The Nurse Practitioner Role in Oncology: Advancing Patient Care
Purpose/Objectives: To explore and describe the characteristics of the nurse practitioner (NP) role in cancer care in a Canadian province, identify the ways in which NPs add value to cancer care, and suggest ways in which organizations can better support the NP role.
Research Approach: Exploratory, qualitative design.
Setting: Three cancer care facilities in a western Canadian province.
Participants: 12 NPs in cancer care, 12 physicians working with NPs, and 5 administrators responsible for implementing the role.
Methodologic Approach: Interpretive description, a qualitative method aimed at systematically exploring and analyzing a topic and applying the findings back into practice.
Findings: Each group had a different perspective on the role and its value. Physicians regarded these high-level practitioners as “help” within their own practices. Administrators tended to use NPs to manage patient workload within the traditional physician-focused system, but they could see value in NP-led innovation. The NPs themselves envisioned a nontraditional, holistic, patient-centered approach to care that challenged the interventionist focus of the medical model. Suggestions for enhancing the potential of the role were offered by all groups.
Conclusions: Lack of clarity about the NP role persists. Traditional professional hierarchies and expectations about care delivery continue to affect role implementation.
Interpretation: Nursing leaders must be proactive about NP role implementation to maximize its potential. Additional research is needed about the outcomes of the role and the process of implementation.
Jump to a section
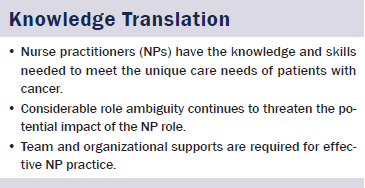
Concerns about the sustainability and effectiveness of Western healthcare systems, including Canada’s, have prompted interest in addressing access issues, providing wellness-oriented early intervention, shifting toward less institutionalized care, and using human resources more effectively. The nurse practitioner (NP) role has been in place in Canada for several decades and is looked to as a way of achieving such changes. Particularly in cancer care, increasing acuity and rising patient volumes highlight the need to diversify the healthcare workforce to provide patient care. Although research to date has demonstrated that NPs give high-quality care with excellent patient outcomes, a chronic lack of role clarity and acceptance has hindered the implementation of this role and constrained its potential to contribute to meaningful system change (DiCenso & Bryant-Lukosius, 2010). This article reports the findings of a qualitative study designed to explore and describe the characteristics of the NP role in cancer care in a Canadian province, identify the ways in which NPs add value to cancer care, and suggest ways in which organizations can better support the NP role.
Background
The NP role is part of a set of nursing roles that constitute advanced nursing practice. In oncology, as in other practice settings, the advanced practice nurse is a “registered nurse, prepared with a minimum of a Master’s degree in nursing, who has acquired in-depth knowledge and clinical experience in oncology” (Canadian Association of Nurses in Oncology, 2001, p. 61). Advanced practice roles have existed in many countries for more than 40 years, but the use of these roles has been hindered by role clarity and scope of practice issues and has ebbed and flowed depending on government, physician, administrative, and public support (Andregárd & Jangland, 2015; DiCenso & Bryant-Lukosius, 2010; Kleinpell, Hudspeth, Scordo, & Magdic, 2012). Nevertheless, advanced nursing practice, including the NP role, is described as the “future frontier” for nursing practice because it offers a way of questioning current practices, improving healthcare delivery, and creating new models of patient care (Bryant-Lukosius, DiCenso, Browne, & Pinelli, 2004).
NPs have competencies that are relevant to the challenges facing health care today (Spross & Heaney, 2000). The NP role has been seen as a way to address service gaps, physician workload, lack of continuity of care, and less-than-optimal care interventions (Andregárd & Jangland, 2015; Kilpatrick et al., 2010). In short, this role can meet the “needs of patients that are not being adequately met by the healthcare system with its current configuration of roles” (Pringle, 2007, p. 5). NPs can improve patient outcomes related to health and functional status, quality of life, and satisfaction with care (Bryant-Lukosius et al., 2004). Research has shown that NP care is characterized by at least equivalent health outcomes when compared to physician practice and, in many cases, more thorough diagnostic assessment, greater rates of symptom resolution, increased patient satisfaction, more teaching about self-care, and more complete record keeping (Brown & Grimes, 1995; Bryant-Lukosuis et al., 2007; Horrocks, Anderson, & Salisbury, 2002).
According to the Canadian Cancer Society’s Steering Committee on Cancer Statistics (2012), the incidence of cancer in Canada is increasing, owing largely to a growing and aging population. American statistics suggest that people diagnosed and living with cancer will increase by 81% by 2020 (Bishop, 2009). Cancer-related mortality is declining (Canadian Cancer Society’s Steering Committee on Cancer Statistics, 2012), and cancer increasingly is being treated as a chronic disease. New treatments mean that people live longer with cancer and, therefore, require longer-term care (Bishop, 2009). Rising patient volumes and increased patient acuity, along with advances in science and technology related to cancer care, highlight the need for effective advanced practice roles for nurses that allow them to interpret and apply research evidence, manage complex therapies, and generally improve care and system access for patients with cancer (Bakker et al., 2013; Bishop, 2009). Oncology is a relatively new area of practice for NPs, and NPs are well positioned to fill the expanding service gap in cancer care.
Unfortunately, the optimal use of NPs’ knowledge and skills has been elusive and role ambiguity is a chronic problem generally and specifically within oncology (Bishop, 2009; DiCenso & Bryant-Lukosius, 2010; Gardner, Chang, & Duffield, 2007). Issues, such as interprofessional tensions and boundary conflicts, team acceptance, lack of systemwide and organizational support and resources, a view of NPs as physician replacements, and the diversity of titles and scopes of practice across jurisdictions and settings, constrain the potential of this role and limit the contribution that NPs can make to care delivery, as well as education, leadership, and research (Andregárd & Jangland, 2015; Bryant-Lukosius et al., 2004; Gardner et al., 2007; Harvey, Papps, & Roberts, 2015; Kilpatrick et al., 2010; Kleinpell et al., 2012; Lowe, Plummer, O’Brien, & Boyd, 2012; Naylor & Kurtzman, 2010). Overall, these factors contribute to role ambiguity and create role deployment issues that Andregárd and Jangland (2015) have described as “a tortuous journey towards a partially unknown destination” (p. 10). Indeed, the issue of NP role ambiguity pervades the literature about NP practice and, therefore, demands attention so that the full potential of the NP role can be realized (DiCenso & Bryant-Lukosius, 2010; Hurlock-Chorostecki, Forchuk, Orchard, van Soeren, & Reeves, 2014).
Methods
The purpose of this study was to explore and describe the characteristics of the NP role in cancer care and to identify the unique value of NP-provided care. Another goal of this study was to provide helpful evidence for organizational leaders in support of effective implementation of the NP role because patient care outcomes are affected by the way in which clinical care is organized and structured (Spross & Heaney, 2000). Study participants were asked about the functions of the NP role, the ways in which NPs added value to patient care, the ways in which the NP role responded to contemporary demands in healthcare delivery, and the organizational and team-based expectations of the NP role.
The method used for this study was interpretive description (ID). ID is a qualitative method in which researchers connect with participants who have rich experience with a particular topic that is shared, to some extent, with others in the field (Thorne, 2008; Thorne, Reimer Kirkham, & MacDonald-Emes, 1997; Thorne, Reimer Kirkham, & O’Flynn-Magee, 2004). Interviews are a primary form of data collection in ID, and small sample sizes are typical. According to Thorne et al. (2004), ID generates “a meaningful account of experiential knowledge” that goes beyond a simple description to offer an interpretation that illuminates the characteristics, patterns, and structure of the clinical issue in a useful manner (p. 3). The fundamental goal of this method is to ensure that the findings of the research are returned to the context of practice so that changes can be made (Thorne, 2008).
Data were collected via one-on-one, in-person interviews, held in late 2013, with 12 NPs, 12 oncologists, and 5 administrators from 3 cancer care hospitals (all part of one larger organization). Oncologists and administrators were included in the sample because of the influence that these groups typically have over the NP role definition and implementation. Participants were recruited via an initial email; snowball sampling was used to recruit additional participants. Interviews were audio recorded and transcribed. Data collection was finished when all interested members of the sample groups were able to participate and data saturation had been achieved (when no new themes or leads emerge from continued data collection) (Mayan, 2009).
Data analysis focused on “struggling to apprehend the overall picture with questions such as ‘what is happening here?’ and ‘what am I learning about this?’” to identify themes and generate a coherent analytic framework that could be meaningfully recontextualized (Thorne, 2008; Thorne et al., 1997; Thorne et al., 2004). The analysis was conducted by the researcher (first author) in constant consultation with the collaborating partner (second author) to ensure the validity of the interpretations made.
This study was granted approval from the research ethics board at the University of Alberta in Edmonton.
Findings
Responses from each participant category (NPs, oncologists, and administrators) were highly consistent. Among the NPs, who are the main focus of this article, the primary themes pertained to role clarity and evolution, role responsibilities, role acceptance, the value-added contributions of the role, and organizational supports and facilitators for the role. Oncologists tended toward a more traditional perspective on role functions and interprofessional relationships in cancer care, and administrators managed the complicated balance among operational needs, tradition, and innovation in their approach to NP role implementation.
Role Clarity and Evolution
Ambiguity around the NP role was the key theme. Considerable variation, lack of clarity, and ongoing change were associated with the role across all settings in which NPs worked. One NP recalled, “Starting out, the ambiguity was a challenge for everyone. It overlapped with medicine. It overlapped with nursing. What was the unique contribution of the NP? That’s a question that everyone is still asking.” Several nurses acknowledged that role ambiguity was, in some ways, a strength because “you can weave yourself into situations to try and fix them and work them out and then weave yourself out,” keeping the role flexible and adaptable. However, the level of concern and frustration with the uncertainty around the role was overwhelming, which led to inconsistencies and excessive workload.
One NP noted, “People see you as a nurse, which is a great thing, but it can be challenging” when NPs are not well differentiated from staff nurses or fully appreciated for what they could offer. One NP pointed out that, in many ways, she thought that an NP was perceived as “basically a staff nurse waiting for someone to tell you what to do except that you’re well educated at it.” One administrator described NPs as “basically RNs on steroids.” An experienced NP shared that a staff nurse was upset with her because, she said, “I wasn’t bringing the patients into the room. So I’m not sure what her expectation was about the role.” The issue was resolved by “explaining my role . . . that we’re kind of a resident with the benefit of being a nurse.” The NPs themselves found negotiating the boundaries of their role in relation to the staff nurse role to be difficult. One explained that she would do basic nursing tasks if necessary, but she acknowledged that “you have to be careful that you don’t get sucked in to doing a bunch of things” that may not be the best use of an NP’s skill set.
The NP role was implemented in different ways across various work areas, but, in general, NPs were added to teams because a service gap was identified by physicians and administrators. As one NP described, “We’ll plunk an NP in it, but we’ll give no real thought to what [the] job looks like.” Often, a care team “just wanted a nurse practitioner without a real sense of what that person would do, how they would integrate them with the team—things that merit some thought.” Another NP noted that “the lack of clear, upfront communication is a huge barrier to actually moving forward and developing the role into something that could be vibrant and sustained.” Instead, an NP said, “A tumor group needs some help, and then that just morphs into a job—that’s how it currently stands.” NPs and oncologists pointed out that the role evolved based on past experience with the role, NPs’ interests, and patient needs in specific care areas. One oncologist described the NP role development experience as “trial by fire” as his specialty tried to “figure out what to do with the people that we have around us.” In general, the NP role underwent “numerous reincarnations” and became “many different things for many different people.” Although openness existed within some teams to clarify the role, individual NPs usually were left to define the role for themselves.
Role Responsibilities
Despite the tremendous lack of role clarity, the study participants were able to articulate some specific role responsibilities and could describe their typical day-to-day activities. They described a wide range of responsibilities, but many activities were common across all of them (see Figure 1).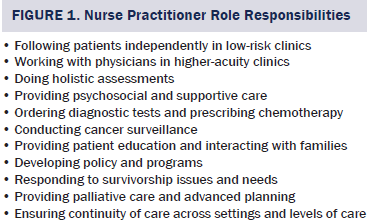
At best, role responsibilities seemed to be informally negotiated among team members, and, in many cases, job duties seemed to be decided on an ad hoc, hierarchical basis, with oncologists largely in control of what NPs would take on, rather than being driven by nursing priorities and the skills and interests of the NPs. NPs tended to have more autonomy in lower-acuity situations, which oncologists were more eager to give away so that they could attend to the more complex, high-acuity patients. One NP noted,
The oncologists value that I save them a lot of time. . . . We can take away some of their workload. . . . We’re like a clinical workhorse. . . . We’re doing the stuff that the medical oncologists really aren’t interested in doing.
The NPs perceived that they often were regarded as “more people to see patients” and do the “beck-and-call work,” or, as one described it, “scut work” that no one else wanted. Almost all of the NPs described how they were relied upon to cover for absent or busy physicians and were often “asked to troubleshoot on problems that aren’t really with my own patients.” Overall, as one NP explained,
There does not seem to be a large appetite for us creating our own job. While they’re somewhat open to it and they encourage us to expand on our capabilities, when it comes down to it, they haven’t been that supportive.
One NP found it “very frustrating that my job was defined by someone else.” Generally, NPs were regarded by oncologists as help in reducing physician workload. When administrators discussed the NP role responsibilities, they emphasized the clinical role and the contribution that NPs made to providing physician coverage, acting as “physician extenders,” and filling the most pressing organizational service gaps. In the oncologists’ and administrators’ views, the medical model of care was sustained and supported; however, some administrators observed that NPs thrived when they were able to function independently in self-defined, more nursing-oriented roles, such as survivorship transition, care coordination, and supportive care.
Despite the constraints, the NPs valued and promoted a unique nursing perspective. Each of them was able, to varying degrees, to carve out a small niche where they could define their practice. As one NP said, “I am not a medical oncologist. My job is to support those patients making sure that their symptoms are well managed and that they’re thriving,” which conveyed her nursing-based, holistic perspective. Another described how she was able to “sit and discuss things with a patient, work on improving policies, do patient education.” A couple pointed out their role in ensuring continuity of care for patients with cancer, with one NP explaining, “These patients need to have somebody shepherd them through this whole system.”
Role Acceptance and Recognition
Because of role ambiguity and role overlap, the NPs struggled with acceptance and recognition. One NP reflected, “When you think about an evolving profession, people don’t really understand at first why you’re there.” Some struggled with role acceptance for years. The NPs experienced a “constant state of trying to prove your worth” to patients, physicians, and other nurses. Several of the NPs spoke about being undervalued. Some said that the physicians they worked with did not have a full appreciation for what NPs contributed and, despite considerable rhetoric about the significance of the role, NPs continued to be underappreciated and invisible.
Most oncologists expressed appreciation for the NPs’ contributions. Many of them spoke of NPs as colleagues and as equal and valued members of the team who were knowledgeable, capable, and vital to patient care. However, a strong undercurrent of hierarchy and tradition was seen in the comments of the oncologists. One oncologist explained that it was “nice to have a colleague that can help me treat my patients” or, as another said, “free up time at the physician level.” Although NP skills were valued, they were almost always thought of as “a great addition to my practice” rather than independent providers in their own right. Summing up a common physician perspective, one oncologist said,
Not to take anything away from the ‘specialist nurses,’ but they are not independent practitioners. The physician is still left holding the bag and is the one at the end of the line as far as responsibility goes.
Administrators had mixed feelings about the NP role in their organizations. They could see the potential of the role to change cancer care and provide innovative patient services. On the other hand, they were focused on responding to increasing patient volumes and acuity and wanted the NPs to do whatever was required to meet service demands. One administrator summed up this tension, saying,
From a professional preparedness perspective, an individual NP can do anything, establish their professional domain. That said, we all work within systems and within cancer care, we have our obligations and need to define what our expectation of this resource will be.
Value-Added Contributions
In spite of role ambiguity and tension around the value of the role, all of the NPs were able to articulate the value-added dimensions of NP care and described receiving very satisfied feedback from patients. Regardless of the frustrations that these NPs experienced with their role, one of them expressed a common sentiment in saying, “I’m at the point now where I get justification from my patients, and that is really all I care about now.”
Patient satisfaction was fundamental to defining the value-added aspects of NP care. The NPs were committed to patient- and family-centered care and “seeing that they get what they need to get through the hardest journey of their life.” Being able to spend time with patients was of central importance. One NP said, “The patients are happy because they get the care. They get the conversation. They get the education and meaningful information-giving.” Another NP said,
In cancer care, we’re allowed to spend more time with the patients to be more holistic in our approach. So we can address not just the physical needs of the patient but the psychosocial and spiritual and the other needs as well.
As one NP explained,
I do the medical part. I know I need to evaluate from a medical point of view, and then I also ask them, “How are things going? What’s life at home like? How has your relationship changed? How can we improve things? Are there things we can work on to make your days at home better or your relationships better?” So that’s the value-added part. The medical part’s the relatively easy part. It’s more about what I can add to the visit that they’ll take home that will be meaningful for them.
Measuring the value of NP care was difficult. As one NP said, “In the medical field, it’s all about numbers, how many people you see, how fast you’re putting people through.” Quantifying the patient and operational outcomes associated with the time taken with patients was difficult. However, time spent with patients allowed the NPs to attend to things that the oncologists were not identifying, thereby avoiding unnecessary emergency visits, hospital admissions, and telephone calls from patients and families, not to mention patient anxiety, caregiver burnout, and family breakdown. NPs and administrators alike called for effective measures of NP care outcomes, but some NPs did observe that “they don’t ask physicians to justify what they do” in a system in which the medical model is the norm.
Organizational Context and Supports
At the most practical level, NPs expressed a strong need for daily supports for their practice, including clerical support, a staff nurse to work with in their clinics, and office space that afforded privacy. Strong and supportive team relationships also were noted to be important in facilitating the success of the NP role. At the organization level, the NPs observed, “There is a lack of commitment to the role; senior administration are not excited about it.” Some of the NPs felt that they were regarded simply as cheap labor. This was corroborated by one oncologist, who stated that administrators focused on “hours and pay scale and the final budget . . . and what they’ve lost sight of is the care of the patient.” Inconsistent role implementation and the ad hoc nature of its development were cited as reasons for the significant level of role ambiguity that existed. The NPs called for inclusion in care delivery planning, strong nursing leadership, and an increased organizational commitment to developing the role. The administrators themselves were aware of the historic gaps in planning. Some were frustrated that the NPs were unable to repair the situation themselves by taking charge of the situation and advocating for their work in their clinical areas. Other administrators wanted to take a step back, enhance communication among NPs, build leadership within and in support of the NP group, and build evidence about the effectiveness of the role to build a vision and plan for the role. Almost everyone was overwhelmed by the magnitude of the issues.
Discussion and Implications
The experiences of the NPs in this study are consistent with examples in the literature. These nurses faced significant role ambiguity, issues with role acceptance, and a lack of organizational support and planning, and struggled with hierarchical issues in a persistently traditional system. They, like many other NPs, found the potential of their role to be constrained and limited. According to previous research, organizations tend to implement the NP role as an ad hoc solution to an immediate local problem, rather than as a strategic, well-defined initiative, which results in wide role variation, lack of role clarity, and inconsistent expectations (Bryant-Lukosius et al., 2004). Insufficient planning and administrative support for the NP role results in suboptimal role use and presents a barrier to realizing its full potential (Bryant-Lukosius et al., 2004, 2007). The NPs in this study experienced these issues in the implementation and understanding of their own roles, frustrations that also were shared, to some extent, by their physician colleagues. Some administrators were reflecting on these concerns and endeavoring to respond by enhancing communication and planning.
The nurses in this study had a strong sense of their contributions to patient care and organizational effectiveness. Although the scopes of practice of NPs and physicians can overlap (DiCenso & Bryant-Lukosius, 2010; Lowe et al., 2012), NPs are capable of not only taking on the clinical tasks that are offloaded by their medical colleagues, but also remaining nursing-oriented and using the therapeutic benefit of nursing to “facilitate efficient and high-quality care for patients” (Hopwood, 2006, p. v), emphasizing values of holism, collaboration, coordinated care, advocacy, egalitarian partnerships with patients and families, and diverse interpersonal, counseling, and technical skills (Bakker et al., 2013; Bryant-Lukosius et al., 2007; Spross & Heaney, 2000). This positions NPs to add considerable value to patient care in response to the changing context of cancer care delivery.
As previously noted, today’s healthcare leaders are struggling to find new ways of delivering care and supporting health. System pressures have led to scrutiny about organizational structures and care processes, and NPs have been seen as an important resource for addressing the complex demands of contemporary healthcare delivery (Lowe et al., 2012; Spross & Heaney, 2000). Knowledge of the context of oncology practice, to which this study contributes, can help support the creation of practice environments that enable nurses with unique knowledge and skills, such as NPs, to meet the unique care needs of patients with cancer (Bakker et al., 2013).
The findings of this study have implications for NPs, administrators, and physicians as they work together to integrate the NP role into healthcare delivery; these implications are consistent with strategies suggested in the existing literature on the NP role. The NPs in this study described how their roles developed according to individual perspectives and specific local needs and evolved reactively over time, which led to inconsistencies in role implementation, ineffective use of NP skills and knowledge, and confusion and conflict across departments and professional groups. Kilpatrick, Lavoie-Tremblay, Lamothe, Ritchie, and Doran (2013) pointed out that structural factors affect the day-to-day working of healthcare teams. Therefore, national, regulatory, and organizational coordination and planning are vital to NP role clarity and sustainability (Harvey et al., 2015; Kilpatrick et al., 2010, 2013).
NPs’ personal qualities, such as their pioneering spirit and interpersonal skills, have been identified as being important to the success of NP role implementation (Andregárd & Jangland, 2015; Brown & Draye, 2003). However, this places a burden on individual NPs to manage issues that reach far beyond their personal spheres of influence. Increasingly, the employer’s role in creating favorable conditions that support the NP role is recognized (Andregárd & Jangland, 2015; Bakker et al., 2013; Spross & Heaney, 2000). Andregárd and Jangland (2015) argued that the NP role would be better incorporated if healthcare organizations had clear, long-term strategies for implementation that involved leadership, facilitation, and communication. Although some of the nurses in this study worked with supportive physicians, support for the NP role was not necessarily present at broader levels of the organization. Leadership and advocacy for the role were inconsistent, and NPs were left to manage their work issues in isolation. However, what is known from previous research is that NP role enactment is more effectively progressed when organizational support includes a nursing or medical role champion, clear and consistent messages from nursing and medical leaders, face-to-face supervision from engaged administrators, and formalized mentorship for NPs in developing roles (Andregárd & Jangland, 2015; Kilpatrick et al., 2013).
Because of the overlap of physician and NP practice, physicians should be included in planning and discussions as key stakeholders. However, the development of this role also should be led by nurses who have the professional jurisdiction over their scope of practice. The nurses in this study struggled to have the nursing aspects of their job recognized and valued; however, they themselves were clear about the value that the NP role added to patient care. The competence of NPs to manage patient care is well documented, as noted previously. Bryant-Lukosius et al. (2004) argued that it is critical to “support the development of a strong nursing orientation to advanced practice [that is] characterized by patient-centered, health-focused and holistic care” as a way of moving forward in care provision to society (p. 527).
In 2002, the Commission on the Future of Health Care in Canada reiterated longstanding calls to make fundamental changes to healthcare delivery and to address the need to change healthcare providers’ scopes and patterns of practice, transforming Canada’s healthcare system. A report from the Institute of Medicine (now called the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine) (2011) stated that nurses, because of their adaptive capacity, have the ability to “lead in the improvement and redesign of the health care system and its many practice environments” (p. 3) if enabled to practice to their full capabilities.
Conclusion
NPs are well prepared to develop and lead initiatives to ensure that patients with cancer receive high-quality care (Spross & Heaney, 2000). NPs should not be regarded as cheap labor in a traditional system. Instead, they are best thought of as high-level providers who infuse a new perspective on health and health care and provide thorough, holistic care that reduces unnecessary resource use by responding proactively to patient need. NP role implementation and sustainability depend on cooperation, leadership, and research that will establish the foundation for the role and an appreciation for its capacity to transform care delivery in the contemporary healthcare system (DiCenso & Bryant-Lukosius, 2010; Lowe et al., 2012).
[[{"type":"media","view_mode":"media_original","fid":"24591","attributes":{"alt":"","class":"media-image","height":"530","typeof":"foaf:Image","width":"365"}}]]
References
Andregárd, A.C., & Jangland, E. (2015). The tortuous journey of introducing the nurse practitioner as a new member of the healthcare team: A meta-synthesis. Scandinavian Journal of Caring Sciences, 29, 3–14. doi:10.1111/scs.12120
Bakker, D., Strickland, J., MacDonald, C., Butler, L., Fitch, M., Olson, K., & Cummings, G. (2013). The context of oncology nursing practice: An integrative review. Cancer Nursing, 36, 72–88. doi:10.1097/NCC.0b013e31824afadf
Bishop, C.S. (2009). The critical role of oncology nurse practitioners in cancer care: Future implications. Oncology Nursing Forum, 36, 267–269. doi:10.1188/09.ONF.267-269
Brown, M.A., & Draye, M.A. (2003). Experiences of pioneer nurse practitioners in establishing advanced practice roles. Journal of Nursing Scholarship, 35, 391–397. doi:10.1111/j.1547-5069.2003.00391.x
Brown, S.A., & Grimes, D.E. (1995). A meta-analysis of nurse practitioners and nurse midwives in primary care. Nursing Research, 44, 332–339. doi:10.1097/00006199-199511000-00003
Bryant-Lukosius, D., DiCenso, A., Browne, G., & Pinelli, J. (2004). Advanced practice nursing roles: Development, implementation and evaluation. Journal of Advanced Nursing, 48, 519–529. doi:10.1111/j.1365-2648.2004.03234.x
Bryant-Lukosuis, D., Green, E., Fitch, M., Macartney, G., Robb-Blenderman, L., McFarlane, S., . . . Milne, H. (2007). A survey of oncology advanced practice nurses in Ontario: Profile and predictors of success. Nursing Leadership, 20, 50–68.
Canadian Association of Nurses in Oncology. (2001). Standards of care, roles in oncology nursing, and role competencies. Retrieved from http://www.aqio.org/docs/normes_de_soins_anglais.pdf
Canadian Cancer Society’s Steering Committee on Cancer Statistics. (2012). Canadian cancer statistics 2012. Retrieved from http://bit.ly/25gCLm6
Commission on the Future of Health Care in Canada. (2002). Building on values: The future of health care in Canada—Final report. Retrieved from http://publications.gc.ca/collections/Collection/CP32-85-2002E.pdf
DiCenso, A., & Bryant-Lukosius, D. (2010). The long and winding road: Integration of nurse practitioners and clinical nurse specialists into the Canadian health-care system. Canadian Journal of Nursing Research, 42(2), 3–8.
Gardner, G., Chang, A., & Duffield, C. (2007). Making nursing work: Breaking through the role confusion of advanced practice nursing. Journal of Advanced Nursing, 57, 382–391. doi:10.1111/j.1365-2648.2007.04114.x
Harvey, C., Papps, E., & Roberts, J. (2015). Obstacles that prevent nurse practitioners in New Zealand fulfilling their roles. Primary Health Care, 25(5), 24–29. doi:10.7748/phc.25.5.24.e935
Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine. (2011). The future of nursing: Leading change, advancing health. Washington, DC: National Academies Press.
Hopwood, L. (2006). Developing advanced nursing practice roles in cancer care. Nursing Times, 102(15), iv–v.
Horrocks, S., Anderson, E., & Salisbury, C. (2002). Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. British Medical Journal, 324, 819–823. doi:10.1136/bmj.324.7341.819
Hurlock-Chorostecki, C., Forchuk, C., Orchard, C., van Soeren, M., & Reeves, S. (2014). Hospital-based nurse practitioner roles and interprofessional practice: A scoping review. Nursing and Health Sciences, 16, 403–410. doi:10.1111/nhs.12107
Kilpatrick, K., Harbman, P., Carter, N., Martin-Misener, R., Bryant-Lukosius, D., Donald, F., . . . DiCenso, A. (2010). The acute care nurse practitioner role in Canada. Nursing Leadership, 23, 114–139. doi:10.12927/cjnl.2010.22272
Kilpatrick, K., Lavoie-Tremblay, M., Lamothe, L., Ritchie, J.A., & Doran, D. (2013). Conceptual framework of acute care nurse practitioner role enactment, boundary work, and perceptions of team effectiveness. Journal of Advanced Nursing, 69, 205–217.
Kleinpell, R.M., Hudspeth, R., Scordo, K.A., & Magdic, K. (2012). Defining NP scope of practice and associated regulations: Focus on acute care. Journal of the American Academy of Nursing Practitioners, 24, 11–18. doi:10.1111/j.1745-7599.2011.00683.x
Lowe, G., Plummer, V., O’Brien, A.P., & Boyd, L. (2012). Time to clarify—The value of advanced practice nursing roles in health care. Journal of Advanced Nursing, 68, 677–685. doi:10.1111/j.1365-2648.2011.05790.x
Mayan, M.J. (2009). Essentials of qualitative inquiry. Walnut Creek, CA: Left Coast Press.
Naylor, M.D., & Kurtzman, E.T. (2010). The role of nurse practitioners in reinventing primary care. Health Affairs, 29, 893–899. doi:10.1377/hlthaff.2010.0440
Pringle, D. (2007). Nurse practitioner role: Nursing needs it. Nursing Leadership, 20(2), 1–5. doi:10.12927/cjnl.2007.18894
Spross, J.A., & Heaney, C.A. (2000). Shaping advanced nursing practice in the new millennium. Seminars in Oncology Nursing, 16, 12–24. doi:10.1016/S0749-2081(00)80004-2
Thorne, S. (2008). Interpretive description. Walnut Creek, CA: Left Coast Press.
Thorne, S., Reimer Kirkham, S.R., & MacDonald-Emes, J. (1997). Interpretive description: A noncategorical qualitative alternative for developing nursing knowledge. Research in Nursing and Health, 20, 169–177. doi:10.1002/(SICI)1098-240X(199704)20:2<169::AID-NUR9>3.0.CO;2-I
Thorne, S., Reimer Kirkham, S., & O’Flynn-Magee, K. (2004). The analytic challenge in interpretive description. International Journal of Qualitative Methods, 3, 1–11.
About the Author(s)
Stahlke Wall is an associate professor in the Faculty of Nursing at the University of Alberta in Edmonton, and Rawson is a senior practice consultant of advanced practice nursing and a nurse practitioner for Alberta Health Services–CancerControl in Calgary, both in Canada. Stahlke Wall received an honorarium from the Canadian Association of Nurses in Oncology for a webinar presentation on the findings of this research. Both authors contributed to the conceptualization and design of the study and the preparation of the manuscript. Stahlke Wall completed the data collection and analysis, with input from Rawson. Stahlke Wall can be reached at sarah.stahlke@ualberta.ca, with copy to editor at ONFEditor@ons.org. Submitted March 2015. Accepted for publication August 20, 2015.

