Perceived Needs, Preparedness, and Emotional Distress of Male Caregivers of Postsurgical Women With Gynecologic Cancer
Objectives: To describe the perceived needs, preparedness, and emotional distress of male caregivers of postsurgical patients with gynecologic cancer during the transition from hospital to home.
Sample & Setting: 50 male caregivers of patients with gynecologic cancer on an inpatient unit at University Hospitals Seidman Cancer Center in Cleveland, OH.
Methods & Variables: Caregiver needs, perceived preparedness, and emotional distress were measured at admission and at one week postdischarge. Instruments included the Comprehensive Needs Assessment Tool for Cancer Caregivers, Preparedness for Caregiving Scale, and National Comprehensive Cancer Network Distress Thermometer. The analysis consisted of descriptive statistics, Spearman’s correlations, and univariate linear regressions.
Results: At both time points, male caregivers’ greatest needs were interaction with the healthcare staff and information. Perceived preparedness was not associated with emotional distress. Male caregivers who were young, were employed, were unmarried, and had a lower income had greater needs.
Implications for Nursing: A relational nursing care approach that maintains effective communication with male caregivers is essential. Nurses should broaden the caregiver assessment beyond the practical care of the patient.
Jump to a section
Surgical patients with gynecologic cancer often are discharged to their home with a new or recurrent cancer diagnosis and with multiple complex postsurgical needs. Physical needs related to surgical incision care, pain management, drain or ostomy care, and nutrition may be accompanied by significant emotional or psychological reactions of distress, anxiety, depression, and uncertainty (Schulman-Green, Ercolano, Dowd, Schwartz, & McCorkle, 2008). Family caregivers play a pivotal role during this transition in promoting physical and psychological recovery and in preventing unplanned readmission to the hospital. The readmission rate in an analysis of 12,804 patients who had undergone gynecologic cancer surgery was 6.5%, with about 75% of readmissions occurring within the first two weeks after discharge (Uppal et al., 2016).
The hospital-to-home transition after surgery is a critical period during which family caregivers assume a great deal of responsibility and burden. Family caregivers of individuals with cancer report being unprepared and lacking skills to assume the broad scope of clinical caregiving tasks that include managing symptoms and pain, administering medications, changing bandages, and monitoring tubes, lines, and appliances (van Ryn et al., 2011). Although most family caregivers are typically female (National Alliance for Caregiving and AARP Public Policy Institute, 2015), in the gynecologic cancer population, a large proportion of caregivers are likely to be male. However, little is known about the experiences and needs of male caregivers during the postsurgical transition.
Background
In general, male caregivers are described as experiencing less depression, burden, and negative aspects of caregiving than female caregivers (Li, Mak, & Loke, 2013; Nijboer et al., 2000; Pinquart & Sörensen, 2006). These gender differences may subside in certain subgroups. In a study of 429 caregivers of cancer survivors, Kim, Loscalzo, Wellisch, and Spillers (2006) found that male spousal caregivers were more distressed than female counterparts when their wives had poorer psychosocial functioning. In addition, they noted that poorer physical functioning of the care recipient was associated with greater stress in the caregiver, regardless of caregiver gender (Kim et al., 2006).
Studies have found that male caregivers believe caregiving involves achieving competency for the essential caregiving tasks, which can lead to feelings of satisfaction and mastery (Ussher & Sandoval, 2008). However, they view dealing with a care recipient’s emotions as a negative aspect of caregiving and have difficulty expressing their emotions (Li et al., 2013; Ussher & Sandoval, 2008). Beyond the adjustment of assuming the caregiving role, in the early recovery period, male partners of women with gynecologic cancer often must learn to cope with communication and intimacy issues (Maughan, Heyman, & Matthews, 2002). The findings of a qualitative study of male caregivers of women with breast and gynecologic cancer suggest that men may not express their concerns and stress openly and have difficulty identifying supportive resources (Lopez, Copp, & Molassiotis, 2012). These characteristics, along with inadequate identification of learning needs by clinicians, can place male caregivers at risk for being unprepared for caregiving during the postsurgical transition. Lack of preparedness for the caregiving role can cause further stress in male caregivers (Li et al., 2013).
Caregiver Preparedness
Preparedness is defined as a caregiver’s perceived readiness for the caregiving role, which encompasses multiple domains, including provision of physical care, emotional support, and instrumental support (Schumacher, Stewart, & Archbold, 1998). It differs from the concept of self-efficacy in that it refers to broad domains of caregiving, rather than confidence for performing a specific caregiving task (Archbold, Stewart, Greenlick, & Harvath, 1990). Limited research explores the concept of preparedness in family caregivers of patients with cancer. In a study of 87 family caregivers during cancer treatment, increased caregiver preparedness was associated with decreased fatigue and mood disturbance, and was found to interact with mutuality (relationship quality) in buffering stress responses to high caregiver demands (Schumacher et al., 2008; Schumacher, Stewart, & Archbold, 2007). Similarly, Fujinami et al. (2015) reported a significant inverse association between preparedness and distress in 163 family caregivers of patients with lung cancer in an outpatient medical oncology setting. Scherbring (2002) examined the preparedness of caregivers during the transition from hospital to home in a sample of 59 nonsurgical inpatients with cancer who had mixed diagnoses. The significant inverse relationship between preparedness and caregiver burden was constant from predischarge to one month postdischarge, and for every one unit increase in preparedness, the burden score decreased by about 17% (Scherbring, 2002).
Research supports the development of interventions that target caregiver preparedness because it is a key factor in caregiver physical and psychological well-being. However, more research is needed to describe preparedness and other factors that may influence the transition after surgery in subgroups of caregivers, such as male caregivers, who are often underrepresented in research studies. In addition, no studies were identified that explored perceived needs of family caregivers in relation to preparedness and distress.
The primary aim of this study was to describe the perceived needs, preparedness, and emotional distress of male caregivers of postsurgical patients with gynecologic cancer during the transition from the hospital to home. Secondary aims were to describe the following:
• Correlates of male caregiver needs, preparedness, and distress
• The relationship between distress and preparedness
• The moderating role of distress on the relationship between preparedness and perceived needs
• The relationship between caregiver preparedness and patient readmission within 30 days postdischarge
Methods
Design, Sample, and Setting
A descriptive, correlational design was used to describe the relationships among needs, preparedness, and emotional distress within 48–72 hours of admission and five to seven days postdischarge. The study was approved by the University Hospitals Case Medical Center Institutional Review Board. From August 2014 to March 2015, a convenience sample of patients and family caregivers was obtained from the gynecologic/oncology inpatient unit at the University Hospitals Seidman Cancer Center, which is a member of the National Cancer Institute–designated Comprehensive Cancer Center of Case Western Reserve University in Cleveland, Ohio.
Adult gynecologic inpatients, with or without a cancer diagnosis, who underwent a surgical procedure, chemotherapy, radiation therapy, and/or symptom management, were included. All surgical inpatients were enrolled because the final diagnostic pathology report was not available until after discharge at the postoperative follow-up appointment. Inclusion criteria for family caregivers were as follows: (a) adult male, aged 18 years or older, (b) designated by the patient as the primary caregiver, and (c) able to speak and understand English. Caregivers of patients who actively were dying or who were in the process of establishing hospice care at discharge were excluded.
Potential participants were identified from review of the daily admission schedules to the gynecologic/oncology unit by the research nurse, who was also the care coordinator on the unit. Further identification of patients with male caregivers occurred through chart review and during routine interdisciplinary patient rounds, within 48 hours of admission. Verbal consent and permission to contact the caregiver were obtained from the patient. The male caregiver then was invited to participate in the study, and written consent was obtained. Caregivers completed surveys in person within 48–72 hours of admission and then via telephone five to seven days postdischarge.
Measures
Preparedness: Caregiver-perceived preparedness was measured using the Preparedness for Caregiving Scale (PCS) of the Family Care Inventory (Archbold et al., 1990). This is a self-report instrument that consists of eight items that represent the domains of caregiving, such as attending to physical and emotional needs, setting up support services, coping with the stress of caregiving, responding to emergencies, and accessing resources and information. One question asks the caregiver to rate his overall global assessment of preparedness. Responses are rated on a five-point Likert-type scale, with scores ranging from 0 (not at all prepared) to 4 (very well prepared). A mean score for the eight items is calculated, with higher scores indicating more perceived preparedness. Reliability and validity of the PCS has been supported in caregiver samples in palliative care and oncology (Henriksson et al., 2015; Schumacher et al., 2008). The Cronbach alpha was 0.895 in the current study.
Caregiver needs: Caregiver needs were assessed using the Comprehensive Needs Assessment Tool for Cancer Caregivers (CNAT-C) (Shin et al., 2011), which is a 41-item self-report survey with seven domains. The health and psychological problems domain (six items) assesses needs related to caregiver health, patient concerns, depression, anger, loneliness, and anxiety. The family/social support domain (five items) addresses needs concerning help with patient overdependence, lack of appreciation with caregiving, family and interpersonal relationships, and caregiver relaxation and personal life. Needs related to interactions with physicians, communication, decision making, and relationship with nurses (e.g., empathy, instructions, attention to the patient) are assessed with the healthcare staff domain (eight items). The informational and educational domain (eight items) evaluates needs related to information about the patient’s illness, tests, treatments, and care, as well as complementary and alternative medicine, hospitals and physicians, financial support, communication, and caregiver stress management. The domain of needs for religious support and finding meaning in the situation is assessed with two items. The hospital facilities and services domain (six items) covers needs related to counseling, navigation and guidance, space for caregivers, home care, and opportunities to talk with other caregivers. Lastly, the practical support domain (six items) evaluates needs related to transportation, lodging, financial assistance, care assistance, and help with housekeeping and child care. Caregivers rated the extent to which a need existed within the past week on a four-point Likert-type scale ranging from 0 (no need) to 3 (high need). Scoring of the CNAT-C involves calculating an average score for each domain and then using linear transformation to a scale of 0–100 (Zhang et al., 2015). Reliability and content validity of the CNAT-C has been supported (Shin et al., 2011). In the current study, the Cronbach alpha for the total scale was 0.959, and the Cronbach alphas for the subscales ranged from 0.625 (religious and spiritual support subscale) to 0.923 (healthcare staff subscale).
Emotional distress: Using the National Comprehensive Cancer Network ([NCCN], 2017) Distress Thermometer (DT), participants rated their level of emotional distress during the past week on a single-item scale ranging from 0 (no distress) to 10 (extreme distress). The validity of the DT as a clinical screening tool for distress in family members of patients with cancer has been supported (Zwahlen, Hagenbuch, Carley, Recklitis, & Buchi, 2008).
Other measures: Information regarding age, race, ethnicity, marital status, employment status, education, income, and living arrangement were collected from caregivers and patients. The caregiver’s relationship to the patient, assistance in providing care, and whether he was providing care to another person were assessed. At enrollment, caregivers reported their chronic health conditions and rated their overall health and quality of life as excellent, very good, good, fair, or poor. Information regarding cancer diagnosis, type of surgery, stage of cancer, recurrence, previous and concurrent treatments, performance status, discharge disposition, and length of hospitalization was collected from the patient’s medical record. Whether a patient was readmitted to the hospital within 30 days of discharge was noted with the readmission diagnosis.
Data Analyses
Data were analyzed using IBM SPSS Statistics, version 24.0, R version 3.1.2, and SAS 9.4. Scores for the total CNAT-C and subscales were transformed to a scale of 0–100. Frequency tables with means and standard deviations were generated to describe the distribution of the main outcomes (total CNAT-C and subscales, total preparedness score, and distress score) at time 1 (within 48–72 hours of hospitalization) and time 2 (five to seven days postdischarge). Paired t tests were used to compare the means of each of the main outcomes at time 1 and 2. For each of the main outcomes, covariates, including patient age, cancer stage, caregiver age, caregiver marital status, caregiver employment, and caregiver socioeconomic status, were assessed univariately at each time point. The association between preparedness and emotional distress was assessed by Spearman’s correlation as well as univariate linear regression at each time point. Similarly, the relationships between preparedness and the CNAT-C subscales were assessed by Spearman’s correlation and univariate linear regression at each time point. Alpha was set at 0.05.
Results
Sample Characteristics
Of the 236 patients screened, 137 (58%) did not qualify because of the caregiving situation (female caregiver, no caregiver, inconsistent caregivers, and hospice), and 34 caregivers were missed because of scheduling. Fifty male caregivers and their care recipients participated in the study, representing a 77% enrollment rate. However, seven caregivers did not complete the surveys at time 2; four were lost to follow-up, and three had a change in patient medical status. When comparing caregiver dropouts to caregivers who completed the study, statistically significant differences were found for three variables. Caregivers who did not respond to the survey at time 2 were more likely to be in a nonspousal relationship with the patient (chi-square[1, n = 49] = 12.58, p = 0.000), have other assistance in caring for the patient (chi-square[1, n = 49] = 3.86, p = 0.049), and be caring for a patient having a readmission within 30 days of discharge (chi-square[1, n = 49] = 10.04, p = 0.002). No statistical differences were found on baseline scores for preparedness, distress, and needs.
[[{"type":"media","view_mode":"media_original","fid":"39976","attributes":{"alt":"","class":"media-image","height":"576","typeof":"foaf:Image","width":"300"}}]]
The mean age was 60.64 years (SD = 12.53) for caregivers and 60.06 years (SD = 12.1) for patients. Forty-three patients had a cancer diagnosis at the time of enrollment. Of these patients, 11 had a cancer recurrence and 24 had previous treatment. The mean time since diagnosis was 16.49 months (SD = 4.26, median = 3). On average, the length of hospitalization was 6.44 days (SD = 5.32, median = 5). Twelve patients were readmitted within 30 days of diagnosis, most commonly because of wound issues (n = 5), failure to thrive (n = 2), and lack of symptom control (n = 2). The typical caregiver was Caucasian, married, and in a spousal or partner relationship with the patient. Nineteen caregivers reported having other caregiving assistance, and five caregivers were providing care to other individuals. The median number of chronic health conditions reported by caregivers was two, with heart disease, diabetes, and arthritis being the most common. Twenty-five caregivers rated their health as very good or excellent, and 30 rated their quality of life as very good or excellent. Sample demographic and medical characteristics are shown in Tables 1 and 2.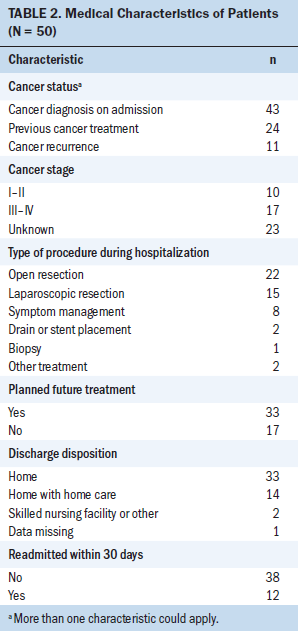
Descriptive Statistics
Table 3 shows the mean scores for CNAT-C subscales, preparedness, and emotional distress. At both time points, male caregivers’ greatest needs were in two domains of the CNAT-C: interaction with the healthcare staff and information. The health and psychological problems domain was the third and fourth greatest area of need within 48–72 hours of admission (time 1) and at five to seven days postdischarge (time 2), respectively. Statistically significant reductions in mean scores at time 2 occurred in the domains of healthcare staff and health and psychological problems. Religious support was the only domain that did not have a reduction in mean scores at time 2. On average, at time 2, perceived preparedness increased and emotional distress decreased, and these changes were statistically significant.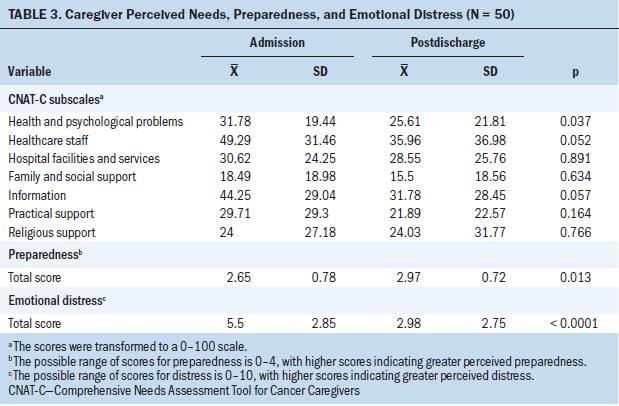
Correlates of Needs, Preparedness, and Distress
During hospitalization (time 1), older caregiver age was significantly associated with fewer needs on four CNAT-C domains: healthcare staff (p = 0.01), information (p = 0.004), hospital facilities and services (p = 0.021), and practical support (p = 0.0001). After discharge (time 2), fewer needs in the domains of information and practical support were significantly associated with older caregiver age (p = 0.017, p = 0.023) and older patient age (p = 0.040, p = 0.02). Employed caregivers, when compared to those who were unemployed, had statistically greater needs in the domain of healthcare staff at time 1 (p = 0.025) and time 2 (p = 0.013). They also had greater needs for information at time 2 (p = 0.01). Married caregivers had fewer needs than unmarried caregivers in the domains of practical support at time 1 (p = 0.031) and family and social support at time 2 (p = 0.026). Reported annual income in two groups ($21,000–$49,000 and greater than $50,000) was associated with fewer needs only in the domain of practical support and only at time 1 (p = 0.05 and p = 0.002, respectively), when compared to the $20,999 or less group.
Cancer stage was the only correlate of perceived preparedness. During hospitalization (time 1), having a stage II cancer diagnosis was associated with significantly greater preparedness than having a stage I cancer diagnosis (p = 0.015). Age, cancer stage, employment, marital status, and annual income were not statistically associated with emotional distress.
Relationships Among Needs, Preparedness, and Distress
Perceived preparedness was not statistically significantly associated with emotional distress at either time point and was related only to the CNAT-C domain of family and social support during hospitalization (time 1). A higher preparedness score was associated with significantly lower needs related to family and social support (p = 0.019).
When controlling for perceived preparedness, increase in distress scores was associated with greater needs at both time points in the CNAT-C domains of health and psychological problems (time 1: p < 0.0001, time 2: p < 0.0001), religious and spiritual support (time 1: p = 0.033, time 2: p = 0.045), and hospital facilities and services (time 1: p = 0.005, time 2: p = 0.049). In addition, greater needs in the domain of family and social support were associated with higher distress scores, when controlling for preparedness, at time 2.
Lastly, the odds of being readmitted to the hospital within 30 days of discharge were not related to perceived preparedness or emotional distress at either time point. Having greater needs in the CNAT-C domain of hospital facilities and services was associated with slightly greater odds of readmission (odds ratio = 1.038, 95% confidence interval [1.007, 1.07], p = 0.016).
Discussion
The current study contributes to the limited body of research describing the experiences of male caregivers by specifically focusing on their perceived needs, preparedness, and distress during the transition from hospital to home. The finding that male caregivers’ greatest needs were related to interactions with healthcare staff and information is consistent with other studies of family caregivers (Dougherty, 2010; Heckel et al., 2015; Lund, Ross, Petersen, & Groenvold, 2015). This is not surprising considering that hospitalization and the transition to home is characterized by uncertainty related to the diagnosis and the patient’s medical condition, ambivalence about assuming the caregiver role, communication with numerous care providers, and the need to learn new skills related to caring for the patient after surgical treatment. This period also may be an emotional time for the caregiver if a new diagnosis is made or if a change in the status of the patient occurs. However, the focus of care is often patient-centered, rather than family-centered, and caregivers, as described in a qualitative study by Foust, Vuckovic, and Henriquez (2012), assume a “peripheral status in care transitions” (p. 206). Caregivers want to be acknowledged and recognized during interactions with healthcare professionals (Harding et al., 2012; Lund et al., 2015).
An important finding in the current study was that emotional distress was not related to perceived preparedness, which infers that a nurse cannot assume that a prepared caregiver has less distress and vice versa. This finding contrasts with findings by Fujinami et al. (2015), who reported a significant inverse association between preparedness and distress in family caregivers of patients with lung cancer receiving outpatient treatment. Distress is a multidimensional experience with multiple triggers (NCCN, 2017), and although sources of distress were not measured in the current study, the male caregivers may have experienced distress associated with factors other than preparedness (e.g., the wait for surgery results, the hospital environment, concern for their loved one). The trajectory of high caregiver distress during the hospitalization period with lower distress after discharge in the current study contrasts with the findings of Kim et al. (2016), who found that distress levels in 41 family caregivers of individuals having lung cancer surgery, as measured with the DT, remained elevated at 6 and 12 weeks after surgery. Cancer diagnoses, prognoses, and surgical procedures likely may account for the difference in results between the two studies.
Limitations
A limitation of the current study was that data were collected by the care coordinator on the unit, who also was responsible for discharge of the patient. Although strategies were enacted to reduce bias, some participants’ responses may have been influenced by this relationship. Also, sample characteristics and the use of a small convenience sample on a single hospital unit limits generalizability. In addition, differences in participants who did not respond at time 2 were significant and could represent a subgroup whose responses may have altered the study results.
Implications for Nursing
The importance of engaging family caregivers in transitional care has been affirmed with the Caregiver Advise, Record, and Enable (CARE) Act (Reinhard & Ryan, 2016). Focused on hospitalization, this legislation has the following three main provisions (Reinhard & Ryan, 2016):
• A family caregiver must be recorded in the medical record.
• The family caregiver must be notified of when the patient is to be discharged.
• The family caregiver must receive in-person instructions about how to perform medical tasks at home for the patient.
These are essential elements of good transitional care (Coleman, 2016) and represent a critical first step in addressing preparation of family caregivers. The findings from the current study—that male caregivers have strong needs for a relationship with the healthcare team and for information—suggest that a relational, family-centered approach also is needed during hospitalization, encompassing routine caregiver assessment, communication, support, and education and training. Communication and interactions that promote relational nursing practice can be extended to family caregivers. A fundamental aspect of relational care for family caregivers is to respectfully acknowledge the caregiver’s presence. Relational inquiry, as described by Doane and Varcoe (2007), is a reflexive process by which nurses move beyond superficial interactions with patients (or caregivers) to understand their unique perspectives, values, goals, and experiences. Asking the caregivers questions, inquiring about their needs and concerns, including the caregivers in discussions, and allowing them to tell their story of caregiving are strategies to support the caregivers, as well as a means to more fully understand the context of the caregiving situation.
Proactively assessing caregiver needs for information is essential, because lack of emotional and informational support has been found to be associated with borderline or clinical anxiety and depression in family caregivers of individuals with cancer (Lambert, Girgis, Lecathelinais, & Stacey, 2013). The scope of caregiver assessment is broad and should include caregiver willingness and capability to assume the caregiving role, including the following (Given, Given, & Sherwood, 2012):
• Caregiver physical and mental health
• Perceived burden
• Competing work and family demands
• Social support and resources
• Unmet training and educational needs regarding practical care of the patient prior to the transition
The current study highlighted subgroups of male caregivers that require a more in-depth assessment of needs—those who are young, are employed, are unmarried, and have a low income. Nurses should screen separately for emotional distress and preparedness and be aware that despite caregivers’ perception of preparedness, their distress may be significant and warrant further evaluation. In the current study, caregivers with elevated distress were more likely to have greater needs during hospitalization and at five to seven days postdischarge. Online tools for assessing caregiver needs specifically for the postdischarge transition can be found at www.nextstepincare.org. 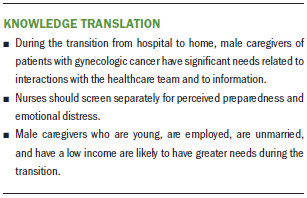
Conclusion
During the transition from hospital to home, male caregivers of patients with gynecologic cancer have significant needs related to interactions with the healthcare team and information. Strategies to enhance relational nursing care and maintain effective communication with male caregivers are essential, as is proactive, comprehensive assessment of caregivers. More studies of male caregivers that focus on care transitions with other cancer populations are needed to design interventions that meet their unique needs.
[[{"type":"media","view_mode":"media_original","fid":"39986","attributes":{"alt":"","class":"media-image","height":"272","typeof":"foaf:Image","width":"626"}}]]
About the Author(s)
Susan R. Mazanec, PhD, RN, AOCN®, is an assistant professor in the Frances Payne Bolton School of Nursing at Case Western Reserve University in Cleveland, OH; Dianne Reichlin, MSN, RN, is an inpatient oncology RN at the Lee Memorial Hospital and Regional Cancer Center in Fort Myers, FL; Haley Gittleman, MS, is a biostatistician in the School of Medicine and the Case Comprehensive Cancer Center at the Case Western Reserve University; and Barbara J. Daly, PhD, RN, FAAN, is a Gertrude Perkins Oliva professor in oncology nursing in the Frances Payne Bolton School of Nursing at Case Western Reserve University. During the writing of this article, Daly was supported by funding from the the National Institutes of Nursing Research, the National Cancer Institute, and the Centers for Medicare and Medicaid Services. Mazanec, Reichlin, and Daly contributed to the conceptualization and design and the manuscript preparation. Reichlin completed the data collection. Mazanec and Gittleman provided statistical support. Mazanec, Gittleman, and Daly provided the analysis. Mazanec can be reached at susan.mazanec@case.edu, with copy to ONFEditor@ons.org. (Submitted July 2017. Accepted September 19, 2017.)
References
Archbold, P.G., Stewart, B.J., Greenlick, M.R., & Harvath, T. (1990). Mutuality and preparedness as predictors of caregiver role strain. Research in Nursing and Health, 13, 375–384.
Coleman, E.A. (2016). Family caregivers as partners in care transitions: The caregiver advise record and enable act. Journal of Hospital Medicine, 11, 883–885. https://doi.org/10.1002/jhm.2637
Doane, G.H., & Varcoe, C. (2007). Relational practice and nursing obligations. Advances in Nursing Science, 30, 192–205. https://doi.org/10.1097/01.ANS.0000286619.31398.fc
Dougherty, M. (2010). Assessment of patient and family needs during an inpatient oncology experience. Clinical Journal of Oncology Nursing, 14, 301–306. https://doi.org/10.1188/10.CJON.301-306
Foust, J.B., Vuckovic, N., & Henriquez, E. (2012). Hospital to home health care transition: Patient, caregiver, and clinician perspectives. Western Journal of Nursing Research, 34, 194–212. https://doi.org/10.1177/0193945911400448
Fujinami, R., Sun, V., Zachariah, F., Uman, G., Grant, M., & Ferrell, B. (2015). Family caregivers’ distress levels related to quality of life, burden, and preparedness. Psycho-Oncology, 24, 54–62. https://doi.org/10.1002/pon.3562
Given, B.A., Given, C.W., & Sherwood, P.R. (2012). Family and caregiver needs over the course of the cancer trajectory. Journal of Supportive Oncology, 10, 57–64. https://doi.org/10.1016/j.suponc.2011.10.003
Harding, R., Epiphaniou, E., Hamilton, D., Bridger, S., Robinson, V., George, R., . . . Higginson, I.J. (2012). What are the perceived needs and challenges of informal caregivers in home cancer palliative care? Qualitative data to construct a feasible psycho-educational intervention. Supportive Care in Cancer, 20, 1975–1982. https://doi.org/10.1007/s00520-011-1300-z
Heckel, L., Fennell, K.M., Reynolds, J., Osborne, R.H., Chirgwin, J., Botti, M., . . . Livingston, P.M. (2015). Unmet needs and depression among carers of people newly diagnosed with cancer. European Journal of Cancer, 51, 2049–2057. https://doi.org/10.1016/j.ejca.2015.06.129
Henriksson, A., Hudson, P., Öhlen, J., Thomas, K., Holm, M., Carlander, I., . . . Arestedt, K. (2015). Use of the Preparedness for Caregiving Scale in palliative care: A Rasch evaluation study. Journal of Pain and Symptom Management, 50, 533–541. https://doi.org/10.1016/j.jpainsymman.2015.04.012
Kim, J.Y., Sun, V., Raz, D.J., Williams, A.C., Fujinami, R., Reckamp, K., . . . Ferrell, B. (2016). The impact of lung cancer surgery on quality of life trajectories in patients and family caregivers. Lung Cancer, 101, 35–39. https://doi.org/10.1016/j.lungcan.2016.08.011
Kim, Y., Loscalzo, M.J., Wellisch, D.K., & Spillers, R.L. (2006). Gender differences in caregiving stress among caregivers of cancer survivors. Psycho-Oncology, 15, 1086–1092. https://doi.org/10.1002/pon.1049
Lambert, S.D., Girgis, A., Lecathelinais, C., & Stacey, F. (2013). Walking a mile in their shoes: Anxiety and depression among partners and caregivers of cancer survivors at 6 and 12 months post-diagnosis. Supportive Care in Cancer, 21, 75–85. https://doi.org/10.1007/s00520-012-1495-7
Li, Q.P., Mak, Y.W., & Loke, A.Y. (2013). Spouses’ experience of caregiving for cancer patients: A literature review. International Nursing Review, 60, 178–187. https://doi.org/10.1111/inr.12000
Lopez, V., Copp, G., & Molassiotis, A. (2012). Male caregivers of patients with breast and gynecologic cancer: Experiences from caring for their spouses and partners. Cancer Nursing, 35, 402–410. https://doi.org/10.1097/NCC.0b013e318231daf0
Lund, L., Ross, L., Petersen, M.A., & Groenvold, M. (2015). The interaction between informal cancer caregivers and health care professionals: A survey of caregivers’ experiences of problems and unmet needs. Supportive Care in Cancer, 23, 1719–1733. https://doi.org/10.1007/s00520-014-2529-0
Maughan, K., Heyman, B., & Matthews, M. (2002). In the shadow of risk. How men cope with a partner’s gynaecological cancer. International Journal of Nursing Studies, 39, 27–34.
National Alliance for Caregiving and AARP Public Policy Institute. (2015). Caregiving in the U.S. 2015. Retrieved from https://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united…
National Comprehensive Cancer Network. (2017). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Distress management [v.2.2017]. Retrieved from https://www.nccn.org/professionals/physician_gls/PDF/distress.pdf
Nijboer, C., Triemstra, M., Tempelaar, R., Mulder, M., Sanderman, R., & van den Bos, G.A. (2000). Patterns of caregiver experiences among partners of cancer patients. Gerontologist, 40, 738–746.
Pinquart, M., & Sörensen, S. (2006). Gender differences in caregiver stressors, social resources, and health: An updated meta-analysis. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 61, P33–P45.
Reinhard, S., & Ryan, E. (2016, June 7). Stepping up to support family caregivers. AARP. Retrieved from https:// http://blog.aarp.org/2016/06/07/stepping-up-to-support-family-caregivers
Scherbring, M. (2002). Effect of caregiver perception of preparedness on burden in an oncology population [Online exclusive]. Oncology Nursing Forum, 29, E70–E76. https://doi.org/10.1188/02.ONF.E70-E76
Schulman-Green, D., Ercolano, E., Dowd, M., Schwartz, P., & McCorkle, R. (2008). Quality of life among women after surgery for ovarian cancer. Palliative and Supportive Care, 6, 239–247. https://doi.org/10.1017/S1478951508000497
Schumacher, K.L., Stewart, B.J., & Archbold, P.G. (1998). Conceptualization and measurement of doing family caregiving well. Image—The Journal of Nursing Scholarship, 30, 63–69.
Schumacher, K.L., Stewart, B.J., & Archbold, P.G. (2007). Mutuality and preparedness moderate the effects of caregiving demand on cancer family caregiver outcomes. Nursing Research, 56, 425–433. https://doi.org/10.1097/01.NNR.0000299852.75300.03
Schumacher, K.L., Stewart, B.J., Archbold, P.G., Caparro, M., Mutale, F., & Agrawal, S. (2008). Effects of caregiving demand, mutuality, and preparedness on family caregiver outcomes during cancer treatment. Oncology Nursing Forum, 35, 49–56. https://doi.org/10.1188/08.ONF.49-56
Shin, D.W., Park, J.H., Shim, E.J., Park, J.H., Choi, J.Y., Kim, S.G., & Park, E.C. (2011). The development of a comprehensive needs assessment tool for cancer-caregivers in patient-caregiver dyads. Psycho-Oncology, 20, 1342–1352. https://doi.org/10.1002/pon.1857
Uppal, S., Penn, C., Del Carmen, M.G., Rauh-Hain, J.A., Reynolds, R.K., & Rice, L.W. (2016). Readmissions after major gynecologic oncology surgery. Gynecologic Oncology, 141, 287–292.
Ussher, J.M., & Sandoval, M. (2008). Gender differences in the construction and experience of cancer care: The consequences of the gendered positioning of carers. Psychology and Health, 23, 945–963. https://doi.org/10.1080/08870440701596585
van Ryn, M., Sanders, S., Kahn, K., van Houtven, C., Griffin, J.M., Martin, M., . . . Rowland, J. (2011). Objective burden, resources, and other stressors among informal cancer caregivers: A hidden quality issue? Psycho-Oncology, 20, 44–52. https://doi.org/10.1002/pon.1703
Zhang, Y.P., Zhao, X.S., Zhang, B., Zhang, L.L., Ni, C.P., Hao, N., . . . Porr, C. (2015). Cross-cultural adaptation and psychometric assessment of the Chinese version of the comprehensive needs assessment tool for cancer caregivers (CNAT-C). Quality of Life Research, 24, 1607–1614. https://doi.org/10.1007/s11136-014-0891-5
Zwahlen, D., Hagenbuch, N., Carley, M.I., Recklitis, C.J., & Buchi, S. (2008). Screening cancer patients’ families with the Distress Thermometer (DT): A validation study. Psycho-Oncology, 17, 959–966. https://doi.org/10.1002/pon.1320




