Facilitating Shared Decision Making About Prostate Cancer Screening Among African American Men
Purpose/Objectives: To describe the development and implementation of a prostate cancer screening intervention and risk assessment decision tool.
Design: Community health promotion with pre- and post-education knowledge questionnaires.
Setting: Two predominantly African American churches in different suburban communities in Southern California.
Sample: A convenience sample of 50 African American men aged from 30–75 years.
Methods: A Prostate Cancer Screening Decision Aid was developed and used in conjunction with an educational intervention for African American men in two suburban communities in Southern California. The educational intervention was implemented in local African American churches. The intervention included a PowerPoint® presentation with a four-minute video. Men completed pre- and post-education knowledge questionnaires and a risk assessment decision tool.
Main Research Variables: Prostate cancer knowledge, awareness of prostate cancer personal risks and benefits of prostate cancer screening, information needed for initiating discussions with provider, and intention to participate in shared decision making with healthcare providers.
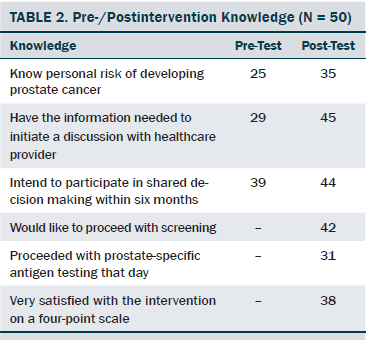
Findings: An 8% increase in knowledge was calculated when comparing pre- and post- education responses. Awareness of personal risks, having the information needed to initiate a discussion with a healthcare provider, intention to participate in shared decision making within six months, prostate cancer knowledge, and having had participated in screening increased.
Conclusions: The intervention was successful in increasing knowledge and awareness of personal risks and providing tools to facilitate shared decision making with healthcare providers.
Implications for Nursing: Nurses can play a meaningful role in collaborating with community lay leaders to develop and implement effective health promotion interventions for African Americans.
Jump to a section
African American men have the highest incidence of prostate cancer and the greatest mortality rates compared to other population groups in the United States (American Cancer Society [ACS], 2010a, 2013). African American men have a 1 in 5 lifetime probability of getting prostate cancer and a 1 in 22 lifetime probability of dying from it (ACS, 2010a, 2013). However, these men also have the lowest rate of participation in prostate cancer screening (National Cancer Institute [NCI], 2012b). Until 2012, prostate cancer screening guidelines recommended routine screening for men beginning at age 40–45 years for high-risk groups and age 50 years for those considered to be at low to average risk for developing prostate cancer. Recently, the value of prostate cancer screening has been controversial among healthcare professionals. Proponents of screening cite evidence showing the benefits of prostate cancer screening in facilitating early detection and treatment of prostate cancer and the resulting improved outcomes. At the same time, ample evidence shows that screening results in overdiagnosis of asymptomatic prostate cancers that may never progress. With research showing that only 1 in 1,000 men avoid death because of screening—and 30–40 are harmed from screening and treatment (U.S. Preventive Services Task Force [USPSTF], 2012a)—the USPSTF revised screening recommendations. Although some opinions still differ among healthcare professionals about who should be screened, most guidelines advise against routine screening. Instead, any decision to be screened is recommended to be shared between the individual and his healthcare provider (ACS, 2010a, 2010b; Carter et al., 2013; USPSTF, 2012b).
If shared decision making is overlooked, African American men likely will face even greater morbidity and mortality from prostate cancer. Although oncology nurses may be aware of these new prostate cancer screening guidelines, they may lack the knowledge or tools to educate men facing screening decisions about how best to proceed.
An evidence-based health promotion intervention was developed to address the serious nature of this community health problem. The intervention addressed the following question: Would African American men who participate in an educational seminar in conjunction with a Prostate Cancer Screening Decision Aid (PCSDA) have increased knowledge about prostate cancer, awareness of personal risks, information about how to initiate discussions with providers, and intention to participate in shared decision making about screening with healthcare providers?
This article describes the development and implementation of an educational intervention that uses a risk assessment decision tool to increase prostate cancer knowledge and to facilitate shared decision making for African American men in two churches in different suburban Southern California communities.
Literature Review
The review of relevant literature was divided into four categories: studies on shared decision making, studies on focus groups, studies on decision aids, and studies on health promotion conducted in faith-based settings. A report from ACS (Wolf et al., 2010) maintained that an ethical mandate exists to provide a man considering prostate cancer screening the opportunity to engage in a decision-making process that is shared with a healthcare provider. However, research suggests that shared decision making may not be routinely taking place (Légaré et al., 2010). Elwyn et al. (2012) outlined a three-step approach to accomplish shared decision making: introduction of choices, a description of the available options, and finalization of the decision.
Focus groups are known to be beneficial with the planning, development, and implementation of community-based interventions (Allen, Kennedy, Wilson-Glover, & Gilligan, 2007; Baker, 2008). Themes emerging from such studies suggest that prostate cancer prevention interventions should be embedded in community settings and should emphasize trust-building relationships between healthcare professionals and members of the community. Building such relationships is key to the success of community-based interventions (Jones, Steeves, & Williams, 2009).
Review of the literature included searching for decision aids used to help make complex health-related decisions. Research findings indicate that implementing such educational interventions using decision aids with men increases their knowledge, reduces decisional conflict, and increases engagement in decision making (O’Connor et al., 2007; Rubel et al., 2010; Stacey et al., 2011; Van Vugt et al., 2010). One intervention, which included 73 African American men who attended a one-time prostate cancer educational seminar in a faith-based setting, used a pre-/post-test design to assess the impact of the intervention on increasing knowledge about the risks and benefits of screening, promoting confidence in decision making, and decreasing decisional conflict (Drake, Shelton, Gilligan, & Allen, 2010). A road map decision aid, which included information about the risks and benefits of screening and viable screening options, was used during the seminar. A brief description of the road map decision aid was given but not included in the literature. The results of the study showed an increase in knowledge by an average of 26% (p < 0.001) and an increase in decisional self-efficacy by an average of 8.9 points (p = 0.025).
Interventions focused on educating African American men about prostate cancer implemented in community settings, such as churches, barbershops, and community centers, showed positive outcomes (Drake et al., 2010). One study conducted by Emerson, Reece, Levine, Hull, and Husaini (2009) included 345 African American men who attended an educational seminar in a faith-based setting on the topic of prostate cancer. These researchers found an increase in knowledge and participation in shared decision making when comparing pre- and post-education responses. Such settings also are found to be ideal for successful recruitment.
Methods
The methods used to develop and implement this educational intervention included developing a decision aid and an educational seminar, which was evaluated by pre- and post-testing.
Theoretical Framework
The Iowa model (Titler, 2002), which incorporates a multidisciplinary approach to guide practitioners in the process of development and implementation of interventions, was used as a framework in developing this educational program. The steps were followed to identify the topic, determine the priority for the organization, formulate the team, assemble and critique relevant research literature to support the intervention, pilot the change in practice, and determine if the change was appropriate for adoption (Titler, 2002).
Two other models guided this project—the Health Belief Model (HBM) (Champion & Skinner, 2008) and the Community Empowerment Model (Persily & Hildebrant, 2008). The HBM, which posits that individuals who believe that their health is at risk will act in response to that perceived threat, provides support for developing an intervention reminding learners about the threats of a potential disease. The Community Empowerment Model stresses the importance of building relationships with community leaders.
Planning the Intervention
With evidence supporting the use of decision aids for individuals who are making a decision about prostate cancer screening (ACS, 2010a; Légaré et al., 2010; Stacey et al., 2011), an up-to-date decision aid for African American men was compiled and trialed. The tool was designed to meet evolving research findings, current screening guidelines, and practice recommendations from national organizations (ACS, 2010a; American Society of Clinical Oncology, 2012; NCI, 2012b).
According to Taylor et al. (2013), a decision aid should be readable at or below an eighth grade level. It should contain current information about benefits and risks of screening and provide encouragement to discuss findings with healthcare providers. O’Connor et al. (2007) suggested that decision aids should present balanced information about options with enough details to allow individuals to come to a decision that matches their personal values. A two-page PCSDA for use with an educational presentation for African American men in a faith-based setting was created. The PCSDA was designed to reflect national screening guidelines and was assessed for readability at a grade of 7.5 on the Flesch-Kincaid readability index (Flesch-Kincaid, n.d.). Content validity was established using a broad spectrum of healthcare professionals in the oncology, urology, and research divisions of Loma Linda University Medical Center in Loma Linda, California. A focus group of community clergy and lay leaders provided input on the clarity, readability, and cultural appropriateness of the decision aid.
The first page of the tool was designed to outline the benefits and risks of prostate cancer testing and treatment. The second page was designed to include a checklist for self-assessment of personal risks. This section was divided into two distinct categories of high- and low-risk items. Individuals are expected to weigh their risks by determining if more items on either side apply to their situation (see Figure 1). In addition, the PCSDA was designed to provide individuals with insight on whether they would consider treatment should they decide to go forward with the screening and subsequently receive a diagnosis of prostate cancer. Finally, the PCSDA was designed to prompt men to share their decision with their family members and healthcare providers. 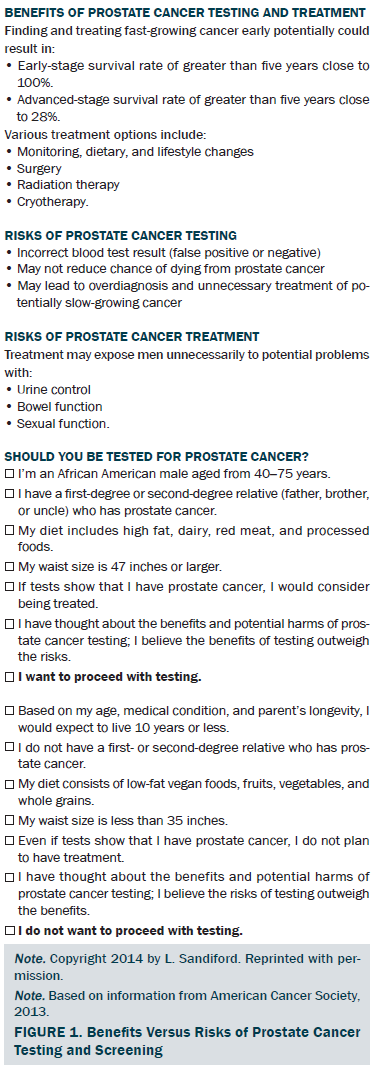
A 30-minute PowerPoint® presentation was developed using information from national organizations such as ACS (2010a) and NCI (2012b). The information provided facts about prostate cancer, including incidence and mortality rates, risk factors, screening guidelines, benefits versus risks of prostate-specific antigen (PSA) testing, survival rates, treatment options, and prevention strategies. The PowerPoint presentation was presented to African American men in the study by a radiation oncology nurse in a group setting.
A 21-item pre-/post-education questionnaire was created by the first author. The pre- and post-education questions were identical, except that the demographic section was not repeated in the post-education questionnaire. Questions were based on information from the educational seminar. This questionnaire reflected a Flesch-Kincaid readability index of grade 5.2 and included questions regarding prostate cancer knowledge, beliefs about personal risks of getting prostate cancer, and intention to initiate discussions about screening with a healthcare provider. The knowledge questions required true or false responses.
Development of Partnerships
Implementation of such an intervention necessitated building strong collaborative partnerships among a local healthcare organization, a university, and community leaders. For example, support was obtained from the executive director of the Loma Linda Cancer Center to absorb the cost for PSA testing.
Content validity for the PCSDA and pre-/post-education questionnaires was provided by six experts to determine the appropriateness and breadth of the questions in the tools. Reviewers included research scientists, advanced practice nurses, educators, a radiation oncologist, and a urologist; each provided feedback on the content of the materials.
In addition, a focus group comprised of local clergy and lay leaders was convened to field test the decision aid and questionnaire for clarity, readability, and cultural appropriateness. The group shared perspectives about the needs of the target population (e.g., availability of screening at an affordable cost) and suggested strategies for overcoming those barriers (e.g., hosting the seminar in the community). They reviewed all materials and provided feedback. Some questions were deleted because of ambiguity, and others were edited for clarity. Although interventions commonly are conducted within the African American community to offer incentives for participation, the focus group felt that this would be unnecessary. They indicated that pastors and lay leaders would recruit participants for the intervention using word-of-mouth invitations, posting fliers in area churches and local barbershops, and placing advertisements in local newspapers.
Intervention
Institutional review board approval from Loma Linda University was obtained prior to implementation of the project. The evidence-based intervention was given the name “Take Time Out to Live.” Anonymous informed consent was obtained prior to individuals completing the PCSDA and questionnaire.
Participants and Setting
The educational intervention was delivered in group sessions at Living Waters Church of God in Fontana and New Hope Missionary Baptist Church in San Bernardino, both in California. Men and women were in attendance at the seminars, but only the men completed the questionnaires and PCSDA. The pre-/post-education questionnaires and PCSDA were completed on the same day. Seventeen men participated at one location, and 42 participated at the other. Nine participants were excluded because they did not meet inclusion criteria. Participants were African American men aged 30–75 years old. The mean age of participants was 57 years.
Procedure
Participants completed a pre-test covering demographic information such as age, marital status, and education level. They then completed a prostate cancer health history, addressing issues such as participation in previous PSA screening, diagnosis of prostate cancer, family history of prostate cancer, and perception of risk of prostate cancer. Finally, participants completed the prostate cancer knowledge questions before listening to the 30-minute educational presentation. The educational program included a lecture, questions and answers, and a four-minute video featuring two African American prostate cancer survivors sharing their experiences of coping with a prostate cancer diagnosis (NCI, 2012a) in which men were encouraged to talk to their family members, friends, and doctor about prostate cancer. Participants then completed a post-test, which contained the same questions as the pre-test. Finally, the PCSDA was completed with participants choosing to proceed with PSA screening or not to proceed with PSA screening. PSA testing was offered on site free of charge. Individuals were provided with the following resources: a wallet-size version of the PCSDA, a brochure containing prostate cancer facts, and a booklet containing a list of facilities that provide low-cost or free options for screening and follow-up health care and information about low-cost health coverage.
Data Analysis
Descriptive statistics were performed on demographic variables using SPSS®, version 22.0. Four categories of information were elicited from the participants: perception of personal risk of developing prostate cancer, knowledge acquisition, information needed to initiate discussion with healthcare providers, and intention to participate in shared decision making. Perception of personal risk was calculated by comparing the percentage of increase in the pre- and post-education responses to the question regarding knowledge of the level of risk. To measure knowledge acquisition, percentages of correct responses were compared on participants’ pre- and post-education scores on a 21-item prostate cancer knowledge questionnaire. A higher difference in post-intervention knowledge reflected knowledge acquisition. Responses to the statements, “I have enough information to initiate discussion with my healthcare provider,” and “I plan to discuss prostate cancer screening with my healthcare provider within the next six months,” were calculated by comparing percentage of increase in the responses “yes,” “no,” and “don’t know” from pre- to post-test.
Results
A convenience sample of 50 men participated in the intervention (see Table 1). The percentage of correct responses to the knowledge questions prior to the intervention was 69%. An 8% increase in knowledge was calculated when comparing pre- and post-education responses, with 69% correct responses pretest and 77% correct responses post-test. Increases were observed in awareness of personal risks, having the information needed to initiate a discussion with a healthcare provider, and intention to participate in shared decision making within six months (see Table 2).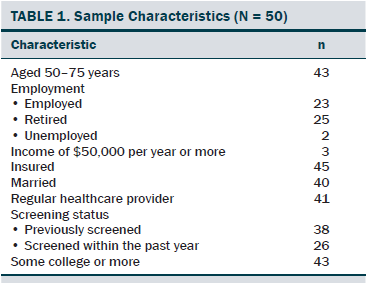
Discussion
The purpose of this project was to implement an evidence-based practice intervention designed to increase knowledge about prostate cancer, awareness of personal risks, information about how to initiate discussion with providers, and intention to participate in shared decision making about screening with healthcare providers. The findings of this intervention showed that participants began with a high level of knowledge, with 69% of the items correctly answered on the pre-test and a modest increase of 8% on the post-test. The majority of participants indicating that they would like to proceed with screening is congruent with studies that showed that participation in educational interventions is associated with willingness to be screened (Taylor et al., 2006).
The intervention had a simple design with low out-of-pocket costs. Key to success was the involvement of church lay leaders and pastors in the planning, development, and implementation of the intervention. Excitement was generated within the community, with invitations already being made for educational interventions for the following year. In addition, the nurse educators were invited to participate in two community health-screening events and were specifically requested to present the PCSDA for men considering prostate cancer screening decisions. The nurse educators also were invited to be interviewed for a community television program to highlight the intervention.
Limitations
The high college education level and high percentage of men reporting being previously screened may account for the high prostate cancer knowledge scores at baseline. This suggests that this sector may have already been exposed to some prostate cancer education. The higher correct knowledge scores at baseline (69%) may account for the modest increase to 77%. Research shows that African American men with higher education are more likely to be medical source seekers and participate in prostate cancer prevention (Ross et al., 2011). Given that the demographic indicators of this sample suggest that it was socioeconomically secure, how this intervention would be received by those who are more impoverished or uneducated is unknown.
The recruitment advertisement was not clear on whether spouses were invited to attend, and although some spouses were in attendance, in other instances, spouses reported that they were on the premises but did not know that they could attend the education seminar. For future programming, educators should clearly indicate that significant others are invited. The participants may have been far less vulnerable than non–church-attending groups in the community. Church-going men may have a higher interest in seeking health promotion information because of religious beliefs about their moral responsibility to care for the body as a gift from God.
Implications for Nursing
Nurses should identify the health concerns of the community in which they serve and be involved in planning and implementing interventions to address those concerns. Oncology nurses must be knowledgeable about the shift in screening guidelines from routine screening to shared decision making and be prepared to educate the community accordingly. Nurses can facilitate shared decision making by providing relevant information and using effective tools, such as the PCSDA, for men facing screening decisions. Nurses involved in community-based education programs may find replication of this intervention for African American men beneficial for increasing awareness of prostate cancer risks and empowering men to initiate discussions about screening with healthcare providers. Collaborating with community leaders in such educational programs would ensure sustainability.
Conclusion
The intervention was a successful outreach to the African American men. The PCSDA was found to be a useful educational tool in the seminar for raising awareness about risks and benefits of screening and in facilitating intent to participate in shared decision making with healthcare providers. The results of this evidence-based practice intervention demonstrates the value of healthcare professionals working together to develop effective community health promotion interventions. The involvement of the pastors and lay leaders with the focus group sessions and with recruitment likewise was crucial to the success of the intervention. Nurses can play a key role in educating individuals about their risks of disease and in using tools to assist them in making informed decisions about participating in prostate cancer screening. 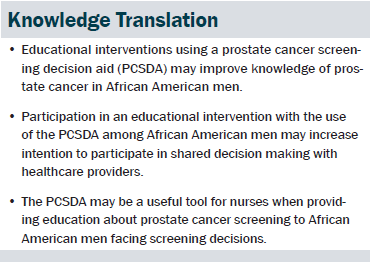
The authors gratefully acknowledge Anita Adorador, DNP, CPCO, for her mentorship in the planning and development of the prostate cancer screening educational program and Elizabeth Johnston-Taylor, PhD, RN, for her editorial assistance with the manuscript.
References
Allen, J.D., Kennedy, M., Wilson-Glover, A., & Gilligan, T.D. (2007). African-American men’s perceptions about prostate cancer: Implications for designing educational interventions. Social Science and Medicine, 64, 2189–2200. doi:10.1016/j.socscimed.2007.01.007
American Cancer Society. (2010a). Cancer facts and figures 2010: Special section—Prostate cancer. Retrieved from http://www.cancer.org/acs/groups/content/@researh/documents/document/ac…
American Cancer Society. (2010b). Testing for prostate cancer: Should I be tested? Is it the right choice for me? Retrieved from http://www.cancer.org/acs/groups/content/@editorial/documents/document/…
American Cancer Society. (2013). Cancer facts and figures for African Americans. Retrieved from http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/docum…
American Society of Clinical Oncology. (2012). ASCO decision aid tool: Prostate cancer screening with PSA testing. Retrieved from https://www.asco.org/sites/www.asco.org/files/psa_pco_decision_aid_7161…
Baker, S.A. (2008). Prostate cancer screening intention among African American men: An instrument development study. Retrieved from http://scholarcommons.usf.edu/etd/128/
Carter, H.B., Albertsen, P.C., Barry, M.J., Etzioni, R., Freedland, S.J., Greene, K.L., . . . Zietman, A.L. (2013). Early detection of prostate cancer: AUA guideline. Retrieved from http://bit.ly/1evyBhT
Champion, V.L., & Skinner, C.S. (2008). The health belief model. In K. Glanz, B.K. Rimer, & K. Viswanath (Eds.), Health behavior and health education: Theory, research, and practice (pp. 45–65). Hoboken, NJ: Wiley.
Drake, B.F., Shelton, R.C., Gilligan, T., & Allen, J.D. (2010). A church-based intervention to promote informed decision making for prostate cancer screening among African American men. Journal of the National Medical Association, 102, 164–171.
Elwyn, G., Frosch, D., Thomson, R., Joseph-Williams, N., Lloyd, A., Kinnersley, P., . . . Barry, M. (2012). Shared decision making: A model for clinical practice. Journal of General Internal Medicine, 27, 1361–1367. doi:10.1007/s11606-012-2077-6
Emerson, J.S., Reece, M.C., Levine, R.S., Hull, P.C., & Husaini, B.A. (2009). Predictors of new screening for African American men participating in a prostate cancer educational program. Journal of Cancer Education 24, 341–345. doi:10.1080/08858190902854749
Flesch-Kincaid. (n.d.). The Flesch grade level readability formula. Retrieved from http://www.readabilityformulas.com/flesch-grade-level-readability-formu…
Jones, R.A, Steeves, R., & Williams, I. (2009). Strategies for recruiting African American men into prostate cancer screening studies. Nursing Research, 58, 452–456.
Légaré, F., Ratté, S., Stacey, D., Kryworuchko, J., Gravel, K., Graham, I.D., & Turcotte, S. (2010). Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database of Systematic Reviews, 5, CD006732.
National Cancer Institute. (2012a). An African American man’s prospective: Prostate cancer survival. Retrieved from https://www.youtube.com/watch?v=5pmijciboDc
National Cancer Institute. (2012b). Fact sheet: Prostate-specific antigen test. Retrieved from http://1.usa.gov/UtgLW8
O’Connor, A.M., Wennberg, J.E., Legare, F., Llewellyn-Thomas, H.A., Moulton, B.W., Sepucha, K.R., . . . King, J.S. (2007). Toward the ‘tipping point’: Decision aids and informed patient choice. Health Affairs, 26, 716–725. doi:10.1377/hlthaff.26.3.716
Persily, C., & Hildebrandt, E. (2008). The theory of community empowerment. In M.J. Smith & P. Liehr (Eds.), Middle range theory for nursing (pp. 111–205). New York, NY: Springer.
Ross, L., Dark, T., Orom, H., Underwood, W., III, Anderson-Lewis, C., Johnson, J., & Erwin, D.O. (2011). Patterns of information behavior and prostate cancer knowledge among African-American men. Journal of Cancer Education, 26, 708–716.
Rubel, S.K., Miller, J.W., Stephens, R.L., Xu, Y., Scholl, L.E., Holden, E., . . . Volk, R.J. (2010). Testing the effects of a decision aid for prostate cancer screening. Journal of Health Communication, 15, 307–321.
Stacey, D., Bennett, C.L., Barry, M.J., Col, N.F., Eden, K.B., Holmes-Rovner, M., . . . Thomson, R. (2011). Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews, 10, CD001431.
Taylor, K.L., Davis, J.L., III, Turner, R.O., Johnson, L., Schwartz, M.D., Kerner, J.F., & Leak, C. (2006). Educating African American men about the prostate cancer screening dilemma: A randomized intervention. Cancer Epidemiology Biomarkers and Prevention, 15, 2179–2188. doi:10.1158/1055-9965.EPI-05-0417
Taylor, K.L., Williams, R.M., Davis, K., Luta, G., Penek, S., Barry, S., . . . Miller, E. (2013). Decision making in prostate cancer screening using decision aids vs usual care: A randomized clinical trial. JAMA Internal Medicine, 173, 1704–1712.
Titler, M.G. (2002). Toolkit for promoting evidence-based practice. Iowa City, IA: University of Iowa Hospital and Clinics, Department of Nursing Services and Patient Care.
U.S. Preventive Services Task Force. (2012a). Prostate cancer: Screening. Retrieved from http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummar…
U.S. Preventive Services Task Force. (2012b). Understanding taskforce recommendations: Screening for prostate cancer. Retrieved from http://www.uspreventiveservicestaskforce.org/prostatecancerscreening/pr…
van Vugt, H.A., Roobol, M.J., Venderbos, L., Joosten-van Zwanenburg, E., Essink-Bot, M., Steyerberg, E.W., . . . Korfage, I.J. (2010). Informed decision-making on PSA testing for the detection of prostate cancer: An evaluation of a leaflet with risk indicator. European Journal of Cancer, 46, 669–677.
Wolf, A.M., Wender, R.C., Etzioni, R.B., Thompson, I.M., D’Amico, A.V., Volk, R.J., . . . Smith, R.A. (2010). American Cancer Society guideline for the early detection of prostate cancer: Update 2010. Retrieved from http://pressroom.cancer.org/download/2010+prostate+cancer+early+detecti…
About the Author(s)
Sandiford is a manager of referral and intake development in the James M. Slater Proton Treatment Center at the Loma Linda University Medical Center in California and D’Errico is an associate professor in the School of Nursing at Loma Linda University in California. The prostate-specific antigen testing used in this study was sponsored by the Loma Linda University Cancer Center. Sandiford and D’Errico contributed to the conceptualization and design, analysis, and manuscript preparation. Sandiford completed the data collection. D’Errico provided statistical support. Sandiford can be reached at lynettesandiford3@gmail.com, with copy to editor at ONFEditor@ons.org. Submitted March 2015. Accepted for publication May 25, 2015.

