Use of Virtual Reality to Distract From Pain and Anxiety
Objectives: To determine the effects of a virtual reality intervention on pain and anxiety in patients undergoing a bone marrow aspiration and biopsy procedure.
Sample & Setting: 97 adults in an outpatient cancer center in the midwestern United States.
Methods & Variables: In this quasiexperimental study, participants were assigned to either the experimental group (use of virtual reality goggles) or the control group (standard treatment). Vital signs, pain, and anxiety were measured before and after the procedure. T tests and chi-square tests were used to compare the two groups based on demographic data, pain, anxiety, and total amount of medication used during the procedure.
Results: Participants who wore virtual reality goggles during a bone marrow aspiration and biopsy procedure did not experience a statistically significant decrease in pain and anxiety. However, the experimental and control groups showed a decrease in pain and anxiety levels from pre- to postprocedure.
Implications for Nursing: Virtual reality goggles may be a feasible, noninvasive alternative to traditional pharmacologic treatment. The cost of any intervention would need to be considered. Virtual reality should be researched and adapted to benefit patients in appropriate settings.
Jump to a section
Examination of bone marrow is an important aspect of the diagnosis and management of hematologic diseases, including various cancers. Patients undergoing the bone marrow aspiration and biopsy procedure commonly experience pain, anxiety, and stress (Degen, Christen, Rovo, & Gratwohl, 2010). However, distraction has been shown to be a useful nonpharmacologic intervention to decrease pain and anxiety (Hjortholm, Jaddini, Hałaburda, & Snarski, 2013). The purpose of the current study was to determine if the use of virtual reality goggles involving visual and auditory stimuli would decrease the amount of pain and anxiety experienced by patients during the bone marrow aspiration and biopsy procedure, as compared to the practice of viewing a television with sound.
Bone Marrow Aspiration and Biopsy
Hematologic malignancies, such as leukemia, non-Hodgkin lymphoma, Hodgkin lymphoma, and multiple myeloma, may begin in blood-forming tissue (e.g., bone marrow) or in the cells of the immune system (National Cancer Institute, n.d.). The bone marrow aspiration and biopsy procedure is performed during various phases of the patient’s illness, including at diagnosis, during treatment, and during long-term follow-up. The patient is awake and aware of the procedure, which can cause anxiety for the patient because it can be painful and the results may indicate disease presence. In the outpatient setting, limitations exists concerning the amount and type of medication that can be used during the bone marrow aspiration and biopsy procedure. The most common complication is pain, with more than 63% of patients (N = 406) reporting having experienced it in a study by Degan et al. (2010). In another study, 78% of patients reported pain during the bone marrow aspiration and biopsy procedure and 71% of patients reported anxiety (N = 152) (Brunetti et al., 2011). In addition, nurses and physicians were found to underestimate the pain and anxiety levels experienced by patients (Lidén, Olofsson, Landgren, & Johansson, 2012).
A local anesthetic may be given to numb the area above the iliac crest. The inside of the bone is not numbed by the local anesthetic, so patients may feel pain when the bone is penetrated. A small amount of anti-anxiety and pain medications can be given for this procedure (e.g., lorazepam and fentanyl citrate lozenges). However, in one study, the negative side effects of premedications were reported as drowsiness, tiredness, dizziness, and nausea (Degen et al., 2010).
Theoretical Framework
The use of virtual reality goggles to reduce pain and anxiety during the bone marrow aspiration and biopsy procedure is based on the concept that the perception of pain can be controlled because an individual is able to process only a limited amount of information at once (Wint, Eshelman, Steele, & Guzzetta, 2002). As such, the use of virtual reality during painful procedures may serve as a distraction. In addition, human information processing is limited if an individual’s attention is predominantly engaged in a specific task because the attention available for another task is also restricted (Wahn & König, 2017). The virtual reality goggles fit tightly on the face, blocking out negative stimuli (e.g., laboratory technician setup of biopsy tray, preparation of slides and equipment for procedure, sound of needle penetrating bone).
Review of the Literature
Nonpharmacologic measures exist in the hospital and ambulatory settings to decrease or control side effects in patients with cancer. A systematic review by Chirico et al. (2016) found that the use of virtual reality goggles during cancer treatment improved emotional well-being and decreased cancer-related side effects, such as stress, anxiety, and fear. In a case study, Gershon, Zimand, Lemos, Rothbaum, and Hodges (2003) observed that an eight-year-old child with cancer had lower pain and anxiety ratings, reduced pulse, and fewer observed behavioral indices of distress during port access with interactive virtual reality distraction, compared to non-virtual reality distraction on a computer screen. The use of virtual reality goggles results in a positive environment for patients and offers a calming experience by altering their perceptions of time (Schneider & Hood, 2007). This research demonstrates that virtual reality goggles offer an alternative to pain medication or a reduction in dosage of pain medication.
Several studies have shown positive effects of virtual reality used as a distraction (Schneider & Hood, 2007; Schneider, Prince-Paul, Allen, Silverman, & Talaba, 2004; Wint et al., 2002; Wolitzky, Fivush, Zimand, Hodges, & Rothbaum, 2005), and a number of studies have reported decreased chemotherapy-related side effects in adults. In studies involving children, virtual reality has been examined for its ability to distract and alleviate stress during painful procedures (Wint et al., 2002; Wolitzky et al., 2005), including dressing changes of chronic wounds on lower limbs (Hua, Qiu, Yao, Zhang, & Chen, 2015).
Virtual reality also has been proven to reduce the vividness of memories one week later in a simulated dental context (patients listened to an audio recording of a dental procedure, such as cavity filling or tooth extraction, as they sat in a dental chair in a simulated dental office environment); a greater reduction in memory vividness was shown in participants with higher levels of dental anxiety (Tanja-Dijkstra et al., 2014). Walker et al. (2014) found that patients using virtual reality distraction had higher levels of pain and anxiety than the control group; however, these pain and anxiety levels were not significantly different. In the Walker et al. (2014) study, members of the control group had the ability to see their cystoscopy occurring on a display monitor and converse with the urologist, which may have diminished the experience of pain.
Other nonpharmacologic interventions, used as adjuncts to local anesthetics, that have demonstrated some effectiveness in the amount of pain reported include provision of sufficient information about the procedure (Grønkjær et al., 2016), use of different types of biopsy devices (e.g., needle brand, motorized versus nonmotorized needle), hypnosis (Hjortholm et al., 2013), and music therapy (Shabanloei, Golchin, Esfahani, Dolatkhah, & Rasoulian, 2010).
In a review of the literature on the bone marrow aspiration and biopsy procedure, Zahid (2015) concluded that the procedure causes discomfort for most patients, regardless of whether a pharmacologic or nonpharmacologic intervention is employed. Tanasale, Kits, Kluin, Trip, and Kluin-Nelemans (2013) noted that bone marrow biopsies performed by an experienced provider may still cause pain, ranging from mild to severe, and recommended consideration of systemic analgesics and anxiety reduction methods in addition to local anesthetics. Even though the bone marrow aspiration and biopsy procedure was developed in the 19th century, patients continue to report pain, suggesting that the management of this pain has not evolved over time (Hjortholm et al., 2013). Local anesthesia with lidocaine is unable to alleviate all pain during this procedure or the anticipatory anxiety related to recalling the pain thereafter (Cerichione et al., 2017).
Limited research has investigated the use of virtual reality during the bone marrow aspiration and biopsy procedure. Consequently, the purpose of this study was to determine if the use of virtual reality goggles decreased anxiety in adult patients undergoing the bone marrow aspiration and biopsy procedure. Researchers hypothesized (a) that patients who received the virtual reality intervention would report less pain and anxiety following the bone marrow aspiration and biopsy procedure than those who did not receive the intervention and (b) that patients who received the virtual reality intervention would have a decreased need for pain or anxiety medication during the bone marrow aspiration and biopsy procedure than those who did not receive the virtual reality intervention.
Methods
A quasiexperimental research design was used. After being introduced to the study by the clinic nurse and signing an informed consent form, participants were assigned to the experimental group or the control group on an “every-other-one” basis, with even-numbered participants assigned to the virtual reality goggle treatment group and odd-numbered participants assigned to the standard treatment group. During the bone marrow aspiration and biopsy procedure, the experimental group used virtual reality goggles, whereas the control group received standard care, which included watching and listening to a television. A power analysis was not conducted. The sample of 100 patients was based on availability of the target population and the feasibility of completing data collection within six months.
Participants
Participants in this study consisted of individuals who underwent the bone marrow aspiration and biopsy procedure in an outpatient cancer center, the University of Kansas Cancer Center in Westwood. Inclusion criteria for the study were being able to speak English, being aged 18 years or older, and having had at least one bone marrow aspiration and biopsy procedure prior to the study. Exclusion criteria were blindness, concurrent severe mental illness, and inability to answer questions based on the pain and anxiety scales. All other individuals who had had a prior bone marrow aspiration and biopsy procedure, regardless of their ethnic background, age, or gender, could participate if consent was given. Patients were from the general hematology clinic or blood and marrow transplantation clinic, all with a hematologic diagnosis.
Intervention
The intervention involved the use of ezVision X4 virtual reality goggles, which were placed over participants’ eyes before the outpatient procedure began. Participants could choose among three relaxing nature scenes (i.e., babbling brooks, swaying palm trees, or undersea life) that would then be projected through the goggles by a DVD for the duration of the procedure, which lasts, on average, 15 minutes. Participants wore the goggles while lying in the prone position for the bone marrow aspiration and biopsy procedure. Relaxing music was heard through earphones built into the goggles.
Procedure
In 2008, the current authors’ pilot study was approved by the cancer center’s protocol review monitoring committee and the hospital’s human subjects committee, with an accrual of 20 participants. Based on the results of the pilot study, virtual reality was found to be a feasible and potentially useful intervention. A formal study was submitted, approved, and launched in 2010, with an accrual of 100 participants. No major changes were made in the study procedures based on the pilot study.
One week prior to their scheduled bone marrow aspiration and biopsy procedure, patients were telephoned to solicit their interest in participating in the study. If patients met the inclusion criteria, the study was explained and they were given the option to participate. On the day of the bone marrow aspiration and biopsy procedure, patients were provided with the consent form to read. Those participating in the study were escorted to the procedure room, where questions were answered and the consent form was signed following nurse review of the procedure. The participants then completed the pain and anxiety scales. After completion of the scales, the nurse reviewed the procedure again. The provider entered the room and explained how the procedure would be performed. Participants in the experimental group assumed the prone position, and the virtual reality goggles were placed over their eyes. The DVD of relaxing nature scenes was started, based on each participant’s preference. Participants in the control group were placed in the same position and received the standard distraction procedure of viewing relaxing nature scenes on the television and/or listening to music. The provider performed the procedure, and participants then completed the postprocedure surveys regarding this experience and the pain and anxiety experienced.
Measures
The nurse measured vital signs (e.g., blood pressure, pulse, respiration, temperature, oxygen saturation percentage) before and after the bone marrow aspiration and biopsy procedure. Medication used during the procedure and the provider’s perception of the participant’s level of anxiety were recorded. A pain scale and an anxiety scale were used to measure participants’ perceptions of pain and anxiety, respectively.
Pain associated with the procedure was measured with a numerical pain scale (NPS) with vertical numbers ranging from 0 (no pain) to 10 (extreme or most pain possible). Single-item scales have been used successfully in clinical practice and in research involving patients with cancer, chronic pain, and postoperative pain (Harrington, Gilchrist, & Sander, 2014; Kjeldsen, Klaussen, & Rosenberg, 2015). The NPS has a reported reliability of 0.87 and a convergent validity of 0.85; this has been demonstrated across many populations, including patients with breast cancer (Harrington et al., 2014).
Anxiety associated with the procedure was measured with a five-item Likert-type scale ranging from 0 (no anxiety at all) to 4 (very anxious). This scale was based on one used with patients prior to surgery (Kindler, Harms, Amsler, Ihde-Scholl, & Scheidegger, 2000) but was modified slightly to reflect the bone marrow aspiration and biopsy procedure. Kindler et al. (2000) tested the original scale on 685 patients, and it was found to be able to detect patients with high levels of anxiety, especially that related to fear of the unknown, fear of feeling ill, and fear for one’s life. The Cronbach alpha was 0.7.
Data Analysis
Researchers used descriptive statistics, including frequencies and means, to analyze demographic information. T tests and chi-square tests were conducted to compare the experimental and control groups based on their responses to the pain and anxiety scales, as well as the total amount of medication used during the bone marrow aspiration and biopsy procedure. Prior to examining participants’ responses to treatment, independent t tests were used to determine if groups were equivalent. The anxiety scale was analyzed for reliability (Cronbach alpha). In addition, Cohen’s d was used to calculate effect size on variables of interest (i.e., expected pain, actual pain, anxiety, and medication).
Results
Of the 100 participants included in the formal study, 1 had not previously undergone the bone marrow aspiration and biopsy procedure; therefore, that participant’s data were excluded. One participant withdrew from the study, and one participant’s data were not retrieved. Forty-nine individuals were in the experimental group, and 48 individuals received treatment as usual in the control group.
Sample Characteristics
Researchers used t-test values (p < 0.05) and chi-square distributions to determine equivalency of the experimental and control groups at baseline. No statistically significant differences were noted between the groups related to demographic characteristics, percentage of patients with a previous negative experience during the bone marrow aspiration and biopsy procedure, or expected or actual procedural pain levels. Overall, participants’ ages ranged from 19–70 years, with a mean age of 50.2 years (SD = 12.6). Among those in the experimental group (N = 49), the mean age was 51.4 years (SD = 12.4), whereas among those in the control group, the mean age was 48.9 years (SD = 12.8). More than half of the 97 participants were men (n = 52), and 71 had at least some college education (see Table 1). All but one of the participants reported having health insurance. About one-third (n = 33) of the participants reported having a negative experience during a previous bone marrow aspiration and biopsy procedure. 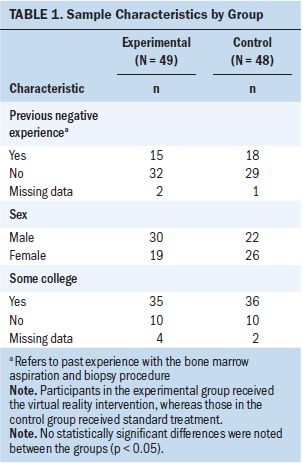
Group Differences on Study Outcomes
Table 2 displays the differences between study groups related to the outcome measures. No statistically significant or clinically meaningful differences were noted between the groups related to the pain or anxiety outcomes. More than half (51%) of the study participants reported some amount of anxiety reduction after the bone marrow aspiration and biopsy procedure, based on their reported anxiety score prior to the procedure. Twenty-eight percent of participants reported an increase in anxiety, and 21% had no change in anxiety level. No significant differences were observed between the groups related to the expected and actual amounts of pain reported. The average number of anti-anxiety and pain medications required by each group did not differ significantly. Twenty participants received anti-anxiety and pain medications during the bone marrow aspiration and biopsy procedure, with 12 of those participants in the control group and 8 in the experimental group. 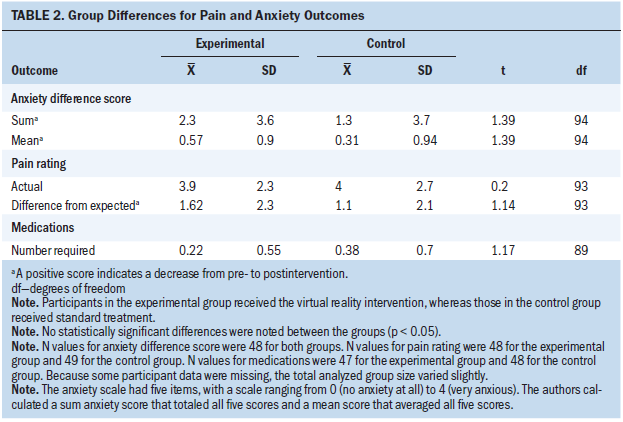
Discussion
Participants who wore virtual reality goggles during the bone marrow aspiration and biopsy procedure did not experience a statistically significant decrease in pain and anxiety—a finding that is inconsistent with the study’s hypotheses. However, participants in the experimental and control groups did report a decrease in pain and anxiety levels from pre- to postprocedure. Possible factors that may have influenced the results need to be explored and considered for future research. For instance, participants in the experimental and control groups viewed nature scenes and listened to relaxing music; the main difference between participants in the two groups was the medium in which the scenes were viewed. Those who had undergone multiple bone marrow aspiration and biopsy procedures prior to the study may be desensitized to the pain and stress associated with the procedure, or they may, conversely, experience heightened anxiety based on their previous experiences. In addition, pain tolerance levels may differ among participants. Given this information, the data collected are pertinent in providing current information to oncology nurses on the subject of virtual reality, a potential new area of pain management during painful procedures. In addition, the intervention was noninvasive and did not cause additional harm to patients undergoing the bone marrow aspiration and biopsy procedure.
Tse, Ng, Chung, and Wong (2002) conducted a randomized, controlled study to determine if replacing hospital surroundings with a more pleasing environment via virtual reality would alleviate pain and anxiety; they reported an increased pain threshold and pain tolerance in patients. Additional studies are needed to assess specific levels of anxiety and psychological data associated with pain scores. In an experimental study involving the use of virtual reality goggles during lumbar puncture, Wint et al. (2002) concluded that virtual reality was a feasible, noninvasive intervention for patients undergoing the procedure, even though no remarkable influence was noted on pain levels. Most participants in the virtual reality group reported that the virtual reality goggles distracted them from the lumbar puncture and requested to use them again; this suggests that use of the intervention made the lumbar puncture a tolerable experience (Wint et al., 2002). Similarly, in the current study, the virtual reality intervention during the bone marrow aspiration and biopsy procedure did not negatively affect patients’ experiences or increase their levels of pain. Patients also indicated that they enjoyed the use of the goggles. A nurse involved with the current study noted the following: “What we’re finding is patients who use the goggles are less anxious about what’s going on around them. It allows them to escape a little bit.”
Malloy and Milling (2010), in a systematic review, found that virtual reality was an effective distraction for reducing pain and discomfort associated with procedures that did not involve needles, such as burn injury care; they found that needle-related studies were less consistent. In a study of needle-related pain, Nilsson, Finnström, Kokinsky, and Enskär (2009) observed no significant differences among the control group and the experimental (virtual reality) group, although the children in the study said they liked virtual reality games and thought the games distracted them. Lechtzin et al. (2010) found that listening to nature sounds and viewing nature scenes were cost-effective means to alleviate pain during the bone marrow aspiration and biopsy procedure. From a clinical standpoint, the finding that the use of virtual reality is similar or even slightly better than standard care for pain and anxiety during the bone marrow aspiration and biopsy procedure is important because nurses can consider it as another tool for patient comfort and support.
Limitations
The bone marrow aspiration and biopsy procedure was performed by different providers, which may have produced different levels of pain and anxiety in patients. This limitation was minimized by the use of consistent procedure room staff, a defined procedure, and randomization of participant selection. In addition, the virtual reality goggles were cumbersome, and participants were required to lie face down on the table during the procedure, resulting in possible discomfort or inability to experience the full virtual reality scene. Occasionally, patients complained of dizziness associated with the goggles; however, this was rare. The earphones became defective after multiple uses (e.g., sound and audio not clear, static) and were difficult to keep positioned inside patients’ ears.
Several unmeasured factors (including patient characteristics, like comorbidities, disease severity, functional status, and personal coping) may have also confounded the findings. Replicating this study with a true random assignment or while controlling for patient characteristics would further inform researchers of the impact of virtual reality on patient outcomes. This type of additional research would also be useful in helping nurses to identify patients for which this intervention would be most effective.
The current study may be limited by the similarity of the experimental and control groups. Researchers originally thought that using the goggles would block out more of the procedure than watching the television. Because both groups viewed similar scenes during the procedure, the virtual reality goggles were the only difference between groups. Their similarity is likely the reason no difference in pain and anxiety levels was reported. Taking away the television for the control group would be unethical because viewing a television during the procedure was considered to be standard practice and was what patients were accustomed to.
Another possible weakness to consider is power of the sample size. One difficulty in calculating power is determining what is a clinically significant difference. Walker et al. (2014), in a study of virtual reality distraction in reduction of pain and anxiety during cytoscopy, found that a power analysis with a 20% difference between groups was a clinically significant difference. The sample size in the current study was double that in the Walker et al. (2014) study (22 in the experimental group, which used virtual reality during cystoscopy; 23 in the control group), but results of the current study showed no significant differences between groups. It is possible that a larger sample in the current study may have produced statistically significant differences between groups, but the sample size was apparently adequate to show a 20% difference.
Strengths of the current study include the use of subjective and objective (vital signs) measures. The virtual reality goggles proved to be a feasible, noninvasive alternative to traditional pharmacologic treatment, and they did not increase the level of pain in participants undergoing the bone marrow aspiration and biopsy procedure. Their use has proved to be at least as effective as the current practice of watching similar scenes on a television. It is important to note that virtual reality technology has improved and expanded since this study was first designed. Further research is needed with various types of virtual reality technologies to determine if virtual reality goggles are an effective alternative to other forms of nonpharmacologic care during painful procedures, such as bone marrow aspiration and biopsy.
Implications for Nursing
Nonpharmacologic measures exist in the hospital and ambulatory settings to decrease or control symptoms in patients with cancer. Nurses should advocate for interventions with minimal side effects or sequela and particularly for those done solely as a nursing intervention, without the order of a physician. In a study by Nilsson et al. (2009), qualitative data suggested that if a virtual reality game (which provides interaction and engagement of the user’s senses because he or she is challenged by the goals of the game) is used, it should be enjoyable and age appropriate.
Virtual reality can have a significant impact on health care, including in education and training via simulation laboratories, in practice with robotic surgery and diagnostics, and in patient care with the addressing of stress and pain. More opportunities to apply technology in health care, particularly in terms of patient care, will be available in the near future. Nurses should research and adapt technology to benefit patients in all appropriate settings. Continued study will offer insight into novel means to address patients’ needs. 
Conclusion
Virtual reality goggles give patients with cancer an important option for distraction that may reduce pain and anxiety associated with the bone marrow aspiration and biopsy procedure, particularly in patients with virtual reality experience. Using the virtual reality goggles may help to distract patients from the procedure and the clinical environment in a way that is similar to watching television. To advocate for and provide optimal patient care, nurses should consider cost-effective, easy-to-use, and noninvasive complementary therapies, including virtual reality. The costs of virtual reality goggles (about $200–$800) will have to be taken into consideration.
Based on the findings of the current study, future research and investigation of the use of virtual reality distraction in clinical application is needed to establish research-based practices for management of procedural pain. Advances in virtual reality technology may offer more insight and information on the benefits associated with this supportive intervention for pain and anxiety during the bone marrow aspiration and biopsy procedure.
The authors gratefully acknowledge Jenny Arthur, RN, MS, OCN®, and Marcia Jacobson, MSN, RN, OCN®, for clinical assistance with the study.
About the Author(s)
Catherine Glennon, RN, MHS, OCN®, NE-BC, is the director of patient and community education at the University of Kansas Cancer Center in Kansas City; Susan F. McElroy, PhD, RN, NEA-BC, is the senior director of patient care services research at Children’s Mercy Hospital in Kansas City, MO; Lynne M. Connelly, PhD, RN, is an adjunct professor in the Department of Nursing at the University of Saint Mary in Leavenworth, KS; Lisa Mische Lawson, PhD, CTRS, is an associate professor in the Department of Occupational Therapy Education at the University of Kansas Medical Center in Kansas City; Abigail M. Bretches, MOT, is an occupational therapist at Blue Valley School District in Kansas City, KS; Allyson R. Gard, MOT, is an occupational therapist at Aegis Therapies in Parsons, KS; and Lexsie R. Newcomer, MOT, is an occupational therapist at Quantum Health Professionals in Overland Park, KS. Glennon serves on speakers bureaus for Merck and Novartis Pharmaceuticals, and has received additional support from Sigma Theta Tau International, Delta chapter. Glennon and Connelly contributed to the conceptualization and design. Glennon completed the data collection. Glennon, McElroy, Mische Lawson, and Newcomer provided statistical support. Glennon, McElroy, Connelly, Mische Lawson, Bretches, and Newcomer provided the analysis. All authors contributed to the manuscript preparation. Glennon can be reached at cglennon@kumc.edu, with copy to ONFEditor@ons.org. (Submitted August 2017. Accepted February 12, 2018.)
References
Brunetti, G.A., Tendas, A., Meloni, E., Mancini, D., Maggiore, P., Scaramucci, L., . . . Alimena, G. (2011). Pain and anxiety associated with bone marrow aspiration and biopsy: A prospective study on 152 Italian patients with hematological malignancies. Annals of Hematology, 90, 1233–1235.
Cerichione, C., Picardi, M., Pugliese, N., Pepa, R.D., Gravetti, A., Casoria, A., . . . Martinelli, V. (2017). Combined oral administration of analgesia and anxiolysis for pain associated with bone marrow aspiration and biopsy. Blood, 130(Suppl. 1), 4715.
Chirico, A., Lucidi, F., De Laurentiis, M., Milanese, C., Napoli, A., & Giordano, A. (2016). Virtual reality in health system: Beyond entertainment. A mini-review on the efficacy of VR during cancer treatment. Journal of Cellular Physiology, 231, 275–287.
Degen, C., Christen, S., Rovo, A., & Gratwohl, A. (2010). Bone marrow examination: A prospective survey on factors associated with pain. Annals of Hematology, 89, 619–624.
Gershon, J., Zimand, E., Lemos, R., Rothbaum, B.O., & Hodges, L. (2003). Use of virtual reality as a distractor for painful procedures in a patient with pediatric cancer: A case study. Cyberpsychology and Behavior, 6, 657–661.
Grønkjær, M., Hasselgren, C.F., Østergaard, A.S., Johansen, P., Korup, J., Bøgsted, M., . . . Jensen, P. (2016). Bone marrow aspiration: A randomized controlled trial assessing the quality of bone marrow specimens using slow and rapid aspiration techniques and evaluating pain intensity. Acta Haematologica, 135, 81–87.
Harrington, S., Gilchrist, L., & Sander, A. (2014). Breast Cancer EDGE Task Force outcomes: Clinical measures of pain. Rehabilitation Oncology, 32, 13–21.
Hjortholm, N., Jaddini, E., Hałaburda, K., & Snarski, E. (2013). Strategies of pain reduction during bone marrow biopsy. Annals of Hematology, 92, 145–149.
Hua, Y., Qiu, R., Yao, W.-Y., Zhang, Q., & Chen, X.-L. (2015). The effect of virtual reality distraction on pain relief during dressing changes in children with chronic wounds on lower limbs. Pain Management Nursing, 16, 685–691.
Kindler, C.H., Harms, C., Amsler, F., Ihde-Scholl, T., & Scheidegger, D. (2000). The visual analog scale allows effective measurement of preoperative anxiety and detection of patients’ anesthetic concerns. Anesthesia and Analgesia, 90, 706–712.
Kjeldsen, H.B., Klaussen, T.W., & Rosenberg, J. (2015). Preferred presentation of the visual analog scale for measurement of postoperative pain. Pain Practice, 16, 980–984.
Lechtzin, N., Busse, A.M., Smith, M.T., Grossman, S., Nesbit, S., & Diette, G.B. (2010). A randomized trial of nature scenery and sounds versus urban scenery and sounds to reduce pain in adults undergoing bone marrow aspirate and biopsy. Journal of Alternative and Complementary Medicine, 16, 965–972.
Lidén, Y., Olofsson, N., Landgren, O., & Johansson, E. (2012). Pain and anxiety during bone marrow aspiration/biopsy: Comparison of ratings among patients versus health-care professionals. European Journal of Oncology Nursing, 16, 323–329.
Malloy, K.M., & Milling, L.S. (2010). The effectiveness of virtual reality distraction for pain reduction: A systematic review. Clinical Psychology Review, 30, 1011–1018.
National Cancer Institute. (n.d.). NCI dictionary of cancer terms: Hematologic cancer. Retrieved from https://bit.ly/2sylxot
Nilsson, S., Finnström, B., Kokinsky, E., & Enskär, K. (2009). The use of virtual reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. European Journal of Oncology Nursing, 13, 102–109.
Schneider, S.M., & Hood, L.E. (2007). Virtual reality: A distraction intervention for chemotherapy. Oncology Nursing Forum, 34, 39–46. https://doi.org/10.1188/07.ONF.39-46
Schneider, S.M., Prince-Paul, M., Allen, M.J., Silverman, P., & Talaba, D. (2004). Virtual reality as a distraction intervention for women receiving chemotherapy. Oncology Nursing Forum, 31, 81–88. https://doi.org/10.1188/04.ONF.81-88
Shabanloei, R., Golchin, M., Esfahani, A., Dolatkhah, R., & Rasoulian, M. (2010). Effects of music therapy on pain and anxiety in patients undergoing bone marrow biopsy and aspiration. AORN Journal, 91, 746–751. https://doi.org/10.1016/j.aorn.2010.04.001
Tanasale, B., Kits, J., Kluin, P.M., Trip, A., & Kluin-Nelemans, H.C. (2013). Pain and anxiety during bone marrow biopsy. Pain Management Nursing, 14, 310–317.
Tanja-Dijkstra, K., Pahl, S., White, M.P., Andrade, J., Qian, C., Bruce, M., . . . Moles, D.R. (2014). Improving dental experiences by using virtual reality distraction: A simulation study. PLOS ONE, 9, e91276. https://doi.org/10.1371/journal.pone.0091276
Tse, M.M., Ng, J.K., Chung, J.W., & Wong, T.K. (2002). The effect of visual stimuli on pain threshold and tolerance. Journal of Clinical Nursing, 11, 462–469.
Wahn, B., & König, P. (2017). Is attentional resource allocation across sensory modalities task-dependent? Advances in Cognitive Psychology, 13, 83–96.
Walker, M.R., Kallingal, G.J., Musser, J.E., Folen, R., Stetz, M.C., & Clark, J.Y. (2014). Treatment efficacy of virtual reality distraction in the reduction of pain and anxiety during cystoscopy. Military Medicine, 179, 891–896.
Wint, S.S., Eshelman, D., Steele, J., & Guzzetta, C.E. (2002). Effects of distraction using virtual reality glasses during lumbar punctures in adolescents with cancer [Online exclusive]. Oncology Nursing Forum, 29, E8–E15. https://doi.org/10.1188/02.ONF.E8-E15
Wolitzky, K., Fivush, R., Zimand, E., Hodges, L. & Rothbaum, B.O. (2005). Effectiveness of virtual reality distraction during a painful medical procedure in pediatric oncology patients. Psychology and Health, 20, 817–824.
Zahid, M.F. (2015). Methods of reducing pain during bone marrow biopsy: A narrative review. Annals of Palliative Medicine, 4, 184–193.




