Virchow’s Node and Carcinoma of Unknown Primary
Virchow’s node is the enlargement of the left supraclavicular lymph node and is considered by clinicians to be a strong indicator of metastatic abdominal malignancy. Virchow’s node is located medially and is a deep-seeded node, making it difficult to assess in a healthy individual.
Jump to a section
A 45-year-old woman presents late one afternoon to a walk-in clinic seeking antibiotics for an infection she says she has had for a few weeks. Her concern is a sore neck and a swollen, non-tender lymph node. She has no significant medical conditions and is not currently taking any regular medications. She denies any fever, cough, weight loss, changes in her appetite, or bowel habits. She looks and feels well aside from reports of mild fatigue that she attributes to a busy schedule and a stiff neck, which has negatively affected her sleep. She is a well-groomed, affluent, married mother of two who works part-time as a physiotherapist. Her family history is noncontributory, and she drinks alcohol socially and is a lifelong nonsmoker. Her physical examination is essentially unremarkable: vital signs are stable, skin is dry and intact, chest is clear on auscultation, and abdomen is soft with no distention or ascites. However, a solitary lymph node is visible, measuring 3 cm to the left supraclavicular area, which has been enlarged for a few weeks. She also has small, palpable lymph nodes in her left axilla. She is wearing a scarf to cover her neck because friends keep asking her about “the lump,” which she finds annoying. The patient says she has been meaning to see her family doctor but is busy and keeps forgetting to make an appointment. She was driving by the clinic and, because it didn’t look busy, she thought she would stop in and “get some antibiotics to clear it up.”
After the initial assessment, the nurse practitioner (NP) requests blood work and a chest x-ray. The patient is becoming increasingly anxious to get her antibiotics and go home. She does not understand why she needs these tests and continues to tell the nurse that she does not have time for “all this fuss.” Her complete blood count (CBC) and electrolyte results come back within normal limits, and her chest x-ray shows no obvious signs of infection and appears normal; however, a small shadow is seen at the base of the left lung. The NP requests for a radiologist to review the film before discharge, but the patient is increasingly impatient and agitated about having to wait. Instead, she says to forget the antibiotics and that she will see her own doctor when she has time. Despite a waiting room that is quickly filling up, the NP is determined to keep the patient there until radiology reviews her film. As she begins to leave, the NP asks her again to reconsider. She is concerned that, despite a lack of obvious symptomology, that the woman has cancer.
Signal Nodes
Virchow’s node is the enlargement of the left supraclavicular lymph node and is considered by clinicians to be a strong indicator of metastatic abdominal malignancy (Frank-Stromberg & Cohen, 2005). First described in the literature by German pathologist Rudolf Virchow, MD, in 1848 as an enlarged gland that was associated with gastric cancers, it has come to be known as a signal node, signaling the presence of an underlying cancer from a primary lesion in the upper abdomen (Bickley, 2009). Although strongly associated with the presence of gastric carcinomas, case reports in the literature link Virchow’s node with primary breast, lung, intestine, pancreas, testicular, and bladder carcinomas, as well as lymphoma (Anastassiades & Poterucha, 2006; Cervin, Silverman, Loggie, & Geisinger, 1995; Hemalatha, Batra, Ramah, & Shashikumar, 2013; Komala, 2014). In contrast, the enlargement of the right supraclavicular lymph node is more often associated with Hodgkin and non-Hodgkin lymphoma, as well as lung and esophageal cancers (Cervin et al., 1995).
Limited information exists in the literature on Virchow’s node but, in a retrospective review of 152 fine-needle aspirate samples of supraclavicular lymphadenopathy, Cervin et al. (1995) found 96 (63%) to be positive for malignancy (58 in left-sided nodes and 38 in right-sided nodes). Pelvic and abdominal malignancies were more likely to metastasize to the left supraclavicular node, with 16 of 19 pelvic tumors metastasizing to the left, and all six primary abdominal malignancies spreading to the left node rather than the right. Cervin et al. (1995) concluded that right- and left-sided supraclavicular lymphadenopathy are indicative of distinctly different primary tumors with thoracic, breast, and head and neck cancers showing no difference in metastatic patterns.
Virchow’s node is located medially and is a deep-seeded node, making it difficult to assess in a healthy individual. Asking patients to engage in the Valsalva maneuver causes the node to rise, allowing for easier palpation on physical examination (Frank-Stromberg & Cohen, 2005). The enlargement of the left supraclavicular lymph node in the presence of metastatic abdominal disease is related to location and drainage patterns of the lymphatic system. Virchow’s node is the end node of the supraclavicular chain of lymph nodes and is located at the thoracic duct near the jugulo-subclavian venous junction where incoming lymph is introduced back into the venous circulation through the subclavian vein; therefore, any malignancies rising from the thorax or abdomen can be responsible for the enlargement of the supraclavicular node. Gastric carcinoma tends to metastasize by means of tumor emboli migrating through the thoracic duct where the subdiaphragmatic lymphatic drainage enters the venous circulation in the subclavian vein (Siosaki & Tarsila-Sousa, 2013). Malignancy of internal organs often is advanced at the time of diagnosis as many patients with early-stage disease experience few symptoms; complications related to site of metastases is one of the first indicators of disease (Sundriyal, Kumar, Dubey, & Walia, 2013).
The pathology of lymphadenopathy varies and is not always caused by an underlying malignancy; the differential diagnosis of Virchow’s node is abdominal malignancy, breast cancer, lymphoma, and/or infection (Cervin et al., 1995). An excisional tissue biopsy is necessary to confirm pathology of the primary tumor (Tan, 2015).
The Case
The NP was an experienced clinician and took the time to settle the patient, review the assessment findings that led to her conclusion, and discuss the next steps with the patient. A biopsy of her enlarged node would be required to confirm the presence of cancer. The NP was familiar with the referral process to the local cancer center and facilitated quick and seamless consultation. The patient was referred to surgical oncology for fine-needle aspiration. The results confirmed the presence of malignant cells, but the sample contained insufficient tissue for a definitive diagnosis. A subsequent excisional biopsy reported metastatic carcinoma that was poorly differentiated but favoring metastatic non-small cell carcinoma of the lung rather than metastatic breast cancer. A variety of tests were ordered (bilateral mammography and magnetic resonance imaging [MRI] of the breasts; computed tomography [CT] of the head, neck, and abdomen; pelvic examination and Papanicolaou test; and upper and lower gastrointestinal endoscopy) to determine the primary site; however, all were non-diagnostic. A CT of her chest showed a 5 x 3 cm triangular soft tissue mass present along the left hemithorax and along the mediastina pleural/right anterior mediastinum. A focal pleural soft tissue nodule also was present in relation to the right seventh rib. Serum tumor marker CA-125 was slightly elevated at 58 U/ml, but CA 19-9, CEA, alpha feto-protein, beta HCG, and lactate dehydrogenase (LDH) were within normal limits. Despite numerous investigations, no primary site was found, and she was started on a multidrug chemotherapy regimen for carcinoma of unknown primary, which included paclitaxel (Taxol®), carboplatin (Paraplatin®), and gemcitabine (Gemzar®).
Carcinomas of Unknown Primary
Carcinomas of unknown primary (CUP) account for 2%–6% of all malignant diagnoses in the United States and are comprised of a group of heterogeneous tumors involving metastatic epithelial disease with no identifiable origin at the time of diagnosis (Boyland & Davis, 2008). Men and women are affected equally, with the median age at diagnosis being 72 years (Tan, 2015). Treatment options are limited, and prognosis tends to be poor with a median survival of 4–11 months with one- and five-year survival rates of 15%–20% and 5%–10%, respectively (Boyland & Davis, 2008; Tan, 2015). Patients with CUP and multiple sites of organ involvement fare poorly, with an average prognosis of three to four months (Tan, 2015). CUP are presumed to be at an advanced stage (stage IV) at the time of presentation, with the most common tissue subtypes being adenocarcinoma (60%), poorly differentiated (30%), squamous cell (5%), and neuroendocrine (5%) (Oien & Dennis, 2012).
Receiving any cancer diagnosis is a life-changing moment and a significant source of stress for individuals (Bennett & Alison, 1996). Patients who are diagnosed with CUP often experience greater levels of anxiety and greater difficulty accepting and coping with the cancer diagnosis because the primary site cannot be determined (Boyland & Davis, 2008). Specifically, a mixed design exploratory study of 10 patients with CUP found that patients diagnosed with CUP experience greater uncertainty because of the unpredictability of their situations, are constantly seeking a firm diagnostic label to increase their understanding and gain a greater sense of control, and experience difficulty identifying and relating to other patients with cancer (Boyland & Davis, 2008). About 15% of all patients with cancer present with or experience symptoms directly caused by a site of metastasis rather than the primary tumor, as is the case with Virchow’s node, with the primary site being identified with further investigations in about 66% of cases (Oien, 2009; Oien & Dennis, 2012).
Serum tumor markers, such as CA-125, CA 19-9, or CEA, are non-specific and may not be used to establish a definitive diagnosis. However, when combined with diagnostic imaging (e.g., CT, MRI), they may provide clinicians with greater insight into the primary site (Tan, 2015). The diagnostic procedure of choice is tissue biopsy (Tan, 2015). When no primary site is identified, determining effective treatments and predicting outcomes and overall prognosis can be difficult, which also can provoke anxiety for patients and caregivers (Tan, 2015).
Implications for Oncology Nursing
Virchow’s node is an ominous sign for oncology clinicians, alerting them to the possibility of an underlying abdominal malignancy. Patients want and expect to be well informed and presented with all the available information, good and bad, as it becomes known. Keeping patients informed involves disclosure and truth telling (see Figure 1). Oncology nurses should be present during difficult conversations about diagnosis and prognosis to translate technical information; clarify the patients understanding of the situation; ensure the provision of privacy, sensitivity, and adequate time; and to allow patients to feel and express all emotions, good and bad, as they are felt (Bennett & Alison, 1996). The challenge in disclosing information in acute care settings, such as emergency departments, is to disclose information in the best possible way, in a manner that is efficient, effective, and appropriate for each situation (Tobin, 2012). When there is only a suspicion of malignancy, specific and substantial information may not be readily available, and confirming the clinician’s suspicion requires open biopsy and pathology review, which require time and organization. During periods of high uncertainty, such as the disclosure of a new cancer diagnosis and at times of disease relapse, an individual’s sense of hope is threatened; therefore, to maintain hope, oncology nurses must be present, knowledgeable, confident, realistic, truthful, and honest (Thorne, Oglov, Armstrong, & Hislop, 2007). Regardless of the content of the disclosure, patients want to receive news from clinicians who are caring and sensitive and who offer hope and reassurance (Okamura, Uchitomi, Sasako, Eguchi, & Kakizoe, 1998).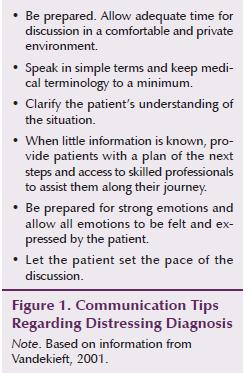
When revealing distressing news to patients, nurses should guide patients away from their perception of the situation to the reality and gravity of the situation at a pace the patient finds manageable (Mauri, Vegni, Lozza, Parker, & Moja, 2009). This poses a challenge in busy acute care settings, such as emergency departments. However, regardless of location, receiving distressing news has a lasting effect and impression on patients and families and must be delivered in a sensitive, thorough, and thoughtful manner.
References
Anastassiades, C.P., & Poterucha, T.H. (2006). Virchow’s node, jaundice, and weight loss-lymphoma mimicking gastrointestinal malignancy. Nature Clinical Practice: Gastroenterology and Hepatology, 3, 645–648.
Bennett, M., & Alison, D. (1996). Discussing the diagnosis and prognosis with cancer patients. Postgraduate Medical Journal, 72, 25–29.
Bickley, L.S. (Ed). (2009). Bates’ guide to physical examination (10th ed.). Philadelphia, PA: Lippincott Williams and Wilkins.
Boyland, L., & Davis, C. (2008). Patients’ experiences of carcinoma of unknown primary site: Dealing with uncertainty. Palliative Medicine, 22, 177–183.
Cervin, J.R., Silverman, J.F., Loggie, B.W., & Geisinger, K.R. (1995). Virchow’s node revisited. Analysis with clinicopathologic correlation of 152 fine-needle aspiration biopsies of supraclavicular lymph nodes. Archives of Pathology and Laboratory Medicine, 119, 727–730.
Frank-Stromberg, M., & Cohen, R. (2005). Assessment and intervention for cancer detection. In C. Henke-Yarbro, M. Hansen-Frogge, M. Goodman, & S.L. Groenwald (2005). Cancer nursing: Principles and practice (5th ed., pp. 150–188). Boston, MA: Jones and Bartlett.
Hemalatha, A.L., Batra, N., Ramah, D.B., & Shashikumar, S.D. (2013). Virchow’s node not always signifies a primary gut or lung malignancy. Look further and farther. International Journal of Case Reports in Medicine. Retrieved from http://bit.ly/1k9LZOE
Komala, B. (2014). Virchow’s node: A look beyond gut carcinoma. American Journal of Experimental and Clinical Research, 1(2), 33–34.
Mauri, E., Vegni, E., Lozza, E., Parker, P.A., & Moja, E.A. (2009). An exploratory study on the Italian patient’s preferences regarding how they would like to be told about their cancer. Supportive Care in Cancer, 17, 1523–1530.
Oien, K.A. (2009). Pathological evaluation of unknown primary cancer. Seminars in Oncology, 36, 8–37.
Oien, K.A., & Dennis, J.L. (2012). Diagnostic work-up of carcinoma of unknown primary: From immunohistochemistry to molecular profiling. Annals of Oncology, 23(Suppl. 10), 271–277.
Okamura, H., Uchitomi, Y., Sasako, M., Eguchi, K., & Kakizoe, T. (1998). Guidelines for telling the truth to cancer patients. Japanese Journal of Clinical Oncology. Retrieved from http://bit.ly/1VpL0uC
Siosaki, M.D., & Tarsila-Sousa, A. (2013). Virchow’s node. New England Journal of Medicine, 368(6), e7.
Sundriyal, D., Kumar, N., Dubey, S., & Walia, M. (2013). Virchow’s node. BMJ Case Reports. Retrieved from http://bit.ly/1LoqbWk
Tan, W. (2015). Metastatic cancer with unknown primary site. Retrieved from http://bit.ly/1LdO4Su
Thorne, S., Oglov, V., Armstrong, E.A., & Hislop, T.G. (2007). Prognosticating futures and the human experience of hope. Palliative and Supportive Care, 5, 227–239.
Tobin, G.A. (2012). Breaking bad news. Cancer Nursing, 35, E21–E29.
Vandekieft, G.K. (2001). Breaking bad news: Discussion of preparation and techniques. American Family Physician, 64, 1975–1978.
About the Author(s)
Erin Streu, RN, MN, CON(C), is a clinical nurse specialist at CancerCare Manitoba in Winnipeg, Canada. No financial relationships to disclose. Mention of specific products and opinions related to those products do not indicate or imply endorsement by the Oncology Nursing Forum or the Oncology Nursing Society. Streu can be reached at estreu@cancercare.mb.ca, with copy to editor at ONFEditor@ons.org.

