
Dominick, S.A., McLean, M.R., Whitcomb, B.W., Gorman, J.R., Mersereau, J.E., Bouknight, J.M., & Su, H.I. (2015). Contraceptive practices among female cancer survivors of reproductive age. Obstetrics and Gynecology, 126, 498–507. doi:10.1097/AOG.0000000000000963
Finer, L.B., & Zolna, M.R. (2016). Declines in unintended pregnancy in the United States, 2008–2011. New England Journal of Medicine, 374, 843–852. doi:10.1056/NEJMsa1506575
Gonçalves, V., Sehovic, I., & Quinn, G. (2013). Childbearing attitudes and decisions of young breast cancer survivors: A systematic review. Human Reproduction Update, 20, 279–292. doi:10.1093/humupd/dmt039
Green, D.M., Whitton, J.A., Stovall, M., Mertens, A.C., Donaldson, S.S., Ruymann, F.B., . . . Robison, L.L. (2002). Pregnancy outcome of female survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. American Journal of Obstetrics and Gynecology, 187, 1070–1080.
Güth, U., Huang, D.J., Bitzer, J., Tirri, B.F., & Moffat, R. (2015). Contraception counseling for young breast cancer patients: A practical needs assessment and a survey among medical oncologists. Breast, 30, 217–221. doi:10.1016/j.breast.2015.10.003
Guttmacher Institute. (2016). Contraceptive use in the United States. Retrieved from https://www.guttmacher.org/sites/default/files/factsheet/fb_contr_use_0…
Kal, H.B., & Struikmans, H. (2005). Radiotherapy during pregnancy: Fact and fiction. Lancet Oncology, 6, 328–333. doi:10.1016/S1470-2045(05)70169-8
Karaöz, B., Aksu, H., & Küçük, M. (2010). A qualitative study of the information needs of premenopausal women with breast cancer in terms of contraception, sexuality, early menopause, and fertility. International Journal of Gynecology and Obstetrics, 109, 118–120. doi:10.1016/j.ijgo.2009.11.027
Kelvin, J.F., Steed, R., & Jarrett, J. (2014). Discussing safe sexual practices during cancer treatment. Clinical Journal of Oncology Nursing, 18, 449–453. doi:10.1188/14.CJON.449-453
Klosky, J.L., Foster, R.H., Li, Z., Peasant, C., Howell, C.R., Mertens, A.C., . . . Ness, K.K. (2014). Risky sexual behavior in adolescent survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Health Psychology, 33, 868–877. doi:10.1037/hea0000044
Klosky, J.L., Howell, C.R., Li, Z., Foster, R.H., Mertens, A.C., Robison, L.L., & Ness, K.K. (2012). Risky health behavior among adolescents in the childhood cancer survivor study cohort. Journal of Pediatric Psychology, 37, 634–646. doi:10.1093/jpepsy/jss046
Laurence, V., Gbolade, B.A., Morgan, S.J., & Glaser, A. (2004). Contraception for teenagers and young adults with cancer. European Journal of Cancer, 40, 2705–2716.
Laurence, V., & Rousset-Jablonski, C. (2012). Contraception and cancer treatment in young persons. In G.P. Quinn & S.T. Vadaparampil (Eds.), Reproductive health and cancer in adolescents and young adults (pp. 41–60). Netherlands: Springer.
Loren, A.W., Mangu, P.B., Beck, L.N., Brennan, L., Magdalinski, A.J., Partridge, A.H., . . . Oktay, K. (2013). Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. Journal of Clinical Oncology, 31, 2500–2510. doi:10.1200/JCO.2013.49.2678
Maslow, B.S., Morse, C.B., Schanne, A., Loren, A., Domchek, S.M., & Gracia, C.R. (2014). Contraceptive use and the role of contraceptive counseling in reproductive-aged women with cancer. Contraception, 90, 79–85. doi:10.1016/j.contraception.2014.03.002
Meneses, K., & Holland, A.C. (2014). Current evidence supporting fertility and pregnancy among young survivors of breast cancer. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 43, 374–381. doi:10.1111/1552-6909.12301
Miauton, L., Narring, F., & Michaud, P.A. (2003). Chronic illness, life style and emotional health in adolescence: Results of a cross-sectional survey on the health of 15-20-year-olds in Switzerland. European Journal of Pediatrics, 162, 682–689. doi:10.1007/s00431-003-1179-x
Morice, P., Uzan, C., & Uzan, S. (2012). Cancer in pregnancy: A challenging conflict of interest. Lancet, 379, 495–496. doi:10.1016/S0140-6736(11)61814-X
Oeffinger, K.C., Mertens, A.C., Sklar, C.A., Kawashima, T., Hudson, M.M., Meadows, A.T., . . . Robison, L.L. (2006). Chronic health conditions in adult survivors of childhood cancer. New England Journal of Medicine, 355, 1572–1582. doi:10.1056/NEJMsa060185
Patel, A., Roston, A., Stempinski, K., Zimmerman, L., O’Neill, E., & Patel, A.R. (2014). Oncocontraception. In R.H. Allen & C. Cwiak (Eds.), Contraception for the medically challenging patient (pp. 255–271). New York, NY: Springer.
Patel, A., Roston, A., Uy, A., Radeke, E., Roston, A., Keith, L., & Zaren, H.A. (2015). Reproductive health and endocrine disruption in women with breast cancer: A pilot study. Supportive Care in Cancer, 23, 411–418. doi:10.1007/s00520-014-2381-2
Patel, A., & Schwarz, E.B. (2012). Cancer and contraception. Contraception, 86, 191–198. doi:10.1016/j.contraception.2012.05.008
Patel, A., Sreedevi, M., Malapati, R., Sutaria, R., Schoenhage, M.B., Patel, A.R., . . . Zaren, H.A. (2009). Reproductive health assessment for women with cancer: A pilot study. American Journal of Obstetrics and Gynecology, 201, 191. doi:10.1016/j.ajog.2009.04.021
Patient-Centered Outcomes Research Institute. (2013). Patient-centered outcomes research. Retrieved from http://www.pcori.org/research-results/patient-centered-outcomes-research
Phillips, S.M., Padgett, L.S., Leisenring, W.M., Stratton, K.K., Bishop, K., Krull, K.R., . . . Armstrong, G.T. (2015). Survivors of childhood cancer in the United States: Prevalence and burden of morbidity. Cancer Epidemiology, Biomarkers, and Prevention, 24, 653–663.
Quinn, M.M., Letourneau, J.M., & Rosen, M.P. (2014). Contraception after cancer treatment: Describing methods, counseling, and unintended pregnancy risk. Contraception, 89, 466–471. doi:10.1016/j.contraception.2014.01.014
Royal College of Obstetricians and Gynecologists. (2011). Pregnancy and breast cancer: Green-top guideline no. 12. Retrieved from https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_12.pdf
Salem, W.H., Letourneau, J.M., Chan, J., Chan, S.-W., Cedars, M., & Rosen, M.P. (2013). Women with gynecologic cancers are suboptimally counseled about post treatment reproductive health outcomes. Fertility and Sterility, 3(Suppl.), S65. doi:10.1016/j.fertnstert.2013.07.1881
Schover, L.R., Rybicki, L.A., Martin, B.A., & Bringelsen, K.A. (1999). Having children after cancer: A pilot study of survivors’ attitudes and experiences. Cancer, 86, 697–709.
Spring, B. (2007). Evidence-based practice in clinical psychology: What it is, why it matters; what you need to know. Journal of Clinical Psychology, 63, 611–631. doi:10.1002/jclp.20373
Stensheim, H., Møller, B., van Dijk, T., & Fosså, S.D. (2009). Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: A registry-based cohort study. Journal of Clinical Oncology, 27, 45–51. doi:10.1200/JCO.2008.17.4110
Suris, J.C., & Parera, N. (2005). Sex, drugs and chronic illness: Health behaviours among chronically ill youth. European Journal of Public Health, 15, 484–488. doi:10.1093/eurpub/cki001
Suris, J.C., Resnick, M.D., Cassuto, N., & Blum, R.W. (1996). Sexual behavior of adolescents with chronic disease and disability. Journal of Adolescent Health, 19, 124–131. doi:10.1016/1054-139X(95)00282-W
Taplin, S.H., Anhang Price, R., Edwards, H.M., Foster, M.K., Breslau, E.S., Chollette, V., . . . Zapka, J. (2012). Introduction: Understanding and influencing multilevel factors across the cancer care continuum. Journal of the National Cancer Institute Monographs, 2012, 2–10. doi:10.1093/jncimonographs/lgs008
Thewes, B., Meiser, B., Rickard, J., & Friedlander, M. (2003). The fertility- and menopause-related information needs of younger women with a diagnosis of breast cancer: A qualitative study. Psycho-Oncology, 12, 500–511. doi:10.1002/pon.685
Thewes, B., Meiser, B., Taylor, A., Phillips, K.A., Pendlebury, S., Capp, A., . . . Friedlander, M.L. (2005). Fertility- and menopause-related information needs of younger women with a diagnosis of early breast cancer. Journal of Clinical Oncology, 23, 5155–5165. doi:10.1200/JCO.2005.07.773
Vadaparampil, S.T., Gwede, C.K., Meade, C., Kelvin, J., Reich, R.R., Reinecke, J., . . . Quinn, G.P. (2016). ENRICH: A promising oncology nurse training program to implement ASCO clinical practice guidelines on fertility for AYA cancer patients. Patient Education and Counseling, 99, 1907–1910. doi:10.1016/j.pec.2016.05.013
Winther, J.F., Boice, J.D., Jr., Svendsen, A.L., Frederiksen, K., & Olsen, J.H. (2009). Induced abortions in Danish cancer survivors: A population-based cohort study. Journal of the National Cancer Institute, 101, 687–689. doi:10.1093/jnci/djp064
Zebrack, B.J., Casillas, J., Nohr, L., Adams, H., & Zeltzer, L.K. (2004). Fertility issues for young adult survivors of childhood cancer. Psycho-Oncology, 13, 689–699. doi:10.1002/pon.784




